Abstract
Purpose
Single center study to evaluate the incidence and long-term outcome of laser pointer maculopathy (LPM).
Methods
Medical records of 909,150 patients visiting our institution between 2007 and 2020 were screened in our electronic patient record system using the keywords "laserpointer," "laser pointer," and "solar."
Results
Eight patients (6/2 male/female, 11 eyes) with a history of LPM were identified by fundoscopy and optical coherence tomography (OCT), all of whom were children (6/2 male/female). Mean age at injury was 12.1 years (range 6–16). Five children (62.5%) were injured between 2019 and 2020, three (37.5%) between 2007 and 2018. Median best-corrected visual acuity (BCVA) of affected eyes at first presentation was 20/25 (range 20/50–20/16). Follow-up examination was performed in seven children (10 eyes) with a median follow-up period of 18 months (range 0.5–96). BCVA improved in 4 children (5 eyes; BCVA at follow-up 20/22.5, range 20/40–20/16). Three of these four children were treated with oral steroids. OCT revealed acute signs such as intraretinal fluid to resolve quickly, while outer retinal disruption persisted until the last follow-up in eight of eleven eyes. These lesions resembled lesions of patients with solar retinopathy of which seven cases (11 eyes) were identified between 2007 and 2020.
Conclusion
Readily available consumer laser pointers can damage the retina and the underlying retinal pigment epithelium, possibly leading to long-lasting visual impairments. The number of laser pointer injuries has increased over the last years. Therefore, access to laser pointers for children should be strictly controlled.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laser pointers play an increasingly important role as tools and toys in the modern world. However, the risks of handling laser pointers are often underestimated. In particular, vulnerable groups such as children are at risk of irreversible injury to themselves and others through irresponsible use of mostly imported and incorrectly labeled laser pointers [1, 2]. While all ocular compartments can be damaged by lasers, [3] the retina represents a predilection site due to the focusing of light onto the macula as well as the fixation behavior [4].
The risk and extent of the injury to the retina depend on the power and wavelength of the laser. Lasers are classified according to their accessible emission limits (AEL) by the IEC (International Electrotechnical Commission) 60,825 standard. Exposure to class III and IV lasers (> 1 mW) is known to have potentially detrimental effects on the eye [4, 5]. Thus, lasers are regulated in the USA by the American National Standard Institute[6] and in the European Union by the European Commission Decision of February 5, 2014, [7] allowing only the sale of up to class IIIR lasers (< 5 mW) in the USA and up to class 2 lasers (< 1 mW) in Europe [8, 9].
However, ownership and use of higher-power laser pointers are not restricted, and higher-power laser pointers are readily available on the Internet [2].
Accordingly, it is not surprising that cases of laser pointer maculopathy (LPM) have been reported with increasing frequency in recent years [10,11,12]. Therefore, the purpose of this study is to investigate the number of such cases in the recent past and the respective short- and long-term clinical consequences of laser pointer injuries. Thus, we aim to raise awareness for this sight-threatening condition and provide data to facilitate market regulations by national legislators.
Methods
Study design
In this retrospective, monocentric, observational study, we identified patients with unintended retinal laser injury, seen in the University Eye Center Freiburg, from the medical records of a total of 909,150 patients who were referred between 2007 and 2020. The keywords "laser pointer," "laserpointer" and "solar retinopathy" were used for screening in our electronic patient record system.
Examinations
The clinical investigations performed were part of routine clinical care. Visual acuity, pupil dilation, color fundus photography (FF 450 Plus Fundus Camera, Zeiss), and spectral domain OCT (Spectralis OCT, Heidelberg Engineering) were performed in all children. Case notes including case history, fundus photography and optical coherence tomography were reviewed.
Ethics
The study has been approved by the Central Ethics Commission in Freiburg (#21–1610) on November 4th, 2021. We comply with the Declaration of Helsinki, local laws and ICH-GCP.
Data presentation and statistical analysis
A probability (P) value of < 0.05 was considered statistically significant. For the descriptive data analysis, median values and minimal and maximal values were calculated. Visual acuity is given as decimal. For comparison of BCVA improvements between children treated with oral steroids (Prednisolone 1 mg/kg body weight) and children not treated with oral steroids, we performed a two-way ANOVA test with the factors therapy (steroids or no steroids) and time of presentation (first and last presentation).
