Abstract
A simultaneous increase in the prevalence of diabetes mellitus (DM), a risk factor for cardiovascular diseases (CVDs), has contributed to the escalation of CVD related mortalities. To date, oxidative stress and inflammation are increasingly recognized as significant drivers of cardiovascular complications in patients with diabetes. Therefore, this study aims to explore the correlation between oxidative stress, inflammation, and hematological indices in diabetic patients with CVDs. Patients were allocated into five groups: healthy controls; nondiabetic patients with myocardial infarction; diabetic patients with myocardial infarction; nondiabetic patients with heart failure; and diabetic patients with heart failure. The results revealed that the malondialdehyde levels were increased; whereas superoxide dismutase enzyme activities were markedly reduced in all CVD groups compared with those of healthy controls. Although the mRNA expression levels of interleukin (IL)-6, IL-18, and IL-38 were significantly increased, those of the anti-inflammatory cytokine, IL-35, have been reduced in all CVD groups compared with healthy controls. Regarding hematological indices, hematocrit, red blood cell distribution width, mean platelet (PLT) volume, plateletcrit, PLT distribution width, leukocyte count, and PLT-to-lymphocyte and neutrophil-to-lymphocyte ratios were markedly increased in the diabetic and nondiabetic CVD groups compared with those of the healthy controls. Oxidative stress and cytokine biomarkers may play a significant role in the complications of diabetic cardiomyopathy. Moreover, hematological indices are particularly sensitive to systemic inflammatory changes and are novel markers for the early detection of diabetic cardiomyopathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Diabetes mellitus (DM) is a global health issue and is concomitant with cellular, metabolic, and blood cell abnormalities [1]. The American Heart Association regards diabetes as one of the key risk factors for cardiovascular diseases (CVDs) [2]. DM is often accompanied by cardiovascular disturbances, including coronary artery disease (CAD) and peripheral artery disease. Diabetes-induced pathological disorders may cause tissue damage in one-third to one-half of people with diabetes [3].
Oxidative stress is an imbalance in reactive oxygen species (ROS) and antioxidant defense mechanisms [4]. Cardiovascular insulin resistance, diabetic cardiomyopathy, and heart failure are accelerated by oxidative stress [5]. Recently, hypertriglyceridemia was demonstrated to increase CVD-related deaths in patients with diabetes [6]. According to human and animal studies, hyperglycemia may trigger an inflammatory response through oxidative pathways, which results in cardiac fibrosis and cardiomyocyte death, followed by cardiac dysfunction [7]. Indeed, inflammation, which is common in diabetes, can impact cardiomyocyte contractility and survival through various mechanisms, such as peroxynitrite formation and alterations in the extracellular matrix composition; dynamics are hypothesized to contribute to cytokine-induced cardiac contractile failure [8]. Interleukin (IL)-6 plays a vital role in the pathophysiology of CVD and its complications. Different immune responses and susceptibility to CAD are produced by genetic differences in IL-6 [9]. IL-38, a recently revealed member of the IL-1 cytokine family with anti-inflammatory activity, is generally recognized as a key regulator of inflammation. IL-38 is commonly expressed in the heart, and IL-38 polymorphisms are associated with coronary artery syndrome [10]. Moreover, IL-35, an anti-inflammatory cytokine, is involved in various disorders, including CVD and diabetes [11]. Hematological alterations in diabetes may occur due to ROS production as a consequence of long-term hyperglycemia [12]. Excessive ROS production causes oxidative stress, which leads to tissue damage and hematological alterations, including endothelial dysfunction, platelet (PLT) hyperactivity, and red blood cell (RBC) dysfunction [13]. Hematological alterations have been encountered in patients with DM, including alterations in the structure, function, and metabolism of PLT, RBC, white blood cell (WBC), and the coagulation system [12].
The role of inflammation in diabetic CVD has been recently reported; however, its mechanism requires more exploration. In particular, the interplay between DM-induced inflammation and hematological disorders in the risk of CVD requires further investigation. Therefore, this study aims to explore the relationship between oxidative stress, inflammation, and alteration in hematological indices and the risk of developing diabetic cardiomyopathy.
MATERIALS AND METHODS
Study Population
A total of 120 patients with both myocardial infarction (diabetic type 2 and nondiabetic) and heart failure (diabetic type 2 and nondiabetic) who visited the Cardiac and Chest Intensive Care Unit of Beni-Suef University Hospital (Beni-Suef, Egypt) were enrolled in this cross-sectional study. The data was collected using a paper questionnaire and clinical laboratory reports. Eligible patients were allocated into four groups based on the clinical and biochemical investigations. Moreover, thirty normal healthy participants were selected as healthy controls. Moreover, all patients provided a written consent and blood samples during the period from March 2019 to November 2019 following protocol approval by the Beni-Suef University Hospital Ethics Committee (BNS/2019/2).
Inclusion and Exclusion Criteria and Experimental Design
The adult patients (males, 72; females, 78; aged 40–70 years), including healthy controls, diabetic and nondiabetic patients with heart failure, and diabetic and nondiabetic patients with myocardial infarction, were enrolled in this study (Fig. 1). The healthy subjects consisted of participants who had no significant health-related issues. All participants (healthy controls and patients) were free of asthma symptoms, alcohol abuse, infectious diseases, allergies, kidney failure, eczema, thyroid diseases, autoimmune disorders, and liver dysfunction.
