Abstract
Purpose
Distribution of intermediate filament (IF) proteins in normal extraocular muscles (EOMs) showed that the EOMs differ significantly from the other muscles in the body with respect to their IFs composition, including desmin and nestin. The aim of the present study was to investigate the pathological changes in the medial rectus (MR) in patients with concomitant exotropia (XT).
Methods
Forty-six MR muscle samples from 46 patients with XT were analyzed pathologically and processed for immunohistochemistry with specific antibodies against desmin and nestin.
Results
Although most of MR muscles remained normal structures relatively, they presented high expression of desmin, and in contrast, nestin was absent in a large proportion of the MR muscles.
Conclusion
Desmin, which is downregulated in normal EOMs, had high expression in MR muscles of patients with XT. Nestin, which is present in a high proportion of normal EOMs, was downregulated in MR muscles of patients with XT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Strabismus, including concomitant strabismus and incomitant strabismus, is one of the most common disorders in pediatric ophthalmology, with an estimated prevalence of 3–5% worldwide [1]. Concomitant strabismus is characterized by a constant angle of deviation in all fields of gaze, and the deviation amplitude remains the same with either eye fixating. Hitherto in this type of horizontal deviation, there was no characteristic pathological change detected in extraocular muscles (EOMs) and its neurological innervations. And, the horizontal rectus muscle path lengths are not significantly abnormal in concomitant strabismus [2]. So, in the absence of obvious structural abnormalities of the eye or brain, the etiology of concomitant strabismus remains unclear.
The normal EOMs differ from typical skeletal muscles at the cellular and molecular level, in particular regarding the composition of the major proteins determining contraction force and velocity, calcium transportation proteins, extracellular matrix proteins, and neuromuscular junction gangliosides [3,4,5,6]. So in the patients with concomitant strabismus, the pathological structures and protein levels are probably more different from the normal EOMs and typical skeletal muscles. Indeed, our previous study confirmed the abnormal expression of structural proteins in some of the 324 EOMs of 278 patients with concomitant strabismus (unpublished data). And, we also found abnormal expression of myogenesis-related genes in EOMs of patients with concomitant strabismus [7]. Recent study on distribution of intermediate filament (IF) proteins in normal EOMs showed that the EOMs differ significantly from the other muscles in the body with respect to their IFs composition, including desmin and nestin [8].
In the present study, we investigated the pathological changes in the medial rectus (MR) muscles in patients with concomitant exotropia (XT), in order to identify whether there are special morphologic changes or expression of IF proteins in these muscles. Remarkably, we found changes in IFs composition of MR muscles with XT.
Materials and methods
Samples
The MR muscles were obtained from patients with XT during strabismic surgery at Zhongshan Ophthalmic Center, Guangzhou, China. A total of 46 MR muscles from 46 patients with XT were analyzed in this study. All of the muscle samples were obtained at least 2 mm from the insertion of each muscle into the globe, and the average muscle sizes dissected were 4–8 (6 ± 1.32) mm. All of the surgeries were taken by the same surgeon (Deng D.M.), and the force duction test was processed in all of the cases before the surgery in order to assess the restriction of ocular movements. Before the surgery, the clinical information of the individuals had been collected as shown in Table 1, including gender, duration of disease, angle of deviation, visual acuity, refraction, and function of binocular vision. None of the included cases was treated by Botox.
This study was performed in accordance with the tenets of the Declaration of Helsinki. Informed consent was obtained in every case from participants or their guardians before the collection of muscle samples. This study was approved by the Institutional Review Board of the Zhongshan Ophthalmic Center.
Masson’s trichrome (MT) staining
The muscle samples were embedded in paraffin and processed for coronal sectioning at 10 μm thickness, as described previously [9]. The MR muscle samples were step-sectioned transversely at intervals of 200 μm. The sections were mounted on poly-l-lysine-coated slides, dried at 60 °C overnight, dewaxed with xylene, and gradually hydrated. MT stain was applied to dewaxed sections to visualize muscle and connective tissue constituents [10].
Immunohistochemical analysis
Antigen retrievals of the dewaxed sections were achieved by pressure-cooking in 0.01 mol/L citrate buffer for 15 min. Endogenous peroxidase was blocked by incubation with 3% hydrogen peroxide (H2O2) for 10 min. To reduce nonspecific binding, the sections were incubated with 20% normal goat serum for 10 min at 37 °C. Primary antibodies were incubated overnight at 4 °C, followed by rinsing with phosphate-buffered saline (PBS). Then, the slides were incubated for 10 min at room temperature with secondary antibodies and were stained for 10 min with 3,3′-diaminobenzidine tetrahydrochloride (DAB). Negative controls were subjected to the same procedure, except that the primary antibody was replaced by PBS.
All of the antibodies were purchased from BioVision in the USA (BioVision, Inc., Milpitas, CA, USA), and the finial dilutions were 1:50.
