Abstract
Background
It is known that severe acute respiratory coronavirus 2 (SARS-CoV-2) is the viral strain responsible for the recent coronavirus disease 2019 (COVID-19) pandemic. Current documents have demonstrated that the virus causes a PGE2 storm in a substantial proportion of patients via upregulating cyclooxygenase-2 (COX-2) and downregulating prostaglandin E2 (PGE2)-degrading enzymes within the host cell.
Aim
Herein, we aimed to study how short-term treatment with celecoxib (Celebrex), a selective COX-2 inhibitor, affects demographic features, early symptoms, O2 saturation, and hematological indices of cases with COVID-19.
Methods
A total of 67 confirmed COVID-19 cases with a mild or moderate disease, who had been referred to an institutional hospital in south-eastern Iran from October 2020 to September 2021, were enrolled. Demographic characteristics, symptoms, and hematological indices of the patients were recorded within different time periods. One-way ANOVA or Kruskal–Wallis tests were used to determine differences between data sets based on normal data distribution.
Results
O2 saturation was statistically different between the control group and patients receiving celecoxib (p = 0.039). There was no marked difference between the groups in terms of the symptoms they experienced (p > 0.05). On the first days following Celebrex therapy, analysis of complete blood counts showed that white blood cell (WBC) counts were markedly lower in patients treated with a high dose of celecoxib (0.4 g/day) than in controls (p = 0.026). However, mean lymphocyte levels in patients receiving a high dose of celecoxib (0.4 g/day) were markedly higher than in patients receiving celecoxib with half of the dose (0.2 g/day) for one week or the untreated subjects (p = 0.004). Changes in platelet count also followed the WBC alteration pattern.
Conclusion
Celecoxib is a relatively safe, inexpensive, and widely available drug with non-steroidal anti-inflammatory properties. The therapeutic efficacy of celecoxib depends on the administrated dose. Celecoxib might improve disease-free survival in patients with COVID-19.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An infection of the respiratory tract, coronavirus disease 2019 (COVID-19), is caused by the newly identified severe acute respiratory distress syndrome coronavirus 2 (SARS-CoV-2) (Ghaznavi et al. 2022; Heidari Nia et al. 2021; Sivasankarapillai et al. 2020), imposing an average mortality rate of 14% to the communities worldwide (Ghaznavi et al. 2022). Recognized widely as a systemic hyper-inflammatory condition in severe cases, COVID-19 is associated with excess production of several cytokines and chemokines, several of which are directly modulated by the SARS-CoV-2 virus itself (Liu et al. 2007; Yan et al. 2006). Recent investigations have reported an increased serum level of prostaglandin E2 (PGE2) in COVID-19 patients, which is suggested to be caused by the positive regulatory effect of SARS-CoV-2 on cyclooxygenase-2 (COX-2) (Hong et al. 2020), a well-known inflammatory modulator involved in the arachidonic acid metabolic pathway, resulting in a significant accumulation of prostaglandins (PGs) (Kuehl and Egan 1980). Another reason behind the upregulated levels of PGE2 in COVID-19 is thought to be the downregulation of PG-degrading enzymes, which is, again, a consequence of SARS-CoV-2 infection (Al Saleh and AlQahtani 2021). Additionally, the PGs system has partial overlap, which means that other mediators, such as endogenous nitric oxide (NO), could play a role in COVID-19 etiology (Pieretti et al. 2021). NO is thought to cause vasodilation in the cardiovascular system and immunological reactions involving cytokine-activated macrophages, which produce high NO levels. Moreover, NO is involved in the pathophysiology of pulmonary inflammatory diseases (Sharma et al. 2007). NO exacerbates the inflammatory process by causing the creation of more PGs (Salvemini et al. 1993). The severity of COVID-19 can be associated with elevated PGE2 levels along with overproduction of NO and thromboxanes (Al-Hakeim et al. 2021; Smeitink et al. 2020).
PGE2 is a metabolite of arachidonic acid with a positive regulatory effect on vascular endothelial growth factor (VEGF) (Kwong et al. 2008), which was found to be overproduced in critically ill COVID-19 patients and proposed to serve as a target for anti-VEGF agents to treat acute respiratory distress syndrome (ARDS) related to COVID-19 (Hong et al. 2020). There is now precedent that the COVID-19-related respiratory failure might predispose patients to ischemic brain injury (DeKosky et al. 2021), pathology of the central nervous system that is thought to be mediated, in part, by COX-2 (Dembo et al. 2005). Else, PGE2 can also be induced by nitric oxide (NO), a vasodilatory byproduct of inducible nitric oxide (iNOS). The expression of NO itself is said to be under the influence of COX-2 (Sharma et al. 2007) as COX-2 inhibitors are suggested to repress iNOS, thus, opposing NO's vasodilating effects (Ukawa et al. 1998). Excess concentrations of PGE2 might aggravate the cytopathic effects of SARS-CoV-2 infection by repressing the innate immune response in COVID-19 patients (Hong et al. 2020; Morimoto et al. 2014; Niwa et al. 2009; Säfholm et al. 2013; Zamora et al. 1993). This is illustrated in detail in Fig. 1.
