Abstract
Purpose
To compare the diurnal IOP-lowering efficacy and safety of cyclocryocoagulation (CCC) and cyclophotocoagulation (CPC) in patients with refractory glaucoma.
Methods
Forty eyes of 40 Caucasian patients with advanced primary or secondary glaucoma with only tunnel vision left were included in this retrospective, comparative interventional case series. Twenty eyes treated with CCC were compared with 20 eyes treated with CPC. Primary endpoint was the reduction of 24 h mean diurnal intraocular pressure (IOP; mean of 6 measurements), peak IOP and diurnal IOP fluctuations 3 and 6 months post-treatment. Secondary outcomes were the occurrence of postoperative complications and the identification of factors influencing the postoperative IOP reduction.
Results
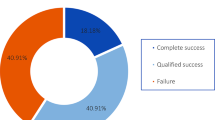
In the CCC group (mean age 70.6 ± 13.4 years), mean diurnal IOP was significantly reduced from 20.0 ± 4.5 mmHg to 14.7 ± 2.5 (p < 0.001) at 3 months and 13.9 ± 3.34 mmHg at 6-month follow-up (p < 0.001). In the CPC group (mean age 74.9 ± 9.0 years), mean diurnal IOP significantly decreased from 18.2 ± 3.1 mmHg to 13.2 ± 2.2 (p < 0.001) at 3 months and 13.1 ± 2.6 mmHg (p < 0.001) at 6 months. At 6 months, 75% of the CCC and 63% of the CPC group had mean diurnal IOP reductions of 20% or more. The most frequent complication (25%) was a transient IOP increase during the first days after CCC. A higher preoperative mean diurnal IOP was recognized as the only factor influencing the postoperative IOP reduction after CCC and CPC.
Conclusions
Both cyclodestructive methods seem to be reasonably safe and effective in lowering 24 h mean diurnal IOP in the perspective of 6 months in patients with refractory glaucoma. The IOP-lowering effect after CCC was better but not statistically significantly different compared to CPC. A higher rate of complications was observed in the CCC group, however.


Similar content being viewed by others
Availability of data and materials
All data relevant to the study are included in the article or uploaded as supplementary information.
References
Foster A, Resnikoff S (2005) The impact of Vision 2020 on global blindness. Eye (Lond) 19:1133–1135
Taylor HR, Keeffe JE (2001) World blindness: a 21st century perspective. Br J Ophthalmol 85:261–266
Boland MV, Ervin AM, Friedman DS et al (2013) Comparative effectiveness of treatments for open-angle glaucoma: a systematic review for the US Preventive Services Task Force. Ann Intern Med 158:271–279
Rodríguez-García A, González-González LA, Alvarez-Guzmán JC (2016) Trans-scleral diode laser cyclophotocoagulation for refractory glaucoma after high-risk penetrating keratoplasty. Int Ophthalmol 36:373–383
Bietti G (1950) Surgical intervention on the ciliary body. New trends for the relief of glaucoma. JAMA 142:889–897
Fankhauser F, Kwasniewska S, Van der Zypen E (2004) Cyclodestructive procedures. I. Clinical and morphological aspects: a review. Ophthalmologica 218:77–95
Weekers R, Lavergne G, Watillon M et al (1961) Effects of photocoagulation of ciliary body upon ocular tension. Am J Ophthalmol 52:156–163
Frezzotti P, Mittica V, Martone G et al (2010) Long-term follow-up of diode laser trans-scleral cyclophotocoagulation in the treatment of refractory glaucoma. Acta Ophthalmol 88:150–155
Leske MC, Heijl A, Hyman L et al (2007) Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology 114:1965–1972
Nicaeus T, Derse M, Schlote T et al (1999) Cyclocryocoagulation in treatment of therapy refractory glaucoma: a retrospective analysis of 185 cryocoagulation procedures. Klin Monbl Augenheilkd 214:224–230
Goldenberg-Cohen N, Bahar I, Ostashinski M et al (2005) Cyclocryotherapy versus transscleral diode laser cyclophotocoagulation for uncontrolled intraocular pressure. Ophthalmic Surg Lasers Imaging 36:272–279
Tzamalis A, Pham DT, Wirbelauer C (2011) Diode laser cyclophotocoagulation versus cyclocryotherapy in the treatment of refractory glaucoma. Eur J Ophthalmol 21:589–596
Gorsler I, Thieme H, Meltendorf C (2015) Cyclophotocoagulation and cyclocryocoagulation as primary surgical procedures for open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol 253:2273–2277
Ishida K (2013) Update on results and complications of cyclophotocoagulation. Curr Opin Ophthalmol 24:102–110
Liu GJ, Mizukawa A, Okisaka S (1994) Mechanism of intraocular pressure decrease after contact transscleral continuous-wave Nd:YAG laser cyclophotocoagulation. Ophthalmic Res 26:65–79
Suki B, Parameswaran H, Imsirovic J et al (2016) Regulatory roles of fluctuation-driven mechanotransduction in cell function. Physiology (Bethesda) 31:346–358
Ebneter A, Wagels B, Zinkernagel MS (2009) Non-invasive biometric assessment of ocular rigidity in glaucoma patients and controls. Eye (Lond) 23:606–611
Asrani S, Zeimer R, Wilensky J et al (2000) Large diurnal fluctuations in intraocular pressure are an independent risk factor in patients with glaucoma. J Glaucoma 9:134–142
Konstas AG, Topouzis F, Leliopoulou O et al (2006) 24-hour intraocular pressure control with maximum medical therapy compared with surgery in patients with advanced open-angle glaucoma. Ophthalmology 113:761–765
Nouri-Mahdavi K, Hoffman D, Coleman AL et al (2004) Predictive factors for glaucomatous visual field progression in the Advanced Glaucoma Intervention Study. Ophthalmology 111:1627–1635
Burgoyne CF, Downs JC, Bellezza AJ et al (2005) The optic nerve head as a biomechanical structure: a new paradigm for understanding the role of IOP-related stress and strain in the pathophysiology of glaucomatous optic nerve head damage. Prog Retin Eye Res 24:39–73
Downs JC, Roberts MD, Burgoyne CF (2008) Mechanical environment of the optic nerve head in glaucoma. Optom Vis Sci 85:425–435
The AGIS Investigators (2000) The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol 130:429–440
Brindley G, Shields MB (1986) Value and limitations of cyclocryotherapy. Graefes Arch Clin Exp Ophthalmol 224:545–548
Benson MT, Nelson ME (1990) Cyclocryotherapy: a review of cases over a ten- year period. Br J Ophthalmol 74:103–105
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by SW, RH, LEP and KRP. The first draft of the manuscript was written by SW, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
S. W. has no financial disclosures. R. H. has no financial disclosures. L. E. P. has received lecture fees from Allergan and Santen and is on the Advisory Board for Allergan, Santen and Aerie and received grant support from Novartis. K. R. P. has received lecture fees from Allergan and Novartis. None of the authors has any financial interest or any conflict of interest related to the subject matter.
Ethics approval
Ethical approval was waived by the local Ethics Committee of the Technical University of Dresden in view of the retrospective nature of the study, and all the procedures being performed were part of the routine care.
Human and animal participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Waibel, S., Herber, R., Pillunat, L.E. et al. Comparison of the diurnal efficacy and safety of cyclocryocoagulation and cyclophotocoagulation in patients with refractory glaucoma. Int Ophthalmol 40, 2191–2199 (2020). https://doi.org/10.1007/s10792-020-01402-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-020-01402-8