Biochemical Investigations
After overnight fasting, blood samples were collected in sodium fluoride, ethylenediaminetetraacetic acid (EDTA), and plain tubes (5 mL each). The EDTA blood samples were used to estimate complete blood count and glycated hemoglobin (HbA1c). Samples were stored at − 40 °C until use. Sodium fluoride tubes were used to collect blood samples to determine fasting blood sugar (FBS) level. Plasma FBS and serum cholesterol, high-density lipoprotein (HDL), and triglycerides levels were assessed using a reagent kit (Spinreact Co., Spain). Subsequently, low-density lipoprotein (LDL) and very low-density lipoprotein (vLDL) levels were calculated based on the formula of Friedewald et al. [14]. Cardiovascular risks (1 and 2) were calculated following the formula of Ross [15]. The HbA1c level was determined using a reagent kit (Stanbio Laboratory, TX, USA). Furthermore, serum insulin was assessed using radioimmunoassay kits (Diagnostic Products Corporation, LA, USA). Homeostatic model assessment for insulin resistance (HOMA-IR) values was calculated using the following equation: HOMA-IR = fasting insulin (U/L) × fasting glucose (mg/dL)/405 [16]. The C-reactive protein (CRP) was estimated using a reagent kit (Spinreact Co., Spain). Serum CK-MB and troponin I levels were determined using test kits (HUMAN, Germany). Moreover, malondialdehyde (MDA) levels and superoxide dismutase (SOD) activities were determined using a reagent kit (BioVision, Milpitas, CA, USA). Hematology parameters, including hemoglobin, RBCs, hematocrit, mean corpuscular hemoglobin, mean corpuscular hemoglobin content, mean corpuscular volume, RBC distribution width (RDW), PLT count, plateletcrit (PCT), PLT distribution width (PDW), mean PLT volume (MPV), WBC count, and differential leukocyte count, were determined using a MICROS ABX autoanalyzer. All procedures were performed following the kit manufacturers’ instructions.
Real-Time Polymerase Chain Reaction
RNA was isolated from the blood samples using a GeneJET™ RNA purification kit (Thermo Fisher Scientific Inc., Rochester, NY, USA). RNA was purified and spectrophotometrically quantified. Consequently, the target DNA cDNA was amplified using GoTaq Green Master Mix (Promega, WI, USA) using the following sets of primers: 5ˋ-GGTACATCCTCGACGGCATCT-3ˋ (forward primer) and 5ˋ-GT GCCTCTTTGCTGCTTTCAC-3ˋ (reverse primer) for IL-6, 5ˋ -GCTTCCTCTCGC AAC AAA C-3ˋ(forward primer) and 5ˋ -CACTTCACAGAGATAGTTACAGCC-3ˋ(reverse primer) for IL-18, 5ˋ-TGTTCTCCATGGCTCCCTA-3ˋ(forward primer) and 5ˋ-TTATGAAAGGCACGAAGCTG-3ˋ(reverse primer) for IL-35, 5ˋ- AAGAAGGACCTCCGGCTCT -3ˋ(forward primer) and 5ˋTGACTCAGAATCTGGC5GTATTTC-3ˋ (reverse primer) for IL-38, and 5ˋ- TCACCCTGAAGTACCCCATGGAG-3ˋ(forward primer) and 5ˋ TTGGCCTTGGGGTTCAGGGGG -3ˋ (reverse primer) for β-actin. Green Master Mix (Promega, WI, USA) and T100TM thermal cycler (Bio-Rad Laboratories, CA, USA) were used for PCR under the following conditions: initial denaturation at 95 °C for 5 min, 35 cycles set at 95 °C (1 min) for denaturation, 60 °C (1 min) for annealing, and 72 °C (1 min) for extension, and ultimately at 72 °C (5 min) to finish the extension reaction. Values were normalized to the quantity of β-actin. All molecular assays were conducted at the Molecular Biology Laboratory of CliniLab (Cairo, Egypt).
Statistical Analysis
Results were presented as mean values and SEM. Shapiro–Wilk normality test showed that the data were not normally distributed, and thus a non-parametric Kruskal–Wallis test followed by the post hoc test using a pairwise multiple-comparative analysis was used to determine the statistical differences between groups using a computer software package (SPSS version 20, IBM Corp., 2011). A simple linear correlation study was conducted using Spearman’s correlation analysis to estimate the degree of the relationship between the variables. A P value < 0.05 was considered statistically significant.
RESULTS
The results revealed that the body mass index values were significantly higher (p < 0.001) in all CVD patient groups compared with the healthy control group. Meanwhile, all patient groups showed a significant (p < 0.001) increase in systolic and diastolic blood pressures compared with the healthy control group. Moreover, the diabetic myocardial infarction and diabetic heart failure groups showed a significant (p < 0.001) increase in the FBS level compared with the nondiabetic myocardial infarction, nondiabetic heart failure, and healthy control groups. However, the diabetic CVD groups exhibited a significant (p < 0.001) decline in the insulin level compared with the nondiabetic CVD and healthy control groups. The diabetic myocardial infarction and diabetic heart failure groups revealed a significant (p < 0.001) increase in HbA1c% and HOMA-IR values compared with the nondiabetic CVD and healthy control groups. All CVD patient groups showed a highly significant (p < 0.001) increase in serum CK-MB and troponin I levels compared with the healthy control group, with a marked increase in both myocardial infarction groups (Table 1).
Regarding lipid profile results, all CVD groups exhibited a significant (p < 0.001) increase in serum triglycerides, cholesterol, LDL-c, and vLDL-c levels, as well as cardiovascular risks 1 and 2 values, than healthy controls. However, HDL and anti-atherogenic index values showed a notable (p < 0.001) reduction in the diabetic CVD groups compared with those in the nondiabetic CVD and healthy control groups (Fig. 2).