Hypothesis; excessive inflammation may be a key in the pathology of COVID-19, and COX-2 could be a critical target for therapy. To test this hypothesis, COVID-19 patients received celecoxib, a specific inhibitor of COX-2, in the short term as adjuvant therapy to evaluate correlation with disease status
The COVID-19 infection is characterized by a bursting production of cytokines that increase the severity of the infection, primarily due to the unique immunopathogenic features of the virus. The use of typical medicines to inhibit these overexpressed immunogenic pathways in coronavirus-infected tissues has been debated since the epidemic began. The efficacy of non-steroidal anti-inflammatory drugs (NSAIDs) such as celecoxib (Celebrex) in COVID-19 coagulopathy, inhibiting severe acute respiratory syndrome (SARS) viral replication, inflammasome inhibition, and synergic suppression of H5N1 infection with antiviral medications, combined, has created a glimmer of hope in adjuvant COVID-19 therapy (Robb et al. 2020).
Celecoxib, also known as Celebrex, belongs to the family of NSAIDs and is essentially a selective inhibitor of COX-2. While celecoxib and its novel formulations are predominantly used to treat rheumatologic diseases (Abualhasan et al. 2021; Chan et al. 2004; Hosseinikhah et al. 2021), it could still be repurposed as an adjuvant treatment for COVID-19 due to its counter-regulatory effects on COX-2, PGE2, and inducible nitric oxide synthase/ nitric oxide (iNOS/NO). We know that PGE2 can suppress the activation and proliferation of lymphocytes by binding to the EP4 receptor and downregulating the CD25 lymphocyte marker (Dutton et al. 2018), an adverse outcome in the case of COVID-19 that celecoxib can potentially reverse. Besides, selective COX-2 inhibitors might also prove effective in managing COVID-19-related thrombocytopenia, which occurs in 5–41% of patients (Singh et al. 2021). This speculation is based on the fact that celecoxib downregulates prostacyclin I2 (PGI2) more potently than the platelet activator thromboxane A2 (TXA2), resulting in a reduced prostacyclin I2/thromboxane A2 (PGI2/TXA2) ratio and an overall procoagulant state (Grimm et al. 2018).
With the current therapeutic regimes concentrated on viral S proteins, viral 3CL protease enzyme, immune regulation, viral replication prevention, and symptomatic relief, the repurposing of pharmaceuticals to fulfill the need for therapy has become the need of the hour to meet the rising urgency of treatment. Our hypothesis proposes that short-term treatment with Celebrex reduces vasodilation by explicitly inhibiting the COX-2 enzyme and further dramatically reducing the expression of PGs and other inflammatory mediators. As a result, the production and secretion of NO are reduced. This process limits the subsequent mechanisms of inflammation such as vasodilation, secretion of cytokines and pulmonary edema, and overall positive feedback of lung tissue inflammation. This view can help alleviate pulmonary symptoms, better control the disease, and significantly reduce mortality in COVID-19 cases.
Materials and methods
Study design and participants
The present experiment is an in-hospital prospective study conducted at Zahedan University of Medical Sciences, Zahedan, Iran. According to a previously published protocol, patients with SARS-CoV-2 infection were confirmed by reverse transcription-polymerase chain reaction (RT-PCR) (Heidari Nia et al. 2021; Lee et al. 2008). A total of 67 confirmed COVID-19 patients with a mild or moderate scenario, who had been referred from October 2020 to September 2021, were enrolled in this study. The demographic characteristics of patients are reported in Table 1.
At the beginning of the study, the enrolled cases were fully informed of the study's goal, merits, and potential hazards and signed informed permission. The protocol of the study was approved by the ethics committee of Zahedan University of Medical Sciences (Ethical code: IR.ZAUMS.REC.1399.197) (Webpage of ethical approval code is: https://ethics.research.ac.ir/EthicsProposalViewEn.php?id=149801). The study was registered on the Iranian Registry of Clinical Trials (IRCT) under the Trial ID: IRCT20200907048644N1. The clinical criteria for the categorization of COVID-19 are as follows, according to Iran's "Diagnosis and Treatment Guideline for COVID-19." Mild: the clinical symptoms are mild, and no pneumonia manifestation can be found in computed tomography (CT) imaging; moderate: fever and respiratory tract symptoms, etc., and pneumonia manifestation can be seen in CT imaging. The overall procedure of the study is illustrated in Fig. 2.
Inclusion and exclusion criteria
Our studied groups included group A (N = 21), group B (N = 20), and group C (N = 26). Patients with the mild or moderate condition and below characteristics were enrolled in the present trial:
-
1.
