Abstract
Dilated cardiomyopathy (DCM) is a primary heart muscle disease characterized by left or biventricular systolic impairment. Historically, most of the clinical attention has been devoted to the evaluation of left ventricular function and morphology, while right ventricle (RV) has been for many years the forgotten chamber. Recently, progresses in cardiac imaging gave clinicians precious tools for the evaluation of RV, raising the awareness of the importance of biventricular assessment in DCM. Indeed, RV involvement is far from being uncommon in DCM, and the presence of right ventricular dysfunction (RVD) is one of the major negative prognostic determinants in DCM patients. However, some aspects such as the possible role of specific genetic mutations in determining the biventricular phenotype in DCM, or the lack of specific treatments able to primarily counteract RVD, still need research. In this review, we summarized the current knowledge on RV involvement in DCM, giving an overview on the epidemiology and pathogenetic mechanisms implicated in determining RVD. Furthermore, we discussed the imaging techniques to evaluate RV function and the role of RV failure in advanced heart failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dilated cardiomyopathy (DCM) is a primary heart muscle disease defined as the impairment of left or biventricular systolic function, often associated with dilation, in absence of coronary artery disease or valvular heart disease [1]. Left ventricular (LV) morphology and function have been the predominant field of interests of clinicians, while a relatively few evidence was available about the significance of right ventricular (RV) involvement in DCM [2, 3]. Indeed, the right ventricle (RV) has been the “forgotten” chamber in the evaluation of DCM and, more in general, heart failure (HF) patients. This depends on various reasons and might be partially explained by the challenges imposed by RV anatomy and function, with clear limitations affecting its evaluation.
However, in the last years, we have faced a new renaissance for the RV. Progresses in cardiac imaging, mainly due to the advent of cardiac magnetic resonance (CMR) and the implementation of speckle tracking and 3D echocardiography, showed that RV involvement is common in DCM [2, 4,5,6,7,8], carrying important prognostic and therapeutic implications [2, 3, 9]. These elements highlight the importance of an accurate and serial evaluation of RV in all DCM patients, with a particular focus on its dynamic behavior during the course of the disease [3, 10].
In this review, we highlight the epidemiology, the pathogenetic mechanisms, and the possible best management of RV involvement in DCM patients. Furthermore, we discussed the imaging techniques to evaluate RV function and the role of RV failure in advanced heart failure. We also focused on the imaging techniques available for a multimodality RV assessment, along with the prognostic implications of RV impairment in specific settings of DCM.
Epidemiology and pathogenesis
The prevalence of right ventricular dysfunction (RVD) in DCM varied in previous reports, ranging from 20 to 65%, and approaching 30% in the most recent series [2, 3, 8,9,10] (Table 1). Genetics play a key role in DCM but, apparently, the prevalence of RVD at diagnosis is similar between genetic and non-genetic forms [10]. Importantly, during the follow-up, a significant percentage of patients improve their RV function and the prevalence of RVD is generally lower in the natural history of the disease, with approximately 80% of patients normalizing their RV function under guideline medical treatment (GDMT) [3].
Several mechanisms might be involved in the pathogenesis of RVD in DCM (Fig. 1). The most common one is related to the complex interventricular relationship. The systo-diastolic impairment of the LV, increased LV filling pressure, and relevant mitral regurgitation (MR) might in turn increase the pulmonary pressure. These factors lead to a type 2 pulmonary hypertension and consequently chronic pressure overload of the RV, which culminates in RV dilation and dysfunction [11]. Optimizing loading conditions with the implementation of loop diuretics and counteracting the detrimental activation of the sympathetic and renin-angiotensin system with GDMT usually have a positive effect on the RV function [12].
While the latter mechanism is common in all forms of heart failure with reduced ejection fraction (HFrEF), in DCM the presence of RVD might also be determined by a primary cardiomyopathic process, leading to an impaired RV myocardial contractility [13]. This specific mechanism could probably be more frequent in some specific genetic etiologies of DCM, such as pathogenic mutations in desmosomal genes, Desmin (DESM), Filamin C (FLNC), and Lamin (LMNA) genes, leading to an overlap between the DCM phenotype and specific forms of arrhythmogenic cardiomyopathy (AC) with biventricular involvement [14, 15]. RVD is usually involved in the so-called AC, irrespectively from the hemodynamic status and LV impairment, or it can develop during the long term of the disease as a progress of the cardiomyopathic process [15].
Further contributors to RVD may be the decreased RV coronary perfusion by a failing LV [16], as well as LV dilation in a restricted pericardial compartment that may limit RV diastolic function [17].
All these aforementioned mechanisms are not mutually exclusive. A complex interplay can be present in the same patient and a comprehensive evaluation is therefore mandatory to implement individualized solutions.
Role of cardiac imaging in the assessment of right ventricular function
Great progresses in cardiac imaging have been observed in the last years relatively to the RV function assessment (Table 2). In the past, the evaluation of RV was limited to gross data derived from chest X-ray [18] or to those derived by invasive, time-consuming, and radiation-based procedures such as RV angiography or radionuclide-based techniques [19].