Results
Number of laser pointer cases from 2007 to 2020
Twelve patients with suspected laser pointer-induced retinal injuries were identified (Fig. 1, dashed line). Organic damage was confirmed in eight of these patients (11 eyes, Fig. 1, solid line). Five of these eight patients (62.5%) sustained injury in 2019/2020, while only three patients (37.5%) suffered injury between 2007 and 2018.
Temporal distribution of laser pointer maculopathy cases in the eye center of the university Freiburg, Germany, from 2007 to 2020. Temporal distribution of cases with suspected laser injury from laser pointers (dashed line, triangles) and cases with confirmed laser injury from laser pointers (solid line, circles)
Spectrum of cases with laser pointed-induced maculopathy
Detailed information of every case is presented in Table 1. Three patients were affected bilaterally, five only unilaterally. All eight patients with confirmed laser pointer-induced maculopathy (LPM) were children (6/2 male/female). The mean age at the time of injury was 12.1 years (range 6–16 years).
In half of the cases, the retinal injuries occurred during school excursions, in the other half while playing with siblings or friends. The laser pointers emitted either red or green light. The eyes were exposed to direct laser light for 3–20 s at a distance of a few centimeters to one meter. One laser pointer could be obtained for laser power measurements (patient no. 7). This laser pointer emitted red light and had a maximum power of around 5.8 mW as measured with a laser power meter (measured with full batteries and in the immediate vicinity of the sensor; Thorlabs S130 VC), which would place the laser pointer in laser class IIIB (see Online Resource 1).
Functional damage
Out of the eight injured children, four suffered from blurred vision and three children complained of a central scotoma in the affected eye(s). One child reported no visual deterioration. Median best-corrected visual acuity (BCVA) of affected eyes at first presentation was 20/25 (range 20/25–20/16). Follow-up examination was performed in seven children (10 injured eyes) with a median follow-up period of 18 months (range 0.5–96 months). BCVA improved in five of these eyes (median BCVA at follow-up examination 20/22.5, range 20/40–20/16). Overall, six of seven children (7 of 10 eyes) describing functional problems at initial examination described clinical residuals at follow-up that were qualitatively similar to the original symptoms but mostly milder.
Influence of oral steroids on functional outcome
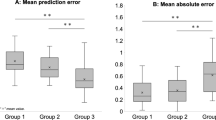
Half of the children received oral steroid therapy (Prednisolone 1 mg/kg body weight)–either for five days (three children) or tapering off over 6 weeks (one child). Visual acuity improved slightly in four of five affected eyes of children being treated with oral steroids (median BCVA at initial presentation 20/32, range 20/50–20/20; median BCVA at follow-up 20/25, range 20/40–20/20) compared with one in five affected eyes of children not treated with oral steroids (median BCVA at initial presentation 20/20, range 20/40–20/16; median BCVA at follow-up 20/20, range 20/40–20/16). BCVA improvements between first and last presentation were not significantly different between groups (two-way ANOVA: no statistically significant interaction between the effects of therapy (steroids or no steroids) and time of presentation (first and last presentation), p = 0.37).
Structural damage at initial examination
Slit lamp microscopy did not reveal damage to the anterior segment of the eye in any of the cases. Figure 2 shows macular OCT images and fundus photography of the macula at the initial examination of the eight patients with confirmed LPM. Fundoscopy revealed multifocal, partially confluent, yellowish-gray spots in the macula of the affected eyes. The lesions had varying phenotypes: Some were round in shape and rather small in diameter (case eye, 1 OD, 3 OD, 4 OS, 5 OD), some were likewise round but larger in diameter (7 OS, 8 OD), and others were organized as streaks (6 OD, 6 OS) or in a dendritic configuration (4 OD).
Macular OCT images of affected eyes also displayed heterogeneous lesion phenotypes ranging from hyperreflective streaks in the outer retinal layers (1 OD, 3 OD, 3 OS, 6 OD, 6 OS), disruptions of the outer retina (all affected eyes), intraretinal and subretinal fluid (1 OD, 6 OD, 6 OS,8 OD). All affected eyes showed loss of the ellipsoid zone.