Aged 18–65 years
-
2.
Positive RT-PCR test
-
3.
With or without fever equal to or greater than 38 degrees
-
4.
Shortness of breath, having chest pain
-
5.
Blood oxygen saturation (SpO2) between 90 and 93%
-
6.
Patient's consent for participation
Patients with severe to critical diseases were excluded. As hyperglycemia, particularly in diabetes, might lead to activation of COX-2 (Rojas-Carranza et al. 2018), participants with diabetes were excluded as well.
Clinical information and celecoxib usage
Subjects' clinical data, including physical exams, laboratory tests, and a chest CT scan (as an additional test), were recorded. The patients in experimental group A (N = 21) and group B (N = 20) were treated with celecoxib (Razi, Iran) in addition to the guideline's recommended routine treatments. The dosage of celecoxib (0.2 g/time) was twice a day (group A) or once a day (group B) for 7 days by oral intake. The dosage and period of medication were likely to be modified depending on each case. Group control (C, N = 26) received the exact same treatment as the experimental groups and naproxen (as NSAID, 0.25 g/time, twice a day), instead of celecoxib. All patients had clinical examinations like laboratory tests on the first and seventh days of the study. The physical information of patients is listed in Table 2.
Single-blinded procedure and Celecoxib and Naproxen preparation
We used the permuted block randomization method to randomly assign participants to each group (Broglio 2018). Patients who had a positive RT-PCR test result for SARS-CoV-2 infection were then evaluated by a specialist physician against the eligibility criteria and asked to provide demographic information, after which they each would be assigned with a unique patient code and begin receiving therapeutic regimens according to the guidelines provided by Ministry of Health and Medical Education of Iran. Participants requiring outpatient treatment, i.e., patients with mild to moderate disease who did not need to be hospitalized, received the routine therapeutic regimen for COVID-19 along with celecoxib.
The present clinical trial was a single-blind study, as participants in each group were unaware of the type of investigational intervention (Celecoxib or Naproxen) they were receiving. Participants in group A received a total daily dose of 400 mg, divided into two 200 mg doses, in the form of indiscernible capsules, while those in group B were only treated with a daily dose of 200 mg. Patients in group C, on the other hand, were treated with naproxen at a daily dose of 500 mg, divided into two 250 mg doses that were ingested every 12 h. The blood levels of celecoxib were not measured.
Laboratory test results and clinical outcome
After the study period, based on comparing laboratory test results and the changes in symptoms and/or sequential chest CT images, the clinical outcomes were classified into four categories: expiration, hospitalization during celecoxib therapy, and a constant need for therapy, and remission. Remission was defined as the disappearance or clarification of the mass opacities on chest CT scans or as a steady decline in laboratory parameters, such as the D-dimer, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), serum alanine aminotransferase (ALT), and aspartate aminotransferase levels (AST), as well as an improvement in lymphopenia and neutropenia (Table 3). The clinical condition of participants determined the duration of treatment with celecoxib.
Statistical analysis
The quantitative results are presented in mean ± standard error (mean ± SEM). Based on the normal distribution of test results, the differences between the three groups were tested using the one-way ANOVA test or the Kruskal–Wallis test for groups with more than two participants. We used the independent T and Mann–Whitney U tests to compare two groups based on the normal data distribution. Statistical analysis was conducted with SPSS 19.0 software. A p < 0.05 was considered statistically significant.
Results
Demographic characteristics of participants
Table 1 presents the demographic characteristics of patients. 42 women and 25 men participated in the present study with a mean age of 41 ± 1.57 years. 41 participants were employed, 5 were retired, and 18 were housewives. 22.4% of patients were active smokers. The mean body mass index (BMI) was 25.27 ± 0.62. Blood types included 31.3% O, 27.1% A, 27.1% B, and 14.6% AB, of which 95.3% were Rh+ and 4.7% were Rh−. None of the patients presented any types of underlying chronic illnesses.
Symptomatology of patients on the first, third, and seventh day of study
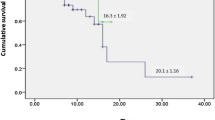
Table 2 lists the symptomatologic profile of COVID-19 patients on the first, third, and seventh days of the study. Statistically, we did not observe any significant effects of celecoxib administration on the symptomatologic profile of patients at the end of the seventh day (p > 0.05), except for O2 saturation, which was higher in group A and lower in group B compared with group C (p = 0.039; Fig. 2). However, in each group, the increased severity of symptoms of the disease on the third day attenuated on the seventh day (Fig. 3).
