Abstract
Purpose
Within a population-based follow-up study, to examine the 10-year incidence of pseudoexfoliation syndrome (PEX), possible risk factors for PEX and its association with ocular aging of the cornea, lens and retina.
Methods
The baseline examination was conducted in 2006 on a random sample of 1,033 adult participants from Kaunas city (Lithuania) population of whom 631 had ophthalmic examination data at attendance of the 10-year follow-up in 2016. Detailed examination of the anterior and posterior segment of the eye was carried out. After diagnostic mydriasis PEX was diagnosed by the presence of typical grayish-white exfoliation material on the anterior capsule surface of the lens. The participants were divided to PEX and non-PEX groups.
Results
PEX prevalence increased from 9.8 to 34.2% from baseline to 10-year follow-up. Nuclear cataract was common both in the PEX group (66.7%) and in those without PEX (72.2%), but this difference did not reach statistically significantly increased risk of developing cataract in those with PEX (OR 1.2; p = 0.61). Central corneal thickness (CCT) was thinner in the PEX group (529 ± 34 μm) and in the oldest group (525 ± 36 μm) (p < 0.001). Compared to baseline, corneal curvature (CC) became flatter in both groups (7.6 ± 0.27 vs 7.7 ± 0.26 mm; p < 0.001) during the follow-up, but the difference did not reach significance between groups. Corneal astigmatism was most commonly with-the-rule in both groups (37 (50.0%) vs 148 (68.5%); p > 0.05). Age, sex and PEX had no influence on age-related macular degeneration distribution.
Conclusion
The prevalence of PEX increased significantly with age in our population, with those with PEX having thinner and flatter corneae, but no difference in cataract and age-related macular degeneration characteristics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pseudoexfoliation syndrome (PEX) is an age-related disorder in which greyish-white flakes accumulate in the anterior segment of the eye. PEX pathogenesis is not completely understood [1]. PEX fibrils appear to be produced by various unrelated endothelial, epithelial, mesenchymal cell types, including lens epithelial cells, trabecular meshwork cells, ciliary epithelial cells, smooth muscle cells and fibroblasts [2] indicating that PEX might be a part of a generalized ageing disorder [3].
Approximately 0.2–30.0% of the global population older than 60 years of age is affected by PEX [4, 5]. The highest PEX prevalence rates, as high as 40.6% in those aged 80 years or over [6], have been reported in Nordic countries [6, 7]. Clinically unilateral ocular involvement varies from 48.0 to 76.0% of patients. Progression to bilateral PEX was described in up to 50.0–71.0% of patients within 5–12 years after diagnosis [8, 9].
A possible correlation has been established between PEX and steeper corneal curvature (CC), central corneal thickness (CCT) and nuclear lens opacifications [10, 11], but not with age-related maculopathy [10].
There is no clearly established gender predilection [12] with conflicting data between Kiliç’s finding for a significant relationship between PEX and advancing age and male sex [13], while the 12-year follow-up of Reykjavik Eye Study, Iceland, found an association with older age and female sex [9]. We are yet to find any follow-up studies that examine PEX and its associations with ophthalmological changes in Baltic countries. In 2006, a population-based epidemiological study that was part of larger Health, Alcohol and Psychosocial Factors In Eastern Europe (HAPIEE) [14] study was conducted in the Hospital of Lithuanian University of Health Sciences. HAPPIE examined the potential associations of ophthalmological and cardiovascular diseases. After 10 years (2016), those willing and able to come back for a follow-up was re-examined.
The aim of this paper was to determine associations of PEX with ocular changes in Lithuanian urban population and identify possible risk factors of PEX 10 years after the baseline study.
Materials and methods
Study sample/study population
During 2006–2008, 7087 subjects from Kaunas city (Lithuania) participated in international Health, Alcohol and Psychosocial Factors in Eastern Europe (HAPIEE) study. In 2006, out of the 7087 invited, 1065 individuals participated in the ophthalmological sub-study [14]. In 2016–2017, 686 subjects were invited and examined in a 10-year follow-up study. The study was approved by the Regional Bioethics Committee and was carried out in accordance with the Declaration of Helsinki. During the study, informed consent was obtained from each participant.
At HAPPIE baseline visit in 2006, ophthalmological examination was carried out on 1,033 participants. Ten years later, 686 returned for a follow-up examination (response rate of 66.4%; 239 males (37.9%) and 392 females (62.1%)). Altogether, 347 individuals did not return due to death (n = 164) and migration/refusal (n = 183).
Of the 686 examined, 55 respondents were not included in the current data analysis as their PEX status could not be determined due to trauma/phthisis, pseudophakia or aphakia in both eyes and lens subluxation, resulting in a cohort of 631 to be included in this study.
Weight and height were measured with a calibrated medical scale and without shoes or heavy clothes. Body mass index (BMI) was calculated as the weight in kilograms divided by the height in meters squared (kg/m2). Normal weight was defined as BMI < 25.0 kg/m2, overweight as BMI ≥ 25.0–29.99 kg/m2 and obesity as BMI ≥ 30.0 kg/m2 [15].