Time course of the structural damage
Figure 3 shows the time course of retinal damage and the development of BCVA. In three of eight children (4 of 11 eyes, cases 4, 5 and 7), the initial presentation in our clinic took place more than 6 months after the causative injury, so that the acute course could not be assessed in these children. In the remaining children, the initial presentation was less than a week after the incident. Patient No. 8 did not show up for follow-up examinations.
In the first days after the causative event, sub- and intraretinal fluid was observed in a few cases with extensive damage (case 1 OD, 6 OD, 6 OS, 8 OD). We also saw irregularities of the outer retina with (case 3 OD) or without (case 2 OS) hyperreflective linear streaks. Sub- and intraretinal fluid resolved within days (case 1 OD) whereas outer retinal irregularities such as pigment epithelium clumping (case 1 OD, 4 OD) and especially ellipsoid zone disruption persisted longer (all injured eyes with follow-up), in some cases even for years (case 2 OS, 4 OD, 4 OS, 5 OD, 6 OD, 6 OS). In fundoscopy, lesions did not show marked changes at follow-up compared with initial presentation (data not shown).
Comparison of laser pointer maculopathy with solar retinopathy
We also identified seven patients (11 eyes) with confirmed solar retinopathy (SR) in the same timeframe (2007–2020). Five patients were male, and two were female. The median age at the time of injury was 32.5 years (range 18–49 years). Four patients were affected bilaterally and three unilaterally. The symptoms of these patients resembled those of patients with LPM: Four complained of a central scotoma and three of blurry vision in the respective eyes. Fundoscopic lesions were unifocal, sometimes ring-shaped and yellowish (data not shown).
We compared the macular OCT phenotypes of solar retinopathy lesions with lesions found in patients with LPM shown before. Online Resource 2 shows macular OCT images of affected eyes at the first and last presentation with the respective BCVAs at each examination. Similar to cases of LPM, we could identify distinct lesion phenotypes depending on the time that had passed after the acute incident. Macular OCTs that were acquired only few days after the causative incident showed hyperreflective linear streaks in the outer retina (case 1 OD, case 4 OU). As in patients with LPM, these hyperreflective streaks fully resolved but disruptions of the outer retina, especially the ellipsoid zone, could persist (cases 1 and 2).
Discussion
We demonstrate that the number of cases of laser pointer-induced retinal injury has increased in southwestern Germany from 2007 to 2020. Our data also illustrate that the OCT phenotype of laser pointer-induced retinal lesions varies depending on the time passed since injury. In addition, we show that in macular OCT, these lesions strongly resemble lesions found in patients with solar retinopathy.
Concerning time course of the number of patients with LPM, five of eight children were injured in 2019/2020 compared to only three between 2007 and 2018 suggesting an increase in the recent past. On the other hand, the number of cases of SR cases was stable over the same time period (data not shown). In accordance with our data, increasing incidence of LPM has been reported lately [10]–12. The underlying causes remain elusive, but could be attributable to the nonrestrictive legislation regarding the possession and use of higher-power laser pointers in the EU and the US, as well as the easy availability of such devices via the Internet [2].
Patient history may be difficult to obtain since children often do not directly report laser pointer use. Therefore, it is important to look for early retinal signs, which may indicate the past use of a laser pointer. Regarding laser pointer-induced structural retinal damage, our data illustrate that its temporal course is subject to dynamic changes, especially in the first weeks after retinal injury: Acute signs of laser pointer-induced damage in macular OCT include sub- and intraretinal fluid and hyperreflective linear streaks. While these acute signs resolve within days, irregularities or disruptions of the outer retina can persist for long periods of time. Of note, even years after laser pointer-induced retinal damage, we saw disruptions of the ellipsoid zone.
While the spontaneous course is generally positive if the Bruch membrane stays intact and while secondary choroidal neovascularization occurs only in very rare cases [13, 14], the ongoing complaints of patients and the persisting changes in macular OCT even years after the causative incident suggest that some damage may indeed be irreversible [5, 15, 16].
