Abstract
Aim
To determine whether short-phase Occupational Performance Coaching combined with service navigation support is feasible for families waiting for autism assessment.
Method
A pilot feasibility study was conducted using a blinded randomization procedure that allocated participants to one of three trial arms: (1) face-to-face coaching, (2) videoconference coaching, and (3) usual care. Outcomes included a retention aim of 70–80%, goal attainment and secondary standardised measures of adaptive behaviour, social skills, parenting stress, service access and family quality of life.
Results
Caregivers and children (n = 16, child mean age of 3 years 7 months) were recruited following referral for an autism assessment. Retention was 75%, with change scores in performance and satisfaction of selected goals higher in the intervention groups than the usual care group.
Interpretation
Findings support progression to a future randomized controlled trial assessing intervention efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Between 1 and 4% of Australian children are diagnosed with an autism spectrum disorder, herein referred to as autism (May et al., 2017). With onset in early childhood, the disorder is characterised by impairments in social communication and behaviour (American-Psychiatric-Association, 2013). Paediatricians, psychiatrists, and allied health professionals including psychologists, speech pathologists and occupational therapists can be sought to assess a child, working individually or in multidisciplinary teams (Whitehouse et al., 2018; Williams et al., 2014). In public health settings, there is a shortage of assessment services when autism-related concerns exist (Bent et al., 2015; Randall, Albein-Urios, Brignell, Gulenc, Hennel, Coates, Symeonides, Hiscock, Marraffa, Silove, Bayl, Woolfenden, & Williams, 2016).
Debate continues nationally and internationally between the notions of comprehensive autism assessment practices, and the need for early diagnoses to support appropriate service access (McKenzie, Forsyth, O’Hare, McClure, Rutherford, Murray, & Irvine, 2016). As a result, children and families can have unique and lengthy pathways to autism assessment (Hennel, Coates, Symeonides, Gulenc, Smith, Price, & Hiscock, 2016; Ward et al., 2016). The delays and confusion along the path from recognition of concerns to assessment can add to stress and concern for parents and families, and delay service access that could assist with each child’s immediate and long-term development Batool & Khurshid, 2015; Gibbs et al., 2019; Rivard et al., 2014; Whitehouse, Varcin, Alvares, Barbaro, Bent, Boutrus, Chetcuti, Cooper, Clark, & Davidson, 2019; Whitehouse 2017).
National guidelines in Australia have sought to address these issues by recommending standardised diagnostic practices (Whitehouse et al., 2018). Functional assessment and intervention are suggested to occur prior to, or concurrently with, the diagnostic assessment process. These guidelines remain broad to ensure their fit with a wide range of settings across Australia. There remains a lack of clarity around best-practice functional assessment and guidance in the pre-diagnostic stage, and lost opportunities continue to be lamented by researchers in the field (Gibbs et al., 2019; Vivanti & Volkmar, 2019).
Function-focused and goal-directed coaching strategies, such as Occupational Performance Coaching (OPC), are gaining support as an evidence-based intervention for parents of children with neurodevelopmental difficulties (Graham et al., 2013; Rivard et al., 2016; Schwellnus et al., 2020; Ward et al., 2019). OPC is a function-focused coaching approach where participants are supported to develop and implement strategies in the context of self-identified participatory goals (Graham et al., 2020). The approach has been used with a variety of populations, including parents of children with disabilities (Angelin et al., 2021; Graham et al., 2020; Kessler et al., 2017). Goal-directed coaching has been delivered via face-to-face (f2f) and telehealth or videoconference modalities with reported success (Boisvert et al., 2010; Little et al., 2018; Ward et al., 2019). Telehealth or videoconference-delivered interventions, have become increasingly favoured and appropriately prioritised in research following the COVID-19 pandemic (Eapen et al., 2021). These are now deemed to be a critical modality for supporting access to interventions, regardless of rural or metropolitan geographical locations (Camden & Silva, 2021; Eapen et al., 2021).
Service navigation and parent support group strategies have been trialled previously with parents of children waiting for autism assessment, with positive outcomes reported relating to assessment completion and parent knowledge (Connolly & Gersch, 2013; Feinberg, Abufhele, Sandler, Augustyn, Cabral, Chen, Diaz Linhart, Cesar Levesque, Aebi, & Silverstein, 2016).
