Abstract
Purpose
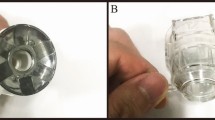
The aim of the study is to study the safety and efficacy of three cyclodestructive treatments; high-intensity focused ultrasound (HIFU) cyclocoagulation versus micropulse cyclophotocoagulation (MP-CPC) versus transscleral continuous-wave cyclophotocoagulation (CW-CPC) for treatment of non-refractory glaucoma.
Methods
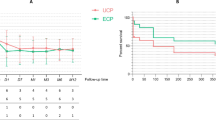
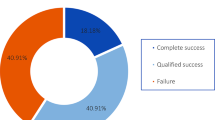
This is a prospective comparative single-center study. Thirty non-refractory, medically uncontrolled, primary open-angle glaucoma patients with good vision were randomized to a single session of HIFU, MP-CPC or CW-CPC. Intraocular pressure (IOP) reduction, number of medications, success rate, visual acuity and complications were compared between the three groups. Success was defined as an IOP reduction of 30% and IOP between 6 and 21 mmHg with or without medications, in the absence of vision-threatening complications.
Results
Thirty patients were enrolled in our study: 10 patients received HIFU, 10 patients received MP-CPC and 10 patients received CW-CPC. At 6 months, IOP was reduced by 31.5%, 23.9% and 19.4% (P = 0.4) achieving a success rate of 50%, 60% and 50% (P = 0.8) for continuous, micropulse and HFU groups, respectively, with reduction in the number of drops and stop of oral acetazolamide. Although the difference in the rate of complications between groups was not significant, CW-CPC group had more complications.
Conclusions
Cyclophotocoagulation could be an option in the treatment of non-refractory glaucoma even in patients with good visual acuity, with similar outcomes between the three types of cyclodestruction.





Similar content being viewed by others
Data availability
No data set associated with this submission.
References
Ansari E, Gandhewar J (2007) Long-term efficacy and visual acuity following transscleral diode laser photocoagulation in cases of refractory and non-refractory glaucoma. Eye 21(7):936–940
Bloom PA, Tsai JC, Sharma K et al (1997) “Cyclodiode”: trans-scleral diode laser cyclophotocoagulation in the treatment of advanced refractory glaucoma. Ophthalmology 104(9):1508–1520
Hauber FA, Scherer WJ (2002) Influence of total energy delivery on success rate after contact diode laser transscleral cyclophotocoagulation: a retrospective case review and meta-analysis. J Glaucoma 11(4):329–333
Egbert PR, Fiadoyor S, Budenz DL, Dadzie P, Byrd S (2001) Diode laser transscleral cyclophotocoagulation as a primary surgical treatment for primary open-angle glaucoma. Arch Ophthalmol 119(3):345–350
Benson MT, Nelson ME (1990) Cyclocryotherapy: a review of cases over a 10-year period. Br J Ophthalmol 74(2):103–105
Michelessi M, Bicket AK, Lindsley K (2018) Cyclodestructive procedures for non‐refractory glaucoma. Cochrane Database of Systematic Reviews 4
Rotchford AP, King AJ (2010) Moving the goal posts: definitions of success after glaucoma surgery and their effect on reported outcome. Ophthalmology 117(1):18–23
Aptel F, Denis P, Rouland JF, Renard JP, Bron A (2016) Multicenter clinical trial of high-intensity focused ultrasound treatment in glaucoma patients without previous filtering surgery. Acta Ophthalmol 94(5):e268–e277
De Gregorio A, Pedrotti E, Stevan G, Montali M, Morselli S (2017) Safety and efficacy of multiple cyclocoagulation of ciliary bodies by high-intensity focused ultrasound in patients with glaucoma. Graefes Arch Clin Exp Ophthalmol 255(12):2429–2435
Hu D, Tu S, Zuo C, Ge J (2018) Short-term observation of ultrasonic cyclocoagulation in chinese patients with end-stage refractory glaucoma: a retrospective study. J Ophthalmol 2018
Giannaccare G, Vagge A, Sebastiani S et al (2019) Ultrasound cyclo-plasty in patients with glaucoma: 1-year results from a multicentre prospective study. Ophthalmic Res 61(3):137–142
Posarelli C, Covello G, Bendinelli A, Fogagnolo P, Nardi M, Figus M (2019) High-intensity focused ultrasound procedure: the rise of a new noninvasive glaucoma procedure and its possible future applications. Surv Ophthalmol 64(6):826–834
Graber M, Rothschild PR, Khoueir Z, Bluwol E, Benhatchi N, Lachkar Y (2018) High intensity focused ultrasound cyclodestruction versus cyclodiode treatment of refractory glaucoma: a retrospective comparative study. J Fr Ophtalmol 41(7):611–618
Williams AL, Moster MR, Rahmatnejad K et al (2018) Clinical efficacy and safety profile of micropulse transscleral cyclophotocoagulation in refractory glaucoma. J Glaucoma 27(5):445–449
Emanuel ME, Grover DS, Fellman RL et al (2017) Micropulse cyclophotocoagulation: initial results in refractory glaucoma. J Glaucoma 26(8):726–729
Tan AM, Chockalingam M, Aquino MC, Lim ZI, See JL, Chew PT (2010) Micropulse transscleral diode laser cyclophotocoagulation in the treatment of refractory glaucoma. Clin Exp Ophthalmol 38(3):266–272
Aquino MC, Barton K, Tan AM et al (2015) Micropulse versus continuous wave transscleral diode cyclophotocoagulation in refractory glaucoma: a randomized exploratory study. Clin Exp Ophthalmol 43(1):40–46
Wilensky JT, Kammer J (2004) Long-term visual outcome of transscleral laser cyclotherapy in eyes with ambulatory vision. Ophthalmology 111(7):1389–1392
AGIS Investigators (1998) The Advanced Glaucoma Intervention Study (AGIS): 4. Comparison of treatment outcomes within race: seven-year results. Ophthalmology 105(7):1146–1164
Denis P, Aptel F, Rouland JF et al (2015) Cyclocoagulation of the ciliary bodies by high-intensity focused ultrasound: a 12-month multicenter study. Invest Ophthalmol Vis Sci 56(2):1089–1096
Funding
The authors have no financial or proprietary interest in any product mentioned in this paper. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
ESH is operating and following up the patients and revising the manuscript. AA was involved in acquisition, analysis, interpretation of data for the work, drafting the work and revising.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Ethical approval
Informed consent was obtained from all the patients. This study followed the tenets of Declaration of Helsinki, and the study protocol was revised and approved by Ophthalmology Department ethical committee at Cairo University.
Animal research
Not applicable.
Consent to participate
Not applicable.
Consent to publish
I confirm that this manuscript has been submitted solely to this journal and is not published in press or submitted elsewhere.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abdullatif, A.M., Ahmed El-Saied, H.M. Various modalities of cyclodestruction in non-refractory glaucoma: a comparative study. Int Ophthalmol 41, 3313–3323 (2021). https://doi.org/10.1007/s10792-021-01893-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-01893-z