Abstract
Background
To investigate the incidence and prevalence of dry eye disease (DED) in Taiwan and to explore its potential risk factors.
Methods
Population-based longitudinal data from 2000 to 2013 based on Taiwan National Health Insurance Research Database were used in this study. To explore potential risks factor of interest, patients who had DED diagnosis before the exposure were excluded. Each patient from the exposure and his/her matched non-exposure controls were followed until either the diagnosis of DED or censorship. Kaplan–Meier method was used to compare the hazard of DED between cohorts. Stratified Cox proportional hazard models were applied to estimate the adjusted effect.
Results
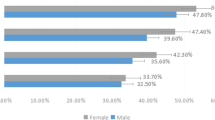
The age-adjusted prevalence for men and women were 6.81% and 16.16%, respectively. The age–gender rate of the same period was 549 per 105 person-years. The propensity-adjusted hazard ratio of DED is 1.816 for the presbyopia versus non-presbyopia (with 95% CI = [1.737, 1.897] with p value < 0.0001).
Conclusions
The DED incidence for women peaked at age 50–74, while that for men peaked at age ≧ 75. The incidence in young people seems stable both for women and for men. While exploring the factors of DED, there is a significant association between presbyopia and DED even after matching age/gender and comorbidity conditions. Further clinical studies are needed to justify whether the corrective refractive treatment such as presbyopic glasses to treat the frequently hyperopic status of these patients could be beneficial to both dry eye and presbyopic condition.



Similar content being viewed by others
Abbreviations
- DED:
-
Dry eye disease
- DM:
-
Diabetes mellitus
- LASIK:
-
Laser-assisted in situ keratomileusis
- MGD:
-
Meibomian gland dysfunction
- NHIRD:
-
National Health Insurance Research Database
- OSDI:
-
Ocular Surface Disease Index
- PK:
-
Penetrating keratoplasty
- PS:
-
Propensity score
- SLE:
-
Systemic lupus erythematosus
- VDT:
-
Video display terminal
References
Solomon JD (2010) Outcomes of corneal spherical aberration-guided cataract surgery measured by the OPD-scan. J Refract Surg 26(11):863–869
Courtin R, Pereira B, Naughton G et al (2016) Prevalence of dry eye disease in visual display terminal workers: a systematic review and meta-analysis. BMJ Open 6:e009675. https://doi.org/10.1136/bmjopen-2015-009675
Schaumberg DA, Sullivan DA, Buring JE, Dana MR (2003) Prevalence of dry eye syndrome among US women. Am J Ophthalmol 136(2):318–326
Schaumberg DA, Dana R, Buring JE, Sullivan DA (2009) Prevalence of dry eye disease among US men: estimates from the Physicians’ Health Studies. Arch Ophthalmol 127(6):763–768. https://doi.org/10.1001/archophthalmol.2009.103
Lin PU, Tsai SY, Cheng CY, Liu JH, Chou P, Hsu WM (2003) Prevalence of dry eye among an elderly Chinese population in Taiwan: The Shihpai Eye Study. Ophthalmology 110:1096–1101
Yen JC, Hsu CA, Li YC et al (2015) The prevalence of dry eye syndrome’s and the likelihood to develop Sjögren’s syndrome in Taiwan: a population-based study. Int J Environ Res Public Health 12:7647–7655. https://doi.org/10.3390/ijerph120707647
Lee AJ, Lee J, Saw SM et al (2002) Prevalence and risk factors associated with dry eye symptoms: a population based study in Indonesia. Br J Ophthalmol 86:1347–1351
Ţuru L, Alexandrescu C, Stana D, Tudosescu R (2012) Dry eye disease after LASIK. J Med Life 5(1):82–84
Yilmaz U, Gokler ME, Unsal A (2015) Dry eye disease and depression-anxiety-stress: a hospital-based case control study in Turkey. Pak J Med Sci 31(3):626–631. https://doi.org/10.12669/pjms.313.7091
Chen CH, Yang TY, Lin CL et al (2016) Dry eye syndrome risks in patients with fibromyalgia: A National Retrospective Cohort Study. Medicine 95(4):e2607
Galor A, Feuer W, Lee JD et al (2011) Prevalence and risk factors of dry eye syndrome in a United States veterans affairs population. Am J Ophthalmol 152(3):377–384. https://doi.org/10.1016/j.ajo.2011.02.026
Denoyer A et al (2015) Dry eye disease after refractive surgery: comparative outcomes of small incision lenticule extraction versus LASIK. Ophthalmology 122:669–676
Rosenbaum PR, Rubin DB (1984) Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc 79:516–524
Kaido M, Kawashima M, Ishida R, Tsubota K (2017) Severe symptoms of short tear break-up time dry eye are associated with accommodative microfluctuations. Clinic Ophthalmol 11:861–869
Acknowledgements
The authors would like to thank Taiwan National Health Research Institute for the approval of using the National Health Insurance Research Data.
Author information
Authors and Affiliations
Contributions
EM conceived the study and drafted the manuscript, CL participated in the design of the study and coordination, IL coordinated the statistical analysis and interpreted the results, RL and CM carried out the data management and analysis, and CC carried out the epidemiological studies and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Availability of data and materials
Data used in analysis are available upon request to corresponding author.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All personal identification numbers in NHIRD used in this study were encrypted by conversion into scrambled numbers before data processing. Because the database used consists of de-identified secondary data released for research purposes, this study was exempt from full review by the Institutional Review Board National Changhua University of Education (No. NCUEREC-103-211).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Rights and permissions
About this article
Cite this article
Mai, E.L.C., Lin, Cc., Lian, I. et al. Population-based study on the epidemiology of dry eye disease and its association with presbyopia and other risk factors. Int Ophthalmol 39, 2731–2739 (2019). https://doi.org/10.1007/s10792-019-01117-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-019-01117-5