Study instrument
All participants underwent ophthalmological examination according to a standard examination protocol and same methodology as at baseline [16,17,18]. The examination was carried out by two trained and certified ophthalmologists who had no access to the subjects’ medical history.
PEX was diagnosed by slit-lamp examination after diagnostic mydriasis with 1 drop of 1% cyclopentolate. PEX was confirmed as definite by the presence of typical grayish-white exfoliation material on the anterior capsule surface of the lens (complete or partial peripheral band and⁄ or a central shield). Other changes associated with PEX such as grayish-white deposits elsewhere in the anterior chamber (iris, cornea), precapsular frosting or haze, supported the diagnosis of PEX. PEX was deemed suspect/possible if precapsular frosting or haze was seen. The participants were classified as having PEX if any typical pseudoexfoliation material was present in at least one eye. For statistical analysis, we used data of the respondents with definite PEX diagnosis as the PEX group. Persons with suspected PEX were grouped together with those without any signs of the PEX.
All study respondents answered a standard questionnaire regarding lifestyle, subjective health and ophthalmological pathology (supplement 1).
Ophthalmological examination
For the 10-year follow-up study, 1262 eyes of 631 individuals' ophthalmic examination results were included. Lens opacification was evaluated at slit lamp by LOCS III international classification: NO/NC—nuclear opalescence/color (evaluation 0.1 to 6.9), C—cortical, P—posterior subcapsular (evaluation 0.1–5.9) [19]. Cataract was evaluated in 1262 eyes.
After diagnostic mydriasis as above, fundus photographs centered on the fovea were taken using Canon CF-60Uvi (Canon Medical Systems, USA). Retinal images were graded by trained and certified ophthalmic graders at Moorfields Eye Hospital Reading Centre in London, UK, primarily based on the International Classification for age-related macular degeneration (AMD). The grading of photographs was carried out by the same graders for both baseline and follow-up studies data [20, 21]. Altogether, 1262 eyes had retina images graded; of these, 45 (3.6%) in baseline and 65 (5.2%) in follow-up had ungradable images due to cataract.
Central corneal pachymetry was measured with pachymeter (ALCON OCUSCAN RxP, Alcon Laboratories inc., USA), in auto mode, averaging 10 readings. In the 10-year follow-up, CCT was measured in 1260 eyes, with only 2 eyes' measurement missing. In the baseline study, eyes were selected randomly for this examination and so only 304 eyes were available for comparison.
Keratometry was taken using the Auto keratorefractometer (ACCUREF-K 9001, SHIN–NIPPON Commerce, inc., Japan). K1, K2, K1-axis, K2-axis and corneal curvature measurements were recorded from keratometry. Corneal astigmatism was calculated as follows: K1–K2 = corneal astigmatism (cylinder (diopters (D)). If the cylinder was < 1.0D, it was considered as no corneal astigmatism; if it was ≥ 1.0D, it was considered as corneal astigmatism. Corneal astigmatism was classified as with-the-rule (ax 90 ͦ ± 30 ͦ), against-the-rule (ax 0 ͦ ± 30 ͦ) and oblique (all the left). The corneal curvature (CC) results were documented from auto keratorefractometer. CC and astigmatism were recorded reliably in 1182 eyes; in 80 eyes dry eye prevented reliable measurements to be taken.
For cataract, AMD, CCT, CC, corneal astigmatism measurements each eye was kept in the analysis. For the incidence of PEX the same eye of the same subjects was evaluated.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics version 20 software. Descriptive statistics were applied for various data points in the PEX and non-PEX groups. Unilateral and bilateral PEX cases were separated into subgroups. Quantitative variables were presented as median, and interquartile range or mean and standard deviation (SD). Categorical data were presented as number (percent).
Data normality detection of continuous variables was checked using Kolmogorov–Smirnov test. In case of non-normality, medians and interquartile ranges (IQR) were calculated and Mann–Whitney U-test was used to compare continuous data between groups. Chi-square (χ2) test or Fisher exact 2-sided test was used to compare categorical variables. For ordinal data χ2 linear-by-linear association test was used for confirmation of the linear trend. The comparison of proportions between groups was performed using z test. McNemar's χ2 test was used to assess the difference between paired proportions. Quantitative variables were compared with Wilcoxon test.
Binary logistic regression analyses were conducted with PEX as predictor controlling for age and gender. Odds ratios (OR) and 95% confidence intervals (CI) of OR were calculated for the risk of new PEX cases and the dependence of risk factors.
Results
Altogether, 631 participants had full examination (392 (62.1%) male and 239 (37.9%) female). Baseline and follow-up characteristics are presented in Tables 1 and 2. The prevalence of PEX in the baseline cohort (2006–2008) was 9.8% (Table 2) [16].