As yet, a brief, individualised coaching intervention combined with service navigation support has not been trialled in a three-arm study, inclusive of a telehealth arm, with parents of children on an autism diagnostic waitlist. Our pilot and feasibility trial aimed to:
-
1.
assess the feasibility, including constructs of acceptability, practicality, and preliminary efficacy, of an RCT study design exploring coaching and service navigation support for families of children waiting for ASD assessment.
-
2.
inform protocol planning for a future RCT to assess efficacy of coaching and service navigation support via face-to-face and videoconference modalities.
Methods
Participants
Participants were identified following referral to either The Royal Children’s Hospital Melbourne (RCH) or Djerriwarrh Health Services in Melton (herein referred to as Melton) for an autism assessment, from December 2018 to June 2019. For referrals relating to children aged 0–7 years (n = 185), parents were sent study information along with their referral outcome letter, and invited to contact the investigator for more information. A follow-up phone call was permitted for the RCH clinic if families did not respond. Interested participants were excluded if the child had already been scheduled for accessed an autism assessment (n = 3), or a parent was currently engaged in regular coaching or mental health support sessions (n = 2). Eligible families who provided written consent participated in baseline measure completion, before being allocated to one of 3 study arms, as below. Enrolled participants were reimbursed for travel and/or parking costs where and when these were incurred, in line with ethics approval from RCH Human Research Ethics Committee.
Intervention
Participants were randomly allocated to one of three study arms; usual-care, videoconference coaching or face-to-face (f2f) coaching. Usual care consisted of existing service access outside of the assessment service to which the child was referred, and telephone access to a part-time assessment service coordinator as required. Participants in the intervention arms received 4 sessions of a manualised intervention, OPC, which has previously been described in detail (Bernie et al., 2021; Graham et al., 2020). In brief, OPC is an evidence-based, function-focused coaching approach, built upon principles of connection, sharing and structure. The approach supports goal attainment for individuals and families through a focus on occupation and enablement. Four sessions of OPC were provided in addition to direct, on-demand service navigation support available to all participants, either face to face or via videoconference modality. Further intervention details are available in the study protocol.
There were no major deviations from the published protocol. Two study participants in the intervention arms accessed an autism assessment at the RCH prior to the 4th session of coaching. The final session of coaching in this instance included a focus on intervention conclusion, and discussing any impact the diagnostic outcome may have had on goal-related strategies or directions developed in previous sessions.
Primary Outcome Measures
Recruitment and retention were calculated at recruitment close and study conclusion. Other primary outcome measures, including goal attainment, were collected at baseline (T0), and follow-up (T1). For families with two parents participating, measures were completed via consensus coding.
Measures were mapped onto feasibility constructs as outlined in the study protocol (Bernie et al., 2021), which included acceptability, practicality, demand, adaptability, and preliminary efficacy. Demand was measured through recruitment, with an aim of between 18 and 24 participants, acceptability and progression to a future RCT via a retention goal of 70–80%, and a post-intervention questionnaire, and preliminary efficacy through functional goal attainment measured by the Canadian Occupational Performance Measure (COPM), 6th Edition (Law et al., 2017). The COPM was administered at baseline (T0) and follow-up (T1), with the support of an interpreter for participants who were not proficient in English. When completing the COPM at baseline, parents identified areas of concern in daily occupations and then prioritised them. These could be concerns for their child or family relating to work or school, self-care activities, leisure or play at home or in the community. Areas of concern rated by the parent(s) for current performance and satisfaction, with higher scores representing higher performance and satisfaction levels.
Secondary Outcome Measures
Participant completion rates and measurement at T0 and T1 were completed, including the Vinelands Adaptive Behaviour Scales (VABS) 3 (Sparrow et al., 2016), the Social Responsiveness Scale (SRS) 2 (Constantino & Gruber, 2012), the Beech Family Quality of Life Scale (FQOL) (Park, Hoffman, Marquis, Turnbull, Poston, Mannan, Wang, & Nelson, 2003), and the short form of the Parenting Stress Index (PSI) (Abidin, 1990). Baseline information including demographic data such as postcode and current service access was also collected via parent questionnaire and included direct reporting of medical and allied health professionals being accessed at baseline and follow-up. Socioeconomic status (Australian Bureau of Statistics, 2011) and other related data are presented in Table 1.
Implementation and Practicality
The Measure of Processes of Care − 20 (MPOC-20) (King et al., 2004) was used for parent ratings about care from current services, and to assess feasibility constructs of implementation and practicality. Parents reported on the nature and family-centredness of care received by rating provisions of specific and general information, respectful and coordinated care, and enabling and partnership on a scale, from “not at all” or 1 to “a very great extent” or 7. For the purposes of this study, parents were asked to provide one aggregate rating for all current services received, including receipt of the study intervention for participants in intervention arms at follow-up (T1).