Laboratory findings of patients and clinical outcome
Table 3 and Fig. 4 present the laboratory findings of patients on the first, third, and seventh study days. Between the several hematologic markers, white blood cells (WBC), lymphocytes, neutrophils, platelets, red blood cells (RBCs), and hemoglobin (Hb) were analyzed. WBC, lymphocyte, and platelets on the seventh day of the study showed a significant difference between the three groups (p < 0.05). Accordingly, the mean level of WBC was significantly lower in group A compared with other groups B and C. In COVID-19 cases, on the 7th day, the lymphocyte count was markedly higher in group A than in groups B and C. At the same time, compared with groups B and C, cases in group A exhibited significantly lower platelet levels 1 week after the admission. Neutrophil count decreased on the seventh day in groups A and B compared to the first day, while the control group showed opposite results. At the same time, the RBC and Hb showed semi-stable levels. No significant differences were found between different groups in terms of neutrophils, RBCs, and Hb levels after the first and 7th day of admission (p > 0.05).
Laboratory findings of patients. a WBC, b lymphocyte, and d platelets on the seventh day of the study showed a significant difference between the three groups (p < 0.05). c Neutrophil decreased on the seventh day in groups A and B compared to the first day, while the co\ntrol group showed vice versa results. At the same time, both e RBC and f Hb showed semi-stable levels
Additionally, the clinical outcome of patients has been evaluated. In groups A, B, and C, we observed that 11, 16, and 19 patients needed continuous therapy after the seventh day of study, respectively, while 10, 4, and 6 patients had already remised.
Discussion
Inhibition of COX-2 by celecoxib was previously reported to downregulate tumor necrosis factor-alpha (TNF-α) and interleukin 6 (IL-6) in H5N1-infected alveolar macrophages (Lee et al. 2008), both of which are extensively involved in SARS-CoV-2 pathogenesis, as well. In addition to inhibiting COX-2, celecoxib may also inhibit p38 mitogen-activated protein kinases (p38 MAPK) (Chen et al. 2015), which is suggested to facilitate SARS-CoV-2 cell entry (Cioccarelli et al. 2021). Despite these beneficial effects, inhibition of COX-2 might disrupt the proper differentiation of B cells and subsequent production of antibodies, which is required for appropriate containment of viral infections (Kim et al. 2018). This information on the dual role of COX-2 inhibitors on the immune system suggests that the length of celecoxib therapy be set individually for each patient based on their clinical state and laboratory results in a tailored manner.
In the present study, we aimed to study how short-term treatment with celecoxib, a selective COX-2 inhibitor, might affect the demographic features, symptoms, O2 saturation, and laboratory findings of COVID-19 patients with mild to moderate disease. The majority of participants were females with an average BMI of 25.27 kg/m2. O/Rh+ was the predominant blood type among patients. O2 saturation was statistically different between the control group and patients who had received celecoxib for seven days. No significant difference was noticed between controls and treatment groups in terms of symptoms, i.e., cough, dry mouth, sore throat, dry throat, eye redness, loss of smell or taste, myalgia, headache, chills, lethargy, vomiting and nausea, diarrhea, confusion, fatigue, bone pain, and chest pain, following celecoxib administration. We also aimed to determine the pattern of changes in patients' complete blood count (CBC). For this purpose, we assessed possible changes in hematological indices of the studied groups on the first and seventh days from the onset of the investigation. The WBC count was markedly lower in patients treated orally with celecoxib (0.4 g/day, group A). Interestingly, one week following the administration of celecoxib, the mean lymphocyte levels in these patients were significantly higher than in cases receiving Celebrex (0.2 g/day, group B) or the untreated subjects.
Changes in platelet levels also followed the WBC alteration pattern. Changes in platelet levels have been reported to be frequent among patients in the intensive care unit (ICU), with 5–41% of these patients suffering from thrombocytopenia (Al Saleh and AlQahtani 2021). Clinical trials on COVID-19 cases have revealed that the number of WBCs, neutrophils, monocytes, eosinophils, and lymphocytes gradually increases within 8–14 days from admission to the hospital, while the RBC count and Hb level continue to decline through the 20th day of admission (Lu and Wang 2020). Eslamijouybari et al. reported that the platelet count, lymphocyte count, and Hb level were significantly lower in COVID-19 patients than in healthy individuals (Eslamijouybari et al. 2020). In their meta-analysis, Feng et al. demonstrated that COVID-19 patients with severe disease were inclined to present leukocytosis, granulocytosis, and lymphopenia compared to patients with mild to moderate illness (Feng et al. 2020). In our study, compared with the control group or cases receiving celecoxib for one week with a twice dose (0.4 g/day), the low dose of the drug (0.2 g/day) increased total WBC count and platelets while decreasing lymphocyte count. Our observations are not completely supported by another investigation on celecoxib by Hong et al., as their study was chiefly concerned with the levels of PGE2 and, therefore, has not reported any findings regarding the CBC of their participants (Hong et al. 2020).