Standard echocardiography provides clinicians with a simple, fast, non-invasive, and widely available method to study RV function. However, the anterior position in the chest of RV, its complex geometric shape, and function limit the accuracy of the echocardiographic-derived measures [20].
The more frequently considered parameters in the evaluation of RV function are the tricuspidal annulus plane systolic excursion (TAPSE), the right ventricular fractional area change (RVFAC), and the tricuspid lateral annular systolic velocity (S’).
TAPSE evaluates the longitudinal RV function measured with the M-mode in the apical 4-chamber view [21]. A value of less than 1.7 cm indicates RV dysfunction [22]. Although widely adopted and simple to measure, it shows clear limitations, reflecting only the longitudinal function of the basal RV wall, possibly overestimating or underestimating RVD in specific settings [23]. Specifically, the value of TAPSE in patients who underwent previous cardiac surgery is usually underestimated and it manifests important drawbacks in this setting [24].
RVFAC is a 2D measure obtained in the RV-focused apical 4-chamber view by manually tracing the endocardial RV borders at end-diastole and end-systole [22]. In comparison to TAPSE, RVFAC offers a more comprehensive evaluation of RV function, even though the RV outflow tract is not considered due to the particular anatomy of RV. A value ≥ 35% of RVFAC is considered normal in adults [22]. An important limitation to the assessment of RVFAC is represented by the prominent trabeculations of the RV, making border definitions particularly challenging [20]. However, previous studies showed that RVFAC might be the 2D echocardiographic parameter with the best correlation with RVEF determined by CMR [25, 26].
The S’ velocity reproduces the tissue Doppler systolic velocity of the tricuspid annulus, being similar to TAPSE, a measure of longitudinal RV function [23]. A value of S’ < 9.5 cm/s is considered the cut-off to identify RVD. It presents the same limitations of TAPSE, including angle and load dependency [27].
Among the abovementioned parameters, S’ appears to be the best potential earlier marker of RVD [28].
Another advantage of standard echocardiography is the possible simultaneous acquisition of hemodynamic information of the right heart through Doppler flow measurements [23]. Of interest is the systolic pulmonary artery pressure (sPAP) that might be estimated by the tricuspid regurgitation (TR) peak velocity [23]. This information could be crucial in differentiating RVD derived from high LV filling pressure (in case of high sPAP, typically ischemic heart disease) or RVD derived from direct cardiomyopathic RV involvement (possible presence of low sPAP) [8].
Advanced echocardiography and cardiac magnetic resonance
Recently, new techniques of advanced echocardiography have shown promising potential value in implementing the information derived from standard echocardiography. Speckle tracking two-dimensional (2D) analysis is able to detect subtle abnormalities of RV function in presence of normal standard echocardiographic assessment, and it is relatively load and angle independent compared to standard parameters [29,30,31]. Previous experiences suggested that right ventricular global longitudinal strain (RVGLS) has better correlation with RVEF calculated by CMR and with major cardiovascular (CV) outcomes compared to standard echocardiographic measurements [32, 33]. Furthermore, in non-selected HFrEF cohorts with apparently normal RV function, subtle functional abnormalities detected by depressed RVGLS carry negative consequences in terms of CV outcomes [34].
Three-dimensional (3D) echocardiography overcomes 2D geometric assumptions, integrating the longitudinal, radial, and antero-posterior components of RV contraction [35]. When validated against CMR, it might represent an important alternative for the assessment of RVEF [36] (Fig. 2). Nevertheless, RV volumes are usually underestimated using this technique compared to CMR [36, 37]. Indeed, especially in the presence of dilated RV and broad distance from the probe to RV wall, a wider band of hues inside the RV wall is seen, and manual tracking might exclude this blurred area resulting in underestimation of the real RV cavity [38].
Cardiac magnetic resonance and 3D echocardiography evaluation of right ventricle. a A dilated right ventricle in a patient affected by dilated cardiomyopathy and biventricular dysfunction. b A dilated cardiomyopathy without involvement of right ventricle. c A severely depressed right ventricular function analyzed with 3D echocardiography
CMR represents actually the gold standard for the assessment of RV function and morphology [28]. Indeed, the multiplanar imaging and 3-dimensional volume acquisition obtained by CMR overcomes the need for geometric assumptions regarding RV shape that limits the accuracy of standard echocardiography [39, 40]. Furthermore, balanced steady-state free-precession cine acquisitions ensure high-spatial and time resolution images, with accurate discrimination between blood and endocardium [39]. Compared to other techniques, CMR shows high accuracy and reproducibility in the estimate of RV volumes and RVEF with good interobserver and intraobserver variability [41,42,43]. Robust evidences exist on the prognostic value of RVEF determined by CMR in DCM [2, 5]. However, while most of the studies found that an RVEF value < 45% is associated with negative CV outcomes, less agreement is available on the RVEF cut-off to define RVD [44, 45]. The other major advantage of CMR is the capability of morphological assessment and tissue characterization beyond RV function. T2-weighted short-tau inversion recovery (T2w-STIR) imaging using an electrocardiogram-gated triple inversion recovery (IR) theoretically is able to depict tissue edema, and might represent a useful diagnostic tool when an overlapping active inflammatory process is suspected, such as in acute or chronic myocarditis or cardiac sarcoidosis [46]. The presence of late gadolinium enhancement at the right RV insertion site has been reported in a variable number of DCM patients studied with CMR, but its significance in terms of prognosis remains uncertain and probably neutral [47, 48]. However, the real prevalence of late gadolinium enhancement in the RV is complicated by the thin wall, which might limit the accuracy in the assessment of possible areas of scar [49]. Nevertheless, due to some major limitations of CMR such as its limited availability, the request of patient compliance, and the troubles of performing the exam in patients wearing a cardiac device, most centers still use echocardiography for the routine assessment of RV.