The changes in the values of A cholesterol, B HDL, C LDL, D triglycerides, E vLDL F risk factor 1, G risk factor 2, and H anti-atherogenic index among healthy controls, myocardial infarction (non-diabetic and diabetic), and heart failure (non-diabetic and diabetic) groups. Mean values and SEM are represented. A non-parametric Kruskal–Wallis test followed by the post hoc test using a pairwise multiple-comparative analysis was used to determine the statistical difference between groups, *p < 0.05, **p < 0.01, ***p < 0.001 as compared to healthy control and with #p < 0.05, ##p < 0.01 as compared with non-diabetic groups. N.S. was not significant. LDL, low-density lipoprotein cholesterol; HDL, high-density lipoprotein cholesterol; vLDL, very low-density lipoprotein cholesterol.
The expression of pro-inflammatory markers, IL-6, IL-18, and IL-38 showed a significant (p < 0.001) upregulation in CVD groups compared with those in the healthy control group and exhibited a significant increase in diabetic patients with CVD compared with that in nondiabetic CVD patients. In contrast, the diabetic and nondiabetic CVD groups showed a highly significant (p < 0.001) downregulation in the IL-35 mRNA expression compared with the healthy control group, with lower levels in diabetic patients than that in nondiabetic CVD patients. All CVD patient groups exhibited a highly significant (p < 0.001) increase in serum CRP levels compared with the healthy control group. Regarding oxidative stress markers, the CVD patient groups showed a highly significant (p < 0.001) increase in MDA levels and a remarkable (p < 0.001) decline in SOD levels compared with the healthy control group. However, the MDA levels exhibited a significant (p < 0.01) increase in the diabetic CVD patient groups compared with those in the healthy control group. Furthermore, SOD levels were significantly decreased (p < 0.05) in CVD diabetic groups than in CVD non-diabetic groups (Fig. 3).
The changes in the values of A IL-6, B IL-18, C IL-35, D IL-38, E CRP, F MDA, and G SOD among healthy controls, myocardial infarction (non-diabetic and diabetic), and heart failure (non-diabetic and diabetic) groups. Mean values and SEM are represented. A non-parametric Kruskal–Wallis test followed by the post hoc test using a pairwise multiple-comparative analysis was used to determine the statistical difference between groups, *p < 0.05, **p < 0.01, ***p < 0.001 when compared to healthy control and with #p < 0.05, ##p < 0.01, ###p < 0.001 when compared with non-diabetic groups. N.S. was not significant. IL, interleukin; MDA, malondialdehyde; SOD, superoxide dismutase; C-RP, C-reactive protein.
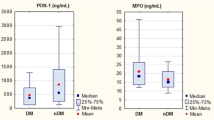
In the present study, both heart failure patient groups exhibited a significant decrease in the hemoglobin content, RBC count, and hematocrit values compared with the healthy control group (Table 2). Moreover, the heart failure patient groups revealed a significant (p < 0.001) increase in RDW% compared with the healthy control group. Additionally, all CVD patient groups displayed a significant (p < 0.001) increase in PDW% compared with the healthy control group (Fig. 3). Regarding PLT indices, the diabetic heart failure group displayed a significant (p < 0.05) increase in the PLT count compared with the healthy control group (Table 2), whereas all CVD patient groups revealed a marked increase in MPV values, except for the diabetic myocardial infarction group, compared with the healthy control group. Meanwhile, the diabetic CVD patient groups showed a marked (p < 0.05) increase in PCT% compared with the healthy control and nondiabetic groups (Fig. 4).
The changes in the values of A RDW%, B MPV, C PCT%, D PDW%, E N/L ratio, F L/M ratio, and G P/L ratio among healthy controls, myocardial infarction (non-diabetic and diabetic), and heart failure (non-diabetic and diabetic) groups. Mean values and SEM are represented. A non-parametric Kruskal–Wallis test followed by the post hoc test using a pairwise multiple-comparative analysis was used to determine the statistical difference between groups, *p < 0.05, **p < 0.01, ***p < 0.001 when compared to healthy control and with #p < 0.05 when compared with non-diabetic groups. N.S. was not significant. PDW, platelets distribution width; RDW, red distribution width; PCT, plateletcrit; MPV, mean platelets volume; N/L, neutrophil/lymphocyte, N/L, lymphocyte/monocyte; P/L, platelets/lymphocyte.
The WBC count increased significantly (p < 0.001) in all CVD patient groups, except for the diabetic heart failure group, compared with that in the healthy control group (Table 2). However, the neutrophil count exhibited a significant increase in all CVD patient groups compared with that in the healthy control group. Conversely, the lymphocyte count showed a remarkable decline in all CVD patient groups compared with that in the healthy control group (Table 2). Concerning PLT-to-lymphocyte (P/L) and neutrophil-to-lymphocyte (N/L) ratios, the results showed a noticeable increase in all CVD patient groups compared with those in the healthy control group. Additionally, the P/L and N/L ratios exhibited remarkable increases in the diabetic CVD patient groups compared with those in the nondiabetic CVD patient groups. However, the lymphocyte-to-monocyte (L/M) ratio revealed a significant decrease in both myocardial infarction patient groups compared with that in the healthy control group, with a remarkably high decrease in the diabetic myocardial infarction patient group (Fig. 4).
In the diabetic CVD groups, HbA1c% displayed a significant positive correlation with IL-6, IL-18, IL-38, MDA, and PDW%, whereas a negative correlation was detected with IL-35 and SOD. In addition, CK-MB exhibited a significant positive correlation with IL-6, IL-18, IL-38, MDA, PDW%, and P/L and N/L ratios, whereas a significant negative correlation was observed with IL-35 and SOD. Moreover, the anti-atherogenic index demonstrated a significant positive correlation with IL-36 and SOD, whereas a significant negative correlation was observed with IL-6, IL-18, IL-38, MDA, PDW%, PCT%, and P/L and N/L% ratios (Table 3).