Few studies have been done to see if Celebrex affects SARS-CoV-2 replication. The cyclooxygenase-1 (COX-1) and COX-2 inhibitors, on the other hand, have been shown to have an inhibitory effect on other coronavirus subtypes as well. It was confirmed by Hong et al. that the urine levels of PGE2 in COVID-19 were considerably greater than those in healthy individuals, indicating an even higher concentration of this prostaglandin in the lungs and blood of these patients. Excess circulating levels of PGE2 have been recognized as a 'prostaglandin storm' that occurs in the hyper-inflammatory phase of COVID-19, which has been shown to be reversed effectively by celecoxib. However, discontinuation of therapy might result in recurrence of PGE2 storm, exacerbating the clinical condition of patients in some instances. Regardless, treatment with celecoxib was still associated with a lower mortality rate in COVID-19, as patients receiving full (200 mg, twice a day) or a half dose (200 mg, once a day) of celecoxib showed 100 and 82% remission rates, respectively (Hong et al. 2020). A study by Raaben et al. found that COX nonselective inhibitors indomethacin and curcumin suppressed the RNA, protein, and virus particle formation in the mouse model of hepatitis coronavirus, following a dose-dependent fashion. Likewise, NS-398 and SC-560 (as COX-1 and COX-2 inhibitors, respectively) diminished mouse hepatitis virus (coronavirus) infection by 65–75% in an in-vitro experiment (Raaben et al. 2007). A study by Amici and his colleagues showed that indomethacin reduces cell infection by directly inhibiting the generation of SARS-CoV and canine coronavirus (CCoV) particles in both in-vitro and in-vivo models (Amici et al. 2006).
Besides its negative effect on PGE2, other mechanisms that might contribute to the beneficial effects of COX-2 inhibitors are yet to be understood. An investigation by Gimeno et al. suggested that COX-2 inhibitors, such as celecoxib, might bind the main protease of SARS-CoV-2 and impair its replication (Gimeno et al. 2020). However, this speculation about celecoxib was later contradicted by Terrier et al. They reported that only naproxen, among NSAIDS, could inhibit the replication of SARS-CoV-2 by binding to its nucleoprotein and that celecoxib did not possess such properties (Terrier et al. 2021). Another study by de Burin et al. concluded that etoricoxib, a selective COX-2 inhibitor, was capable of reducing the viral load in cells infected with SARS-CoV-2, possibly through downregulation of angiotensin-converting enzyme 2 (ACE2), which is a pivotal receptor for SARS-CoV-2 (de Bruin et al. 2022), further indicating the effectiveness of COX-2 inhibitors as an adjuvant treatment for COVID-19. Speculation by Khupse et al. argues that celecoxib competes with SARS-CoV-2 at binding the host cell's bromodomain proteins (BRD)-2/4 and, thus, abrogates SARS-CoV-2 infection (Khupse and Dixit 2020). However, this has not yet been confirmed.
Because the current trial began at the onset of the COVID-19 outbreak, patients were randomized to either the experimental or control group. Our assessments showed that the therapeutic benefits of celecoxib depended on the administrated dose. Hong et al. concluded that COVID-19 individuals could benefit from celecoxib adjuvant therapy, regardless of disease severity, and further decreases the mortality risk in the elderly and those suffering from comorbid conditions (Hong et al. 2020). Our observations were consistent with their findings, as the celecoxib administration enhanced immune system functioning within a week by elevating the WBC count.
Oral celecoxib can be a potential candidate for the in-patient or outpatient management of COVID-19. It is a comparatively safe and inexpensive NSAID, which is widely available around the world. It is easily accessible, reasonably priced, and has a well-documented long-term safety in children and adults with a long track record of medical use for a broad range of medical conditions. Still, there have been concerns regarding the adverse effects of celecoxib on the cardiovascular system. Celebrex's cardiac adverse effects have been explored in empirical investigation. However, some studies indicated that Celebrex is associated with a higher risk of serious cardiac events. Nonetheless, the increased risk of acute myocardial infarction (MI) following celecoxib therapy strongly correlates with the dose and duration of treatment (Masclee et al. 2018). It should be noted that cardiovascular toxicity is time-dependent, occurring primarily in patients with autoimmune diseases who continuously receive NSAIDs for months (Nissen et al. 2016), and the chances of developing acute MI are low following a week-long treatment with celecoxib. For the purpose of COVID-19 treatment, however, this should not be considered a significant disadvantage because the anticipated period of therapy will never exceed a few weeks (Catella-Lawson and Crofford 2001). Still, patients with overt cardiovascular comorbidities are advised to receive NSAID therapy at the discretion of their health consultants.
We did not measure blood levels of celecoxib. Moreover, the sample size in our study was relatively small, which can be considered a limitation. Nevertheless, we believe the present experiment provided a rationale for using celecoxib as an adjuvant to reduce the severity of COVID-19 and enhance the function of the immune system against SARS-CoV-2.
