Abstract
Heart failure (HF) is a clinical syndrome characterized by well-defined signs and symptoms due to structural and/or myocardial functional impairment, resulting in raised intracardiac pressures and/or inadequate cardiac stroke volume at rest or during exercise. This could derive from direct ischemic myocardial injury or other chronic pathological conditions, including valvular heart disease (VHD) and primary myocardial disease. Early identification of HF etiology is essential for accurate diagnosis and initiation of early and appropriate treatment. Thus, the presence of accurate means for early diagnosis of HF symptoms or subclinical phases is fundamental, among which echocardiography being the first line diagnostic investigation. Echocardiography could be performed at rest, to identify overt structural and functional abnormalities or during physical or pharmacological stress, in order to elicit subclinical myocardial function impairment e.g. wall motion abnormalities and raised ventricular filling pressures. Beyond diagnosis of ischemic heart disease, stress echocardiography (SE) has recently shown its unique value for the evaluation of diastolic heart failure, VHD, non-ischemic cardiomyopathies and pulmonary hypertension, with recommendations from international societies in several clinical settings. All these features make SE an important additional tool, not only for diagnostic assessment, but also for prognostic stratification and therapeutic management of patients with HF. In this review, the unique value of SE in the evaluation of HF patients will be described, with the objective to provide an overview of the validated methods for each setting, particularly for HF management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart failure (HF) is the most common cause of death among cardiovascular (CV) diseases [1, 2] and its incidence continues to increase, mainly due to aging of the population. Therefore, new investigations have been developed and others are currently under evaluation to help improving prognosis and quality of life of HF patients. Stress echocardiography (SE) is a validated tool not only for the assessment of ischemic HF [3], but also for non-ischemic HF, such as or valvular heart disease [4] or unmasking significant diastolic dysfunction, allowing the identification of early stages of HF with preserved ejection fraction (HFpEF) [5]. This leads to early start of treatment, with considerable improvement of symptoms and quality of life. SE has also been used in advanced HF to optimize the selection of marginal donors with the aim of extending the pool of donors for heart transplantation [6].
The aim of the present review is to highlight the unique value of SE for the evaluation of HF patients, analyzing the advantages and disadvantages of the various SE modalities and describing different clinical applications in HF setting.
Heart failure: pathophysiology of alterations induced by stress
Valvular heart disease
Resting transthoracic echocardiography is the most used investigation for non-invasive evaluation of valvular heart disease (VHD). However, VHD dynamic component is significantly influenced by loading conditions, ventriculo-arterial coupling and subclinical myocardial dysfunction, which may be underestimated at rest. Thus, SE may add diagnostic information in VHD, through the evaluation of clinical response and dynamic changes in ventricular and valvular function during exercise/stress, e.g. in patients reporting HF exertional symptoms but not showing significant VHD at resting echocardiography.
In mitral valve disease, the increase in heart rate (HR) causes a fall in filling time and LV preload and an increase in left atrial and pulmonary arterial pressures. This may explain symptoms like shortness of breath on exertion, disproportionate to the resting degree of valvular disease, which may in severe cases lead to HF and unexplained acute pulmonary edema [7, 8].
Chronic aortic regurgitation (AR) results in increased LV pressure and volume overload and chronically HF. Symptoms induced by AR have an insidious and late onset. The onset of symptoms at rest is associated with bad prognosis and a reported annual mortality as high as 10–20%, thus Therefore, early identification of AR symptoms by SE may be crucial for its management [9].
Moreover, the use of SE is recommended as part of the diagnostic algorithm of aortic stenosis (AS), particularly in low-flow-low-gradient disease [7]. The presence of AS causes a chronic pressure overload, resulting in the development of concentric LV hypertrophy to maintain an adequate stroke volume (SV) and diastolic dysfunction. Exercise hemodynamics in patients with moderate-severe AS are usually abnormal even in patients without symptoms. Although in these patients resting CO could be normal, its increase with exercise is limited and is primarily mediated by an increase in HR. This results in a short systolic ejection interval with little change in SV and an increase in the velocity of the aortic jet and transvalvular gradient. Initially, aortic valve area tends to slightly increase with exercise (0.2 cm2 on average), underestimating symptoms. With worsening AS, aortic valve area does not significantly increase with exertion, while a further increase in jet velocity and transvalvular gradient could be demonstrated by SE (“true severe AS”) [8, 10]. Furthermore, patients with AS also develop an abnormal blood pressure (BP) response to exercise (increase by < 10 mmHg), which indicates severe valve obstruction, and, typically, this corresponds to the onset of symptoms [10].
Diastolic HF
The use of SE in diastolic HF is based on the so-called “cardiac reserve”, defined as cardiac response to increased preload enhancing CO without significant increase in LV filling pressure, resulting from contractile reserve and relaxation (diastolic) reserve. The impairment of relaxation properties is called “diastolic dysfunction (DD)” and, if leading to HF symptoms is regarded as “diastolic HF” or “HFpEF”, which has gained increasing importance in recent years. In fact, it is the main cause of hospitalization in 40% of patients presenting with symptoms of HF [11, 12].
Patients with HFpEF or DD and little or no sign of congestion at rest may present with exercise intolerance for several reasons: 1) high LV diastolic/pulmonary venous pressure during stress causing reduction in lung compliance, increase breathing work and dyspnea [13]; 2) many patients present with LV concentric hypertrophy with small end-diastolic LV volume, so during exercise the Frank-Starling mechanism limits these ventricles, with compromised SV and CO [14, 15]; 3) subtle and latent contractile abnormalities are typically present in many of these patients, in whom, however, DD is the dominant feature [13]. The investigation of DD by diastolic SE is suggested in the latest HF guidelines of the European Society of Cardiology (ESC) [16] in the presence of equivocal resting echocardiographic and laboratory markers, as an attempt to establish the diagnosis of HFpEF.
Ischemic HF
One of the most conventional applications of SE is to find myocardial ischemia as a transient, regional imbalance between augmented myocardial oxygen demand and inadequate supply. Myocardial ischemia results in a typical cascade of events with well-defined time sequence: regional mechanical dysfunction (with a reduction of segmental motion and thickening) can be early detected by SE, ECG changes and the onset of chest pain occurs later [17]. SE may also be used for follow-up evaluation of patients with CAD with residual coronary stenosis or new onset of symptoms [16]. In the absence of coronary artery disease (CAD), coronary flow reserve (CFR) can be reduced because of microvascular disease, causing angina with ST-segment depression and regional wall motion thickening (RWMT) abnormalities during stress [18, 19].
The loss of myocytes secondary to myocardial necrosis in CAD is the leading cause of HF. Therefore, noninvasive identification of the extent of myocyte loss and estimation of the extent of segmental viability is particularly useful for clinical decision making in patients with ischemic LV dysfunction.
Stress echo – methodology
Protocols and stressors
SE provides dynamic evaluation of myocardium under conditions of physiological (exercise) or pharmacological (inotrope, vasodilator) stress to unveil structural/functional abnormalities, absent at rest, such as wall motion abnormalities, VHD, or other hemodynamic disturbances [20,21,22,23].
Physical exercise SE (treadmill or bicycle) should be the preferred method since it reflects physiological hemodynamic response to exercise and provides information on exercise capacity [24]. For the treadmill test, Bruce/modified Bruce protocols or bicycle ergometer SE are used [25] (Fig. 1).
Stress echo – protocols and stressors description of the Bruce and the modified Bruce protocol, presenting characteristics of all their stages [25]; description of bicycle ergometer SE protocol, with the main echocardiographic parameters to be acquired at each stage; main pharmacological stressors used in stress echocardiography with their administration protocols. HF, heart failure; LV, left ventricle; LVOT, left ventricular outflow tract; MR, mitral regurgitation; RV, right ventricle; RWMA, relative wall motion abnormalities; SPAP, systolic pulmonary artery pressure
In patients unable to undertake physical exercise or those with abnormal resting RWMT, pharmacological SE should be chosen [24]. The commonly used stressors are dobutamine and vasodilators. In Fig. 1, information about the administration protocols of pharmacological stressors during SE are reported. Dobutamine acts mainly on myocardial β-1 adrenergic receptors, increasing HR and contractile function, with a consequent higher myocardial oxygen consumption. Myocardial contractility increases over four-fold in healthy subjects and much less (less than two-fold) in patients with HF [26]. The dobutamine activation of β-2 adrenergic receptors, through a vasodilatory effect, may contribute to a mild decrease in BP at higher doses. Compared with exercise SE, the increase in wall stress is lower, due to reduced recruitment of venous blood volume with dobutamine. During or soon after the maximum dose of dobutamine, atropine can be administered to increase heart rate and improved test-accuracy [24].
Vasodilator SE can be performed with dipyridamole, adenosine, or regadenoson. All these stressors share the same metabolic pathway. Dipyridamole increases endogenous adenosine levels, adenosine increases exogenous adenosine levels, while regadenoson acts directly on vascular A2A adenosine receptors, with higher receptor specificity, less test duration and less potential for complications. The activation of this pathway produces a small decrease in BP, modest tachycardia, and a mild increase in myocardial function [27, 28]. In the presence of a critical epicardial stenosis or microcirculation dysfunction, vasodilator administration causes a heterogeneity of coronary blood flow between stenotic and normal coronary arteries subtended areas. This provokes a supply–demand mismatch, and therefore, via steal phenomenon, a reduction in subendocardial flow in areas of coronary artery stenosis.
Indications—when and which SE modality should be preferred
Patients able to perform physical exercise should undergo physical stress, as described in Table 1. This preserves the integrity of the electro-mechanical response and allows the correlation of symptoms with CV workload, wall motion abnormalities, and hemodynamic responses, such as pulmonary pressure and transvalvular flows and gradients. Semi-supine bicycle exercise is technically easier than upright bicycle or treadmill exercise, especially when multiple stress parameters are assessed at peak exercise.
