Abstract
This research analyzes the cost-efficiency of the Patient Centered Medical Home (PCMH) model vis-à-vis the traditional care delivery model in the Federally Qualified Health Centers (FQHC). We apply the three-stage least squares modeling approach on 2014 UDS data on all FQHCs to estimate per-visit and per-patient cost functions. Log-quadratic and linear-quadratic functional forms of cost are used for the analysis. The estimated models reveal substantial scale economies and cost advantages associated with PCMH status. Aggregate cost-saving impact of PCMH across all FQHCs in 2014 is estimated to be $1.05 billion. Simulations reveal that the PCMH impact on cost savings grows with the size of the patient population. Reaching the full cost-saving potential in PCMH-recognized FQHCs hinges on expanding the health workforce at all levels of care to meet the need of the growing patient population due to aging and Medicaid expansion. For FQHCs that are not PCMH-recognized, capacity/infrastructural expansion appears to be the immediate policy choice.


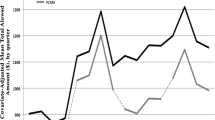
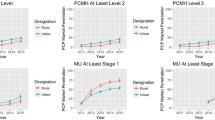
Source: Author's calculations based on simulated scenarios
Similar content being viewed by others
Notes
For more detailed description on FQHCs, reader may see HRSA official website at https://www.hrsa.gov/opa/eligibility-and-registration/health-centers/fqhc/index.html.
The focus variable in the study, PCMH status, being a binary variable, a longitudinal or panel study based on a number of years would not be possible. The reason is that the focus variable will drop out of the estimation equation for many health centers that do not change their status during the whole or part of the study period.
References
American Hospital Association (2012). American Hospital Association’s Physician Leadership Forum. Team-based health care delivery: Lessons from Field. Last Accessed on July 14, 2020. Available at: http://www.ahaphysicianforum.org/resources/leadership-development/team-based-care/team-delivery-report.pdf.
David, G., Saynisch, P. A., & Smith-McLallen, A. (2018). The economics of patient-centered care. Journal of Health Economics, 59(1), 60–77.
Day, J., Scammon, D.L., Sheet-Mervis, A., et al. (2013). Quality, satisfaction, and financial efficiency associated with elements of primary care practice transformation: Preliminary findings. Annals of Family Medicine, 11(1) (supplement): s50-s59.
DeVries, A., Li, C. H. W., Sridhar, G., Hummel, J. R., et al. (2012). Impact of medical homes on quality, healthcare utilization, and costs. American Journal of Managed Care, 18(9), 534–544.
Edwards, S. T., Bitton, A. H., J., , et al. (2014). Patient-centered medical home initiatives expanded in 2009–13: Providers, payments, and payment incentives increased. Health Affairs, 33(10), 1823–1831.
Fields, D., Leshen, E., & Patel, K. (2010). Driving quality gains and cost savings through adoption of medical homes. Health Affairs, 29(5), 819–827.
Friedberg, M. W., Lai, D. J., Hussey, P. S., & Schneider, E. (2009). A guide to the medical home as a practice-level intervention. American Journal of Managed Care, 15, S291–S299.
Geographic Cost Price Indices (2017). Geographic Price Cost Indices by Zip Code. Department of Labor, Office of the Workers’ Compensation Programs (OWCP). Last accessed on July 14, 2020. Available at: https://www.dol.gov/owcp/regs/feeschedule/fee/fee15/download.htm.
Greene, W.H. (2011). Econometric Analysis. Seventh Ed. Pearson, Chapter 15.
Goldberg, D.G., Mick, S.S., Kuzel, A.J., et al. (2013). Why do some primary care services engage in practice improvement efforts whereas others do not? Health Services Research, 48(2) (Part 1), 398–416.
Hasselt, M. V., McCall, N., Keyes, V., et al. (2015a). Total cost of care lower among Medicare Fee-for-Service beneficiaries receiving care from patient-center medical homes. Health Services Research, 50(1), 253–272.