Conclusion and future perspectives
Taken together, upregulation of COX-2 is a well-established pathogenic mechanism involved in developing COVID-19. Celecoxib, a selective COX-2 inhibitor, could be considered a suitable candidate for treating mild to moderate COVID-19. Nonetheless, our experiment was not a well-planned, randomized, double-blind, and controlled clinical trial, which warrants further investigations on this particular subject.
Data availability
All data are available.
Abbreviations
- ACE2:
-
Angiotensin-converting enzyme 2
- ALT:
-
Serum alanine aminotransferase
- AST:
-
Aspartate aminotransferase levels
- ARDS:
-
Acute respiratory distress syndrome
- BMI:
-
Body mass index
- BRD:
-
Bromodomain proteins
- CCoV:
-
Canine coronavirus
- Celebrex:
-
Celecoxib
- COVID-19:
-
Coronavirus disease 2019
- COX-1:
-
Cyclooxygenase-1
- COX-2:
-
Cyclooxygenase-2
- CRP:
-
C-reactive protein
- CT:
-
Computed tomography
- ESR:
-
Erythrocyte sedimentation rate
- Hb:
-
Hemoglobin
- IL-6:
-
Interleukin 6
- iNOS/NO:
-
Inducible nitric oxide synthase/ nitric oxide
- MI:
-
Myocardial infarction
- NO:
-
Nitric oxide
- IRCT:
-
Iranian Registry of Clinical Trials
- NSAIDs:
-
Non-steroidal antiinflammatory drugs
- p38 MAPK:
-
P38 mitogen-activated protein kinases
- PGs:
-
Prostaglandins
- PGE2:
-
Prostaglandin E2
- PGI2:
-
Prostacyclin I2
- PGI2/TXA2:
-
Prostacyclin I2/thromboxane A2
- RBCs:
-
Red blood cells
- RT-PCR:
-
Reverse transcription-polymerase chain reaction
- SARS:
-
Severe acute respiratory syndrome
- SARS-CoV-2:
-
Severe acute respiratory coronavirus 2
- SpO2:
-
Blood oxygen saturation
- TNF-α:
-
Tumor necrosis factor-alpha
- TXA2:
-
Thromboxane A2
- VEGF:
-
Vascular endothelial growth factor
- WBC:
-
White blood cells
References
Abualhasan M, Zatar N, Shehab KA, Shraim N (2021) Tablet formulation of a synthesized celecoxib potassium salt and development of a validated method for its analysis. Curr Pharm Des 27(25):2872–2880
Al Saleh K, AlQahtani RM (2021) Platelet count patterns and patient outcomes in sepsis at a tertiary care center: beyond the APACHE score. Medicine 100(18):e25013
Al-Hakeim HK, Al-Hamami SA, Almulla AF, Maes M (2021) Increased serum thromboxane A2 and prostacyclin but lower complement C3 and C4 levels in COVID-19: associations with chest CT scan anomalies and lowered peripheral oxygen saturation. COVID 1(2):489–502
Amici C, Caro AD, Ciucci A, Chiappa L, Castilletti C, Martella V et al (2006) Indomethacin has a potent antiviral activity against SARS coronavirus. Antivir Ther 11(8):1021–1030
Broglio K (2018) Randomization in clinical trials: permuted blocks and stratification. JAMA 319(21):2223–2224
Catella-Lawson F, Crofford LJ (2001) Cyclooxygenase inhibition and thrombogenicity. Am J Med 110(3):28–32
Chan FK, Hung LC, Suen BY, Wong VW, Hui AJ, Wu JC et al (2004) Celecoxib versus diclofenac plus omeprazole in high-risk arthritis patients: results of a randomized double-blind trial. Gastroenterology 127(4):1038–1043
Chen J, Jiang L, Lan K, Chen X (2015) Celecoxib inhibits the lytic activation of Kaposi’s sarcoma-associated herpesvirus through down-regulation of RTA expression by inhibiting the activation of p38 MAPK. Viruses 7(5):2268–2287
Cioccarelli C, Angioni R, Venegas FC, Bertoldi N, Munari F, Cattelan A et al (2021) IL1β promotes TMPRSS2 expression and SARS-CoV-2 cell entry through the p38 MAPK-GATA2 axis. Front Immunol 12:781352. https://doi.org/10.3389/fimmu.2021.781352
de Bruin N, Schneider A-K, Reus P, Talmon S, Ciesek S, Bojkova D et al (2022) Ibuprofen, flurbiprofen, etoricoxib or paracetamol do not influence ACE2 expression and activity in vitro or in mice and do not exacerbate in-vitro SARS-CoV-2 infection. Int J Mol Sci 23(3):1049
DeKosky ST, Kochanek PM, Valadka AB, Clark RS, Chou SH-Y, Au AK et al (2021) Blood biomarkers for detection of brain injury in COVID-19 patients. J Neurotrauma 38(1):1–43
Dembo G, Park SB, Kharasch ED (2005) Central nervous system concentrations of cyclooxygenase-2 inhibitors in humans. J Am Soc Anesthesiol 102(2):409–415