Statistical Analysis
Analyses included proportions for recruitment and retention (expected 70–80%), and change scores in COPM “performance” and “satisfaction” ratings, with a change of 2 points considered to be clinically significant (Verkerk et al., 2006). The direction of change across a number of secondary outcomes measuring child adaptive skills, social skills, service access, parenting stress and family quality of life were also explored (detailed below).
Results
Recruitment, retention and study flow are detailed in Fig. 1.
Recruitment
128 children at RCH and 57 children at Melton were considered eligible during the recruitment period from December 2018 to May 2019. At RCH, 31 (24%) expressed interest for further information, and 12 (21%) responded with interest at Melton, with a parent information form sent. Of those, 20 families from RCH returned consent forms and 2 from Melton. Three parents reported their child had already accessed an autism assessment elsewhere and were deemed ineligible, and a further child was excluded because their parent was engaged in regular mental health support. One family was lost-to-follow-up before being allocated a study number. Overall 16 families (9% of eligible participants) were recruited. No further recruitment was sought due to researcher time constraints.
The characteristics of recruited families are reported in Table 1.
Of the 16 families, there were 12 mother-child dyads, 1 father-child dyad, and 3 mother-father-child triads (hereon groups will be referred to as participants). Recruited child participants were 11 males and 5 females. All families lived in Victoria, Australia, with 14 of the 16 families (87.5%) from metropolitan Melbourne.
Retention
In total, four enrolled families withdrew from the study to yield an overall retention of 75%. Three withdrew from usual-care, and one withdrew from f2f coaching. The two families recruited from Melton were not retained.
Measure Completion
Primary outcome measure completion (detailed in Table 2) was 100% for retained participants. All parents were able to identify between 2 and 4 functional goals pertaining to their child and family for observation over the study period. Secondary measures were completed by at least 75% of participants. Reasons for reduced completion were the child being too young for age range of questionnaire (n = 2), interpreter not available (n = 2) and questionnaire burden/time limitations (n = 3).
Most participants (n = 10, 92%) attended two baseline sessions to complete study measures. Baseline sessions occurred within 2 weeks of each other for all participants. The mean duration between final baseline session (T0) and follow up (T1) for all families was 5.1 months (SD of 1.0 months). There were no significant differences between study arms for duration between baseline and follow up (F(2, 9) = 1.39, p = 0.299). All participants, apart from those that used interpreters (n = 2), completed follow-up measures within one hour.
Acceptability of Intervention from Parent Report
Participants who received coaching intervention were asked about aspects of the intervention and its practicality via an optional, anonymous questionnaire which asked about intervention attributes such as location, duration, and satisfaction with outcomes (included as supplementary material). All questionnaire responders (N = 6, 75%) reported that they agreed or strongly agreed that they were satisfied with the intervention overall.
Implementation, Integration and Practicality
Intervention Implementation
All retained participants in the intervention arms participated in 4 interventions sessions, lasting between 35 min and 1 h and 10 min. Interval times between sessions ranged from 1 week to 5 weeks (median of 2 weeks). Strategies to address goals identified at baseline were developed and discussed throughout the sessions in line with OPC principles. Participants were able to trial strategies developed during coaching across relevant contexts and reflect on those in subsequent sessions. All participants in Videoconference Coaching were all able to download and use videoconference technologies to engage in the intervention.
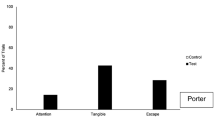
Implementation and Practicality of Care (Measure of Processes of Care − 20)
At baseline, 8/12 (75%) of participants were accessing services of an ongoing nature to enable ratings of service quality across five subtests of the MPOC-20. All participants rated care processes at follow-up. For those with available pre and post data, gains occurred with higher frequency for those in the intervention arms (n = 4) across the five subtests of the MPOC-20 (n = 13/20, 65%), than in the usual-care (n = 4) group (n = 8/20, 40%). Greatest gains in the intervention arms were seen for the subtests of Providing General Information (mean change of 4.4 versus 1.0 for usual-care), Providing Specific Information (mean change of 2.8 compared with 0.8 for usual-care) and Coordinated Care (mean change of 2.5 compared with 0.3 for usual-care).