Semiquantitative evaluation of staining
The pathologist, who was unaware of the patients, independently examined the slides. For this study, only the cytoplasmic immunohistological staining was scored, and only the staining of myocytes was obtained. Staining intensity was categorized into four groups by comparing the staining intensity of muscle cells with that of vascular endothelial cells. The staining intensity was scored as 0 (no staining), 1 (faint yellow), 2 (brown-yellow), or 3 (dark yellow). The extent of staining was scored according to the proportion of positive cells in the muscle cells, as 0 (< 5%), 1 (5–25%), 2 (26–75%), or 3 (more than 76%). The final score of 0–6 was obtained by summing the two scores above, and the expression categories of desmin and nestin were defined as follows: − (0), + (1–2), ++ (3–4), and +++ (5–6).
Statistical analysis
Statistical analysis was carried out using SPSS version 11.0 (SPSS Inc., Chicago, IL, USA). The Chi-squared tests were applied to compare the complete fibrosis in horizontal rectus muscles among different groups. The Wilcoxon rank sum tests were used to evaluate the correlation between desmin or nestin expression and clinical parameters, including duration of strabismus and degree of deviation.
The duration of strabismus was calculated from age of onset to surgery, and the degree of deviation was determined by the largest value of the deviation in both eyes at distance or vicinity. Differences were considered to be statistically significant at p < 0.01.
Results
Clinical findings
The ocular deviations with naked eyes were measured for all of the 46 patients with XT before the surgery by perimeter arc, and the synoptophore was used to obtain the function of binocular vision (Table 1). All of the patients had normal ocular movements. No restriction of movements was revealed in all directions under general anesthesia by the force duction test.
Morphology
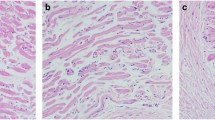
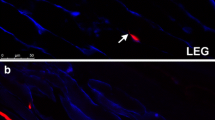
The hematoxylin and eosin (HE) staining and Masson’s trichrome staining of MR muscle in XT showed almost normal structure of muscle cells (Fig. 1).
Immunohistochemical staining
We found high expression (++/+++) of desmin in the cytoplasm of muscle cells in most (92.7%, 38/41) of samples, while the expression of nestin was low (+) or absent (−) in most (82.9%, 34/41) of samples (Table 2, Fig. 1).
After excluding five MR muscles with complete fibrosis, statistical analysis of the expression of desmin and nestin in cytoplasm of the muscle fibers was processed in 41 MR muscles from patients with XT (Table 2). No significant correlation was observed between desmin or nestin expression and clinical parameters, including duration of strabismus and degree of deviation (Tables 3 and 4).
Discussion
Previous studies had already paid attention to the pathological changes in EOMs in patients with strabismus, showing that fibrous atrophy of EOMs in patients with concomitant strabismus was common [11, 12]. However, we detected that MR muscles in XT were almost normal in this study regardless of duration of strabismus and degree of deviation. It may indicate that the pathological change of the EOMs in concomitant strabismus may not be in morphological aspect but in the changes in specific protein composition.
Recent study on distribution of IF proteins in normal EOMs showed that the EOMs differ significantly from the other muscles in the body [8]. According to the previous study in normal LR muscles and superior rectus muscles, desmin was absent or only present in a very low level in a subset of muscle fibers, and nestin was present in a high level in muscle fibers [8]. However, in contrast, we found high expression of desmin in MR muscles of patients with concomitant XT in the present study, and the expression of nestin was low or absent in most of the samples (Table 2).
Desmin, which is the most abundant IF protein in mature skeletal muscles, plays an essential role in maintaining cytoarchitecture, positioning and functioning of organelles, and the intercellular signaling pathway [13,14,15]. Nestin, which is co-expressed transiently during early development of muscles and downregulated postnatally in skeletal muscles [16,17,18], is a reliable marker of neural stem cells and is closely correlated with poor prognosis in several tumors [19, 20]. The high expression of desmin and the absence/low levels of nestin in MR muscles of patients with XT indicate that these EOMs had abnormal expression of IF proteins. It has been reported that modifying the surgical dose according to age can improve the success in patients with intermittent exotropia, indicating changes in EOMs with age in horizontal strabismus [21]. But according to the results of the present study, we found no significant correlation between desmin or nestin expression and clinical parameters, including duration of strabismus and degree of deviation (Tables 3 and 4).
Results of this study should be understood within the context of limitations imposed by no normal controls. Because the human EOMs of normal controls can only be obtained at autopsy, we compared the results of this study with the previous study in healthy human rectus muscles. And, we collected the MR muscle samples during the resection process of the strabismic surgery, so the involved samples were closer to the tendon of the MR muscle, and this might have affected the difference in expression of desmin and nestin in the MR muscles.
In conclusion, the present study on changes in IFs in MR muscles in patients with XT showed that the expression of desmin was upregulated in MR muscles in patients with XT, while the expression of nestin was downregulated.