DISCUSSION
After controlling for inflammatory markers and classical risk factors, patients with diabetes had almost twice the risk of cardiovascular mortality compared with those without diabetes [1]. Furthermore, the increase in the number of patients with T2DM highlights the necessity of early CVD detection in patients with diabetes [6]. Thus, this study was anticipated to explore the interplay of DM-induced oxidative stress and inflammation with hematological abnormalities in CVD risk.
In our study, the myocardial infarction and heart failure groups exhibited a significant increase in serum cholesterol, triglyceride, LDL, vLDL-c levels, and risks factors 1 and 2, compared with the healthy control group. However, HDL levels and the anti-atherogenic index showed a notable reduction in the diabetic CVD groups compared with those in the nondiabetic CVD and healthy control groups. High glucose levels and dyslipidemia are complicated in atherosclerosis pathogenesis that eventually leads to CVD deaths. Chronic inflammation is one of the leading causes of atherosclerosis development [17]. The increase in serum CK-MB, troponin I, and lipid profile markers, including risks factors 1 and 2, confirmed the cardiac dysfunction of patients with diabetes, which leads to exploring diabetes cardiomyopathy complications.
In this study, MDA displayed a significant increase in the CVD patient groups with a marked elevation in the diabetic groups compared with the healthy control and nondiabetic groups. At the same time, SOD levels exhibited a remarkable decline in all CVD groups with a significant decrease in diabetic patients with CVD compared with those in the healthy control nondiabetic groups. Our results revealed a significant correlation among both MDA and SOD and HbA1c, CK-MB, and the anti-atherogenic index, indicating that dyslipidemia- and hyperglycemia-associated oxidative stress may induce the development of diabetic cardiomyopathy complications. These results are consistent with the study of Fathelbab et al. [18] in which it was observed that MDA levels were significantly increased in diabetic patients with CVD, and SOD levels in the diabetic CVD group were significantly reduced compared with those in the control group, indicating the role of oxidative stress-mediated tissue injury in diabetic patients with CVD. Moreover, a marked reduction in all antioxidant enzymes was observed, including SOD, in patients with metabolic syndrome (patients with dyslipidemia, hypertension, and T2DM) compared with the healthy controls [19]. Oxidative stress in heart failure occurs as a consequence of the excessive ROS production that can enhance lipid peroxidation and oxidize proteins to inactive states and cause DNA damage [20]. In addition, high ROS production may trigger maladaptive signaling pathways, which results in cell death and promotes abnormal cardiac remodeling, ultimately leading to diabetic cardiomyopathy-related functional abnormalities [21]. SOD is a member of the metalloproteinase family, and its overproduction is related to hypertension, diabetes, and CVD [22]. Additionally, SOD decline was associated with endothelial dysfunctions and hypertension [19]. When acute myocardial infarction occurs, it almost reduces SOD’s ability to scavenge free radicals. Increased MDA levels, followed by ROS accumulation, resulted in acute myocardial infarction [23]. Moreover, low antioxidant enzyme levels led to excessive insulin resistance that enhanced stress-related pathways, leading to diabetic cardiovascular events [24].
CVD is an inflammatory condition, whereas CRP is an acute-phase protein. Notably, clinical studies have demonstrated that CRP is a predictor of CVD [25] and associated complications [26]. The current study showed that all CVD groups (myocardial infarction and heart failure) exhibited higher CRP levels compared with the healthy controls. Moreover, CVD groups with diabetes had higher CRP levels than the corresponding normoglycemic groups. Furthermore, our results suggest a strong correlation between inflammatory cytokines and oxidative biomarkers in diabetic CVD groups. Our results are consistent with the results of previous studies, which declared that CRP is a novel marker for predicting CVDs in patients with diabetes mellitus [27]. Thus, our findings indicate that diabetes may worsen inflammatory responses and oxidative stress and could contribute to adverse outcomes in CVD.
Notably, the current data found a strong correlation between pro-inflammatory cytokines (IL-6, IL-18, and IL-38) and HbA1c, CK-MB, and anti-atherogenic index biomarkers. Additionally, the results showed that IL-6, IL-18, and IL-38 mRNA expressions exhibited a significant upregulation in the diabetic and nondiabetic CVD groups compared with those in the healthy control group, with a highly significant increase in diabetic patients with CVD. Cytokines, TNF-α, IL-1β, and IL-6, were found to be elevated in patients with heart failure, and their higher levels appear to be directly related to LVEF dysfunction [28]. Myocardial damage, heart failure, and mortality are linked to high levels of circulating IL-6 during and immediately after an acute myocardial infarction [29]. IL-6 levels in patients with left ventricular diastolic dysfunction (LVDD) were found to be substantially linked with the levels of fibrotic parameters, suggesting that IL-6 may play a role in increasing myocardial fibrosis and LV remodeling, finally leading to LVDD [30].
IL-18 is a pro-inflammatory cytokine that is predominantly produced by macrophages and binds to its receptor on the membranes of endothelial cells, lymphocytes, and smooth muscle cells to cause the production of interferon gamma, endothelial dysfunction, and plaque instability [31]. Our results are consistent with the results of Xiao et al. [32] in which it was revealed that increased IL-18 levels have been related to an increased risk of CVD. Several studies found that IL-18 was considerably higher in the plasma of patients who had coronary events [33], which agrees with our results. Notably, continued IL-18 suppression by IL-18-binding protein leads to cardiac fibrosis reduction and NF-κB phosphorylation, diastolic function improvement, electrical remodeling normalization, and IL-18-mediated ventricular tachycardia reduction in mice [34]. The IL-38 mRNA expression was upregulated in the mouse heart following myocardial infarction and exhibited a decrease in dendritic cell–mediated immune response [35]. Consequently, targeting IL-38 may hold new therapeutic approaches in the treatment of patients with myocardial infarction.
