Abstract
Purpose
To investigate the clinical features, management, and prognosis of full-thickness macular holes (FTMHs) inadvertently created during vitrectomy for eyes with proliferative diabetic retinopathy (PDR) and fibrovascular proliferation (FVP).
Methods
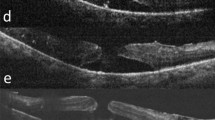
Eyes with PDR and FVP that had intraoperatively created FTMHs were retrospectively collected as the study group, and age- and sex-matched subjects with PDR and FVP who did not have intraoperative FTMHs were selected as the control group. Fundus abnormalities, optical coherence tomography (OCT) features, and anatomical and functional outcomes were compared between the two groups.
Results
Eleven eyes of 11 patients (5 male and 6 female) were identified as the study group. Follow-up duration was 36.8 ± 47.2 months. FTMHs were managed by ILM peeling or the inverted ILM flap technique. Anatomical success and MH closure were achieved in 100% of eyes in the study group. In comparison to the control group, the study group had a higher proportion of condensed prefoveal tissue (63.6% vs. 22.7%, p = 0.028), and a higher ratio of silicone oil tamponade (63.6% vs. 18.2%, p = 0.014), whereas there were no differences in preoperative and final BCVA, and the severity, activity, and locations of FVP between the two groups.
Conclusion
Condensed prefoveal tissue was a risk factor of FTMHs created during operation for eyes with PDR and FVP. The ILM peeling or the inverted ILM flap technique may be beneficial for the treatment with favorable anatomical and functional outcomes.




Similar content being viewed by others
Data availability
Data will be available under reasonable request to the corresponding author.
References
Garcia-Arumi J, Corcostegui B, Cavero L, Sararols L (1997) The role of vitreoretinal surgery in the treatment of posttraumatic macular hole. Retina 17(5):372–377
Ho AC, Guyer DR, Fine SL (1998) Macular hole. Surv Ophthalmol 42(5):393–416
Kwok AK, Cheng LL, Gopal L, Sharma T, Lam DS (2000) Endolaser around macular hole in the management of associated retinal detachment in highly myopic eyes. Retina 20(5):439–444
Lai C-T, Yang C-M (2015) Development of macular holes in diabetic retinopathy with fibrovascular proliferation: report of four cases. Taiwan J Ophthalmol 5(2):85–89. https://doi.org/10.1016/j.tjo.2015.03.002
Tsui MC, Hsieh YT, Lai TT, Lai CT, Lin HC, Ho TC et al (2021) Full-thickness macular hole formation in proliferative diabetic retinopathy. Sci Rep 11(1):23839
Kase S, Saito W, Ohgami K, Yoshida K, Furudate N, Saito A et al (2007) Expression of erythropoietin receptor in human epiretinal membrane of proliferative diabetic retinopathy. Br J Ophthalmol 91(10):1376–1378
Abu El-Asrar AM, Missotten L, Geboes K (2010) Expression of advanced glycation end products and related molecules in diabetic fibrovascular epiretinal membranes. Clin Exp Ophthalmol 38(1):57–64
Abu El-Asrar AM, Struyf S, Opdenakker G, Van Damme J, Geboes K (2010) Expression of stem cell factor/c-kit signaling pathway components in diabetic fibrovascular epiretinal membranes. Mol Vis 15(16):1098–1107
Iannetti L, Accorinti M, Malagola R, Bozzoni-Pantaleoni F, Da Dalt S, Nicoletti F et al (2011) Role of the intravitreal growth factors in the pathogenesis of idiopathic epiretinal membrane. Invest Ophthalmol Vis Sci 52(8):5786–5789
Shukla D, Dhoble P, Jager RD, Aiello LP, Ramasamy K (2006) Closure of macular hole following vitrectomy for diabetic tractional macular detachment. Eye (Lond) 20(12):1386–1388
Mason JO, Somaiya MD, White MF, Vail RS (2008) Macular holes associated with diabetic tractional retinal detachments. Ophthalmic Surg Lasers Imag Retina 39(4):288–293. https://doi.org/10.3928/15428877-20080701-12
Yeh PT, Cheng CK, Chen MS, Yang CH, Yang CM (2009) Macular hole in proliferative diabetic retinopathy with fibrovascular proliferation. Retina 29(3):355–361
Chen SN, Yang CM (2018) Internal limiting membrane flaps for coexistent macular hole and retinal detachment in eyes with proliferative diabetic retinopathy. J Ophthalmol 2018:3470731
Karimov M, Akhundova L, Aliyeva T (2020) Pars plana vitrectomy for full-thickness macular holes in patients with proliferative diabetic retinopathy and active fibrovascular proliferation. Clin Ophthalmol 14:4125–4133
Babu N, Kohli P, Mishra C, Rajan RP, Kumar K, Ramasamy K et al (2021) Surgical outcome of full-thickness macular hole secondary to tractional retinal detachment in proliferative diabetic retinopathy. Indian J Ophthalmol 69(11):3302–3307
Kumar V, Surve A, Mondal S, Azad SV (2021) Macular hole formation following panretinal photocoagulation in proliferative diabetic retinopathy. BMJ Case Rep 14(2):e240730. https://doi.org/10.1136/bcr-2020-240730
Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E et al (2013) The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 120(12):2611–2619