Pharmacological stress is usually not able to replicate the complex exercise-triggered hemodynamic and neurohormonal changes [29,30,31]. Among all pharmacological stressors, dobutamine is the preferred for the evaluation of contractile function and flow reserve. Different protocols have been used to evaluate contractile reserve, changes in LV volumes and ejection fraction (EF), including low-dose (10 mg/kg/min) to high-dose (40 mg/kg/min) dobutamine SE. High-dose is the preferred method in ischemic HF, while in patients with non-ischemic HF there is no consensus on the optimal dobutamine protocol [32, 33].
Vasodilator SE may be preferred for combined assessment of wall motion and CFR, which may be impaired in dilated non-ischemic cardiomyopathy and hypertrophic cardiomyopathy [27, 28]. Dipyridamole SE is not often used to study contractile reserve, but may be useful if patients are under treatment with β-blockers. It is associated with less arrhythmias [33]. Regadenoson, due to its high cost, is usually preferred in patients with chronic obstructive pulmonary disease and asthma [24].
Standard pharmacological ischemia protocol consists of three stages (rest, intermediate, peak), while the presence of RWMT abnormality necessitates a four-stage viability protocol for assessment of biphasic response. In patients with permanent pacemaker, exercise SE or combination of pacing with pharmacological stress can be performed solely with appropriate programming of the permanent pacemaker (i.e. high-rate pacing [34, 35].
Advantages/limitations
SE is a validated, non-invasive, available, bed-side, low-cost investigation and is widely used for its ability to assess segmental LV function continuously and simply on a beat-by-beat basis. Echocardiography performed with vasodilator or inotropic stress has proved to be a clinically useful test for the assessment of myocardial ischemia and viability in the evaluation of VHD and cardiomyopathies. Compared with the competing nuclear or cardiac magnetic resonance (CMR) techniques, SE offers comprehensive information on VHD, despite some well-known limitations. These include subjectivity, particularly for the interpretation of wall motion and thickening, with a significant inter- and intra-observer variability. The variability appears to be very small when baseline image quality is good but turns out to be significant for patients with poor acoustic window [36, 37]. There is also a significant degree of variability of interpretation of SE depending on the level of expertise of the operator and center experience [38].
Stress echo – clinical applications in heart failure
In the latest guidelines of the European Society of Cardiology (ESC) for the diagnosis and treatment of acute and chronic HF, [16] SE role is mentioned for the evaluation of the underlying disease causing the HF, prognostic stratification and therapeutic management. The clinical applications of SE in HF setting could be categorized in two main subsets: SE in ischemic HF and SE in non-ischemic HF.
Ischemic HF
SE can detect both myocardial ischemia and viability in patients with CAD [39]. Wall motion may visually and semi-quantitatively be graded in 16 segments on a 4 grade Likert scale: 1 = normal, 2 = hypokinesia, 3 = akinesia, and 4 = dyskinesia. Then, the sum of the scores of each segment constitutes wall motion score index. The preferred SE method for the detection of both ischemia and viability is high-dose dobutamine [40] (which may cause arrhythmias), while low- dose dobutamine is sufficient if the evaluation of ischemia is not required [41]. Ischemia is diagnosed if at least two segments in the same coronary territory degrade by at least one-point with high-dose dobutamine. Viability is detected when at least two dysfunctional segments in the same coronary territory improve at low-dose dobutamine by at least one-point or present a biphasic response at high-dose dobutamine infusion [42].
In the latest ESC HF guidelines exercise or pharmacological SE was suggested for the assessment of inducible ischemia [16]. Particularly, the guidelines state that non-invasive stress imaging [CMR, stress echocardiography or nuclear imaging may be considered (class IIb recommendation)] for the assessment of myocardial ischemia and viability in patients with CAD suitable for coronary revascularization [43], and these may serve as a guide for invasive coronary angiography, which may be considered (IIb) in patients with HF while reduced EF (HFrEF) with an intermediate to high pre-test probability of CAD in presence of ischemia on non-invasive stress test [44].
In fact, SE application for diagnosis of significant CAD has a sensitivity and specificity of 85% and 77% respectively. Besides, with a negative exercise SE, patients have a very low mortality and significant events rate (0.6–0.8% per patient/year), even with an intermediate-high pretest probability [45]. The outcome of patients with an abnormal SE compared to normal SE is significantly worse (survival 71.2% vs 92%, respectively) [3].
The identification of dysfunctional but viable myocardium with SE, with its subsequent revascularization, may allow improvement of regional and global cardiac systolic function [46,47,48]. Moreover, several non-randomized studies have evaluated the endpoint of death, suggesting that viability-guided revascularization might improve patients’ survival [49,50,51]. However, these results have not been confirmed in different prospective randomized trials [48, 52,53,54,55,56]. For this reason, current guidelines do not advocate (Class IIb indication) routine testing of myocardial viability to select revascularization of patients with HF. Considerable debate remains on how these results should be interpreted, [57] and viability assessment remains widely used in clinical practice.
Currently, the study of myocardial viability is suggested in the following clinical settings [58]:
-
to guide revascularization of patients with HF, known CAD and wall motion abnormalities (ESC Class IIb Level B);
-
to guide revascularization of patients presenting with HF and late presentation of acute coronary syndrome;
-
to select optimal revascularization (percutaneous vs. surgical) strategy in patients with complex multivessel CAD;
-
to decide upon percutaneous revascularization or medical therapy in patients with chronic total occlusions.
Furthermore, the study of myocardial viability is applicable even in VHD:
-
to determine the mechanism of ischemic MR and guide decision making for valve replacement and revascularization in patients with ischemic MR, LVEF < 30% and an option for surgical revascularization (ESC Class IIa Level C);
-
to determine the contractile response (low-dose dobutamine echocardiography) in low-flow AS (ESC Class IIa Level C).
In patients with normal LV kinetics at peak SE measuring CFR could provide an additional value. It is assessed as the ratio between stress to baseline peak diastolic coronary Doppler flow velocities, usually obtained from left anterior descending artery (LAD) images. In all types of SE, the main challenges are the visualization of LAD in the 4-chamber view and the acquisition of a correct Doppler signal, as the Doppler cursor has to be aligned with a moving small vessel. For these reasons, the most feasible modality of SE for CFR assessment proved to be dipyridamole. CFR has shown to be of additional prognostic value to RWMT assessment [10] and might be useful in microvascular disease recognition in different subsets of patients, such as diabetics, hypertensives, and those with hypertrophic or dilated cardiomyopathy [3].
Importantly, an emerging diagnostic stress technique for assessing myocardial perfusion in ischemic heart disease is myocardial contrast stress echocardiography (MCSE). Since perfusion abnormalities occur earlier than wall motion abnormalities, MCSE may be helpful in patients who cannot exercise, or those intolerants of high inotropic doses. It has higher sensitivity compared to single positron emission computer tomography (SPECT) (75.2% versus 49.1%) in the detection of CAD in a population with chest pain and high incidence of risk factors, particularly for the detection of microvascular disease [43, 44]. However, it has lower specificity compared to SPECT. Furthermore, high-dose dobutamine MCSE has shown similar diagnostic accuracy for diagnosing significant CAD, compared with CMR [45].
Non-ischemic HF
In patients with HF symptoms and non-ischemic cardiomyopathy, various etiologies may be involved (cardiomyopathies, VHD, diastolic HF, cardiotoxicity, etc.). These conditions are relatively common and are associated with high mortality rate [59]. In early disease stages, when LV EF is still preserved, a reduction in the contractile reserve during SE identifies subclinical myocardial dysfunction, thus might help clarifying the diagnosis; HFpEF, VHD, or unexplained dyspnea [37]. SE should also assist in detecting early chemotherapy-induced cardiotoxicity [24], hypertensive as well as diabetic cardiomyopathy and thalassemia [37, 60,61,62,63,64].
On the other hand, in advanced HF residual myocardial contractile reserve assessed by SE can differentiate ischemic from non-ischemic cardiomyopathies, for prognostic stratification, and to guide clinical decision making [65]. Independent of LV EF, the absence of contractile reserve is often associated with limited CFR [66, 67], a marker of latent LV systolic dysfunction and sub-clinical cardiomyopathy. Moreover, the presence of inotropic contractile reserve has been associated with less need for cardiac transplantation [68, 69], being inversely correlated with the extent of interstitial fibrosis and scarred myocardium [70] and with better survival rate, fewer hospitalizations for HF [71], and increase in LV EF during follow-up [72]. A reduction or the absence of CFR and contractile reserve during dipyridamole SE in patients with non-ischemic cardiomyopathy proved to be a marker of poor prognosis [73, 74].
The addition of lung ultrasound to SE has provided useful in demonstrating HF. B-lines (or lung comets) are vertical, hyperechoic images that start from the pleural line and extend to the bottom of the display, without fading but move synchronously with respiration. In patients with HF, the presence and the number of B-lines has been shown to correlate with the presence of pulmonary interstitial edema and raised LV filling pressure [43, 75, 76]. During exercise SE, the appearance of B-lines might be used to demonstrate that exertional dyspnea is consequent to pulmonary congestion as a sign of HF [77].
The evaluation of B-lines has been proposed in the ABCDE-SE protocol introduced in the SE2020 study [78, 79]. This is a five-step protocol based on the shift in the pathophysiological model from stenosis vulnerability to patient vulnerability which emerged in the last decade, focusing not only on angina during the evaluation of SE. The currently ongoing SE2030 study is articulated in 12 different projects, in order to provide further evidence to finally recommend SE as the optimal and versatile imaging modality for functional testing [80].
Diastolic stress echocardiography
SE has been affirmed as a tool for detecting impaired LV diastolic function reserve and the subsequent increase in LV filling pressures [81,82,83] in patients with unexplained dyspnea or suspected subclinical diastolic dysfunction.