Moreover, our data demonstrated a correlation among IL-35 and HbA1c, CK-MB, and anti-atherogenic index biomarkers; it may be a novel therapeutic target in patients at risk for diabetic CVD. IL-35 has been linked to several cardiovascular disorders, including atherosclerosis and viral myocarditis [36]. IL-35 reduces doxorubicin-induced heart damage by increasing STAT3 signaling, lowering oxidative stress, and blocking mitochondrial-related apoptotic pathways [37]. The abovementioned studies are consistent with our study, showing a significant decrease in IL-35 levels in the CVD patient groups compared with those in the healthy control group. IL-35 can reduce myocardial ischemia/reperfusion (I/R) dysfunction by reducing mtROS. Furthermore, it was believed that IL-35 protects cardiomyocytes by inhibiting apoptosis, thereby minimizing cardiac I/R injury [38].
Furthermore, anemia is related to microvascular complications, diabetic nephropathy, neuropathy, and CVD [39]. HB content, RBCs count, and HCT% exhibited a significant decrease in CVD groups compared with healthy controls. Moreover, RBCs of a patient with diabetes combined more willingly, thereby augmenting whole blood viscosity and harming the microcirculation, finally leading to microangiopathy [40]. Moreover, all CVD patient groups revealed a significant increase in PDW% compared with the healthy control group. A high RDW is a disease severity metric associated with a variety of adverse outcomes, including CV and non-CV death, in patients with T2DM who have recently had an acute coronary syndrome [41]. Despite the completely unclear mechanisms between the RDW and adverse health consequences, it was recommended that it might be associated with the increase in ROS and pro-inflammatory cytokine levels [42].
PLTs are essential for maintaining normal homeostasis, and MPV is the indicator of their function. PLTs play a substantial role in atherosclerosis development and acute thrombotic cardiovascular event progression [43]. Our findings of higher MPV among patients with T2DM are consistent with those of several studies [44] that reported that the diabetic CVD group showed a significant increase in MPV compared with the healthy group. Elevated MPV has been seen in diabetic patients with retinopathy, nephropathy, and coronary heart disease; it represents alterations in PLT stimulation or PLT production rate [45]. PDW is a specific PLT reactivity biomarker that can help predict CVD [46], which is consistent with our study that showed that the CVD group showed a significant increase in PDW compared with the healthy control group. In our study, the CVD groups showed a significantly increased PCT% compared with the healthy control group. PLTs release various mediators, including thromboxanes, which can cause inflammation; increased PCT levels at the time of admission have been linked to poor long-term outcomes in patients with myocardial infarction [47].
WBCs are a biological systemic inflammation indicator, and an increased WBC count is linked to an increased risk of CAD, mortality rate, and stroke [48]. In this study, the CVD groups demonstrated a significant elevation in the neutrophil count compared with the healthy control group. The current results revealed that CK-MB and the anti-atherogenic index exhibited a positive correlation with the P/L and N/L ratios. Neutrophils are leukocytes that serve as the first line of defense against pathogens and damages caused by inflammation. The increase in neutrophil blood count has been linked to the severity of coronary damage and the prevalence of heart failure [49]. Lymphocytes reflect a calm and controlled immune response that causes less cardiac damage; lymphocyte levels decrease as apoptosis increases. In individuals with chronic heart failure, a low blood lymphocyte count has been linked to worse cardiovascular outcomes [50].
Recently, PDW, MPV, and N/L and P/L ratios were identified as microvascular diabetic issue indicators and announced as novel inflammatory biomarkers in cardiac diseases. The results of the previous studies [51, 52] are consistent with the results of our study, revealing that the N/L ratio had a significant increase in the CVD groups compared with that in the healthy control group. The N/L ratio, a simple, inexpensive, and innovative inflammatory biomarker, was shown to be higher in patients with diabetes and was related to poor glycemic control and may be prognostic predictors in cardiovascular events [53]. In patients with heart failure, neutrophilia, lymphopenia, and a higher N/L ratio have been linked to heart failure severity [54].
Additionally, our results showed that the N/L, L/M, and P/L ratios beside MPV, PDW, and PCT% were considered novel inflammatory biomarkers, confirming that the impaired hematological indices are one of the diagnostic markers in the development of diabetic cardiomyopathy. Also, the P/L and N/L ratios exhibited remarkable elevations in the diabetic CVD patient groups compared with those in the nondiabetic CVD patient groups. The P/L ratio is significantly and independently linked with the occurrence of in-hospital severe adverse cardiovascular events as a novel inflammatory marker. In patients with acute myocardial infarction, there was additional evidence of a link between the P/L ratio and long-term prognoses [55]. Additionally, the combination of the N/L and P/L ratios had both short- and long-term predictive significance [56]. These previous studies [55, 56] agree with our study, which reported a significant increase in the P/L ratio in the CVD groups compared with that in the healthy control group. Moreover, our findings revealed that the CVD groups exhibited a significant decrease in the L/M ratio compared with the healthy control group. These findings were consistent with those of [57] which reported that the L/M ratio was also linked to the prognosis of individuals with myocardial infarction, heart failure, and stable CAD. Notably, a lower L/M ratio is linked to a higher frequency of unstable angina pectoris or myocardial infarction in patients with CVD. Furthermore, the L/M ratio is an independent indicator of heart failure re-hospitalization in patients with CVD [58]. The study had some limitations, however, including the sample size and separation of the results based on age, sex, and disease duration. Moreover, this study lacks data on physical activity, drug use, and the serum protein levels of the tested cytokines.