During 10 years of follow-up (2016–2017) PEX prevalence increased to 34.2% (216 subject, (85 (39.4%) male and 131 (60.6%) female) (Table 1). There was no statistically significant difference of PEX frequency between males and females, 35.6 and 33.4%, respectively (p > 0.05). Mean age was significantly higher in the PEX group compared to the non-PEX group (73.01 ± 7.97 years vs 68.70 ± 8.16 years, p = 0.001).
The subjects’ distribution by sex and PEX occurrence is shown in Table 1.
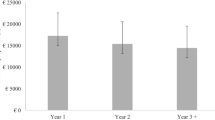
PEX affected males and females in all age groups equally, while there was an increasing trend for the 10-year age-brackets: 23.3% of participants aged 55–65 years, 32.1% of those aged 66–75 years, and 47.3% of those aged 76–83 years were affected by PEX, this trend was statistically significant (p < 0.001) (Table 3). Comparing age group 55–65 and 66–75, 55–65 and 76–83, 66–75 and 76–83, significance was reached (p < 0.05; Table 3).
Those with PEX were statistically older in the follow-up study, age median in the PEX group was higher than that in the non-PEX group (74 vs 68 years respectively; p < 0.001; Table 3), and in the baseline study age medians in the PEX and non-PEX groups were 68 years versus 59 years (p < 0.001).
At baseline, there were 37 unilateral and 25 bilateral PEX cases, increasing to 86 unilateral (13.6%) and 130 bilateral (20.6%) cases in the 10-year follow-up (Tables 1 and 2). Of those with unilateral PEX at baseline, 20 became bilateral and nineteen (48.7%) remained unilateral during the 10-year follow-up (p < 0.001). A total of 154 (71.3%) new PEX cases were diagnosed at the 10-year follow-up (Table 2).
PEX risk factors of lifestyle are presented in Table 4. There was no statistically significant difference between those affected by PEX and those who were not PEX-subjects, in univariate logistic regression analysis.
Age, gender, alcohol consumption, BMI, education and marital status did not increase the probability of having PEX.
In multivariate logistic regressions only age increased the risk of having PEX significantly (p < 0.001). Secondary education, in comparison with primary education showed a tendency for higher risk of having PEX in men (p = 0.08), but did not reach statistical significance.
Adjusting by multivariate risk factors, alcohol consumption 1–4 time/month and alcohol consumption > 1 time/week, marital status—married, former and current smoking, and normal weight reduced the probability of developing PEX in men, but not significantly.
Similarly, secondary and university education, normal weight and overweight reduced the probability of having PEX in women, but not significantly.
Cataract
Of the available 1262 eyes, some degree of lens opacities was diagnosed in 1116 (95.1%) eyes and no cataract—in 58 (4.9%) eyes. Prevalence of cataract was significantly higher in the oldest age group, there was a 43.4% (95% CI 5.939–316.572, p < 0.001) increase in those in the oldest compared to the youngest groups. Comparing the youngest and middle age group, the risk to have cataract significantly increased 3.4 times (95% CI 1.833–6.330; p < 0.001). Cataract was diagnosed more frequently in females (63.3%) than in males (36.7%) (p = 0.01). There were statistically significantly more cataract diagnosed in the non-PEX group when compared to the study subjects with PEX (73.4 vs 26.6%, p > 0.05). Nuclear cataract was the most common type (70.7%) with no statistically significant difference between PEX/non-PEX groups. Mixed cataract was found frequently both in the non-PEX and the PEX groups (27.4 vs 28.9%; p > 0.05) (Table 5). We noticed a tendency in the PEX group to have a bigger risk of developing cataract by 21% (95% CI 0.576–2.574, p = 0.61); however, this trend was not statistically significant.
Age-related macular degeneration
Of the available 1197 eyes with comparable fundus imaging, any AMD was diagnosed in 937 (78.3%) eyes and no AMD in 260 (21.7%), respectively (Table 6). In the 10-year follow-up study, there were 383 new any AMD cases. There was no statistically significant difference in the prevalence of AMD between females and males (598 (63.8%) and 339 (36.2%), respectively, p = 0.18). The age-groups we had showed no statistically significant difference in the presence of any AMD nor was any association between PEX and AMD distribution (Table 6).
Central corneal thickness
CCT was measured in 1262 eyes of 631 patients. In the follow-up study, CCT was significantly thinner in the PEX group than in those without (529 ± 34 μm vs 532 ± 33 μm, respectively, p < 0.001). CCT became significantly thinner with age (p < 0.001), as it was 537 ± 30 μm in 55–65 years age group, 533 ± 33 μm in those aged 66–75 years, and 525 ± 36 μm in the over 75 s (p < 0.001). The thinnest central cornea was in the oldest age group both in the PEX and non-PEX groups (521 ± 33 μm; p < 0.001 vs 527 ± 37 μm; p = 0.006, respectively). Pearson correlation between age and CCT was weak but significant (r = −0,159; p < 0.001). There was no statistically significant difference between the PEX and non-PEX groups with respect to gender and CCT.