Parent Report
Participants who completed the post-hoc feasibility questionnaire agreed that coaching sessions were easy to take part in, and the number of sessions were appropriate for family needs. Responders who participated via videoconference agreed that technologies were easy to use and download, and that the location of intervention (their homes) was a good fit. Two of the 3 families (66%) in f2f coaching were uncertain whether the location was a good fit. Most who received intervention (83%) found the length of the sessions to be appropriate.
Cost, Resources, Time
Participants required a mean of 2.5 h of clinician researcher time to complete baseline and follow-up measures. In the intervention arms, participants required a mean of 4 h for the four coaching sessions. Those allocated to f2f coaching had additional travel time to and from sessions, varying from 50 min to 3 h of travel time, and parking costs at approximately $8.00 per hour. Participant’s funded their own internet access and devices for Arm B (intervention via videoconference).
Adaptation and Expansion
OPC was successfully delivered in a 4-session format for participating families, with adequate fidelity in both videoconference and f2f modalities. Four participants were randomly selected for OPC fidelity measurement, from groups of 3 enrolled participants, in line with recommended procedures. Fidelity scores ranged from 72 to 84%, with a mean score of 81% (Graham et al., 2020).
From the post-intervention questionnaire, most participants (n = 5, 83%) reported that they would recommend the intervention to others who are either waiting for an autism assessment, or to families of children with additional support needs.
Limited Efficacy Testing (Primary Outcomes)
In the intervention arms, 6 out of 8 participants (75%) moved on average 2 points or greater on the performance and satisfaction scales. In the usual-care group, 1of 4 (25%) participants moved 2 points or more on average on the performance and satisfaction scales. Table 2 details mean change scores and effect size calculations for performance and satisfaction ratings from T0 to T1 across each intervention arm.
Limited Efficacy Testing (Secondary Outcomes)
Standardised and non-standardised measures were collected to inform limited efficacy findings and explore participation rates for tool and data completion. Table 3 details completion rates and findings for secondary measures.
Discussion
This pilot and feasibility trial explored the use of pre-assessment Occupational Performance Coaching or OPC, in addition to service navigation support, to better utilise waiting times that may in turn improve family and child outcomes. It was the first to compare usual-care, face-to-face and videoconference coaching for families of children waiting for an autism assessment. Findings indicate that both the study and the intervention were feasible for participants, with retention meeting pre-designated standards, and high ratings of intervention acceptability and practicality from parent reports. Parent-reported satisfaction with OPC, when applied to children and families awaiting autism assessment, is in line with previous OPC studies (Graham et al., 2013, 2020).
Retention was higher in the intervention arms of the study, and highest for videoconference coaching, with no withdrawals. These findings support growing evidence that videoconference-delivered coaching is feasible and acceptable to families, in line with shifts in recent years to this mode of intervention delivery (Eapen et al., 2021; Gentry, Puspitasari, McKean, Williams, Breitinger, Geske, Clark, Moore, Frye, & Hilty, 2021; Taylor, Caffery, Gesesew, King, Bassal, Ford, Kealey, Maeder, McGuirk, Parkes, & Ward, 2021). OPC is built on principles of connection and sharing, and emphasises explicit relationship development with autonomy support strategies (Graham et al., 2020). These attributes are likely to be facilitative in engaging participants in the intervention from early in sessions, with no barriers observed in the videoconference modality in relationship-building or support provision. The foundations of OPC and known benefits of goal-setting (Cusick et al., 2007) are likely contributors in observed retention in this study, which was similar to other feasibility studies exploring occupation-focused coaching (Kessler et al., 2017; Little et al., 2018). .
All participants made gains on selected goal performance and satisfaction, measured by the COPM. This is not unexpected given enrolled participants were likely motivated to seek services and support for their child and family within and outside of the study. Of note was the greater magnitude of change in goal performance and satisfaction in the intervention arms, compared with usual-care. These preliminary efficacy findings are important because they support the notion that OPC can help families achieve functional goals for the child and family, prior to receiving information provided following diagnostic assessment. This is a critical time to act when considering lengthy waitlists and optimal time for neurodevelopmental change, and findings are in contrast to the notion that diagnostic clarification is required before individualised therapy can commence (Mandell et al., 2010; Matson, 2007). This finding, in combination with high intervention fidelity ratings, provides support for further efficacy testing in an appropriately-powered RCT, to explore potential intervention benefits for families on a larger scale.
