Abstract
Purpose
To investigate corneal sub-basal nerve morphology changes in primary Sjogren’s syndrome (SS) dry eye (SSDE) patients and determine the association with disease severity at microstructural level.
Methods
Twenty-eight eyes of 17 SSDE and 82 eyes of 47 age- and sex-matched non-SS dry eye (NSSDE) patients were included. The Ocular Surface Disease Index questionnaire (OSDI), Schirmer’s test (ST), tear meniscus height (TMH), non-invasive breakup time (NIBUT), meibomian gland (MG) morphology, and ocular staining score (OSS) were assessed. In vivo confocal microscopy was performed to observe corneal sub-basal nerve morphology (length, reflectivity, width, and tortuosity). Associations between clinical features and nerve parameters were analysed.
Results
SSDE patients more frequently had increased nerve reflectivity (151.12 ± 17.07 vs. 139.37 ± 14.31 grey value), width (4.45 ± 0.87 vs. 3.92 ± 0.81 μm), tortuosity (132.90 ± 8.04 vs. 129.50 ± 7.33 degree), and higher reflectivity, width, and total nerve grades than NSSDE individuals (all P < 0.05). Significant associations were found between nerve reflectivity/width and anti-SSA [OR = 1.139 (1.013–1.281)/1.802 (1.013–4.465)]/labial gland biopsy [OR = 1.046 (1.002–1.161)/1.616 (1.020–3.243)]. Higher nerve width was associated with increased OSDI [β = 0.284 (0.187–0.455)], MG score [β = 0.185 (0.109–0.300)] and OSS [β = 0.163 (0.020–0.345)], but decreased NIBUT [β = − 0.247 (− 0.548 ~ − 0.154)]. Higher nerve total grade was associated with increased OSDI [β = 0.418 (0.157–0.793)] and OSS [β = 0.287 (0.027–0.547)], but decreased ST [β = − 0.410 (−0.857 ~ − 0.138)].
Conclusions
Corneal nerve morphology changes associated with clinical features in SS patients. These changes may facilitate severity evaluation and management of the disease.


Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Mariette X, Criswell LA (2018) Primary Sjögren’s syndrome. N Engl J Med 378:931–939
Shiboski CH, Shiboski SC, Seror R et al (2017) 2016 American college of Rheumatology/European league against rheumatism classification criteria for primary Sjögren’s syndrome: a consensus and data-driven methodology involving 3 international patient cohorts. Ann Rheum Dis 76:9–16
Bjordal O, Norheim KB, Rødahl E, Jonsson R, Omdal R (2020) Primary Sjögren’s syndrome and the eye. Surv Ophthalmol 65:119–132
Margaretten M (2017) Neurologic manifestations of primary Sjögren syndrome. Rheum Dis Clin North Am 43:519–529
Chen FY, Lee A, Ge S, Nathan S, Knox SM, McNamara NA (2017) Aire-deficient mice provide a model of corneal and lacrimal gland neuropathy in Sjögren’s syndrome. PLoS ONE. https://doi.org/10.1371/journal.pone.0184916
Seeliger T, Prenzler NK, Gingele S et al (2019) Neuro-Sjögren: peripheral neuropathy with limb weakness in Sjögren’s syndrome. Front Immunol. https://doi.org/10.3389/fimmu.2019.01600
Ye W, Chen S, Huang X et al (2018) Clinical features and risk factors of neurological involvement in Sjögren’s syndrome. BMC Neurosci. https://doi.org/10.1186/s12868-018-0427-y
Gemignani F, Ferrari G, Vitetta F, Giovanelli M, Macaluso C, Marbini A (2010) Non-length-dependent small fibre neuropathy Confocal microscopy study of the corneal innervation. J Neurol Neurosurg Psychiatry 81:731–733
Lanza M, Iaccarino S, Varricchi G, D’Errico T, Gironi Carnevale UA, Bifani M (2017) Corneal confocal microscopy alterations in Sjögren’s syndrome dry eye. Acta Ophthalmol 95(5):e366–e372. https://doi.org/10.1111/aos.13194
Giannaccare G, Pellegrini M, Sebastiani S, Moscardelli F, Versura P, Campos EC (2019) In vivo confocal microscopy morphometric analysis of corneal subbasal nerve plexus in dry eye disease using newly developed fully automated system. Graefes Arch Clin Exp Ophthalmol 257:583–589
Tuisku IS, Konttinen YT, Konttinen LM, Tervo TM (2008) Alterations in corneal sensitivity and nerve morphology in patients with primary Sjögren’s syndrome. Exp Eye Res 86:879–885
Winter K, Scheibe P, Guthoff RF, Allgeier S, Stachs O (2017) Morphometric characterization of the subbasal nerve plexus: detection and analysis of networks of nerve fibers. Ophthalmologe 114:608–616
Liu Y, Chou Y, Dong X et al (2019) Corneal subbasal nerve analysis using in vivo confocal microscopy in patients with dry eye: analysis and clinical correlations. Cornea 38:1253–1258
Craig JP, Nichols KK, Akpek EK et al (2017) TFOS DEWS II definition and classification report. Ocul Surf 15(3):276–283
Levy O, Labbé A, Borderie V et al (2017) Increased corneal sub-basal nerve density in patients with Sjögren syndrome treated with topical cyclosporine A. Clin Exp Ophthalmol 45(5):455–463
Semeraro F, Forbice E, Nascimbeni G et al (2016) Effect of autologous serum eye drops in patients with Sjögren syndrome-related dry eye: clinical and in vivo confocal microscopy evaluation of the ocular surface. In Vivo 30(6):931–938
Mahelková G, Burdová MC, Malá Š, Hoskovcová L, Dotrelová D, Štechová K (2018) Higher total insulin dose has positive effect on corneal nerve fibers in DM1 patients. Invest Ophthalmol Vis Sci 59(10):3800–3807