Its application is of additive value in patients with suspect HFpEF, in whom SE is currently recommended in the HFA-PEFF algorithm [84] as a component of the diagnostic workflow in cases of uncertainty (intermediate risk) after clinical assessments and standard diagnostic tests to confirm the diagnosis of HFpEF using a supine bicycle [84]. Post-exercise assessment should be performed during recovery, especially in patients with a rapid increase in HR at low level exercise. Moreover, a simple non-exercise modality for preload augmentation is passive leg raise, which may identify patients with raised stress-induced LV filling pressure causing lower exercise capacity [85] (Fig. S1).
The most investigated parameter in diastolic SE in previous studies is E/eʹ ratio as an index of filling pressures [86, 87]. To overcome the limit of high HR with E/A wave fusion, E/e’ ratio during low-level exercise (20W) proved to have higher feasibility and accuracy in predicting PCWP during peak exercise, hence supporting its use as an alternative to the peak exercise value in ruling out HFpEF in patients with dyspnea [88].
Another key marker for assessing LV diastolic function during SE is sPAP [8, 82, 89]. Exercise septal E/ e′ > 13, lower amplitude of changes in diastolic longitudinal velocities, and induced pulmonary hypertension (sPAP ≥ 50 mmHg) are markers of adverse outcomes in patients with HF [89,90,91,92,93].
However, E/eʹ may be misleading in the presence of mitral annular calcification, moderate/severe MR, constrictive pericarditis, mitral valve replacement/repair, left bundle branch block, or significant AR [91], and sPAP may be difficult to evaluate in the absence of TR or may be underestimated in the presence of a severe TR or impairment of RV function [89]. Therefore, new parameters have been evaluated, such as the ratio of early diastolic velocity of mitral inflow to the flow propagation velocity (E/Vp), marker of LV filling pressure, diastolic functional reserve index (DFRI), based on changes in e' velocity on exercise, isovolumic relaxation time (IVRT), LV diastolic strain rate and diastolic dyssynchrony. However, to date, these markers need to be validated [89]. For these reasons, currently, E/eʹ and sPAP are still the most used echocardiographic markers of LV filling pressure.
Another parameter which may be used to estimate DD is derived from the ratio between CO and invasive mean PCWP, a surrogate marker of left atrial pressure, both measured at baseline and during stress (Table 2), a stress marker of diastolic function compared to right heart catheterization [82, 85, 94,95,96,97]. However, the accuracy of the relationship between LV filling pressure and CO has been evaluated only in small and cross-sectional studies, and its clinical implications is limited [85, 94,95,96,97,98].
Valvular heart disease
The role of SE for the evaluation of VHD has been fully addressed in the latest guidelines of international societies [7, 103]. In these patients, symptoms may develop slowly, hence many patients may refer to be asymptomatic. For this reason, guidelines emphasize the use of exercise testing to assess objective evidence of symptoms and exercise capacity [7, 103]. Moreover, SE could be of value when there is discordance among baseline measurements and the symptoms [103]. In patients with prosthetic valves, disproportionate increase in mean transvalvular gradient during exercise (i.e. > 20 mmHg for aortic prostheses or > 12 mmHg for mitral prostheses) suggests severe prosthesis stenosis or significant patient-prosthesis mismatch [103]. Overall, SE is regarded a second line examination in VHD (usually after transthoracic and, sometimes, transesophageal echocardiography), to further assess etiology, severity, and prognosis [7]. In VHD, physical exercise is the test of choice since it provides the most physiological assessment, and a semi-supine bike is recommended [7, 104].
Mitral valve disease
SE may be useful to establish the etiology of MR (class of recommendation 1 for 2020 American guidelines) and to assess myocardial viability [7] in chronic secondary MR. It may also add prognostic information, as an increase in the effective regurgitant orifice area ≥ 13 mm2 during exercise is associated with higher risk of CV events in medically treated patients [105]; then, an increase in sPAP [105] and the development of exercise-induced B-lines [106] (signs of pulmonary hypertension and systemic hemodynamic congestion, respectively) are independently associated with higher rates of cardiac events in patients with MR. Marked changes in MR severity (at least 1 grade) [4] are associated with an increase in sPAP and reduced symptom-free survival [107].
Interestingly, Kusunose et al. have shown that in asymptomatic primary MR, RV function worsening during SE, shown as a tricuspid annular plane systolic excursion < 19 mm, might stratify prognosis independently of the onset of pulmonary hypertension [108].
In rheumatic mitral stenosis, SE is recommended to evaluate symptoms, exercise capacity, variation of mean mitral gradient and of sPAP [7]. An increase in mean transmitral gradient ≥ 15 mmHg or a sPAP ≥ 60 mmHg during exercise/stress is considered abnormal [103].
Aortic valve disease
In asymptomatic patients with severe AS, SE is recommended by international guidelines as it provides diagnostic and prognostic information beyond aortic valve area and transvalvular pressure and gradients at rest. In patients with suspected low-flow, low-gradient severe AS with reduced LV EF, low-dose dobutamine SE is recommended by ESC VHD guidelines (class I) to distinguish between true severe and pseudo-severe AS (increase in valve area to > 1.0 cm2) and identify patients with no flow (or contractile) reserve [7]. In patients with no flow reserve (increase in indexed SV ≤ 20%) “indeterminate AS severity” is diagnosed if aortic valve area and transvalvular gradient do not change. The absence of contractile reserve occurs in up to 30% of AS patients and is a predictor of high mortality in the perioperative period after surgical aortic valve replacement. [7] However, this pattern does not correlate with post-operative late survival, hence should not contraindicate surgical or percutaneous procedures as they improve long-term prognosis and LV function [7]. A fall in systolic BP ≥ 20 mmHg during SE and decreased exercise tolerance are indications of intervention (class IIa and I for 2020 American and 2021 ESC guidelines respectively) in patients with severe AS asymptomatic at rest.
Importantly, SE is not indicated and can be harmful (contraindicated, class III) in symptomatic patients with severe AS [7].
In patients with AR, neither exercise nor dobutamine SE is indicated to grade valvular disease severity, since the stress-induced increase in HR shortens diastole, therefore limiting the quantification of AR severity. Exercise echocardiography may help assessing the symptomatic status of the patients with severe AR, with a dramatic change in prognosis [9] and to evaluate LV contractile reserve [109]. In these patients, the timing of intervention could be anticipated in the presence of a lack of LV contractile reserve (defined as an increase in EF < 5%) [4].
Tricuspid regurgitation
SE could be used to assess exercise capacity in patients with severe tricuspid regurgitation (TR) irrespective of symptoms. It may aid the assessment of stress-induced worsening valve dysfunction, sPAP increase and myocardial ischemia. Furthermore, RV functional reserve may be assessed by measuring tricuspid annular plane systolic excursion (TAPSE), RV tissue doppler imaging S’, and RV fractional responses during stress [66]. RV longitudinal strain by speckle tracking echocardiography may also be measured, even though limited by high HR [110]. A decrease or lack of augmentation of these indices highlights an impairment in RV functional reserve and a worse outcome in patients with concomitant left-sided valve disease [111].
Advanced heart failure—The ADONHERS protocol
Another potential application of SE in HF patients is in potential heart donors for patients with advanced HF, and thus is used as a mean to overcome the challenge of heart donor shortage in heart transplantation [112]. The ADONHERS protocol was developed in Italy to obtain a possible extension of eligible donors, despite age and non-significant comorbidities, applying an accurate screening by SE [6]. After excluding a severe LV hypertrophy or VHD and resting global or RWMT abnormalities, the brain-dead potential donor, aged > 55 (and less than 65) years or < 55 years with known multiple CV risk factors, undergoes dipyridamole SE. In the presence of preserved LV contractile function, assessed by systolic BP/LV end-systolic volume stress/rest ratio (Sagawa index) and normal global and regional function after stress, the potential donor can be considered eligible [113, 114]. Speckle-tracking echocardiography may be used as a valuable additional tool to overcome operator-dependency [115].
Stress echo – new perspectives
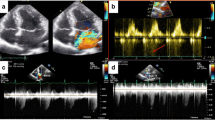
Contrast-enhanced stress echocardiography
Endocardial border definition may deteriorate at stress for translational heart movement produced by tachycardia or rapid chest wall movement (during exercise). To overcome these limitations, during SE, the intravenous injection of contrast agents, mainly microbubbles that contain air or high molecular weight gas may be used (Fig. 2). These help to identify RWMT abnormalities that could be missed, particularly in obese patients (sensitivity 91%, vs 80% of normal SE) [46]. Moreover, the use of contrast enhanced SE increases the inter-observer agreement (79% vs 69% in normal SE) [116] and improves the concordance of the interpretation of novice operators to the expert readers [117].
Myocardial contrast stress echocardiography
MCSE can measure rest and stress perfusion of the myocardium without using ionizing radiation. It utilizes inert gas-filled microbubbles that entirely remain within the vascular space and have a rheology in the vessels like that of the red blood cells [118, 119]. This method provides an estimation of the two components of capillary perfusion: flow velocity and blood volume fraction, which product is proportional to CFR [120].
MCSE has shown promising results in the detection of ischemia, but it could also aid prognostic stratification of patients with HF and ischemic cardiomyopathy. Compared to clinical, LV functional parameters and SPECT, MCSE resulted as the only independent predictor of improvement of LV function in hibernating myocardium [121]. Vasodilator MCSE is capable of distinguishing physiological from pathological LV hypertrophy, since CFR is significantly reduced in patients with hypertrophic cardiomyopathy compared to athletes [122]. Finally, in patients with Tako-Tsubo cardiomyopathy, vasodilator MCE reveals a reversible perfusion defect, while the perfusion defect is persistent in patients with ST elevation myocardial infarction [123].