The variation in access to existing services by study participants, both at baseline and across the study period, is likely to reflect both variable clinical presentations and service access inequities. At baseline, some families were not yet accessing any intervention services, whilst others had engaged multiple therapies prior to study enrolment. Participants’ service access also changed over the study period, with slightly higher mean increases observed in the intervention groups for numbers of services accessed. These findings provide further support for continued exploration of coaching while waiting for autism assessment, which may be able to facilitate more equitable access to needed services in this period. From a study viewpoint, service access variability is likely to interact with efficacy outcome measures and subsequent RCT findings. A future RCT will need to consider closer tracking of the number, type, duration, and intensity of current and newly-engaged services across the study period, to allow for further analyses relating to their contribution.
Secondary measures were feasible for most families to complete at baseline and follow-up. Results pertaining to secondary measures were not powered to assess efficacy, especially given the variable nature of child developmental trajectories and variation in service engagement observed in the sample. Initial positive trends for decreased parental stress, particularly in the videoconference arm of the study, are nonetheless a promising preliminary finding. Parental stress relating to caring for children diagnosed with ASD, and those waiting on waiting lists, is elevated compared to those not waiting or diagnosed (Batool & Khurshid, 2015; Feinberg et al., 2016; Rivard et al., 2014). It is important to further evaluate the efficacy of pre-diagnostic coaching, such as OPC, in reducing parental stress, particularly when delivered via videoconference. Data on parent sense-of-competence was not collected in this study, and should be included in a future trial, in line with recent recommendations for coaching studies involving primary caregivers (20).
The sample size for this study was small due to study design, recruitment limitations and study withdrawals, particularly from usual-care. Recruitment may have been limited by the exploratory nature of this study, and it is anticipated that a future RCT imbedded in clinical care will overcome this limitation. Participants receiving usual-care were asked to complete a number of measures without any option for future intervention, which may account for this study arm having highest rates of withdrawal. These limitations can be addressed in future studies by ensuring particular elements, such as standardised best-care assessment and goal-setting, are embedded in standards of care prior to commencement. Recruitment and retention in the field of childhood disability research is an ongoing challenge for investigators, particularly for intervention studies that require time investment from carers of young children (Phoenix et al., 2020). This is despite efforts, such as those undertaken in this study, to ensure participation is cost neutral and burdens are ethically appropriate. The burdens of travel were, and should continue to be minimised by utilising videoconference modalities. Extensive questionnaire completion was noted as a reason for withdrawals in this study, and should also be minimised, with information collection in a future RCT restricted to those of high value in service development decision making. Weighted randomisation may be an additional consideration so that predicted withdrawals can occur without compromising RCT aims and minimum sample size requirements. In this trial randomisation was blinded, however, the researcher completing data collection was not blinded to arm allocation. To avoid bias, a future RCT should be double-blinded.
Interpreters were used for two primary-carer participants who were not proficient in English. Both required the maximum permissible time of two one-hour-long sessions to complete baseline measures, and a small number of secondary measures were not completed. The optional post-intervention questionnaire was not completed by these caregivers, and the applicability of feasibility findings to individuals with English as a second language should be interpreted with caution. Neither family withdrew from the study, despite time requirements and communication challenges. Extended time provisions, in addition to use of questionnaires that have been validated in a participants’ first language, would need to be considered in future RCT planning to continue to ensure equitable family inclusion.
Findings indicate that the present study was able to be implemented as designed, with high retention rates and parent-reported satisfaction, as well as preliminary findings indicating the potential to improve child and family outcomes prior to autism assessment. Of particular note are the positive findings around feasibility of OPC when delivered via videoconference, and the positive outcome trends observed in this intervention arm. Given the pandemic-related service changes currently occurring worldwide, and growing support for videoconference interventions broadly, it is prudent to focus on further efficacy testing of OPC and service navigation support delivered using this modality. There is the potential to turn wasted waiting times into active intervention periods that can benefit the child, parents, and family.