Dutton LC, Dudhia J, Catchpole B, Hodgkiss-Geere H, Werling D, Connolly DJ (2018) Cardiosphere-derived cells suppress allogeneic lymphocytes by production of PGE2 acting via the EP4 receptor. Sci Rep 8(1):1–14
Eslamijouybari M, Heydari K, Maleki I, Moosazadeh M, Hedayatizadeh-Omran A, Vahedi L et al (2020) Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in COVID-19 patients and control group and relationship with disease prognosis. Caspian J Intern Med 11(Suppl 1):531
Feng X, Li S, Sun Q, Zhu J, Chen B, Xiong M, Cao G (2020) Immune-inflammatory parameters in COVID-19 cases: a systematic review and meta-analysis. Front Med 7:301
Ghaznavi H, Shirvaliloo M, Sargazi S, Mohammadghasemipour Z, Shams Z, Hesari Z et al (2022) SARS-CoV-2 and influenza viruses: strategies to cope with coinfection and bioinformatics perspective. Cell Biol Int 46(7):1009–1020. https://doi.org/10.1002/cbin.11800
Gimeno A, Mestres-Truyol J, Ojeda-Montes MJ, Macip G, Saldivar-Espinoza B, Cereto-Massagué A et al (2020) Prediction of novel inhibitors of the main protease (M-pro) of SARS-CoV-2 through consensus docking and drug reposition. Int J Mol Sci 21(11):3793
Grimm H, Kretzschmar J, Cook MD, Brown MD (2018) The effects of exercise, aspirin, and celecoxib in an atherogenic environment. Med Sci Sports Exerc 50(10):2033–2039
Heidari Nia M, Rokni M, Mirinejad S, Kargar M, Rahdar S, Sargazi S et al (2021) Association of polymorphisms in tumor necrosis factors with SARS-CoV-2 infection and mortality rate: a case–control study and in silico analyses. J Med Virol 94:1502–1512
Hong W, Chen Y, You K, Tan S, Wu F, Tao J et al (2020) Celebrex adjuvant therapy on coronavirus disease 2019: an experimental study. Front Pharmacol. https://doi.org/10.3389/fphar.2020.561674
Hosseinikhah SM, Barani M, Rahdar A, Madry H, Arshad R, Mohammadzadeh V, Cucchiarini M (2021) Nanomaterials for the diagnosis and treatment of inflammatory arthritis. Int J Mol Sci 22(6):3092
Khupse R, Dixit P (2020) Potential antiviral mechanism of hydroxychloroquine in COVID-19 and further extrapolation to celecoxib (Celebrex) for future clinical trials. Available at SSRN 3570102
Kim N, Lannan KL, Thatcher TH, Pollock SJ, Woeller CF, Phipps RP (2018) Lipoxin B4 enhances human memory B cell antibody production via upregulating cyclooxygenase-2 expression. J Immunol 201(11):3343–3351
Kuehl FA Jr, Egan RW (1980) Prostaglandins, arachidonic acid, and inflammation. Science 210(4473):978–984
Kwong K, Kollarik M, Nassenstein C, Ru F, Undem BJ (2008) P2X2 receptors differentiate placodal vs. neural crest C-fiber phenotypes innervating guinea pig lungs and esophagus. Am J Physiol-Lung Cell Mol Physiol 295(5): L858-L865
Lee SM, Cheung C-Y, Nicholls JM, Hui KP, Leung CY, Uiprasertkul M et al (2008) Hyperinduction of cyclooxygenase-2-mediated proinflammatory cascade: a mechanism for the pathogenesis of avian influenza H5N1 infection. J Infect Dis 198(4):525–535
Liu M, Yang Y, Gu C, Yue Y, Wu KK, Wu J, Zhu Y (2007) Spike protein of SARS-CoV stimulates cyclooxygenase-2 expression via both calcium-dependent and calcium-independent protein kinase C pathways. FASEB J 21(7):1586–1596
Lu G, Wang J (2020) Dynamic changes in routine blood parameters of a severe COVID-19 case. Clin Chim Acta 508:98–102
Masclee GM, Straatman H, Arfè A, Castellsague J, Garbe E, Herings R et al (2018) Risk of acute myocardial infarction during use of individual NSAIDs: a nested case-control study from the SOS project. PLoS ONE 13(11):e0204746
Morimoto K, Shirata N, Taketomi Y, Tsuchiya S, Segi-Nishida E, Inazumi T et al (2014) Prostaglandin E2–EP3 signaling induces inflammatory swelling by mast cell activation. J Immunol 192(3):1130–1137
Nissen SE, Yeomans ND, Solomon DH, Lüscher TF, Libby P, Husni ME et al (2016) Cardiovascular safety of celecoxib, naproxen, or ibuprofen for arthritis. N Engl J Med 375:2519–2529
Niwa H, Satoh T, Matsushima Y, Hosoya K, Saeki K, Niki T et al (2009) Stable form of galectin-9, a Tim-3 ligand, inhibits contact hypersensitivity and psoriatic reactions: a potent therapeutic tool for Th1-and/or Th17-mediated skin inflammation. Clin Immunol 132(2):184–194