Strain and strain rate stress imaging
The study of myocardial deformation during SE may also be of added value. Speckle tracking analysis is currently the most used and has been shown to overcome many tissue-Doppler limitations, above all angle-dependence and, being a semi-automated technique, poor inter-operator agreement [124,125,126,127]. LV global longitudinal strain (GLS) is most reproducible in all stages of dobutamine SE [128] and offers important additive information in ischemic HF, such as for the detection of ischemia, since the longitudinal subendocardial fibres are the first ones to be affected in the ischemic cascade, for the diagnosis of microvascular angina [124, 129]; for the assessment of viability in patients with severe LV systolic impairment; and for the differentiation between stunned and hibernating myocardium [130,131,132]. Furthermore, stress GLS during SE may be used for prognostic assessment of low-flow low-gradient AS, as it performs better than myocardial contractile reserve [133].
LV GLS can also be used in diagnostic assessment of cardiomyopathies, as it only slightly increases during stress in hypertension, and demonstrates significantly blunted augmentation in hypertrophic cardiomyopathy, with a similar absence of incremental increase in longitudinal diastolic function during exercise. Furthermore, time to peak strain measured during stress may be used for differential diagnosis in hypertrophic cardiomyopathy compared with hypertension [134]. Finally, STE could be an important tool in the detection and monitoring of early RV abnormalities. In arrhythmogenic RV dysplasia, RV strain values are reduced at rest and do not significantly increase during SE [135].
In dilated cardiomyopathy, the assessment of left atrial strain variation, as manifestation of functional reserve, has been proved to be an independent predictor of CV events. LA functional reserve could therefore act in people with HF as an additional prognostic tool together with LV contractile or diastolic reserve [136, 137].
However, speckle tracking during stress has some limitations (Fig. 2). Fast HR induced with stress, reduces image frame rate, 40–90 frames/sec, despite the overall accuracy it is described as only reasonable [128, 132]. Moreover, since in exercise SE post-ischemic RWMT anomalies persist even after recovery, speckle tracking has comparable sensitivity to that of conventional SE [138].
Three-dimensional stress echocardiography
Three-dimensional (3D) echocardiography can be used with SE to provide incremental anatomic information, allowing direct visualization of RWMT and providing accurate measurements of LV ejection fraction and volumes. A correct acquisition of parasternal short axis view (PSAX) allows better appreciation of basal wall motion abnormalities, thus resulting in higher accuracy of 3D echocardiography compared to the multiplane mode, particularly for right coronary artery territory lesions [139]. Furthermore, by cropping the 3D volumetric dataset along the correct axes, the method avoids apical foreshortening, so becoming less likely to miss apical segments’ ischemia and LAD disease [140, 141]. Its main limitation is the low temporal resolution (Fig. 2). However, improvement of the technology has allowed the acquisition of the full volume in a single beat, with good image quality product (up to 40 volumes/sec) and elimination of artifacts related to body movement, increased respiration, or arrhythmias.
Conclusions
SE plays an important role in the evaluation of HF patients, not only for accurate diagnosis but also for prognostic stratification and for planning therapeutic management strategies. The application of SE extends from the evaluation of ischemic HF, where it mainly detects myocardial ischemia and viability to providing significant therapeutic indications, to the study of non-ischemic HF. SE has also been recommended for diastolic HF and valvular pathologies, while further information is needed about the role of SE in patients with other cardiomyopathies, pulmonary hypertension, and on its impact on improving patient’s outcome (Central Illustration as Supplementary Material). Beyond being a bed-side, low-cost and highly available investigation, the high sensitivity and specificity of SE makes it an invaluable tool in the hands of the clinician. The use of SE with speckle tracking, contrast enhanced SE, MCSE and multidimensional imaging may overcome its limitations and further enhance its feasibility and additive value, thus paving the way for a further increase in its use in clinical practice, with significant benefit for HF patients.
Availability of data and materials
Not applicable.
References
Dewan P, Rørth R, Jhund PS, Shen L et al (2019) Differential impact of heart failure with reduced ejection fraction on men and women. J Am Coll Cardiol 73(1):29–40. https://doi.org/10.1016/j.jacc.2018.09.081. PMID: 30621948
Mentzer G, Hsich EM (2019) Heart failure with reduced ejection fraction in women: epidemiology, outcomes, and treatment. Heart Fail Clin 15(1):19–27. https://doi.org/10.1016/j.hfc.2018.08.003. Epub 2018 Oct 24. PMID: 30449377; PMCID: PMC6298793
Picano E, Pellikka PA (2014) Stress echo applications beyond coronary artery disease. Eur Heart J 35(16):1033–1040. https://doi.org/10.1093/eurheartj/eht350. Epub 2013 Oct 14 PMID: 24126880
Lancellotti P, Pellikka PA, Budts W et al (2017) The clinical use of stress echocardiography in non-ischaemic heart disease: recommendations from the european association of cardiovascular imaging and the american society of echocardiography. J Am Soc Echocardiogr 30(2):101–138. https://doi.org/10.1016/j.echo.2016.10.016. PMID: 28164802
Kusunose K (2020) Clinical application of stress echocardiography in management of heart failure. Heart Fail Clin 16(3):347–355. https://doi.org/10.1016/j.hfc.2020.02.001. Erratum. In: Heart Fail Clin. 16(4):xi. PMID: 32503757
Bombardini T, Gherardi S, Arpesella G et al (2011) Favorable short-term outcome of transplanted hearts selected from marginal donors by pharmacological stress echocardiography. J Am Soc Echocardiogr 24(4):353–362. https://doi.org/10.1016/j.echo.2010.11.014. PMID: 21440213
Vahanian A, Beyersdorf F, Praz F et al (2022) ESC/EACTS Scientific Document Group. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 43(7):561–632. https://doi.org/10.1093/eurheartj/ehab395. Erratum in: Eur Heart J. 2022 Feb 18;: PMID: 34453165
Nishimura RA, Otto CM, Bonow RO et al (2014) American College of Cardiology/American Heart Association task force on practice guidelines. 2014 aha/acc guideline for the management of patients with valvular heart disease: a report of the american college of cardiology/american heart association task force on practice guidelines. J Am Coll Cardiol 63(22):e57–185. https://doi.org/10.1016/j.jacc.2014.02.536. Epub 2014 Mar 3. Erratum in: J Am Coll Cardiol 63(22):2489. Dosage error in article text. PMID: 24603191
Bonow RO, Lakatos E, Maron BJ et al (1991) Serial long-term assessment of the natural history of asymptomatic patients with chronic aortic regurgitation and normal left ventricular systolic function. Circulation 84(4):1625–1635. https://doi.org/10.1161/01.cir.84.4.1625. PMID: 1914102
Braunwald’s Heart Disease (2019) A textbook of cardiovascular medicine (version eleventh edition), eleventh. Elsevier/Saunders, Philadelphia PA
Vasan RS, Larson MG, Benjamin EJ et al (1999) Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population-based cohort. J Am Coll Cardiol 33(7):1948–1955. https://doi.org/10.1016/s0735-1097(99)00118-7. PMID: 10362198
Senni M, Tribouilloy CM, Rodeheffer RJ et al (1998) Congestive heart failure in the community: a study of all incident cases in Olmsted County, Minnesota, in 1991. Circulation 98(21):2282–2289. https://doi.org/10.1161/01.cir.98.21.2282. PMID: 9826315
Gaasch WH, Zile MR (2004) Left ventricular diastolic dysfunction and diastolic heart failure. Annu Rev Med 55:373–394. https://doi.org/10.1146/annurev.med.55.091902.104417. PMID: 14746527
Aurigemma GP, Gaasch WH, McLaughlin M et al (1995) Reduced left ventricular systolic pump performance and depressed myocardial contractile function in patients > 65 years of age with normal ejection fraction and a high relative wall thickness. Am J Cardiol 76(10):702–705. https://doi.org/10.1016/s0002-9149(99)80201-x. PMID: 7572629
Cuocolo A, Sax FL, Brush JE et al (1990) Left ventricular hypertrophy and impaired diastolic filling in essential hypertension. Diastolic mechanisms for systolic dysfunction during exercise. Circulation 81(3):978–86. https://doi.org/10.1161/01.cir.81.3.978. PMID: 2137735
McDonagh TA, Metra M, Adamo M et al (2021) ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 42(36):3599–3726. https://doi.org/10.1093/eurheartj/ehab368. Erratum in: Eur Heart J. 2021 Oct 14; PMID: 34447992
Pellikka PA, Nagueh SF, Elhendy AA et al (2007) American Society of Echocardiography. American Society of Echocardiography recommendations for performance, interpretation, and application of stress echocardiography. J Am Soc Echocardiogr 20(9):1021–41. https://doi.org/10.1016/j.echo.2007.07.003. PMID: 17765820