Healthcare IT News (2011). 500 FQHCs receive $42M as part of PCMH demo project. Last accessed: July 14, 2020. Available at: http://www.healthcareitnews.com/news/500-fqhcs-receive-42m-part-pcmh-demo-project.
Health Resources and Services Administration (2014). Patient-centered medical/health home initiative update. Last accessed on June 5, 2019. Available at: http://bphc.hrsa.gov/qualityimprovement/clinicalquality/accreditation-pcmh/pcmhwebinar06162014.pdf.
Higgins, S., Chawla, R., Colombo, C., et al. (2014). Medical homes and cost and utilization among high-risk patients. American Journal of Medical Care, 20(3), 1–7.
Hoff, T., Weller, W., & DePuccio, M. (2012). The patient-centered medical home: A review of recent research. Medical Care Research and Review, 69(6), 619–644.
Kahn, K.L., Timbie, J.W., Friedbert, M.W., et al. (2015). Evaluation of CMS, FQHC, APCP Demonstration. Rand Corporation. Accessed on July 14, 2020. Available at: https://innovation.cms.gov/files/reports/fqhc-scndevalrpt.pdf.
Lewis, C., Coeman, A., Abrams, M. K., & Doty M. M. (2019). Role of Medicaid expansion in care delivery in community health centers, Commonwealth Fund, April 4, 2019. Accessed on July 14, 2020. Available at: https://www.commonwealthfund.org/publications/issue-briefs/2019/apr/role-medicaid-expansion-care-delivery-FQHCs.
News Release (2015). Health Resources and Services Administration. September 15, 2015. Accessed on July 14, 2020. Available at: http://www.hhs.gov/about/news/2015/09/15/hhs-awards-nearly-500-million-affordable-care-act-funding-health-centers-expand-primary-care.html.
News Release (2016). Health Resources and Services Administration. May 4, 2016. Accessed on July 14, 2020. Available at: http://www.hhs.gov/about/news/2016/05/04/hhs-awards-over-260-million-health-centers-nationwide-build-and-renovate-facilities-serve-more.html.
Nielsen, M, Buelt, L., Patel, K., and Nichols, L.M. (2016). The patient-centered medical home’s impact on cost and quality, Annual review of evidence 2014–15. Patient-Centered Primary Care Collaborative. Accessed on July 14, 2020. Available at: https://www.pcpcc.org/resource/patient-centered-medical-homes-impact-cost-and-quality-2014-2015.
Nocon, R. S., Sharma, R., Bimberg, J. M., et al. (2012). Association between Patient-centered medical home rating and operating cost at federally funded health centers. Journal of American Medical Association, 308(1), 60–66.
Nutting, P. A., Crabtree, B. F., Miller, W. F., et al. (2011). Transforming Physician Practices to Patient-Centered Medical Homes: Lessons from the National Demonstration Project. Health Affairs, 30(3), 439–445.
Paustian, M. L., Alexander, J. A., ElReda, D. K., et al. (2014). Partial and incremental PCMH practice transformation: Implication for quality and costs. Health Services Research, 49(1). Part, 1, 52–74.
Pines, J. M., Keyes, V., Hasselt, M. V., et al. (2015). Emergency department and inpatient hospital use by Medicare beneficiaries in patient-centered medical homes. Annals of Emergency Medicine, 65(6), 652–660.
Pulley, L. B., & Braunstein, Y. M. (1992). A Composite cost function for multiproduct firms with an application to economies of scope in banking. Review of Economics and Statistics, 74, 221–230.
Rosenthal, M. B., Beckman, H. B., Forrest, D. D., et al. (2010). Will the patient-centered medical home improve efficiency and reduce costs of care? A measurement and research agenda. Medical Care Research and Review, 20(10), 1–9.