In conclusion, our findings suggest a possible association of an oxidative stress represented by excess of MDA production and reduced SOD activity, and inflammatory state represented by increased mRNA expressions of the pro-inflammatory cytokines, IL-6, IL-18, and IL-38 and reduced expression of anti-inflammatory IL-35, and the progression of the diabetic cardiovascular diseases. Moreover, impaired hematological indices, including RDW, PLT, PDW%, PDW, PCT%, and N/L, L/M, and P/L ratios, were associated with the development of diabetic cardiomyopathy. Hematological indices are particularly sensitive to systemic inflammatory changes and may be novel markers for predict the progression of diabetic CVD.
Data Availability
All data generated or analyzed during this study are included in the article.
References
Daryabor, G., M.R. Atashzar, D. Kabelitz, S. Meri, and K. Kalantar. 2020. The effects of type 2 diabetes mellitus on organ metabolism and the immune system. Frontiers in Immunology 11: 1582.
Arnett, D.K., R.S. Blumenthal, M.A. Albert, A.B. Buroker, Z.D. Goldberger, E.J. Hahn, et al. 2019. ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology 74: 1376–1414.
Bharath, L.P., J.D. Rockhold, and R. Conway. 2021. Selective autophagy in hyperglycemia-induced microvascular and macrovascular diseases. Cells 10: 2114.
Zhou, Y., D.D. Murugan, H. Khan, Y. Huang, and W.S. Cheang. 2021. Roles and therapeutic implications of endoplasmic reticulum stress and oxidative stress in cardiovascular diseases. Antioxidants 10: 1167.
Salvatore, T., P.C. Pafundi, R. Galiero, G. Albanese, A. Di Martino, A. Caturano, et al. 2021. The diabetic cardiomyopathy: The contributing pathophysiological mechanisms. Frontiers in Medicine 8: 695792.
Tahir, A., P.J. Martinez, F. Ahmad, S.P. Fisher-Hoch, J. McCormick, J.L. Gay, et al. 2021. An evaluation of lipid profile and pro-inflammatory cytokines as determinants of cardiovascular disease in those with diabetes: A study on a Mexican American cohort. Scientific Reports 11: 1–12.
Kaur, N., Y. Guan, R. Raja, A. Ruiz-Velasco, and W. Liu. 2021. Mechanisms and therapeutic prospects of diabetic cardiomyopathy through the inflammatory response. Frontiers in Physiology 12: 694864.
Byrne, N.J., N.S. Rajasekaran, E.D. Abel, and H. Bugger. 2021. Therapeutic potential of targeting oxidative stress in diabetic cardiomyopathy. Free Radical Biology and Medicine 169: 317–342.
Su, J.H., M.Y. Luo, N. Liang, S.X. Gong, W. Chen, W.Q. Huang, et al. 2021. Interleukin-6: A novel target for cardio-cerebrovascular diseases. Frontiers in Pharmacology 12: 745061.
Huard, A., H.N. Do, A.C. Frank, E. Sirait-Fischer, D. Fuhrmann, M.C. Hofmann, et al. 2021. IL-38 ablation reduces local inflammation and disease severity in experimental autoimmune encephalomyelitis. The Journal of Immunology 206: 1058–1066.
Ye, C., H. Yano, C.J. Workman, and D.A. Vignali. 2021. Interleukin-35: Structure, function and its impact on immune-related diseases. Journal of Interferon & Cytokine Research 41: 391–406.
Arkew, M., T. Yemane, Y. Mengistu, K. Gemechu, and G. Tesfaye. 2021. Hematological parameters of type 2 diabetic adult patients at Debre Berhan Referral Hospital, Northeast Ethiopia: A comparative cross-sectional study. PLoS ONE 16: e0253286.
Mahdi, A., M.M. Cortese-Krott, M. Kelm, N. Li, and J. Pernow. 2021. Novel perspectives on redox signaling in red blood cells and platelets in cardiovascular disease. Free Radical Biology and Medicine 168: 95–109.
Friedewald, W.T., R.I. Levy, and D.S. Fredrickson. 1972. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical chemistry 18: 499–502.
Ross, R. 1993. The pathogenesis of atherosclerosis: A perspective for the 1990s. Nature 362: 801–809.
Wallace, T.M., J.C. Levy, and D.R. Matthews. 2004. Use and abuse of HOMA modeling. Diabetes Care 27: 1487–1495.
Poznyak, A., A.V. Grechko, P. Poggio, V.A. Myasoedova, V. Alfieri, and A.N. Orekhov. 2020. The diabetes mellitus–atherosclerosis connection: The role of lipid and glucose metabolism and chronic inflammation. International Journal of Molecular Sciences 21: 1835.
Fathelbab, M., E.M. Fahmy, A.A. Elshormilisy, A.E. Gaafar, and N.E. Waly. 2017. A putative role for oxidative stress in pathophysiology of diabetic cardiomyopathy. Egyptian Journal of Obesity, Diabetes and Endocrinology 3: 95–99.
Abdelazeem, A.H., A.S. Abuelsaad, A. Abdel-Moniem, and M. Abdel-Gabbar. 2021. Association of metabolic syndrome components with alterations in oxidative stress and cytokines expression. Journal of Taibah University for Science 15: 928–940.