Abbreviations
- ASD:
-
Autism Spectrum Disorder
- CONSORT:
-
Consolidated Standards of Reporting Trials
- COPM:
-
Canadian Occupational Performance Measure
- F2f:
-
Face-to-face
- MPOC:
-
Measure of Processes of Care
- OPC:
-
Occupational Performance Coaching
- RCH:
-
The Royal Children’s Hospital, Melbourne, Australia
- RCT:
-
randomised controlled trial
References
Abidin, R. R. (1990). Parenting Stress Index (PSI). Pediatric Psychology Press
American-Psychiatric-Association. (2013). The diagnostic and statistical manual of mental disorders-fifth edition; DSM-5. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425596
Angelin, C. S., Sugi, S., & Rajendran, K. (2021). Occupational Performance Coaching for Mothers of Children with Disabilities in India. Can J Occup Ther, 88(1), 38–47. https://doi.org/10.1177/0008417420972868
Australian Bureau of Statistics. (2011). Socio-economic Indexes for areas 2011. Canberra: Australian Bureau of Statistics
Batool, S. S., & Khurshid, S. (2015). Factors Associated with Stress Among Parents of Children with Autism. J Coll Physicians Surg Pak, 25(10), 752–756. https://doi.org/10.2015/JCPSP.752756 ([Erratum appears in J Coll Physicians Surg Pak. 2016 Feb;26(2):166; PMID: 26876415])
Bent, C. A., Dissanayake, C., & Barbaro, J. (2015). Mapping the diagnosis of autism spectrum disorders in children aged under 7 years in Australia, 2010–2012. Med J Aust, 202(6), 317–320. https://doi.org/10.5694/mja14.00328
Bernie, C., Williams, K., Graham, F., & May, T. (2021). Coaching While Waiting for Autism Spectrum Disorder Assessment: Protocol of a Pilot Feasibility Study for a Randomized Controlled Trial on Occupational Performance Coaching and Service Navigation Support. JMIR Res Protoc, 10(1), e20011. https://doi.org/10.2196/20011
Boisvert, M., Lang, R., Andrianopoulos, M., & Boscardin, M. L. (2010). Telepractice in the assessment and treatment of individuals with autism spectrum disorders: A systematic review. Dev Neurorehabil, 13(6), 423–432. https://doi.org/10.3109/17518423.2010.499889
Camden, C., & Silva, M. (2021). Pediatric teleheath: opportunities created by the COVID-19 and suggestions to sustain its use to support families of children with disabilities. Phys Occup Ther Pediatr, 41(1), 1–17. https://doi.org/10.1080/01942638.2020.1825032
Connolly, M., & Gersch, I. (2013). A support group for parents of children on a waiting list for an assessment for autism spectrum disorder. Educ Psychol Pract, 29(3), 293–308. https://doi.org/10.1080/02667363.2013.841128
Constantino, J. N., & Gruber, C. P. (2012). The Social Responsiveness Scale Manual, Second Edition (SRS-2). Western Psychological Services
Cusick, A., Lannin, N. A., & Lowe, K. (2007). Adapting the Canadian Occupational Performance Measure for use in a paediatric clinical trial. Disabil Rehabil, 29(10), 761–766. https://doi.org/10.1080/09638280600929201
Eapen, V., Hiscock, H., & Williams, K. (2021). Adaptive innovations to provide services to children with developmental disabilities during the COVID-19 pandemic. J Paediatr Child Health, 57(1), 9–11. https://doi.org/10.1111/jpc.15224
Feinberg, E., Abufhele, M., Sandler, J., Augustyn, M., Cabral, H., Chen, N. … Silverstein, M. (2016). Reducing Disparities in Timely Autism Diagnosis Through Family Navigation: Results From a Randomized Pilot Trial. Psychiatr Serv, 67(8), 912–915. https://doi.org/10.1176/appi.ps.201500162
Gentry, M. T., Puspitasari, A. J., McKean, A. J., Williams, M. D., Breitinger, S., Geske, J. R. … Hilty, D. M. (2021). Clinician Satisfaction with Rapid Adoption and Implementation of Telehealth Services During the COVID-19 Pandemic. Telemed J E Health. https://doi.org/10.1089/tmj.2020.0575
Gibbs, V., Aldridge, F., Sburlati, E., Chandler, F., Smith, K., & Cheng, L. (2019). Missed opportunities: An investigation of pathways to autism diagnosis in Australia. Res Autism Spectr Disord, 57, 55–62. https://doi.org/10.1016/j.rasd.2018.10.007
Graham, F., Kennedy-Behr, A., & Ziviani, J. (2020). Occupational Performance Coaching: A Manual for Practitioners and Researchers. Routledge
Graham, F., Rodger, S., & Ziviani, J. (2013). Effectiveness of occupational performance coaching in improving children’s and mothers’ performance and mothers’ self-competence. Am J Occup Ther, 67(1), 10–18. https://doi.org/10.5014/ajot.2013.00464