Tsui M-C, Hsieh Y-T, Yang C-M (2020) Silicone oil removal after extended tamponade in proliferative diabetic retinopathy—a long range of follow-up. Eye 34(12):2307–2314. https://doi.org/10.1038/s41433-020-0815-2
Su CC, Yang CH, Yeh PT, Yang CM (2014) Macular tractional retinoschisis in proliferative diabetic retinopathy: clinical characteristics and surgical outcome. Ophthalmologica 231(1):23–30
Tsui MC, Yang CM (2021) Early and late macular changes after the inverted internal limiting membrane flap technique for a full-thickness macular hole. Retina 41(1):20–28
Henrich PB, Haritoglou C, Meyer P, Ferreira PR, Schotzau A, Katamay R et al (2010) Anatomical and functional outcome in brilliant blue G assisted chromovitrectomy. Acta Ophthalmol 88(5):588–593
Henrich PB, Priglinger SG, Haritoglou C, Josifova T, Ferreira PR, Strauss RW et al (2011) Quantification of contrast recognizability during brilliant blue G- and indocyanine green-assisted chromovitrectomy. Invest Ophthalmol Vis Sci 52(7):4345–4349
Sjaarda RN, Glaser BM, Thompson JT, Murphy RP, Hanham A (1995) Distribution of iatrogenic retinal breaks in macular hole surgery. Ophthalmology 102(9):1387–1392
Al-Harthi E, Abboud EB, Al-Dhibi H, Dhindsa H (2005) Incidence of sclerotomy-related retinal breaks. Retina 25(3):281–284
Ramkissoon YD, Aslam SA, Shah SP, Wong SC, Sullivan PM (2010) Risk of iatrogenic peripheral retinal breaks in 20-G pars plana vitrectomy. Ophthalmology 117(9):1825–1830
Dogramaci M, Lee EJ, Williamson TH (2012) The incidence and the risk factors for iatrogenic retinal breaks during pars plana vitrectomy. Eye (Lond) 26(5):718–722
Figueroa MS, Ruiz-Moreno JM, Gonzalez F, del Valle A, Govetto C, de la Vega R, Plascencia N, Contreras I, Medina JL (2015) Long-term outcomes OF 23-gauge pars plana vitrectomy with internal limiting membrane peeling and gas tamponade for myopic traction maculopathy: a prospective study. Retina 35(9):1836–1843. https://doi.org/10.1097/IAE.0000000000000554
Parolini B, Palmieri M, Finzi A, Besozzi G, Frisina R (2021) Myopic traction maculopathy: a new perspective on classification and management. Asia Pac J Ophthalmol (Phila) 10(1):49–59
Sawaguchi S, Maruko I, Mikami Y, Hasegawa T, Koizumi H, Iida T (2017) Macular hole formation identified with intraoperative oct during vitrectomy for vitreomacular traction syndrome. Retin Cases Brief Rep Fall 11(4):380–382
Stewart MW, Browning DJ, Landers MB (2018) Current management of diabetic tractional retinal detachments. Indian J Ophthalmol 66(12):1751–1762
Michalewska Z, Nawrocki J (2021) Fovea morphology after vitrectomy in eyes with full-thickness macular hole coexisting with diabetic retinopathy. J Vitreoretin Dis 5(1):53–59
Imai M, Iijima H, Gotoh T, Tsukahara S (1999) Optical coherence tomography of successfully repaired idiopathic macular holes. Am J Ophthalmol 128(5):621–627
Michalewska Z, Michalewski J, Cisiecki S, Adelman R, Nawrocki J (2008) Correlation between foveal structure and visual outcome following macular hole surgery: a spectral optical coherence tomography study. Graefes Arch Clin Exp Ophthalmol 246(6):823–830
Antonetti DA, Barber AJ, Bronson SK, Freeman WM, Gardner TW, Jefferson LS et al (2006) Diabetic retinopathy: seeing beyond glucose-induced microvascular disease. Diabetes 55(9):2401–2411
King GL, Brownlee M (1996) The cellular and molecular mechanisms of diabetic complications. Endocrinol Metab Clin North Am 25(2):255–270
Barber AJ (2003) A new view of diabetic retinopathy: a neurodegenerative disease of the eye. Prog Neuropsychopharmacol Biol Psychiatr 27(2):283–290
Wilson DJ, Green WR (1987) Histopathologic study of the effect of retinal detachment surgery on 49 eyes obtained post mortem. Am J Ophthalmol 103(2):167–179
Lecleire-Collet A, Muraine M, Menard JF, Brasseur G (2006) Evaluation of macular changes before and after successful retinal detachment surgery using stratus-optical coherence tomography. Am J Ophthalmol 142(1):176–179
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was approved by the Research Ethics Committee of National Taiwan University Hospital and was conducted in accordance with the Declaration of Helsinki.
Consent to participation
Consent to participate was exempted by the Research Ethics Committee of National Taiwan University Hospital since this is a retrospective study.
Consent for publications
Consent to publish was exempted because no recognizable photo or information was used in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tsui, MC., Yang, CM. & Wang, LC. Characteristics and outcomes of full-thickness macular holes created during vitrectomy for proliferative diabetic retinopathy. Int Ophthalmol 43, 3479–3490 (2023). https://doi.org/10.1007/s10792-023-02753-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02753-8