Pieretti JC, Rubilar O, Weller RB, Tortella GR, Seabra AB (2021) Nitric oxide (NO) and nanoparticles–potential small tools for the war against COVID-19 and other human coronavirus infections. Virus Res 291:198202
Raaben M, Einerhand AW, Taminiau LJ, Van Houdt M, Bouma J, Raatgeep RH et al (2007) Cyclooxygenase activity is important for efficient replication of mouse hepatitis virus at an early stage of infection. Virol J 4(1):1–5
Robb CT, Goepp M, Rossi AG, Yao C (2020) Non-steroidal antiinflammatory drugs, prostaglandins, and COVID-19. Br J Pharmacol 177(21):4899–4920
Rojas-Carranza CA, Bustos-Cruz RH, Pino-Pinzón CJ, Ariza-Marquez YV, Gómez-Bello RM, Canadas-Garre M (2018) Diabetes-related neurological implications and pharmacogenomics. Curr Pharm Des 24(15):1695–1710
Säfholm J, Dahlén SE, Delin I, Maxey K, Stark K, Cardell LO, Adner M (2013) PG E2 maintains the tone of the guinea pig trachea through a balance between activation of contractile EP1 receptors and relaxant EP2 receptors. Br J Pharmacol 168(4):794–806
Salvemini D, Misko TP, Masferrer JL, Seibert K, Currie MG, Needleman P (1993) Nitric oxide activates cyclooxygenase enzymes. Proc Natl Acad Sci 90(15):7240–7244
Sharma J, Al-Omran A, Parvathy S (2007) Role of nitric oxide in inflammatory diseases. Inflammopharmacology 15(6):252–259
Singh S, Sharma R, Singh J, Jain K, Paul D (2021) Thrombocytopenia in COVID-19: focused summary of current understanding of mechanisms and clinical implications. J Pediatr Hematol Oncol 43(7):243–248
Sivasankarapillai VS, Pillai AM, Rahdar A, Sobha AP, Das SS, Mitropoulos AC et al (2020) On facing the SARS-CoV-2 (COVID-19) with combination of nanomaterials and medicine: possible strategies and first challenges. Nanomaterials 10(5):852
Smeitink J, Jiang X, Pecheritsyna S, Renkema H, van Maanen R, Beyrath J (2020) Hypothesis: mPGES-1-derived prostaglandin E2, a so far missing link in COVID-19 pathophysiology? https://doi.org/10.20944/preprints202004.0180.v1
Terrier O, Dilly S, Pizzorno A, Chalupska D, Humpolickova J, Bouřa E et al (2021) Antiviral properties of the NSAID drug naproxen targeting the nucleoprotein of SARS-CoV-2 coronavirus. Molecules 26(9):2593
Ukawa H, Yamakuni H, Kato S, Takeuchi K (1998) Effects of cyclooxygenase-2 selective and nitric oxide-releasing non-steroidal antiinflammatory drugs on mucosal ulcerogenic and healing responses of the stomach. Dig Dis Sci 43(9):2003–2011
Yan X, Hao Q, Mu Y, Timani KA, Ye L, Zhu Y, Wu J (2006) Nucleocapsid protein of SARS-CoV activates the expression of cyclooxygenase-2 by binding directly to regulatory elements for nuclear factor-kappa B and CCAAT/enhancer binding protein. Int J Biochem Cell Biol 38(8):1417–1428
Zamora CA, Baron DA, Heffner JE (1993) Thromboxane contributes to pulmonary hypertension in ischemia-reperfusion lung injury. J Appl Physiol 74(1):224–229
Funding
The protocol of the study was approved by the ethics committee of Zahedan University of Medical Sciences (Ethical code: IR.ZAUMS.REC.1399.197).
Author information
Authors and Affiliations
Contributions
All authors participated in the investigation, design, interpretation of the studies and analysis of the data and review of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The author(s) declare that they have conflict of interest.
Consent for publication
All authors are agreed.
Ethics statement
Webpage of ethical approval code is available at https://ethics.research.ac.ir/ProposalCertificateEn.php?id=149801&Print=true&NoPrintHeader=true&NoPrintFooter=true&NoPrintPageBorder=true&LetterPrint=true.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ghaznavi, H., Mohammadghasemipour, Z., Shirvaliloo, M. et al. Short-term celecoxib (celebrex) adjuvant therapy: a clinical trial study on COVID-19 patients. Inflammopharmacol 30, 1645–1657 (2022). https://doi.org/10.1007/s10787-022-01029-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-022-01029-4