Over the 10 years of follow-up, CCT became statistically significantly thinner compared to baseline (baseline 539 ± 36 μm vs follow-up 531 ± 33 μm, p < 0.001. This also proved to be true in the non-PEX group (in baseline 539 ± 35 μm vs in follow-up 530 ± 31 μm, p = 0.002, respectively), but we were not able to confirm statistical significance in the PEX group (in baseline 539 ± 39 μm vs in follow-up 532 ± 36 μm, p = 0.280).
Corneal curvature
Of the 1182 eyes with corneal curvature (CC) measured, the mean CC was 7.7 ± 0.26 mm (in baseline mean CC 7.6 ± 0.27 mm). CC radius in males was statistically significantly higher than in females (7.8 vs 7.6 mm; p < 0.001). At follow-up, there was a tendency for CC to decrease with age, but not significantly (p > 0.05). At the 10-year follow-up, the cornea became statistically significantly flatter compared to baseline (7.6 ± 0.27 vs 7.7 ± 0.26 mm; p < 0.001), but there was no statistically significant difference between the PEX and non-PEX groups (PEX 7.64 ± 0.24 vs 7.68 ± 0.26, non-PEX 7.66 ± 0.28 vs 7.70 ± 0.27 mm; p = 0.123).
Corneal astigmatism
Of the 1182 eyes with relevant measurements, 290 cases of corneal astigmatism were found. Females had more corneal astigmatism (62.8 vs 37.2%, p = 0.02). In the study population, corneal astigmatism was mostly with-the-rule, and this tendency was evident in both PEX and non-PEX groups other than in the oldest group where against-the-rule corneal astigmatism was statistically significantly more common (p < 0.001). In the baseline study, this group displayed the same trend, but it was then not statistically significant.
Discussion
PEX typically affects the anterior segment of the eye and its worldwide prevalence is estimated to be 0.2–30.0% of people older than 60 years of age[5, 6, 12, 22,23,24,25,26]. Consistent evidence of PEX incidence and prevalence is lacking [3] and previous studies differed based on geographical, ethnic and racial features, as well as in age and gender distributions and diagnostic methods, making comparison difficult.
In Lithuania, PEX prevalence was found to be 47.3% in 76–83-year-old age group, which is slightly higher than a population with similar characteristics in Iceland (40.6% of those who are 80 years old) [6]. PEX prevalence increased with age in all studies [9, 12, 13, 23, 26,27,28,29] and this is in agreement with our finding, as in our study PEX subjects were older than those without it (72.2 ± 8.1 years vs 68.6 ± 8.2 years, respectively). Similarly to our results, in Turkey the highest PEX rate was in the 80 years old patients (18.4%) with an increased odds ratio of 45.78 (p < 0.01) when compared to the 40–49 age-group [23].
A previous Lithuanian study [17] found that PEX risk increased by 13.5% with each additional year of life (95% CI 1.1–1.17; p < 0.001), while a Swedish study established the annual PEX incidence as 1.8% (95% CI 1.3–2.4) [7]. The Reykjavik Eye Study found that on average there was a 5% increase in the risk of developing definite PEX for every decade of life in people older than 50 years of age (OR = 1.05; 95% CI 1.01–1.09, p = 0.022) [10].
Incidence data have been provided by a few population based studies such as the Reykjavik Eye Study (5- and 12-year follow-up) [9, 30], the study by Aström et al. [7] in Skelleftea, Northern Sweden (21-year follow-up), Chennai Eye Disease Incidence Study with 6-year follow-up [31]. In the Thessaloniki study the 12-year incidence of PEX was 19.6% (95% CI, 17.1-22.2) [32], similar to ours.
Lithuania is situated on the eastern shore of the Baltic Sea in Northern Europe. In our study, PEX prevalence in Lithuania was found to be 34.2%, higher than previously noted in the neighboring Nordic countries (Sweden—23%, Finland—22%, Iceland—10,7%) [6, 7, 33]. In the 76–83-year-old age group, Lithuanian subjects had similar prevalence to that of other Scandinavian countries: 47.3% in our study that is only slightly higher than in Iceland (40.6% of those who are 80 years old) [6].
In other Baltic states, Estonia recorded 35.4% prevalence in 2004 [11] and 25.5% in 2010 [34], while Latvia reported lower prevalence of 21.6% [35]. Our estimates compare well to similar background of the other Baltic states.
The age-related PEX progression from unilateral to bilateral disease is well established [9]. In our study 53.0% of unilateral PEX progressed to bilateral PEX in 10-year period, this is very similar to the progression rate seen both in Iceland and Sweden [7, 9].
In contrast to some other studies we did not find significant gender differences in our cohort, although there are studies that strengthen our observations as well [26, 36, 37]. Clearly, larger and well characterized samples with detailed ophthalmic examination are required to enable better understanding of this issue.