Sicari R, Nihoyannopoulos P, Evangelista A et al (2008) European Association of Echocardiography. Stress echocardiography expert consensus statement: European Association of Echocardiography (EAE) (a registered branch of the ESC). Eur J Echocardiogr 9(4):415–37. https://doi.org/10.1093/ejechocard/jen175. PMID: 18579481
Picano E (2015) Stress Echocardiography, 6th edn. Springer Verlag, New York
Picano E, Mathias W Jr, Pingitore A et al (1994) Safety and tolerability of dobutamine-atropine stress echocardiography: a prospective, multicentre study. Echo Dobutamine International Cooperative Study Group. Lancet 344(8931):1190–2. https://doi.org/10.1016/s0140-6736(94)90508-8. PMID: 7934540
Lattanzi F, Picano E, Adamo E et al (2000) Dobutamine stress echocardiography: safety in diagnosing coronary artery disease. Drug Saf 22(4):251–262. https://doi.org/10.2165/00002018-200022040-00001. PMID: 10789822
Varga A, Garcia MA, Picano E, International Stress Echo Complication Registry (2006) Safety of stress echocardiography (from the International Stress Echo Complication Registry). Am J Cardiol 98(4):541–3. https://doi.org/10.1016/j.amjcard.2006.02.064. Epub 2006 Jun 28. PMID: 16893714
Kane GC, Hepinstall MJ, Kidd GM et al (2008) Safety of stress echocardiography supervised by registered nurses: results of a 2-year audit of 15,404 patients. J Am Soc Echocardiogr 21(4):337–341. https://doi.org/10.1016/j.echo.2007.08.028. Epub 2007 Sep 29 PMID: 17904811
Novo G, Santoro C, Manno G et al (2021) Usefulness of stress echocardiography in the management of patients treated with anticancer drugs. J Am Soc Echocardiogr 34(2):107–116. https://doi.org/10.1016/j.echo.2020.10.002. Epub 2020 Nov 19 PMID: 33223357
Kelly JP, Andonian BJ, Patel MJ et al (2019) Trends in cardiorespiratory fitness: The evolution of exercise treadmill testing at a single Academic Medical Center from 1970 to 2012. Am Heart J 210:88–97. https://doi.org/10.1016/j.ahj.2019.01.001. Epub 2019 Jan 16. PMID: 30743212; PMCID: PMC6441626
Bombardini T, Costantino MF, Sicari R et al (2013) End-systolic elastance and ventricular-arterial coupling reserve predict cardiac events in patients with negative stress echocardiography. Biomed Res Int 2013:235194. https://doi.org/10.1155/2013/235194. Epub 2013 Aug 19. PMID: 24024185; PMCID: PMC3760182
Cortigiani L, Rigo F, Gherardi S et al (2008) Prognostic implications of coronary flow reserve on left anterior descending coronary artery in hypertrophic cardiomyopathy. Am J Cardiol 102(12):1718–1723. https://doi.org/10.1016/j.amjcard.2008.08.023. Epub 2008 Oct 9 PMID: 19064030
Lowenstein JA, Caniggia C, Rousse G et al (2014) Coronary flow velocity reserve during pharmacologic stress echocardiography with normal contractility adds important prognostic value in diabetic and nondiabetic patients. J Am Soc Echocardiogr 27(10):1113–1119. https://doi.org/10.1016/j.echo.2014.05.009. Epub 2014 Jun 27 PMID: 24984585
Wuthiwaropas P, Wiste JA, McCully RB et al (2011) Neuropsychiatric symptoms during 24 hours after dobutamine-atropine stress testing: a prospective study in 1,006 patients. J Am Soc Echocardiogr 24(4):367–373. https://doi.org/10.1016/j.echo.2010.11.016. Epub 2011 Jan 12 PMID: 21227649
Varga A, Picano E, Lakatos F (2000) Fatal ventricular fibrillation during a low-dose dobutamine stress test. Am J Med 108(4):352–353. https://doi.org/10.1016/s0002-9343(99)00204-1. PMID: 11014735
Poliner LR, Dehmer GJ, Lewis SE et al (1980) Left ventricular performance in normal subjects: a comparison of the responses to exercise in the upright and supine positions. Circulation 62(3):528–534. https://doi.org/10.1161/01.cir.62.3.528. PMID: 7398013
Pratali L, Picano E, Otasevic P et al (2001) Prognostic significance of the dobutamine echocardiography test in idiopathic dilated cardiomyopathy. Am J Cardiol 88(12):1374–1378. https://doi.org/10.1016/s0002-9149(01)02116-6. PMID: 11741555
Pratali L, Otasevic P, Neskovic A et al (2007) Prognostic value of pharmacologic stress echocardiography in patients with idiopathic dilated cardiomyopathy: a prospective, head-to-head comparison between dipyridamole and dobutamine test. J Card Fail 13(10):836–842. https://doi.org/10.1016/j.cardfail.2007.07.011. PMID: 18068617
Gligorova S, Agrusta M (2005) Pacing stress echocardiography. Cardiovasc Ultrasound 9(3):36. https://doi.org/10.1186/1476-7120-3-36.PMID:16336679;PMCID:PMC1334217
Marangelli V, Iliceto S, Piccinni G et al (1994) Detection of coronary artery disease by digital stress echocardiography: comparison of exercise, transesophageal atrial pacing and dipyridamole echocardiography. J Am Coll Cardiol 24(1):117–124. https://doi.org/10.1016/0735-1097(94)90551-7. PMID: 8006254
Hoffmann R, Lethen H, Marwick T et al (1996) Analysis of interinstitutional observer agreement in interpretation of dobutamine stress echocardiograms. J Am Coll Cardiol 27(2):330–336. https://doi.org/10.1016/0735-1097(95)00483-1. PMID: 8557902
Ferro A, Pellegrino T, Spinelli L et al (2007) Comparison between dobutamine echocardiography and single-photon emission computed tomography for interpretive reproducibility. Am J Cardiol 100(8):1239–1244. https://doi.org/10.1016/j.amjcard.2007.05.041. Epub 2007 Jul 19 PMID: 17920364
Picano E, Lattanzi F, Orlandini A et al (1991) Stress echocardiography and the human factor: the importance of being expert. J Am Coll Cardiol 17(3):666–669. https://doi.org/10.1016/s0735-1097(10)80182-2. PMID: 1993786
Sicari R, Nihoyannopoulos P, Evangelista A et al (2009) European Association of Echocardiography. Stress echocardiography expert consensus statement--executive summary: European Association of Echocardiography (EAE) (a registered branch of the ESC). Eur Heart J 30(3):278–89. https://doi.org/10.1093/eurheartj/ehn492. Epub 2008 Nov 11. PMID: 19001473
Geleijnse ML, Fioretti PM, Roelandt JR (1997) Methodology, feasibility, safety and diagnostic accuracy of dobutamine stress echocardiography. J Am Coll Cardiol 30(3):595–606. https://doi.org/10.1016/s0735-1097(97)00206-4. PMID: 9283514
Afridi I, Qureshi U, Kopelen HA et al (1997) Serial changes in response of hibernating myocardium to inotropic stimulation after revascularization: a dobutamine echocardiographic study. J Am Coll Cardiol 30(5):1233–1240. https://doi.org/10.1016/s0735-1097(97)00308-2. PMID: 9350921
Senior R, Lahiri A (1995) Enhanced detection of myocardial ischemia by stress dobutamine echocardiography utilizing the “biphasic” response of wall thickening during low and high dose dobutamine infusion. J Am Coll Cardiol 26(1):26–32. https://doi.org/10.1016/0735-1097(95)00139-q. PMID: 7797760
Solomon SD, Claggett B, Lewis EF et al (2016) Pfeffer MA; TOPCAT Investigators. Influence of ejection fraction on outcomes and efficacy of spironolactone in patients with heart failure with preserved ejection fraction. Eur Heart J 37(5):455–62. https://doi.org/10.1093/eurheartj/ehv464. Epub 2015 Sep 15. PMID: 26374849; PMCID: PMC4751235
Velazquez EJ, Lee KL, Deja MA et al (2011) STICH Investigators. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med 364(17):1607–16. https://doi.org/10.1056/NEJMoa1100356. Epub 2011 Apr 4. PMID: 21463150; PMCID: PMC3415273
Sicari R, Pasanisi E, Venneri L et al (2003) Echo Persantine International Cooperative (EPIC) Study Group; Echo Dobutamine International Cooperative (EDIC) Study Group. Stress echo results predict mortality: a large-scale multicenter prospective international study. J Am Coll Cardiol 41(4):589–95. https://doi.org/10.1016/s0735-1097(02)02863-2. PMID: 12598070
Bax JJ, Poldermans D, Elhendy A et al (2001) Sensitivity, specificity, and predictive accuracies of various noninvasive techniques for detecting hibernating myocardium. Curr Probl Cardiol 26(2):147–186. https://doi.org/10.1067/mcd.2001.109973. PMID: 11276916
Romero J, Xue X, Gonzalez W, Garcia MJ (2012) CMR imaging assessing viability in patients with chronic ventricular dysfunction due to coronary artery disease: a meta-analysis of prospective trials. JACC Cardiovasc Imaging 5(5):494–508. https://doi.org/10.1016/j.jcmg.2012.02.009. PMID: 22595157
Panza JA, Ellis AM, Al-Khalidi HR et al (2019) Myocardial Viability and Long-Term Outcomes in Ischemic Cardiomyopathy. N Engl J Med 381(8):739–748. https://doi.org/10.1056/NEJMoa1807365. PMID: 31433921; PMCID: PMC6814246
Gerber BL, Rousseau MF, Ahn SA et al (2012) Prognostic value of myocardial viability by delayed-enhanced magnetic resonance in patients with coronary artery disease and low ejection fraction: impact of revascularization therapy. J Am Coll Cardiol 59(9):825–835. https://doi.org/10.1016/j.jacc.2011.09.073. PMID: 22361403
Kwon DH, Obuchowski NA, Marwick TH et al (2018) Jeopardized myocardium defined by late gadolinium enhancement magnetic resonance imaging predicts survival in patients with ischemic cardiomyopathy: impact of revascularization. J Am Heart Assoc 7(22):e009394. https://doi.org/10.1161/JAHA.118.009394. PMID:30571486;PMCID:PMC6404459