Wolffsohn JS, Arita R, Chalmers R et al (2017) TFOS DEWS II diagnostic methodology report. Ocul Surf 15:539–574
Arita R, Itoh K, Inoue K, Amano S (2008) Noncontact infrared meibography to document age-related changes of the meibomian glands in a normal population. Ophthalmology 115:911–915
Begley C, Caffery B, Chalmers R, Situ P, Simpson T, Nelson JD (2019) Review and analysis of grading scales for ocular surface staining. Ocul Surf 17(2):208–220
Theander E, Mandl T (2014) Primary Sjögren’s syndrome: diagnostic and prognostic value of salivary gland ultrasonography using a simplified scoring system. Arthritis Care Res 66:1102–1107
Ferdousi M, Kalteniece A, Petropoulos I et al (2020) Diabetic neuropathy is characterized by progressive corneal nerve fiber loss in the central and inferior Whorl regions. Invest Ophthalmol Vis Sci 61(3):48. https://doi.org/10.1167/iovs.61.3.48
Ferdousi M, Kalteniece A, Azmi S et al (2021) Diagnosis of neuropathy and risk factors for corneal nerve loss in type 1 and type 2 diabetes: a corneal confocal microscopy study. Diabetes Care 44(1):150–156
Ponirakis G, Petropoulos IN, Alam U et al (2019) Hypertension contributes to neuropathy in patients with type 1 diabetes. Am J Hypertens 32(8):796–803
Lee OL, Tepelus TC, Huang J et al (2018) Evaluation of the corneal epithelium in non-Sjögren’s and Sjögren’s dry eyes: an in vivo confocal microscopy study using HRT III RCM. BMC Ophthalmol 18(1):309. https://doi.org/10.1186/s12886-018-0971-3
Cardigos J, Barcelos F, Carvalho H et al (2019) Tear meniscus and corneal sub-basal nerve plexus assessment in primary Sjögren syndrome and sicca syndrome patients. Cornea 38:221–228
Stern ME, Beuerman RW, Fox RI, Gao J, Mircheff AK, Pflugfelder SC (1998) The pathology of dry eye: the interaction between the ocular surface and lacrimal glands. Cornea 17:584–589
Tepelus TC, Chiu GB, Huang J et al (2017) Correlation between corneal innervation and inflammation evaluated with confocal microscopy and symptomatology in patients with dry eye syndromes: a preliminary study. Graefes Arch Clin Exp Ophthalmol 255:1771–1778
Kheirkhah A, Satitpitakul V, Hamrah P, Dana R (2017) Patients with dry eye disease and low subbasal nerve density are at high risk for accelerated corneal endothelial cell loss. Cornea 36:196–201
Villani E, Galimberti D, Viola F, Mapelli C, Ratiglia R (2007) The cornea in Sjogren’s syndrome: an in vivo confocal study. Invest Ophthalmol Vis Sci 48:2017–2022
Bron AJ, de Paiva CS, Chauhan SK et al (2017) TFOS DEWS II pathophysiology report. Ocul Surf 15:438–510
Matsumoto Y, Ibrahim OMA, Kojima T, Dogru M, Shimazaki J, Tsubota K (2020) Corneal in vivo laser-scanning confocal microscopy findings in dry eye patients with Sjögren’s syndrome. Diagnostics (Basel) 10(7):497. https://doi.org/10.3390/diagnostics10070497
Bendella H, Rink S, Grosheva M, Sarikcioglu L, Gordon T, Angelov DN (2018) Putative roles of soluble trophic factors in facial nerve regeneration, target reinnervation, and recovery of vibrissal whisking. Exp Neurol 300:100–110
Tzioufas AG, Tsonis J, Moutsopoulos HM (2008) Neuroendocrine dysfunction in Sjogren’s syndrome. NeuroImmunoModulation 15:37–45
Fox RI, Stern M (2002) Sjögren’s syndrome: mechanisms of pathogenesis involve interaction of immune and neurosecretory systems. Scand J Rheumatol Suppl 116:3–13
Johnson EO, Kostandi M, Moutsopoulos HM (2006) Hypothalamic-pituitary-adrenal axis function in Sjögren’s syndrome: mechanisms of neuroendocrine and immune system homeostasis. Ann N Y Acad Sci 1088:41–51
Chrousos GP (1995) The hypothalamic-pituitary-adrenal axis and immune-mediated inflammation. N Engl J Med 332:1351–1362
Sternberg EM (2006) Neural regulation of innate immunity: a coordinated nonspecific host response to pathogens. Nat Rev Immunol 6:318–328
Funding
This work was supported by Capital's Funds for Health Improvement and Research (No.2018–2-4093). The sponsors or funding organizations had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
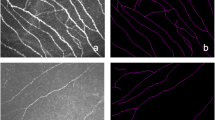
RH, YC and YD setup the protocol and recruited the participants. RH collected and analyzed the data, created the figures, and contributed to the writing. YZ and YD discussed the data and participated in writing manuscript. ZL, YW and XR provided statistical advice and oversaw the statistical analysis. XL setup the protocol oversaw and wrote the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Peking University Third Hospital (No. M2019236).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the images in Fig. 1.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hao, R., Chou, Y., Ding, Y. et al. Corneal subbasal nerve analysis in patients with primary Sjogren’s syndrome: a novel objective grading method and clinical correlations. Int Ophthalmol 43, 779–793 (2023). https://doi.org/10.1007/s10792-022-02478-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02478-0