Not many studies have been able to analyze lifestyle and other factors. In a Saudi Arabian study no significant relation was found between education level, occupation and lifestyle of the patients and the prevalence of PEX [37]. While our study showed some trends in lifestyle and demographic characteristics, none were significant, this is in agreement with the findings of the Thessaloniki Eye Study [32]. It might be worthwhile though pursuing these further if a suitably large cohort is established.
Reykjavik Eye Study had additional data analyzed for PEX risk factors older age, female sex, increased iris pigmentation, moderate use of alcohol, and asthma were all associated with higher PEX prevalence, whereas the consumption of vegetables and fruit was associated with lower PEX prevalence [38]. Five years later, analyzing the same risk factors, significant associations were found only with age and the consumption of fruit [38], but by 12 years there were no statistically significant associations [9, 10, 32]. Being married was shown to be a protective factor for definite PEX in a univariate analysis, but after stratification by the effect of age, the association disappeared [9, 30].
Chennai Eye Disease Incidence Study showed a significant relationship between older age, illiteracy, rural residence, pseudophakia and nuclear cataract and the 6-year incidence of PEX [32, 39]. In our study secondary education for men showed a tendency higher risk of having PEX. Controlling for risk factors (former and current smoking, and normal weight) in a multivariate logistic regression showed the tendency to reduce the probability of having the PEX.
Radius of CC was found to be age-independent and significantly steeper in females than in males [40] and our findings agreed with these. In our study the cornea became flatter during the 10-year follow-up (7.6 vs 7.7 mm; p<0.001). And Hepsen et al. reported significantly steeper corneal curvature in PEX eyes compared to those without PEX [41] but we were unable to confirm this in our study [42].
In Reykjavik Eye Study CCT was found to be independent of age and gender [40]: While our findings regarding gender were the same, we did notice that CCT became significantly thinner with aging (p<0.001). Some studies claimed that in PEX, CCT values were significantly lower than those in non-PEX eyes [43, 44] and our findings are in agreement with these. However, Krysik, for instance, found CCT to be thicker in the PEX group [45]. Many other authors reported that there was no significant difference in CCT between the PEX and non-PEX groups [10, 41, 42, 46,47,48]. Again, a large enough cohort might provide an answer to these conflicting data.
Lens opacification occurs in a high proportion of PEX eyes, resulting in cataract surgeries [34] most commonly nuclear [49]. Nuclear sclerosis was predominant in PEX eyes, compared to those without PEX (57.6 and 36.9%, respectively) [11], confirmed by Blue Mountains Eye Study [50]. In contrast, while we found a large number of nuclear cataract both in the PEX and non-PEX groups, we could not confirm significant difference in our population. In contrast, Gunes found that mixed cataract was the most common cataract type in the PEX patients in Turkey [51]. In a 30-year follow-up study Ekström et al. found that PEX was the second most important predictor for cataract surgery after lens opacities, accounting for a 2.38-fold increased risk with man having a lower risk for cataract formation [52].
In a Greek study the presence of AMD was strongly related to PEX (x2 = 13.675, p = 0.003; Mantel-Haenszel test=13.66, p = 0.002) [53], while in a Turkish population, the prevalence of AMD was found to be significantly higher in the PEX group than in the non-PEX (17.9 vs 9.5%, p = 0.03) [51], but in our study we could not confirm these findings.
Strength and limitations
The main strength of this study is its population-based prospective study design. Detailed ophthalmological examinations were carried out by trained and certified operators using a strict protocol.
The main limitation includes response rate of 66.4%, limiting the generalizability of the study. Cataract surgery had already been performed on 8.02% of those returning for 10-year follow-up, unfortunately there was no information on their PEX status and this might have impacted on our incidence rate [54].
Conclusion
PEX prevalence in this Lithuanian cohort of well characterized patients increased from 9.8 to 34.2% with no significant difference between sexes, but with significant increase with age. Our results showed that detailed characterization of the PEX and non-PEX eyes was beneficial in identifying trends in anterior segment changes. Conversely, there was no significant relationship with any AMD findings for these patients. An appropriate clinical pathway is required to enable timely diagnosis and treatment of these patients in order to keep them active in society.
Data availability
The data used to support the findings of this study are available from the corresponding author upon request. PEX associations with cardiovascular diseases were discussed in our earlier article [54] (PMID: 31956932; https://doi.org/10.1007/s10792-019-01262-x; https://www.ncbi.nlm.nih.gov/pubmed/?term=rumelaitiene).