Kwon DH, Hachamovitch R, Popovic ZB et al (2012) Survival in patients with severe ischemic cardiomyopathy undergoing revascularization versus medical therapy: association with end systolic volume and viability. Circulation 126:S3-8
Underwood SR, Bax JJ, vom Dahl J et al (2004) Study Group of the European Society of Cardiology. Imaging techniques for the assessment of myocardial hibernation. Report of a study group of the european society of cardiology. Eur Heart J 25(10):815–36. https://doi.org/10.1016/j.ehj.2004.03.012. Erratum in: Eur Heart J. 2004 Dec;25(23):2176. PMID: 15140530
Orlandini A, Castellana N, Pascual A et al (2015) Myocardial viability for decision-making concerning revascularization in patients with left ventricular dysfunction and coronary artery disease: a meta-analysis of non-randomized and randomized studies. Int J Cardiol 1(182):494–499. https://doi.org/10.1016/j.ijcard.2015.01.025. Epub 2015 Jan 7 PMID: 25617608
Cleland JG, Calvert M, Freemantle N et al (2011) The Heart Failure Revascularisation Trial (HEART). Eur J Heart Fail 13(2):227–233. https://doi.org/10.1093/eurjhf/hfq230. Epub 2010 Dec 13 PMID: 21156659
Bonow RO, Maurer G, Lee KL et al (2011) STICH Trial Investigators. Myocardial viability and survival in ischemic left ventricular dysfunction. N Engl J Med 364(17):1617–25. https://doi.org/10.1056/NEJMoa1100358. Epub 2011 Apr 4. PMID: 21463153; PMCID: PMC3290901
Beanlands RS, Nichol G, Huszti E et al (2007) PARR-2 Investigators. F-18-fluorodeoxyglucose positron emission tomography imaging-assisted management of patients with severe left ventricular dysfunction and suspected coronary disease: a randomized, controlled trial (PARR-2). J Am Coll Cardiol 50(20):2002–12. https://doi.org/10.1016/j.jacc.2007.09.006. Epub 2007 Oct 10. PMID: 17996568
Shah BN, Khattar RS, Senior R (2013) The hibernating myocardium: current concepts, diagnostic dilemmas, and clinical challenges in the post-STICH era. Eur Heart J 34(18):1323–1336. https://doi.org/10.1093/eurheartj/eht018. Epub 2013 Feb 17 PMID: 23420867
Almeida AG, Carpenter JP, Cameli M et al (2021) Reviewers: This document was reviewed by members of the 2018–2020 EACVI Scientific Documents Committee:; chair of the 2018–2020 EACVI Scientific Documents Committee:; 2018–2020 EACVI President: Multimodality imaging of myocardial viability: an expert consensus document from the European Association of Cardiovascular Imaging (EACVI). Eur Heart J Cardiovasc Imaging 22(8):e97–e125. https://doi.org/10.1093/ehjci/jeab053. PMID: 34097006
Marwick TH, Case C, Sawada S et al (2001) Prediction of mortality using dobutamine echocardiography. J Am Coll Cardiol 37(3):754–760. https://doi.org/10.1016/s0735-1097(00)01191-8. PMID: 11693748
Ryerson AB, Border WL, Wasilewski-Masker K et al (2015) Assessing anthracycline-treated childhood cancer survivors with advanced stress echocardiography. Pediatr Blood Cancer 62(3):502–508. https://doi.org/10.1002/pbc.25328. Epub 2014 Nov 12 PMID: 25393686
Civelli M, Cardinale D, Martinoni A et al (2006) Early reduction in left ventricular contractile reserve detected by dobutamine stress echo predicts high-dose chemotherapy-induced cardiac toxicity. Int J Cardiol 111(1):120–126. https://doi.org/10.1016/j.ijcard.2005.07.029. Epub 2005 Oct 20 PMID: 16242796
Cheung YF, Yu W, Li SN et al (2012) Dynamic dyssynchrony and impaired contractile reserve of the left ventricle in beta-thalassaemia major: an exercise echocardiographic study. PLoS One 7(9):e45265. https://doi.org/10.1371/journal.pone.0045265. Epub 2012 Sep 18. PMID: 23028894; PMCID: PMC3445473
Park S, Seo HS, Shim CY et al (2008) Effect of geometric remodeling on left ventricular longitudinal contractile reserve in patients with hypertension. J Am Soc Echocardiogr 21(3):246–250. https://doi.org/10.1016/j.echo.2007.06.005. Epub 2007 Jul 20 PMID: 17658727
Galderisi M, de Simone G, Innelli P et al (2007) Impaired inotropic response in type 2 diabetes mellitus: a strain rate imaging study. Am J Hypertens 20(5):548–555. https://doi.org/10.1016/j.amjhyper.2006.12.009. PMID: 17485020
Agricola E, Oppizzi M, Pisani M et al (2004) Stress echocardiography in heart failure. Cardiovasc Ultrasound 30(2):11. https://doi.org/10.1186/1476-7120-2-11. PMID: 15285780; PMCID: PMC514499
Zile MR, Kjellstrom B, Bennett T et al (2013) Effects of exercise on left ventricular systolic and diastolic properties in patients with heart failure and a preserved ejection fraction versus heart failure and a reduced ejection fraction. Circ Heart Fail 6(3):508–516. https://doi.org/10.1161/CIRCHEARTFAILURE.112.000216. Epub 2013 Mar 20 PMID: 23515277
Borlaug BA, Melenovsky V, Russell SD et al (2006) Impaired chronotropic and vasodilator reserves limit exercise capacity in patients with heart failure and a preserved ejection fraction. Circulation 114(20):2138–2147. https://doi.org/10.1161/CIRCULATIONAHA.106.632745. Epub 2006 Nov 6 PMID: 17088459
Cifra B, Dragulescu A, Brun H et al (2014) Left ventricular myocardial response to exercise in children after heart transplant. J Heart Lung Transplant 33(12):1241–1247. https://doi.org/10.1016/j.healun.2014.07.011. Epub 2014 Jul 21 PMID: 25130553
Sebbag L, Bergerot C, Jamal F et al (2003) Alteration of the left ventricular contractile reserve in heart transplant patients: a dobutamine stress strain rate imaging study. Transplant Proc 35(8):3072–3074. https://doi.org/10.1016/j.transproceed.2003.10.018. PMID: 14697982
Nagueh SF, Mikati I, Weilbaecher D et al (1999) Relation of the contractile reserve of hibernating myocardium to myocardial structure in humans. Circulation 100(5):490–496. https://doi.org/10.1161/01.cir.100.5.490. PMID: 10430762
Paraskevaidis IA, Adamopoulos S, Kremastinos DT (2001) Dobutamine echocardiographic study in patients with nonischemic dilated cardiomyopathy and prognostically borderline values of peak exercise oxygen consumption: 18-month follow-up study. J Am Coll Cardiol 37(6):1685–1691. https://doi.org/10.1016/s0735-1097(01)01194-9. PMID: 11345385
Scrutinio D, Napoli V, Passantino A et al (2000) Low-dose dobutamine responsiveness in idiopathic dilated cardiomyopathy: relation to exercise capacity and clinical outcome. Eur Heart J 21(11):927–934. https://doi.org/10.1053/euhj.1999.1937. PMID: 10806017
Rigo F, Gherardi S, Galderisi M et al (2007) The independent prognostic value of contractile and coronary flow reserve determined by dipyridamole stress echocardiography in patients with idiopathic dilated cardiomyopathy. Am J Cardiol 99(8):1154–1158. https://doi.org/10.1016/j.amjcard.2006.11.049. Epub 2007 Mar 5 PMID: 17437747
Pratali L, Otasevic P, Rigo F et al (2005) The additive prognostic value of restrictive pattern and dipyridamole-induced contractile reserve in idiopathic dilated cardiomyopathy. Eur J Heart Fail 7(5):844–851. https://doi.org/10.1016/j.ejheart.2004.10.010. PMID: 16087138
Miglioranza MH, Gargani L, Sant’Anna RT et al (2013) Lung ultrasound for the evaluation of pulmonary congestion in outpatients: a comparison with clinical assessment, natriuretic peptides, and echocardiography. JACC Cardiovasc Imaging 6(11):1141–1151. https://doi.org/10.1016/j.jcmg.2013.08.004. Epub 2013 Oct 2 PMID: 24094830
Picano E, Frassi F, Agricola E et al (2006) Ultrasound lung comets: a clinically useful sign of extravascular lung water. J Am Soc Echocardiogr 19(3):356–363. https://doi.org/10.1016/j.echo.2005.05.019. PMID: 16500505
Agricola E, Picano E, Oppizzi M et al (2006) Assessment of stress-induced pulmonary interstitial edema by chest ultrasound during exercise echocardiography and its correlation with left ventricular function. J Am Soc Echocardiogr 19(4):457–463. https://doi.org/10.1016/j.echo.2005.11.013. PMID: 16581487
Zagatina A, Zhuravskaya N, Shmatov D et al (2020) Stress Echo 2020 study group of the Italian society of echocardiography, cardiovascular imaging. Exercise stress echocardiography with ABCDE protocol in unexplained dyspnoea. Int J Cardiovasc Imaging 36(5):823–831. https://doi.org/10.1007/s10554-020-01789-6. Epub 2020 Feb 8. PMID: 32036487
Picano E, Zagatina A, Wierzbowska-Drabik K et al (2020) Sustainability and Versatility of the ABCDE Protocol for Stress Echocardiography. J Clin Med 9(10):3184. https://doi.org/10.3390/jcm9103184. PMID: 33008112; PMCID: PMC7601661
Picano E, Ciampi Q, Cortigiani L et al (2021) The stress echo study group of the Italian society of echocardiography and cardiovascular imaging siecvi. Stress echo 2030: The novel ABCDE-(FGLPR) protocol to define the future of imaging. J Clin Med 10(16):3641. https://doi.org/10.3390/jcm10163641. PMID: 34441937; PMCID: PMC8397117
Ha JW, Oh JK, Pellikka PA et al (2005) Diastolic stress echocardiography: a novel noninvasive diagnostic test for diastolic dysfunction using supine bicycle exercise Doppler echocardiography. J Am Soc Echocardiogr 18(1):63–68. https://doi.org/10.1016/j.echo.2004.08.033. PMID: 15637491