Hennel, S., Coates, C., Symeonides, C., Gulenc, A., Smith, L., Price, A. M., & Hiscock, H. (2016). Diagnosing autism: Contemporaneous surveys of parent needs and paediatric practice. J Paediatr Child Health, 52(5), 506–511. https://doi.org/10.1111/jpc.13157
Kessler, D., Egan, M., Dubouloz, C. J., McEwen, S., & Graham, F. P. (2017). Occupational Performance Coaching for Stroke Survivors: A Pilot Randomized Controlled Trial. Am J Occup Ther, 71(3), 7103190020. https://doi.org/10.5014/ajot.2017.024216
King, S., King, G., & Rosenbaum, P. (2004). Evaluating health service delivery to children with chronic conditions and their families: Development of a refined measure of processes of care (MPOC – 20). Child Health Care, 33(1), 35–57. https://doi.org/10.1207/s15326888chc3301_3
Law, M., Baptiste, S., Carswell, A., McColl, M. A., Polatajko, H. J., & Pollock, N. (2017). COPM: Canadian Occupational Performance Measure 5th Edition. Canadian Assiciation of Occupational Therapists
Little, L. M., Pope, E., Wallisch, A., & Dunn, W. (2018). Occupation-Based Coaching by Means of Telehealth for Families of Young Children With Autism Spectrum Disorder. Am J Occup Ther, 72(2), 7202205020. https://doi.org/10.5014/ajot.2018.024786
Mandell, D. S., Morales, K. H., Xie, M., Lawer, L. J., Stahmer, A. C., & Marcus, S. C. (2010). Age of Diagnosis Among Medicaid-Enrolled Children With Autism, 2001–2004 [research-article]. Psychiatric Services, 61(8), 822–829. https://doi.org/KI
Matson, J. L. (2007). Current status of differential diagnosis for children with autism spectrum disorders. Res Dev Disabil, 28(2), 109–118. https://doi.org/10.1016/j.ridd.2005.07.005
May, T., Sciberras, E., Brignell, A., & Williams, K. (2017). Autism spectrum disorder: updated prevalence and comparison of two birth cohorts in a nationally representative Australian sample. BMJ Open, 7(5), e015549. https://doi.org/10.1136/bmjopen-2016-015549
McKenzie, K., Forsyth, K., O’Hare, A., McClure, I., Rutherford, M., Murray, A., & Irvine, L. (2016). The relationship between waiting times and ‘adherence’ to the Scottish Intercollegiate Guidelines Network 98 guideline in autism spectrum disorder diagnostic services in Scotland. Autism, 20(4), 395–401. https://doi.org/10.1177/1362361315586136
Park, J., Hoffman, L., Marquis, J., Turnbull, A. P., Poston, D., Mannan, H. … Nelson, L. L. (2003). Toward assessing family outcomes of service delivery: validation of a family quality of life survey. J Intellect Disabil Res, 47(Pt 4–5), 367–384. https://doi.org/10.1046/j.1365-2788.2003.00497.x
Phoenix, M., Chiarello, L., Pinto, M., & King, G. (2020). Recruitment in Pediatric Rehabilitation Research: Challenges, Strategies, Impact on Evidence-Informed Care, and a Call to Action. Phys Occup Ther Pediatr, 40(4), 365–370. https://doi.org/10.1080/01942638.2020.1748984
Randall, M., Albein-Urios, N., Brignell, A., Gulenc, A., Hennel, S., Coates, C. … Williams, K. (2016). Diagnosing autism: Australian paediatric research network surveys. J Paediatr Child Health, 52(1), 11–17. https://doi.org/10.1111/jpc.13029
Rivard, M., Morin, M., Mercier, C., Terroux, A., Mello, C., & Lépine, A. (2016). Social Validity of a Training and Coaching Program for Parents of Children With Autism Spectrum Disorder on a Waiting List for Early Behavioral Intervention. J Child Fam Stud, 26(3), 877–887. https://doi.org/10.1007/s10826-016-0604-5
Rivard, M., Terroux, A., Parent-Boursier, C., & Mercier, C. (2014). Determinants of stress in parents of children with autism spectrum disorders [Developmental Disorders & Autism 3250]. J Autism Dev Disord, 44(7), 1609–1620. https://doi.org/10.1007/s10803-013-2028-z(Journal of Autism & Childhood Schizophrenia)
Schwellnus, H., King, G., Baldwin, P., Keenan, S., & Hartman, L. R. (2020). A Solution-Focused Coaching Intervention with Children and Youth with Cerebral Palsy to Achieve Participation-Oriented Goals. Phys Occup Ther Pediatr, 40(4), 423–440. https://doi.org/10.1080/01942638.2020.1711841
Sparrow, S., Cicchetti, D. V., & Saulnier, C. A. (2016). Vineland adaptive behavior scales, (Vineland-3). Psychological Corporation