References
Schlötzer-Schrehardt U, Naumann GOH (2006) Ocular and systemic pseudoexfoliation syndrome. Am J Ophthalmol 141(5):921–937. https://doi.org/10.1016/j.ajo.2006.01.047
Zenkel M, Schlötzer-Schrehardt U (2014) The composition of exfoliation material and the cells involved in its production. J Glaucoma 23(8):S12–S14. https://doi.org/10.1097/IJG.0000000000000123
Tarkkanen A (2008) Is exfoliation syndrome a sign of systemic vascular disease? Acta Ophthalmol 86(8):832–836. https://doi.org/10.1111/j.1755-3768.2008.01464.x
Ritch R, Schlötzer-Schrehardt U (2001) Exfoliation (pseudoexfoliation) syndrome: toward a new understanding. Proceedings of the First International Think Tank. Acta Ophthalmol Scand 79(2):213–217.
Wang W, He M, Zhou M, Zhang X (2014) Ocular pseudoexfoliation syndrome and vascular disease: a systematic review and meta-analysis. PLoS ONE 9(3):1–7. https://doi.org/10.1371/journal.pone.0092767
Arnarsson A, Damji KF, Sverrisson T et al (2007) Pseudoexfoliation in the Reykjavik Eye Study: prevalence and related ophthalmological variables. Acta Ophthalmol Scand 85(8):822–827. https://doi.org/10.1111/j.1600-0420.2007.01051.x
Åström S, Stenlund H, Lindén C (2007) Incidence and prevalence of pseudoexfoliations and open-angle glaucoma in northern Sweden: II. Results after 21 years of follow-up. Acta Ophthal Scand 85 (8):832–837. https://doi.org/10.1111/j.1600-0420.2007.00980.x.
Hammer T, Schlötzer-Schrehardt U, Naumann GOH (2001) Unilateral or asymmetric pseudoexfoliation syndrome? Arch Ophthalmol 119(7):1023–1031. https://doi.org/10.1001/archopht.119.7.1023
Arnarsson A, Sasaki H, Jonasson F (2013) Twelve-year incidence of exfoliation syndrome in the Reykjavik Eye Study. Acta Ophthalmol 91:157–162. https://doi.org/10.1111/j.1755-3768.2011.02334.x
Arnarsson ÁM (2009) Epidemiology of exfoliation syndrome in the Reykjavik eye study. Acta Ophthalmol 87(THESIS3):1–17. https://doi.org/10.1111/j.1755-3768.2009.01806.x
Kaljurand K, Puska P (2004) Exfoliation syndrome in Estonian patients scheduled for cataract surgery. Acta Ophthalmol Scand 82(3 Pt 1):259–263. https://doi.org/10.1111/j.1600-0420.2004.00256.x
Forsius H, Forsman E, Fellman J, Eriksson AW (2002) Exfoliation syndrome: frequency, gender distribution and association with climatically induced alterations of the cornea and conjunctiva. Acta Ophthalmol Scand 80(5):478–484
Kiliç R, Karagöz N, Çetin AB et al (2016) The prevalence of exfoliation syndrome in Turkey. Acta Ophthalmol 94(2):e105–e108. https://doi.org/10.1111/aos.12885
Peasey A, Bobak M, Kubinova R et al (2006) Determinants of cardiovascular disease and other non-communicable diseases in Central and Eastern Europe: rationale and design of the HAPIEE study. BMC Public Health 6:1–10. https://doi.org/10.1186/1471-2458-6-255
Tamosiunas A, Luksiene D, Baceviciene M et al (2014) Health factors and risk of all-cause, cardiovascular, and coronary heart disease mortality: findings from the MONICA and HAPIEE Studies in Lithuania. https://doi.org/10.1371/journal.pone.0114283
Špečkauskas M, Tamošiūnas A, Jašinskas V (2012) Association of ocular pseudoexfoliation syndrome with ischaemic heart disease, arterial hypertension and diabetes mellitus. Acta Ophthalmol 90(6):e470–e475. https://doi.org/10.1111/j.1755-3768.2012.02439.x
Špečkauskas M, Barzdžiukas V, Jašinskas V (2011) Pseudoeksfoliacinio sindromo sindromo paplitimas ir jo sąsajos su glaukoma ir akių hipertenzija Lietuvos suaugusiųjų populiacijoje. Medicina 15(7):499–503
Špečkauskas M (2012) Pseudoeksfoliacinio sindromo paplitimas ir jo pasireiškimo ypatumai, esant akių bei širdies ir kraujagyslių sistemos pokyčiams. Doctoral Dissertation.
Davison JA, Chylack LT (2003) Clinical application of the Lens Opacities Classification System III in the performance of phacoemulsification. J Cataract Refract Surg 29:138–145. https://doi.org/10.1016/S0886-3350(02)01839-4
Lengyel I, Csutak A, Florea D et al (2015) A population-based ultra-widefield digital image grading study for age-related macular degeneration-like lesions at the peripheral retina. Ophthalmology 122:1340–1347. https://doi.org/10.1016/j.ophtha.2015.03.005
Bird AC, Bressler NM, Bressler SB et al (1995) An international classification and grading system for age-related maculopathy and age-related macular degeneration. Surv Ophthalmol 39(5):367–374. https://doi.org/10.1016/S0039-6257(05)80092-X
Ringvold A (1999) Epidemiology of the pseudoexfoliation syndrome: a review. Acta Ophthalmol Scandinavica 77(4):371–375
Yildirim N, Yasar E, Gursoy H, Colak E (2017) Prevalence of pseudoexfoliation syndrome and its association with ocular and systemic diseases in Eskisehir, Turkey. Int J Ophthalmol 10(1):128–134. https://doi.org/10.18240/ijo.2017.01.21.