Burgess MI, Jenkins C, Sharman JE et al (2006) Diastolic stress echocardiography: hemodynamic validation and clinical significance of estimation of ventricular filling pressure with exercise. J Am Coll Cardiol 47(9):1891–1900. https://doi.org/10.1016/j.jacc.2006.02.042. Epub 2006 Apr 3 PMID: 16682317
Nagueh SF, Smiseth OA, Appleton CP et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the american society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr 29(4):277–314. https://doi.org/10.1016/j.echo.2016.01.011. PMID: 27037982
Pieske B, Tschöpe C, de Boer RA et al (2019) How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur Heart J 40(40):3297–3317. https://doi.org/10.1093/eurheartj/ehz641. Erratum. In: Eur Heart J 42(13):1274 . PMID: 31504452
Henein MY, Tossavainen E, A’roch R et al (2019) Can Doppler echocardiography estimate raised pulmonary capillary wedge pressure provoked by passive leg lifting in suspected heart failure? Clin Physiol Funct Imaging 39(2):128–134. https://doi.org/10.1111/cpf.12547. Epub 2018 Oct 8 PMID: 30298591
Mullens W, Borowski AG, Curtin RJ et al (2009) Tissue Doppler imaging in the estimation of intracardiac filling pressure in decompensated patients with advanced systolic heart failure. Circulation 119(1):62–70. https://doi.org/10.1161/CIRCULATIONAHA.108.779223. Epub 2008 Dec 15. PMID: 19075104; PMCID: PMC3169300
Chen ZW, Huang CY, Cheng JF et al (2019) Stress echocardiography-derived e/e’ predicts abnormal exercise hemodynamics in heart failure with preserved ejection fraction. Front Physiol 3(10):1470. https://doi.org/10.3389/fphys.2019.01470.PMID:31849715;PMCID:PMC6901703. PMCID: PMC6901703
Harada T, Obokata M, Kagami K et al (2022) Utility of e/e' ratio during low-level exercise to diagnose heart failure with preserved ejection fraction. JACC Cardiovasc Imaging S1936–878X(22)00666–0. https://doi.org/10.1016/j.jcmg.2022.10.024. Epub ahead of print. PMID: 36752422
Erdei T, Smiseth OA, Marino P et al (2014) A systematic review of diastolic stress tests in heart failure with preserved ejection fraction, with proposals from the EU-FP7 MEDIA study group. Eur J Heart Fail 16(12):1345–1361. https://doi.org/10.1002/ejhf.184. Epub 2014 Nov 12 PMID: 25393338
Nagueh SF, Middleton KJ, Kopelen HA et al (1997) Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 30(6):1527–1533. https://doi.org/10.1016/s0735-1097(97)00344-6. PMID: 9362412
Park JH, Marwick TH (2011) Use and Limitations of E/e' to Assess Left Ventricular Filling Pressure by Echocardiography. J Cardiovasc Ultrasound 19(4):169–73. https://doi.org/10.4250/jcu.2011.19.4.169. Epub 2011 Dec 27. PMID: 22259658; PMCID: PMC3259539
Gola A, Pozzoli M, Capomolla S et al (1996) Comparison of Doppler echocardiography with thermodilution for assessing cardiac output in advanced congestive heart failure. Am J Cardiol 78(6):708–712. https://doi.org/10.1016/s0002-9149(96)00406-7. PMID: 8831417
Pozzoli M, Capomolla S, Cobelli F et al (1995) Reproducibility of Doppler indices of left ventricular systolic and diastolic function in patients with severe chronic heart failure. Eur Heart J 16(2):194–200. https://doi.org/10.1093/oxfordjournals.eurheartj.a060885. PMID: 7744091
Kusunose K, Yamada H, Nishio S et al (2019) Pulmonary artery hypertension-specific therapy improves exercise tolerance and outcomes in exercise-induced pulmonary hypertension. JACC Cardiovasc Imaging 12(12):2576–2579. https://doi.org/10.1016/j.jcmg.2019.07.002. Epub 2019 Aug 14 PMID: 31422131
Keusch S, Bucher A, Müller-Mottet S et al (2014) Experience with exercise right heart catheterization in the diagnosis of pulmonary hypertension: a retrospective study. Multidiscip Respir Med 9(1):51. https://doi.org/10.1186/2049-6958-9-51. PMID: 25352986; PMCID: PMC4210570
Obokata M, Kane GC, Reddy YN et al (2017) Role of diastolic stress testing in the evaluation for heart failure with preserved ejection fraction: a simultaneous invasive-echocardiographic study. Circulation 135(9):825–838. https://doi.org/10.1161/CIRCULATIONAHA.116.024822. Epub 2016 Dec 30. PMID: 28039229; PMCID: PMC5330848
Eisman AS, Shah RV, Dhakal BP et al (2018) Pulmonary capillary wedge pressure patterns during exercise predict exercise capacity and incident heart failure. Circ Heart Fail 11(5):e004750. https://doi.org/10.1161/CIRCHEARTFAILURE.117.004750. PMID: 29695381; PMCID: PMC5937988
Abe Y, Akamatsu K, Furukawa A et al (2017) Pre-Load-Induced Changes in Forward LV Stroke and Functional Mitral Regurgitation: Echocardiographic Detection of the Descending Limb of Starling’s Curve. JACC Cardiovasc Imaging 10(6):611–618. https://doi.org/10.1016/j.jcmg.2016.07.010. Epub 2016 Nov 16 PMID: 27865719
Ha JW, Lulic F, Bailey KR et al (2003) Effects of treadmill exercise on mitral inflow and annular velocities in healthy adults. Am J Cardiol 91(1):114–115. https://doi.org/10.1016/s0002-9149(02)03016-3. PMID: 12505590
Oh JK, Kane GC (2014) Diastolic stress echocardiography: the time has come for its integration into clinical practice. J Am Soc Echocardiogr 27(10):1060–1063. https://doi.org/10.1016/j.echo.2014.08.013. PMID: 25249511
Kane GC, Sachdev A, Villarraga HR et al (2016) Impact of age on pulmonary artery systolic pressures at rest and with exercise. Echo Res Pract 3(2):53–61. https://doi.org/10.1530/ERP-16-0006. PMID: 27343212; PMCID: PMC4989097
Ha JW, Choi D, Park S et al (2009) Determinants of exercise-induced pulmonary hypertension in patients with normal left ventricular ejection fraction. Heart 95(6):490–494. https://doi.org/10.1136/hrt.2007.139295. Epub 2008 Jul 24 PMID: 18653569
Writing Committee Members, Otto CM, Nishimura RA, Bonow RO et al (2021) 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the american college of cardiology/american heart association joint committee on clinical practice guidelines. J Am Coll Cardiol. 2021 Feb 2;77(4):e25-e197. https://doi.org/10.1016/j.jacc.2020.11.018. Epub 2020 Dec 17. Erratum in: J Am Coll Cardiol. 77(4):509. Erratum in: J Am Coll Cardiol. 2021 Mar 9;77(9):1275. PMID: 33342586
Garbi M, Chambers J, Vannan MA et al (2015) Valve stress echocardiography: a practical guide for referral, procedure, reporting, and clinical implementation of results from the havec group. JACC Cardiovasc Imaging 8(6):724–736. https://doi.org/10.1016/j.jcmg.2015.02.010. PMID: 26068289
Piérard LA, Lancellotti P (2004) The role of ischemic mitral regurgitation in the pathogenesis of acute pulmonary edema. N Engl J Med 351(16):1627–1634. https://doi.org/10.1056/NEJMoa040532. PMID: 15483281
Merli E, Ciampi Q, Scali MC et al (2022) Stress echo 2020 and 2030 study group of the Italian Society of Echocardiography and Cardiovascular Imaging (SIECVI). Pulmonary congestion during exercise stress echocardiography in ischemic and heart failure patients. Circ Cardiovasc Imaging 15(5):e013558. https://doi.org/10.1161/CIRCIMAGING.121.013558. Epub 2022 May 17. PMID: 35580160
Magne J, Lancellotti P, Piérard LA (2010) Exercise pulmonary hypertension in asymptomatic degenerative mitral regurgitation. Circulation 122(1):33–41. https://doi.org/10.1161/CIRCULATIONAHA.110.938241. Epub 2010 Jun 21 PMID: 20566950
Kusunose K, Popović ZB, Motoki H et al (2013) Prognostic significance of exercise-induced right ventricular dysfunction in asymptomatic degenerative mitral regurgitation. Circ Cardiovasc Imaging 6(2):167–176. https://doi.org/10.1161/CIRCIMAGING.112.000162. Epub 2013 Jan 28 PMID: 23357242
Lancellotti P, Pibarot P, Chambers J et al (2022) Scientific Document Committee of the European Association of Cardiovascular Imaging. Multi-modality imaging assessment of native valvular regurgitation: an EACVI and ESC council of valvular heart disease position paper. Eur Heart J Cardiovasc Imaging 23(5):e171-e232. https://doi.org/10.1093/ehjci/jeab253. PMID: 35292799
Johnson C, Kuyt K, Oxborough D et al (2019) Practical tips and tricks in measuring strain, strain rate and twist for the left and right ventricles. Echo Res Pract 6(3):R87–R98. https://doi.org/10.1530/ERP-19-0020. PMID: 31289687; PMCID: PMC6612062
Vitel E, Galli E, Leclercq C et al (2018) Right ventricular exercise contractile reserve and outcomes after early surgery for primary mitral regurgitation. Heart 104(10):855–860. https://doi.org/10.1136/heartjnl-2017-312097. Epub 2017 Dec 5 PMID: 29208632
Cameli M, Pastore MC, Campora A et al (2022) Donor shortage in heart transplantation: How can we overcome this challenge? Front Cardiovasc Med 17(9):1001002. https://doi.org/10.3389/fcvm.2022.1001002. PMID: 36324743; PMCID: PMC9618685
Bombardini T, Gherardi S, Leone O et al (2013) Transplant of stunned donor hearts rescued by pharmacological stress echocardiography: a “proof of concept” report. Cardiovasc Ultrasound 2(11):27. https://doi.org/10.1186/1476-7120-11-27. PMID: 23915276; PMCID: PMC3735394
Mandoli GE, Barilli M, Soviero D, Ghionzoli N, Landra F, Maccherini M, Bernazzali S, Natali BM, Focardi M, Cavigli L, D’Ascenzi F, Pastore MC, Sciaccaluga C, Bombardini T, Valente S, Cameli M (2023) ADONHERS (Aged DONor HEart Rescue by Stress Echo) National Protocol: Recipient’s Survival after 10-Year Follow-Up. J Clin Med 12(10):3505. https://doi.org/10.3390/jcm12103505. PMID: 37240611; PMCID: PMC10218963