Rosenthal, M. B., Friedbert, M. W., Singer, S. J., et al. (2013). Effect of multipayer patient-centered medical home on health care utilization and quality: The Rhode Island Chronic Care Sustainability Initiative Pilot Program. Journal of American Medical Association, Internal Medicine, 173(20), 1907–1913.
Timbie, J. W., Setoji, C. M., Kress, A., et al. (2017). Implementation of medical homes in federally qualified health centers. New England Journal of Medicine, 377(3), 246–256.
Ullrich, F. A., Mackinney, A. C., & Mueller, K. J. (2013). Are primary care practices ready to become patient-centered medical homes? The Journal of Rural Health, 29, 180–187.
Uniform Data System (2017). Uniform Data System (UDS) Resources, Health Resources and Services Administration. Last accessed on July 14, 2020. Available at: http://bphc.hrsa.gov/datareporting/reporting/index.html.
van Hasselt, M., McCall, N., Keys, V., et al. (2015b). Total cost of care lower among Medicare fee-for-service beneficiaries receiving care from patient-centered medical homes. Health Services Research, 50(1), 253–272.
Yoon, J., Chow, A., & Rubenstein, L. V. (2016). Impact of medical home implementation through evidence-based quality improvement on utilization and costs. Medical Care, 54(2), 118–125.
Acknowledgement
The author acknowledges with thanks the Fellowship support jointly by the Oak Ridge Associated Universities and Health Resources and Services Administration (HRSA). The author also acknowledges with thanks the support from George Zangaro at the Bureau of Health Workforce, HRSA for providing research support. Detailed comments on the paper by Suma Nair, Alek Sripipatana, and Sue Lin at the Bureau of Primary Health Care, HRSA, are acknowledged. The author would also like to thank the reviewer for detailed and constructive comments which improved the paper significantly. Data-related support provided by the Bureau of Primary Health Care, HRSA, is also acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The author declared no potential conflicts of interest with respect to the authorship and/or publication of this article.
Disclaimer
The views expressed in this article are solely the opinions of the author and do not necessarily reflect the official policies of the U.S. Department of Health and Human Services (HHS) or the Health Resources and Services Administration (HRSA) nor does mention of the names of HHS or HRSA imply endorsement by the U.S. Government.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Modeling framework
The practice establishments, because of their large sizes, locational advantages, better access to financial support for infrastructure development, or their leaderships’ motivation to improve quality and reduce costs may be more likely to implement PCMH capabilities. This is true in the case of FQHCs, since only a fraction of the health centers have competed and participated in the demonstration project. Some of the traits of such establishments may be observed and controlled in a multivariate econometric cost-function model. However, a sizable amount of such traits, such as leadership- and staff-level motivation, existing culture that drives patient-provider relationships, the level of access to external support, etc., may remain unobserved by the researcher. This phenomenon – commonly known as “selective program acceptance” makes the multivariate regression estimates, obtained using the OLS technique, biased, requiring application of the 3SLS technique for estimation of the cost function. The empirical model in this research attempts to address the “selectivity” or the “endogeneity” issue with an application of the 3SLS technique to estimate the cost function and thereby extricate the true effect of PCMH on cost.
The 3SLS technique involves estimation of the following four equations:
where.
y: average cost, which is either medical cost per medical visit or total cost per patient, it is either in logarithmic form or in linear form.
y1: PCMH status = 1, if the health center is PCMH-recognized, = 0, if not,
q: either total number of medical visits, or total number of patients served, in a year,
f: total FTE,
x: set of all exogenous variables used as control,
r: total revenue,
Statedummy: represents 50 state dummies, where the state Wyoming is left out of the regression and kept as the reference category,
\(\varepsilon_{1}\), \(\varepsilon_{2}\), \(\varepsilon_{3}\), and \(\varepsilon_{4}\): represent error terms,
\(\alpha\), \(\beta\), \(\gamma\), and \(\theta\): represent slope parameters of the system of equations.