Mitchell P, Wang JJ, Hourihan F (1999) The relationship between glaucoma and pseudoexfoliation: the Blue Mountains Eye Study. Arch Ophthalmol (Chicago, Ill : 1960) 117 (10):1319–1324.
Vijaya L, Asokan R, Panday M et al (2016) The prevalence of pseudoexfoliation and the long-term changes in eyes with pseudoexfoliation in a South Indian population. Journal of Glaucoma Glaucoma 25:e596–e602. https://doi.org/10.1097/IJG.0000000000000276
Teshome T, Regassa K (2004) Prevalance of pseudoexfoliation syndrome in Ethiopian patients scheduled for cataract surgery. Acta Ophthalmol Scand 82(3I):254–258. https://doi.org/10.1111/j.1395-3907.2004.00263.x.
Anastasopoulos E, Topouzis F, Wilson MR et al (2011) Characteristics of pseudoexfoliation in the Thessaloniki Eye Study. J Glaucoma 20(3):160–166. https://doi.org/10.1097/IJG.0b013e3181d9d8bd
French D, Margo C, Harman L (2012) Ocular pseudoexfoliation and cardiovascular disease: a national cross-section comparison study. N Am J Med Sci 4(10):468–473. https://doi.org/10.4103/1947-2714.101987
Asfuroglu Y, Kemer OE (2019) Central corneal thickness and corneal volume changes in eyes with and without pseudoexfoliation after uneventful phacoemulsification. Int Ophthalmol 39(2):275–280. https://doi.org/10.1007/s10792-017-0804-z
Arnarsson A, Damji KF, Sasaki H et al (2009) Pseudoexfoliation in the Reykjavik Eye Study: five-year incidence and changes in related ophthalmologic variables. AJOPHT 148:291–297. https://doi.org/10.1016/j.ajo.2009.03.021
Gayathri R, Coral K, Sharmila F et al (2016) Correlation of aqueous humor lysyl oxidase activity with TGF-ß levels and LOXL1 genotype in pseudoexfoliation. Glaucoma and Lens 41(10): 1331–1338. https://doi.org/10.3109/02713683.2015.1125505.
Topouzis F, Founti P, Yu F et al (2019) Twelve-year incidence and baseline risk factors for pseudoexfoliation: the Thessaloniki eye study (An American Ophthalmological Society Thesis). Am J Ophthalmol 206:192–214. https://doi.org/10.1016/j.ajo.2019.05.005
Hirvelä H, Luukinen H, Laatikainen L (1995) Prevalence and risk factors of lens opacities in the elderly in Finland. A population-based study. Ophthalmology 102(1):108–117
Kaljurand K, Teesalu P (2010) Prevalence of exfoliation syndrome in Estonia. Eur J Ophthalmol 20(6):1012–1017. https://doi.org/10.1177/112067211002000622
Elksnis Ē, Oberbrinkmann JP (2020) Prevalence of pseudoexfoliation syndrome in cataract patients in Latvia. Rīga Stradiņš Univ
Brajković J, Kalauz-Surać I, Ercegović A et al (2007) Ocular pseudoexfoliation syndrome and internal systemic diseases. Acta Clin Croat 46(46):57–61
Al-Saleh SA, Al-Dabbagh NM, Al-Shamrani SM et al (2015) Prevalence of ocular pseudoexfoliation syndrome and associated complications in Riyadh, Saudi Arabia. Saudi Med J 36(1):108–112. https://doi.org/10.15537/smj.2015.1.9121.