Cameli M, Bombardini T, Dokollari A et al (2016) Longitudinal Strain Stress-Echo Evaluation of Aged Marginal Donor Hearts: Feasibility in the Adonhers Project. Transplant Proc 48(2):399–401. https://doi.org/10.1016/j.transproceed.2015.12.036. PMID: 27109965
Moir S, Shaw L, Haluska B et al (2007) Left ventricular opacification for the diagnosis of coronary artery disease with stress echocardiography: an angiographic study of incremental benefit and cost-effectiveness. Am Heart J 154(3):510–518. https://doi.org/10.1016/j.ahj.2007.04.046. PMID: 17719299
Dolan MS, Riad K, El-Shafei A et al (2001) Effect of intravenous contrast for left ventricular opacification and border definition on sensitivity and specificity of dobutamine stress echocardiography compared with coronary angiography in technically difficult patients. Am Heart J 142(5):908–915. https://doi.org/10.1067/mhj.2001.117608. PMID: 11685180
Jayaweera AR, Edwards N, Glasheen WP et al (1994) In vivo myocardial kinetics of air-filled albumin microbubbles during myocardial contrast echocardiography. Comparison with radiolabeled red blood cells. Circ Res 74(6):1157–65. https://doi.org/10.1161/01.res.74.6.1157. PMID: 8187282
Keller MW, Segal SS, Kaul S et al (1989) The behavior of sonicated albumin microbubbles within the microcirculation: a basis for their use during myocardial contrast echocardiography. Circ Res 65(2):458–467. https://doi.org/10.1161/01.res.65.2.458. PMID: 2752551
Wei K, Jayaweera AR, Firoozan S et al (1998) Quantification of myocardial blood flow with ultrasound-induced destruction of microbubbles administered as a constant venous infusion. Circulation 97(5):473–483. https://doi.org/10.1161/01.cir.97.5.473. PMID: 9490243
Anantharam B, Janardhanan R, Hayat S et al (2011) Coronary flow reserve assessed by myocardial contrast echocardiography predicts mortality in patients with heart failure. Eur J Echocardiogr 12(1):69–75. https://doi.org/10.1093/ejechocard/jeq109. Epub 2010 Sep 6 PMID: 20819838
Chelliah R, Whyte G, Whyte S et al (2013) Myocardial contrast echocardiography distinguishes physiological from pathological grey-zone left ventricular hypertrophy. Heart. 99:A62-A62. https://doi.org/10.1136/heartjnl-2013-304019.99
Galiuto L, De Caterina AR, Porfidia A et al (2010) Reversible coronary microvascular dysfunction: a common pathogenetic mechanism in Apical Ballooning or Tako-Tsubo Syndrome. Eur Heart J 31(11):1319–1327. https://doi.org/10.1093/eurheartj/ehq039. Epub 2010 Mar 9 PMID: 20215125
Mandoli GE, Pastore MC, Vasilijevaite K et al (2020) Speckle tracking stress echocardiography: A valuable diagnostic technique or a burden for everyday practice? Echocardiography 37(12):2123–2129. https://doi.org/10.1111/echo.14894. Epub 2020 Nov 4 PMID: 33145829
Mor-Avi V, Lang RM, Badano LP et al (2011) Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. J Am Soc Echocardiogr 24(3):277–313. https://doi.org/10.1016/j.echo.2011.01.015. PMID: 21338865
Cavalcante JL, Collier P, Plana JC et al (2012) Two-dimensional longitudinal strain assessment in the presence of myocardial contrast agents is only feasible with speckle-tracking after microbubble destruction. J Am Soc Echocardiogr 25(12):1309–1318. https://doi.org/10.1016/j.echo.2012.09.019. Epub 2012 Oct 24 PMID: 23102836
Nagy AI, Sahlén A, Manouras A et al (2015) Combination of contrast-enhanced wall motion analysis and myocardial deformation imaging during dobutamine stress echocardiography. Eur Heart J Cardiovasc Imaging 16(1):88–95. https://doi.org/10.1093/ehjci/jeu171. Epub 2014 Sep 3 PMID: 25187604
Yamada A, Luis SA, Sathianathan et al (2014) Reproducibility of regional and global longitudinal strains derived from two-dimensional speckle-tracking and doppler tissue imaging between expert and novice readers during quantitative dobutamine stress echocardiography. J Am Soc Echocardiogr 27(8):880–7. https://doi.org/10.1016/j.echo.2014.04.016. Epub 2014 Jun 2. PMID: 24891261
Mandoli GE, Cameli M, Minardi S et al (2018) Layer-specific strain in dipyridamole stress echo: A new tool for the diagnosis of microvascular angina. Echocardiography 35(12):2005–2013. https://doi.org/10.1111/echo.14180. Epub 2018 Nov 5 PMID: 30394569
Gong L, Li D, Chen J et al (2013) Assessment of myocardial viability in patients with acute myocardial infarction by two-dimensional speckle tracking echocardiography combined with low-dose dobutamine stress echocardiography. Int J Cardiovasc Imaging 29(5):1017–1028. https://doi.org/10.1007/s10554-013-0185-y. Epub 2013 Jan 29 PMID: 23358919
Voigt JU, Exner B, Schmiedehausen K et al (2003) Strain-rate imaging during dobutamine stress echocardiography provides objective evidence of inducible ischemia. Circulation 107(16):2120–2126. https://doi.org/10.1161/01.CIR.0000065249.69988.AA. Epub 2003 Apr 7 PMID: 12682001
Pastore MC, Mandoli GE, Contorni F et al (2021) Speckle Tracking Echocardiography: Early Predictor of Diagnosis and Prognosis in Coronary Artery Disease. Biomed Res Int 2(2021):6685378. https://doi.org/10.1155/2021/6685378. PMID: 33623788; PMCID: PMC7875622
Dahou A, Bartko PE, Capoulade R et al (2015) Usefulness of global left ventricular longitudinal strain for risk stratification in low ejection fraction, low-gradient aortic stenosis: results from the multicenter True or Pseudo-Severe Aortic Stenosis study. Circ Cardiovasc Imaging 8(3):e002117. https://doi.org/10.1161/CIRCIMAGING.114.002117. PMID: 25681417
Badran HM, Faheem N, Ibrahim WA et al (2013) Systolic function reserve using two-dimensional strain imaging in hypertrophic cardiomyopathy: comparison with essential hypertension. J Am Soc Echocardiogr 26(12):1397–1406. https://doi.org/10.1016/j.echo.2013.08.026. Epub 2013 Oct 3 PMID: 24094559
Vitarelli A, Cortes Morichetti M et al (2013) Utility of strain echocardiography at rest and after stress testing in arrhythmogenic right ventricular dysplasia. Am J Cardiol 111(9):1344–1350. https://doi.org/10.1016/j.amjcard.2013.01.279. Epub 2013 Feb 11 PMID: 23411103
Matsumoto K, Tanaka H, Imanishi J et al (2014) Preliminary observations of prognostic value of left atrial functional reserve during dobutamine infusion in patients with dilated cardiomyopathy. J Am Soc Echocardiogr 27(4):430–439. https://doi.org/10.1016/j.echo.2013.12.016. Epub 2014 Jan 31 PMID: 24491673
Benfari G, Mandoli GE, Magne J et al (2022) MASCOT investigators. Left atrial strain determinants and clinical features according to the heart failure stages. New insight from EACVI MASCOT registry. Int J Cardiovasc Imaging. 38(12):2635–2644. https://doi.org/10.1007/s10554-022-02669-x. Epub 2022 Jul 1. PMID: 36445656; PMCID: PMC9708811
Takagi T, Takagi A, Yoshikawa J (2010) Detection of coronary artery disease using delayed strain imaging at 5 min after the termination of exercise stress: head to head comparison with conventional treadmill stress echocardiography. J Cardiol 55(1):41–48. https://doi.org/10.1016/j.jjcc.2009.08.001. Epub 2009 Sep 20 PMID: 20122547
Yoshitani H, Takeuchi M, Mor-Avi V et al (2009) Comparative diagnostic accuracy of multiplane and multislice three-dimensional dobutamine stress echocardiography in the diagnosis of coronary artery disease. J Am Soc Echocardiogr 22(5):437–442. https://doi.org/10.1016/j.echo.2009.02.005. PMID: 19307099
Aggeli C, Giannopoulos G, Misovoulos P et al (2007) Real-time three-dimensional dobutamine stress echocardiography for coronary artery disease diagnosis: validation with coronary angiography. Heart. 93(6):672–5. https://doi.org/10.1136/hrt.2006.101220. Epub 2006 Nov 3. PMID: 17085530; PMCID: PMC1955206
Badano LP, Muraru D, Rigo F et al (2010) High volume-rate three-dimensional stress echocardiography to assess inducible myocardial ischemia: a feasibility study. J Am Soc Echocardiogr 23(6):628–635. https://doi.org/10.1016/j.echo.2010.03.020. PMID: 20434877
Funding
Open access funding provided by Università degli Studi di Siena within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Consortia
Contributions
Drs. Maria Concetta Pastore, Prof. Michael Henein, Prof. Matteo Cameli, Dr. Antonello D’Andrea contributed to this review conception; Drs. Maria Concetta Pastore and Alessandro Campora performed the literature search and data analysis and drafted the manuscript, Drs. Giulia Elena Mandoli, Matteo Lisi, Giovanni Benfari, Federica Ilardi, Alessandro Malagoli, Simona Sperlongano, Prof. Michael Y Henein, Prof. Matteo Cameli, Dr. Antonello D’Andrea critically revised the work and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent for publication
All the authors have read and approved the final version of the manuscript and gave their consent for publication.
Competing interest
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pastore, M.C., Campora, A., Mandoli, G.E. et al. Stress echocardiography in heart failure patients: additive value and caveats. Heart Fail Rev (2024). https://doi.org/10.1007/s10741-024-10423-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s10741-024-10423-9