Neri, M., V. Fineschi, M. Di Paolo, C. Pomara, I. Riezzo, E. Turillazzi, et al. 2015. Cardiac oxidative stress and inflammatory cytokines response after myocardial infarction. Current Vascular Pharmacology 13: 26–36.
Lee, W.S., and J. Kim. 2017. Diabetic cardiomyopathy: Where we are and where we are going. The Korean Journal of Internal Medicine 32: 404–421.
Gómez-Marcos, M.A., A.M. Blázquez-Medela, L. Gamella-Pozuelo, J.I. Recio-Rodriguez, L. García-Ortiz, and C. Martínez-Salgado. 2016. Serum superoxide dismutase is associated with vascular structure and function in hypertensive and diabetic patients. Oxidative Medicine and Cellular Longevity 2016: 9124676.
Aladağ, N., R. Asoğlu, M. Ozdemir, E. Asoğlu, A.R. Derin, C. Demir, et al. 2021. Oxidants and antioxidants in myocardial infarction (MI): Investigation of ischemia modified albumin, malondialdehyde, superoxide dismutase and catalase in individuals diagnosed with ST elevated myocardial infarction (STEMI) and non-STEMI (NSTEMI). Journal of Medical Biochemistry 40: 286–294.
Darogha, S.N. 2021. Serum levels of TNF-a and IFN-g gene polymorphism in type 2 diabetes mellitus in Kurdish patients. Cellular and Molecular Biology 67: 171–177.
Fu, Y., Y. Wu, and E. Liu. 2020. C-reactive protein and cardiovascular disease: From animal studies to the clinic. Experimental and Therapeutic Medicine 20: 1211–1219.
Zhu, L., Y. Zou, Y. Wang, X. Luo, X. Sun, K., H. Wang, et al. 2017. Prognostic significance of plasma high-sensitivity C-reactive protein in patients with hypertrophic cardiomyopathy. Journal of the American Heart Association 6 (2): e004529.
Koosha, P., H. Roohafza, N. Sarrafzadegan, M. Vakhshoori, M. Talaei, E. Sheikhbahaei, et al. 2020. High sensitivity C-reactive protein predictive value for cardiovascular disease: A nested case control from Isfahan cohort study (ICS). Global Heart 15: 3.
Hage, C., E. Michaëlsson, C. Linde, E. Donal, J.C. Daubert, L.M. Gan, et al. 2017. Inflammatory biomarkers predict heart failure severity and prognosis in patients with heart failure with preserved ejection fraction: a holistic proteomic approach. Circulation: Cardiovascular Genetics 10: e001633.
Fanola, C.L., D.A. Morrow, C.P. Cannon, P. Jarolim, M.A. Lukas, C. Bode, et al. 2017. Interleukin-6 and the risk of adverse outcomes in patients after an acute coronary syndrome: Observations from the SOLID-TIMI 52 (stabilization of plaque using darapladib—thrombolysis in myocardial infarction 52) trial. Journal of the American Heart Association 6: e005637.
Franssen, C., S. Chen, A. Unger, H.I. Korkmaz, G.W. De Keulenaer, C. Tschöpe, et al. 2016. Myocardial microvascular inflammatory endothelial activation in heart failure with preserved ejection fraction. Journal of the American College of Cardiology: Heart Failure 4: 312–324.
Yasuda, K., K. Nakanishi, and H. Tsutsui. 2019. Interleukin-18 in health and disease. International Journal of Molecular Sciences 20: 649.
Xiao, H., H. Li, J.J. Wang, J.S. Zhang, J. Shen, X.B. An, et al. 2018. IL-18 cleavage triggers cardiac inflammation and fibrosis upon β-adrenergic insult. European Heart Journal 39: 60–69.
Bahrami, A., T. Sathyapalan, and A. Sahebkar. 2021. The role of interleukin-18 in the development and progression of atherosclerosis. Current Medicinal Chemistry 28: 1757–1774.
Wei, Y., Y. Lan, Y. Zhong, K. Yu, W. Xu, R. Zhu, et al. 2020. Interleukin-38 alleviates cardiac remodeling after myocardial infarction. Journal of Cellular and Molecular Medicine 24: 371–384.
Gupta, A., Y.D. Fei, T.Y. Kim, A. Xie, K. Batai, I. Greener, et al. 2021. IL-18 mediates sickle cell cardiomyopathy and ventricular arrhythmias. Blood, The Journal of the American Society of Hematology 137: 1208–1218.
Sha, X., S. Meng, X. Li, H. Xi, M. Maddaloni, D.W. Pascual, et al. 2015. Interleukin-35 inhibits endothelial cell activation by suppressing MAPK-AP-1 pathway. Journal of Biological Chemistry 290: 19307–19318.
Ye, J., Y. Huang, B. Que, C. Chang, W. Liu, H. Hu, et al. 2018. Interleukin-12p35 knock out aggravates doxorubicin-induced cardiac injury and dysfunction by aggravating the inflammatory response, oxidative stress, apoptosis and autophagy in mice. eBioMedicine 35: 29–39.
Zhou, F., T. Feng, X. Lu, H. Wang, Y. Chen, Q. Zhang, et al. 2021. Interleukin 35 protects cardiomyocytes following ischemia/reperfusion-induced apoptosis via activation of mitochondrial STAT3. Acta Biochimica et Biophysica Sinica 53: 410–418.
Hosseini, M.S., Z. Rostami, A. Saadat, S.M. Saadatm, and E. Naeimi. 2014. Anemia and microvascular complications in patients with type 2 diabetes mellitus. Nephrourology monthly 6: e19976.