Therapeutic options are limited. Corticosteroids have been proposed for the treatment of laser-induced retinal damage and are used in clinical practice, although their benefit is debatable. Both preclinical and clinical data are partially contradictory and difficult to interpret due to the positive natural course of disease [1, 17, 18]. Our data do not indicate a beneficial effect of oral steroids on the functional outcome in patients with LPM. However, our sample size is small, and therefore, we cannot make any conclusive statement about the effect of oral steroids on the functional outcome after retinal laser pointer injury. Since most, if not all causally related incidents are avoidable, the focus should therefore be to better prevent such laser pointer-induced retinal injuries.
It is known that fixation of the sun can lead to similar injuries [19, 20]. Pathophysiologically, higher power lasers induce photothermal retinal damage within microseconds to seconds, while longer retinal exposure to sunlight leads to photochemical damage [4]. We hence asked whether these pathophysiological differences translate into morphological differences in macular OCT. Patients with LPM and SR shared phenotypic features both in the acute phase and in follow-up examinations. De Silva and colleagues demonstrated that near-infrared reflectance autofluorescence imaging may facilitate discriminating between these disease entities [19]. Other discriminators between these disease entities have been proposed: On the one hand, the age of patients at initial presentation and on the other hand the (multi-)focality of lesions [19, 20]. This is in accordance with our data. While LPM mainly affected children (range in our study: 6–16 years), SR affected patients of all ages (range in our study: 18–49 years). In patients with SR, lesions were unifocal while laser pointers induced multifocal lesions.
Our study has a number of limitations. Of note, the sample size was low due to the monocentric design of the study. Multicentric approaches and meta-analyses/reviews are needed to confirm the notion of increasing incidence of LPM. It has recently been shown that LPM leads to changes in OCT angiography [21] and near-infrared reflectance autofluorescence [19]. Small scotomata often being reported by patients with LPM can be detected by microperimetry. However, due to retrospective nature of the study, these methods were not used in our study. In addition, fundus and macular OCT images were not recorded in a standardized manner. Regarding the temporal course of structural damage in macular OCT, three of eight children did not present to the clinic until 6 months after laser pointer injury. Therefore, the acute course could not be assessed in these children. Also, one child did not appear for follow-up examinations.
In conclusion, our study indicates an increase in cases of LPM in children in recent years. Since LPM is characterized by retinal changes and corresponding symptoms that can persist for years, prevention—especially in vulnerable populations such as children—is of great importance. We therefore recommend that access to laser pointers for children needs to be strictly controlled.
References
Neffendorf JE, Hildebrand GD, Downes SM (2019) Handheld laser devices and laser-induced retinopathy (LIR) in children: an overview of the literature. Eye 33(8):1203–1214. https://doi.org/10.1038/s41433-019-0395-1
Hadler J, Tobares E, Dowell M (2013) Random testing reveals excessive power in commercial laser pointers. J Laser Appl 25(3):032007. https://doi.org/10.2351/1.4798455
Spelsberg H, Hering P, Reinhard T, Sundmacher R (2000) Bilateral scleral thermal injury: complication after skin laser resurfacing. Arch Ophthalmol 116:1686–1687
Barkana Y, Belkin M (2000) Laser eye injuries. Surv Ophthalmol 44(6):459–478. https://doi.org/10.1016/S0039-6257(00)00112-0
Birtel J, Hildebrand GD, Issa PC (2020) Laser pointer: a possible risk for the retina. Klin Monbl Augenheilkd 237(10):1187–1192. https://doi.org/10.1055/a-1250-8471
American National Standards Institute (2014) ANSI Z136.1 (2014)–Safe Use of Lasers. USA
Official Journal of the European Union (2014) Commission decision of 5 February 2014 on the safety requirements to be met by European standards for consumer laser products pursuant to directive 2001/95/EC of the European Parliament and of the Council on general product sa. European Union. pp. 20–21