Arnarsson A, Jonasson F, Damji KF et al (2010) Exfoliation syndrome in the Reykjavik Eye Study: risk factors for baseline prevalence and 5-year incidence. Br J Ophthalmol 94(7):831–835. https://doi.org/10.1136/bjo.2009.157636
Vijaya L, Asokan R, Panday M et al (2015) Six-year incidence and baseline risk factors for pseudoexfoliation in a South Indian Population: The Chennai Eye disease incidence study. Ophthalmology 122(6):1158–1164. https://doi.org/10.1016/J.OPHTHA.2015.02.007
Eysteinsson T, Jonasson F, Sasaki H et al (2002) Central corneal thickness, radius of the corneal curvature and intraocular pressure in normal subjects using non-contact techniques: Reykjavik Eye Study. Acta Ophthalmol Scand 80(1):11–15. https://doi.org/10.1034/j.1600-0420.2002.800103.x
Hepsen IF, Yağci R, Keskin U (2007) Corneal curvature and central corneal thickness in eyes with pseudoexfoliation syndrome. Can J Ophthalmol 42(5):677–680. https://doi.org/10.3129/i07-145
Arnarsson A, Damji KF, Jonasson F (2008) Corneal curvature and central corneal thickness in a population-based sample of eyes with pseudoexfoliation syndrome-Reykjavik Eye Study. Can J Ophthalmol 43(4):484–485. https://doi.org/10.3129/i08-064
Tomaszewski BT, Zalewska R, Mariak Z (2014) Evaluation of the endothelial cell density and the central corneal thickness in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. J Ophthalmol. https://doi.org/10.1155/2014/123683
Özcura F, Aydin S, Dayanir V (2011) Central corneal thickness and corneal curvature in pseudoexfoliation syndrome with and without glaucoma. J Glaucoma 20(7):410–413. https://doi.org/10.1097/IJG.0b013e3181f7afb8
Krysik K, Dobrowolski D, Polanowska K et al (2017) Measurements of corneal thickness in eyes with pseudoexfoliation syndrome: comparative study of different image processing protocols. Journal of Healthcare Engineering 2017:1–6. https://doi.org/10.1155/2017/4315238
Aksoy NÖ, Çakır B, Doğan E, Alagöz G (2018) Evaluation of anterior segment parameters in pseudoexfoliative glaucoma, primary angle-closure glaucoma, and healthy eyes. Turk J Ophthalmol 48:227–231. https://doi.org/10.4274/tjo.03271
Doganay S, Tasar A, Cankaya C et al (2012) Evaluation of Pentacam-Scheimpflug imaging of anterior segment parameters in patients with pseudoexfoliation syndrome and pseudoexfoliative glaucoma. Clin Exp Optom 95(2):218–222. https://doi.org/10.1111/j.1444-0938.2011.00691.x
Omura T, Tanito M, Doi R et al (2014) Correlations among various ocular parameters in clinically unilateral pseudoexfoliation syndrome. Acta Ophthalmol 92(5):e412–e413. https://doi.org/10.1111/aos.12348
Conway RM, Schlötzer-Schrehardt U, Küchle M, Naumann GOH (2004) Pseudoexfoliation syndrome: pathological manifestations of relevance to intraocular surgery. Clin Experiment Ophthalmol 32(2):199–210. https://doi.org/10.1111/j.1442-9071.2004.00806.x
Kanthan GL, Mitchell P, Burlutsky G et al (2013). Pseudoexfoliation syndrome and the long-term incidence of cataract and cataract surgery: The Blue Mountains Eye Study. Am J Ophthalmol. https://doi.org/10.1016/j.ajo.2012.07.002
Gunes A, Yasar C, Tok L, Tok O (2017) Prevalence of pseudoexfoliation syndrome in Turkish patients with senile cataract. Seminars Ophthalmol 32(3):297–301. https://doi.org/10.3109/08820538.2015.1068344
Ekström C, Botling Taube A (2015) Pseudoexfoliation and cataract surgery: a population-based 30-year follow-up study. Acta Ophthalmol 93(8):774–777. https://doi.org/10.1111/aos.12789
Kozobolis VP, Detorakis ET, Tsilimbaris MK et al. (1999) Correlation between age-related macular degeneration and pseudoexfoliation syndrome in the population of Crete (Greece). Arch Ophthalmol (Chicago, Ill : 1960) 117 (5): 664–669. https://doi.org/10.1001/ARCHOPHT.117.5.664.
Rumelaitienė U, Žaliūnienė D, Špečkauskas M et al (2020) Link of ocular pseudoexfoliation syndrome and vascular system changes: results from 10-year follow-up study. Int Ophthalmol. https://doi.org/10.1007/s10792-019-01262-x
Acknowledgements
The authors thank Kristina Jurėnienė, Eglė Šepetauskienė, Emilija Jusevičiūtė, Vaidas Vainauskas for their valuable help and input for the statistical analysis and for their comments on the article.
Funding
The HAPIEE study was funded by grants from the Wellcome Trust (Grant No. 064947⁄Z⁄01⁄Z), the US National Institute on Aging (Grant No. IR0I AG23522-01) and the MacArthur Foundation (Health and Social Upheaval network). Follow-up study was funded by the grant (No. SEN-15028) from the Research Council of Lithuania, the National Program of Sciences “Healthy Aging”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Ethical approval
The study was approved by the Regional Bioethics committee and was carried out in accordance with the Declaration of Helsinki.
Informed consent
Informed consent and consent form for case reports were obtained from all individual participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rumelaitiene, U., Speckauskas, M., Tamosiunas, A. et al. Exploring association between pseudoexfoliation syndrome and ocular aging. Int Ophthalmol 43, 847–857 (2023). https://doi.org/10.1007/s10792-022-02486-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02486-0