Cho, Y.I., M.P. Mooney, and D.J. Cho. 2008. Hemorheological disorders in diabetes mellitus. Journal of diabetes science and technology 2: 1130–1138.
Nada, A.M. 2015. Red cell distribution width in type 2 diabetic patients. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy 8: 525–333.
Lippi, G., G. Targher, M. Montagnana, G.L. Salvagno, G. Zoppini, and G.C. Guidi. 2009. Relation between red blood cell distribution width and inflammatory biomarkers in a large cohort of unselected outpatients. Archives of pathology & laboratory medicine 133: 628–632.
Coenen, D.M., A. Heinzmann, M. Karel, J.M. Cosemans, and R.R. Koenen. 2021. The multifaceted contribution of platelets in the emergence and aftermath of acute cardiovascular events. Atherosclerosis 319: 132–141.
Lebas, H., K. Yahiaoui, R. Martos, and Y. Boulaftali. 2019. Platelets are at the nexus of vascular diseases. Frontiers in cardiovascular medicine 6: 132.
Milosevic, D., and V.L. Panin. 2019. Relationship between hematological parameters and glycemic control in type 2 diabetes mellitus patients. Journal of Medical Biochemistry 38: 164–171.
Kern, A., R.J. Gil, K. Bojko, E. Sienkiewicz, B. Januszko-Giergielewicz, J. Górny, et al. 2017. Platelet distribution width as the prognostic marker in coronary bifurcation treatment. European Journal of Clinical Investigation 47: 524–530.
Feldman, C., and R. Anderson. 2020. Platelets and their role in the pathogenesis of cardiovascular events in patients with community-acquired pneumonia. Frontiers in Immunology 11: 577303.
Okyere, A.D., and D.G. Tilley. 2020. Leukocyte-dependent regulation of cardiac fibrosis. Frontiers in Physiology 11: 301.
Woitas, R.P., and S. Schwab. 2017. Neutrophil counts and their potential prognostic value in cardiovascular diseases. Journal of Laboratory and Precision Medicine 2: 30.
Ibrahim, M.S., A.A. Khalil, and A.S. Ali. 2020. Neutrophils-to-lymphocytes ratio in children with acute heart failure. The Egyptian Journal of Hospital Medicine 81: 1878–1883.
Demirtas, L., H. Degirmenci, E.M. Akbas, A. Ozcicek, A. Timuroglu, A. Gurel, et al. 2015. Association of hematological indices with diabetes, impaired glucose regulation and microvascular complications of diabetes. International Journal of Clinical and Experimental Medicine 8: 11420–11427.
Abdel-Moneim, A., M. Semmler, E.S. Abdel-Reheim, M.I. Zanaty, and W. Addaleel. 2019. Association of glycemic status and interferon-γ production with leukocytes and platelet indices alterations in type2 diabetes. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 13: 1963–1969.
Duman, T.T., G. Aktas, B.M. Atak, M.Z. Kocak, E. Erkus, and H. Savli. 2019. Neutrophil to lymphocyte ratio as an indicative of diabetic control level in type 2 diabetes mellitus. African Health Sciences 19: 1602–1606.
Hussain, M., M. Babar, L. Akhtar, and M.S. Hussain. 2017. Neutrophil lymphocyte ratio (NLR): A well assessment tool of glycemic control in type 2 diabetic patients. Pakistan Journal of Medical Sciences 33: 1366–1370.
Li, X.T., H. Fang, D. Li, F.Q. Xu, B. Yang, R. Zhang, et al. 2020. Association of platelet to lymphocyte ratio with in-hospital major adverse cardiovascular events and the severity of coronary artery disease assessed by the Gensini score in patients with acute myocardial infarction. Chinese Medical Journal 133: 415–423.
Toprak, C., M.M. Tabakci, Z. Simsek, U. Arslantas, H.I. Durmus, L. Ocal, et al. 2015. Platelet/lymphocyte ratio was associated with impaired myocardial perfusion and both in-hospital and long-term adverse outcome in patients with ST-segment elevation acute myocardial infarction undergoing primary coronary intervention. Postępy w Kardiologii Interwencyjnej= Advances in Interventional Cardiology 11: 288–297.
Zhou, Z., M. Liang, H. Wu, S. Huang, R. Weng, J. Hou, et al. 2021. Preoperative lymphocyte-to-monocyte ratio as a prognostic predictor of long-term mortality in cardiac surgery patients: A propensity score matching analysis. Frontiers in Cardiovascular Medicine 8: 639890.
Fan, W. 2017. Epidemiology in diabetes mellitus and cardiovascular disease. Cardiovascular endocrinology 6: 8–16.
Acknowledgement
The authors thank Prof. Malgorzata A. Garstka (Second Affiliated Hospital of Xi’an Jiaotong University, China) for improving the English language of the manuscript.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
Adel Abdel Moneim, Basant Mahmoud, and Hanan Soilman contributed to the study conception and design. Material preparation, data collection and analysis were performed by Basant Mahmoud, Mohamed Y. Zaky, and Howaida Saada. The first draft of the manuscript was written by Adel Abdel Moneim and Mohamed Y. Zaky, and authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate (Human)
All patients provided a written consent and blood samples during the period from March 2019 to November 2019 following protocol approval by the Hospital Ethics Committee (BNS/2019/2).
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Saad, H., Soliman, H.A., Mahmoud, B. et al. The Pathogenic Role of Oxidative Stress, Cytokine Expression, and Impaired Hematological Indices in Diabetic Cardiovascular Diseases. Inflammation 46, 146–160 (2023). https://doi.org/10.1007/s10753-022-01718-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-022-01718-w