International Electrotechnical Commission (2014) IEC60825–1 2014. In: Safety of laser products: part 1—equipment classification and requirements. Geneva
Bundesanstalt für Arbeitsschutz und Arbeitsmedizin (2013) Technische spezifikation zu lasern als bzw. in verbraucherprodukte(n). Germany
Torp-Pedersen T et al (2018) Laser pointer maculopathy—on the rise? Acta Ophthalmol 96(7):749–754. https://doi.org/10.1111/aos.13856
Bhavsar KV, Michel Z, Greenwald M, Cunningham ET, Freund KB (2021) Retinal injury from handheld lasers: a review. Surv Ophthalmol 66(2):231–260. https://doi.org/10.1016/j.survophthal.2020.06.006
Marshall J, O’Hagan JB, Tyrer JR (2016) Eye hazards of laser ‘pointers’ in perspective. Br J Ophthalmol 100(5):583–584. https://doi.org/10.1136/bjophthalmol-2016-308798
Chen X, Dajani OAW, Alibhai AY, Duker JS, Baumal CR (2021) Long-Term Visual Recovery in Bilateral Handheld Laser Pointer-Induced Maculopathy. Retin Cases Brief Rep 15(5):536–539. https://doi.org/10.1097/ICB.0000000000000845
Tran K, Wang D, Scharf J, Sadda S, Sarraf D (2020) Inner choroidal ischaemia and CNV due to handheld laser-induced maculopathy: a case report and review. Eye (Lond) 34(11):1958–1965. https://doi.org/10.1038/s41433-020-0830-3
Lee GD, Baumal CR, Lally D, Pitcher JD, Vander J, Duker JS (2014) Retinal injury after inadvertent handheld laser exposure. Retina 34(12):2388–2396. https://doi.org/10.1097/IAE.0000000000000397
Hossein M, Bonyadi J, Soheilian R, Soheilian M, Peyman GA (2011) SD-OCT features of laser pointer maculopathy before and after systemic corticosteroid therapy. Ophthal Surg Lasers Imaging Retin. https://doi.org/10.3928/15428877-20111208-03
Brown J, Hacker H, Schuschereba ST, Zwick H, Lund DJ, Stuck BE (2007) Steroidal and nonsteroidal antiinflammatory medications can improve photoreceptor survival after laser retinal photocoagulation. Ophthalmology 114(10):1876–1883. https://doi.org/10.1016/j.ophtha.2007.04.035
Schuschereba ST et al (1999) High-dose methylprednisolone treatment of laser-induced retinal injury exacerbates acute inflammation and long-term scarring. Ophthal Technol 3591:430. https://doi.org/10.1117/12.350605
De Silva SR et al (2019) Improved diagnosis of retinal laser injuries using near-infrared autofluorescence. Am J Ophthalmol 208:87–93. https://doi.org/10.1016/j.ajo.2019.06.001
Ortiz Salvador M, Montero Hernández J, Castro Navarro V (2020) Multimodal imaging in laser pointer maculopathy. Arch Soc Esp Oftalmol 95(6):e44. https://doi.org/10.1016/j.oftal.2019.12.015
Tomasso L et al (2017) Optical coherence tomography angiography findings in laser maculopathy. Eur J Ophthalmol 27(1):e13–e15. https://doi.org/10.5301/ejo.5000844
Acknowledgements
We like to thank the “Dr. Gabriele Lederle-Stiftung” for their financial support.
Funding
Open Access funding enabled and organized by Projekt DEAL. The study was financially supported by a Scholarship of Dr. Navid Farassat from the “Dr. Gabriele Lederle-Stiftung.” The sponsor or funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. MR and NF have designed the work and have made substantial contribution to the acquisition, analysis and interpretation of data, as well as conception and design of the manuscript. DB has made substantial contributions to acquisition and interpretation of data. JL has made contributions to the conception of the work and interpretation of the data. TN, HA and TR made contributions to interpretation of data and have been involved in reviewing the manuscript. WL has made substantial contributions to acquisition of data and interpretation of data as well as reviewing of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Competing interest
The authors have no competing interest to disclose.
Ethical approval
The study has been approved by the Central Ethics Commission in Freiburg (21–1610) on November 4th, 2021. We comply with the Declaration of Helsinki, local laws and ICH-GCP.
Consent to participate and consent to publish
The Central Ethics Commission in Freiburg has waived the requirement for individual informed consent to the retrospective scientific analysis of treatment data and publication. Only anonymized data were analyzed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Farassat, N., Boehringer, D., Luebke, J. et al. Incidence and long-term outcome of laser pointer maculopathy in children. Int Ophthalmol 43, 2397–2405 (2023). https://doi.org/10.1007/s10792-023-02638-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02638-w