The variables \(y\), \(y_{1}\), \(y_{1} q\), \(y_{1} q^{2}\) are endogenous variables, all other variables are treated as exogenous to the system. The exogenous instrumental variables are the ones that are not included in the primary equation (A1). Specifically, the variable representing total revenue it square, and all the state dummies represent instrumental variables in the above system.
The variable “total revenue” serves as a good instrumental variable in the cost-function estimation, since higher revenue is associated with a larger size of the practice establishment and consequently, it can be highly correlated with the PCMH status. At the same time, because of the exclusion restriction provided by the economic theory, it cannot be a determinant of cost.24 However, in order to make the instrument more powerful, instead of using the total revenue for the year 2014, we take the average of the total revenue pertaining to year 2014 and the three immediately prior years. The state-specific dummies in the three equations are also powerful exogenous instruments. They represent many unobserved factors that affect participation of the PCMH program, such as the prevailing scope-of-practice laws, unobserved cultural and socioeconomic factors that determine a health center’s decision to participate in the PCMH initiative. This makes state dummies as a group and the PCMH status highly correlated, as desired. On the other hand, since we already have the cost figures regionally adjusted using Geographic Price Cost Indices, there will be very weak association between costs and state dummies, as desired.
The exogenous variables, total FTE and its square deserve special mention as they appear on both primary cost equation as well as in the other three equations. Total FTE reflects the size of the establishment and thus, it can affect the average cost. Also, since large size establishments are more likely to have the PCMH status, total FTE is a determinant of the PCMH status. Moreover, among the practice establishments with the PCMH status there can be relative inefficiencies as it takes a long time to take the full impact of the PCMH to kick in. Thus, it is possible that the average cost will increase with the size of the establishment, as measured by total FTE, but at a decreasing rate. Therefore, we expect the coefficient on the variable total FTE to be positive, but the coefficient on its square to be negative in the primary equations of the “Visit Model” as well as the “Patient Model”.
Economies of scale
Slope of the average cost \(= \frac{\partial y}{{\partial q}} = \beta_{21} + 2\beta_{22} q + \delta_{11} y_{1} + 2\delta_{12} y_{1} q\).
If \(y_{1} = 1\), that is, if the health center has the PCMH status:
If \(y_{1} = 0\), that is, if the health center does not have the PCMH status:
Slope of the average cost
A negative slope of the average cost curve in (A5) and (A6) will reflect economies of scale.
Service provided at the lowest average cost
The lowest average cost occurs when the U-shaped average cost curve has slope zero.
If \(y_{1} = 1\), that is, if the health center has the PCMH status, lowest cost occurs when
If \(y_{1} = 0\), that is, if the health center does not have the PCMH status, lowest cost occurs when
The expressions (A7) and (A8) are utilized in the study to compute the number of medical visits and the number of patients served at the lowest cost.
Computation of marginal effects
The pure PCMH effect can be obtained using the following steps:
Step 1: Plug in the value of \(y_{1} = 1\) and in the cost function, keeping all else the same.
Step 2: Plug in the value of \(y_{1} = 0\) and in the cost function, keeping all else the same.
Step 3: Subtract the value of the cost function obtained in step 2 from the that in step 1.
Step 1:
Step 2:
Subtracting (A10) from (A9) yields the pure effect of PCMH as follows:
Step 3:
The expression (A11) is used to compute the cost impact of PCMH for the 2014 data.
Simulation Steps
Multiply \(q\) (patient population) by 1.10, 1.20, 1.30,……, 1.90, and 2.00 in the expression (A11) in order to obtain the pure effect of PCMH for a hypothetical 10%, 20%, 30%,……, 90%, and 100% increase, respectively, in the “Patient Model”.
Rights and permissions
About this article
Cite this article
Chattopadhyay, S. Cost-efficiency in the patient centered medical home model: New evidence from federally qualified health centers. Int J Health Econ Manag. 21, 295–316 (2021). https://doi.org/10.1007/s10754-021-09295-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10754-021-09295-5