Taylor, A., Caffery, L. J., Gesesew, H. A., King, A., Bassal, A. R., Ford, K. … Ward, P. R. (2021). How Australian Health Care Services Adapted to Telehealth During the COVID-19 Pandemic: A Survey of Telehealth Professionals. Front Public Health, 9, 648009. https://doi.org/10.3389/fpubh.2021.648009
Verkerk, G. J., Wolf, M. J., Louwers, A. M., Meester-Delver, A., & Nollet, F. (2006). The reproducibility and validity of the Canadian Occupational Performance Measure in parents of children with disabilities. Clin Rehabil, 20(11), 980–988. https://doi.org/10.1177/0269215506070703
Vivanti, G., & Volkmar, F. R. (2019). National Guideline for the Assessment and Diagnosis of Autism Spectrum Disorders in Australia (Whitehouse, Evans et al. 2018). In: Springer
Ward, R., Reynolds, J. E., Pieterse, B., Elliott, C., Boyd, R., & Miller, L. (2019). Utilisation of coaching practices in early interventions in children at risk of developmental disability/delay: a systematic review. Disabil Rehabil, 42(20), 2846–2867. https://doi.org/10.1080/09638288.2019.1581846
Ward, S. L., Sullivan, K. A., & Gilmore, L. (2016). Practitioner Perceptions of the Assessment and Diagnosis of Autism in Australia. Aust Psychol, 51(4), 272–279. https://doi.org/10.1111/ap.12211
Whitehouse, A., Evans, K., Eapen, V., & Wray, J. (2018). A National Guideline for the Assessment and Diagnosis of Autism Spectrum Disorder in Australia. Cooperative Research Centre for Living with Autism
Whitehouse, A. J., Varcin, K. J., Alvares, G. A., Barbaro, J., Bent, C., Boutrus, M. … Davidson, E. (2019). Pre-emptive intervention versus treatment as usual for infants showing early behavioural risk signs of autism spectrum disorder: a single-blind, randomised controlled trial. Lancet Child Adolesc Health, 3(9), 605–615. https://doi.org/10.1016/S2352-4642(19)30184-1
Whitehouse, A. J. O. (2017). Elizabeth Usher Memorial Lecture: Rethinking the clinical pathway for autism spectrum disorder and challenging the status quo. Int J Speech Lang Pathol, 19(3), 208–217. https://doi.org/10.1080/17549507.2016.1276963
Williams, K., Woolfenden, S., Roberts, J., Rodger, S., Bartak, L., & Prior, M. (2014). Autism in context 1: Classification, counting and causes. J Paediatr Child Health, 50(5), 335–340. https://doi.org/10.1111/jpc.12451
Acknowledgments and Funding
The research team would like to acknowledge the generous contribution of Sue and Leigh Clifford, whose funding through the Clifford Family Scholarship has enabled this research to take place within allocated time frames and at neutral cost to families. We would also like to acknowledge the support of the Department of Paediatrics at the University of Melbourne, the Murdoch Children’s Research Institute, and The Royal Children’s Hospital, particularly the Allied Health Department. Most importantly, we are grateful to the families who have donated their time to the project. This project has been funded through the Melbourne Research Scholarship, The Clifford Family Scholarship, and the Developmental Disabilities and Rehabilitation Research Top-up Scholarship.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
All authors contributed to the study design and manuscript revisions, following primary contributions by CB, TM, and KW. All authors read and approved the final manuscript. The corresponding author can provide further study details upon request.
Corresponding author
Ethics declarations
Conflicts of Interest
None declared.
Ethics Approval
All procedures in this study were conducted in accordance with the ethical standards of the institutions housed at the Melbourne Children’s Campus, in line with the 1964 Helsinki Declaration and its later amendments. This trial was approved by The Royal Children?s Hospital Human Research Ethics Committee (HREC 38154A).
Trial Registration
ACTRN12620000164998
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bernie, C., Williams, K., Graham, F. et al. Coaching While Waiting for Autism Spectrum Disorder Assessment: A Pilot Feasibility Study for a Randomized Controlled Trial on Occupational Performance Coaching and Service Navigation. J Autism Dev Disord 53, 2905–2914 (2023). https://doi.org/10.1007/s10803-022-05558-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-022-05558-3