References
Arora A, Williams B, Arora AK, McNamara R, Yates J, Fielder A (2005) Decreasing strabismus surgery. Br J Ophthalmol 89(4):409–412. https://doi.org/10.1136/bjo.2004.053678
Rabinowitz R, Demer JL (2014) Muscle path length in horizontal strabismus. J AAPOS 18(1):4–9. https://doi.org/10.1016/j.jaapos.2013.10.019
Kjellgren D, Thornell LE, Andersen J, Pedrosa-Domellof F (2003) Myosin heavy chain isoforms in human extraocular muscles. Invest Ophthalmol Vis Sci 44(4):1419–1425
Pedrosa-Domellof F, Holmgren Y, Lucas CA, Hoh JF, Thornell LE (2000) Human extraocular muscles: unique pattern of myosin heavy chain expression during myotube formation. Invest Ophthalmol Vis Sci 41(7):1608–1616
Kjellgren D, Thornell LE, Virtanen I, Pedrosa-Domellof F (2004) Laminin isoforms in human extraocular muscles. Invest Ophthalmol Vis Sci 45(12):4233–4239. https://doi.org/10.1167/iovs.04-0456
Liu JX, Willison HJ, Pedrosa-Domellof F (2009) Immunolocalization of GQ1b and related gangliosides in human extraocular neuromuscular junctions and muscle spindles. Invest Ophthalmol Vis Sci 50(7):3226–3232. https://doi.org/10.1167/iovs.08-3333
Zhu Y, Deng D, Long C, Jin G, Zhang Q, Shen H (2013) Abnormal expression of seven myogenesis-related genes in extraocular muscles of patients with concomitant strabismus. Mol Med Rep 7(1):217–222. https://doi.org/10.3892/mmr.2012.1149
Janbaz AH, Lindstrom M, Liu JX, Pedrosa Domellof F (2014) Intermediate filaments in the human extraocular muscles. Invest Ophthalmol Vis Sci 55(8):5151–5159. https://doi.org/10.1167/iovs.14-14316
Demer JL, Oh SY, Clark RA, Poukens V (2003) Evidence for a pulley of the inferior oblique muscle. Invest Ophthalmol Vis Sci 44(9):3856–3865
Demer JL, Miller JM, Poukens V, Vinters HV, Glasgow BJ (1995) Evidence for fibromuscular pulleys of the recti extraocular muscles. Invest Ophthalmol Vis Sci 36(6):1125–1136
Gralek M, Krawczyk T (1998) Pathomorphological evaluation of the extraocular muscles during strabismus. Klin Oczna 100(6):373–375
Kim SH, Cho YA, Park CH, Uhm CS (2008) The ultrastructural changes of tendon axonal profiles of medial rectus muscles according to duration in patients with intermittent exotropia. Eye 22(8):1076–1081. https://doi.org/10.1038/eye.2008.133
Li H, Choudhary SK, Milner DJ, Munir MI, Kuisk IR, Capetanaki Y (1994) Inhibition of desmin expression blocks myoblast fusion and interferes with the myogenic regulators MyoD and myogenin. J Cell Biol 124(5):827–841
Weitzer G, Milner DJ, Kim JU, Bradley A, Capetanaki Y (1995) Cytoskeletal control of myogenesis: a desmin null mutation blocks the myogenic pathway during embryonic stem cell differentiation. Dev Biol 172(2):422–439. https://doi.org/10.1006/dbio.1995.8070
Milner DJ, Mavroidis M, Weisleder N, Capetanaki Y (2000) Desmin cytoskeleton linked to muscle mitochondrial distribution and respiratory function. J Cell Biol 150(6):1283–1298
Kachinsky AM, Dominov JA, Miller JB (1994) Myogenesis and the intermediate filament protein, nestin. Dev Biol 165(1):216–228. https://doi.org/10.1006/dbio.1994.1248
Albers K, Fuchs E (1992) The molecular biology of intermediate filament proteins. Int Rev Cytol 134:243–279
Sejersen T, Lendahl U (1993) Transient expression of the intermediate filament nestin during skeletal muscle development. J Cell Sci 106(Pt 4):1291–1300
Singh SK, Clarke ID, Hide T, Dirks PB (2004) Cancer stem cells in nervous system tumors. Oncogene 23(43):7267–7273. https://doi.org/10.1038/sj.onc.1207946
Ryuge S, Sato Y, Wang GQ, Matsumoto T, Jiang SX, Katono K, Inoue H, Satoh Y, Masuda N (2011) Prognostic significance of nestin expression in resected non-small cell lung cancer. Chest 139(4):862–869. https://doi.org/10.1378/chest.10-1121
Awadein A, Eltanamly RM, Elshazly M (2014) Intermittent exotropia: relation between age and surgical outcome: a change-point analysis. Eye 28(5):587–593. https://doi.org/10.1038/eye.2014.29
Acknowledgements
This study was supported by the Natural Science Foundation of Guangdong Province, China (Grant No. 2014A030310213). Tao Shen received the funding. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Shen, T., Lin, J., Li, X. et al. Intermediate filaments in the medial rectus muscles in patients with concomitant exotropia. Int Ophthalmol 40, 403–410 (2020). https://doi.org/10.1007/s10792-019-01197-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-019-01197-3