The importance of a longitudinal evaluation
The concept of longitudinal evaluation in DCM has gained progressively more importance in the last years [50]. Progresses in medical therapy not only dramatically reduced mortality in DCM [51], but also showed the capability of positively counteracting the adverse cardiac remodeling, potentially restoring a normal cardiac shape and function in a substantial number of patients [52]. This phenomenon has been extensively studied in the LV, demonstrating that approximately one-third of patients affected by DCM might undergo through a left ventricular reverse remodeling (LVRR) up to 24 months since the diagnosis, with positive consequences in terms of cardiac outcomes [53, 54].
This capability of cardiac remodeling has been less extensively studied in the RV. In the largest DCM population with available periodical reassessment of RV function with standard echocardiography, approximately 80% of patients with baseline RVD demonstrated a normalization of RV function in the following 6–12 months, with an important predictive value of a subsequent LVRR [3]. Importantly, in another study focused on DCM patients with available genetic data, the percentage of patients normalizing RV function during follow-up was high (≃70%), with similar findings among patients with genetic negative or TTN-determined DCM, while patients affected by other genetic etiologies had a lower probability to improve their RV function, highlighting a possible different pathogenetic mechanism of RVD in these patients [10]. Importantly, RVD might also develop in advanced stages of the disease in patients with baseline normal RV function, conferring negative prognostic value [3, 10].
Currently, echocardiography remains the method of choice for periodical revaluation of cardiac function in DCM, and a particular focus on RV function should be always encouraged during the follow-up of these patients.
Prognostic implications of right ventricular dysfunction and specific therapeutic challenges
Prognostic stratification remains a cornerstone in the management of DCM patients. Among the other parameters, RV involvement, both in terms of morphological and functional alterations, has been proven to be one of the strongest negative outcome modifiers, particularly when combined with concomitant pulmonary hypertension [55].
A reduced benefit from GMDT in terms of LV improvement has been described in DCM patients with persistent RVD [3], reflecting perhaps a more advanced disease. At the same time, the presence of RVD negatively affected the response to CRT [56, 57] and mitral valve repair [58,59,60] in HFrEF of mixed origin, including DCM patients.
Potentially, all reports considering RVD have been variably associated with adverse outcomes. In a previous experience including approximately one hundred DCM patients, a TAPSE ≤ 14 mm was significantly associated with a higher risk of all-cause death (ACD) or heart transplantation (HTx) [61]. Interestingly, even in patients with normal TAPSE, a depressed RV free wall strain is associated with higher risk of CV outcomes [33].
Analogously, a depressed value of RVFAC, both at the initial clinical presentation and at follow-up evaluation, was also associated with higher risk of HTx and ACD in a large series of patients affected by DCM [3].
A reduced RVEF determined by 3D echocardiography was associated with poor CV outcome in patients affected by various CV diseases [62]. Furthermore, recent data showed that an RVEF < 43% determined by 3D echocardiography could predict a worse cardiovascular outcome in DCM [7].
The most robust evidence of the prognostic role of RVD in DCM comes from studies which evaluated RVEF with CMR. In a study of 250 prospectively enrolled DCM patients, Gulati et al. demonstrated a strong and independent role of RVD in determining ACD, HTx, or heart failure hospitalizations (HFH) [2]. Similarly, the presence of RVEF < 45% was associated with a sevenfold increased risk of ventricular arrhythmias and a shorter time to all-cause mortality in more than two hundred DCM patients [6]. In another population of more than four hundred patients affected by DCM, a depressed RVEF was associated with a fivefold increased risk of ACD [5]. Finally, RVGLS analyzed by CMR was demonstrated to show an incremental prognostic role in reclassifying the risk of major cardiovascular events in recent series of DCM patients [63].
All these data taken together show the importance of a comprehensive RV assessment in the prognostic stratification of DCM patients.
Further research is needed to provide a direct comparison of the different RV imaging parameters in the prognostic stratification of patients with DCM and RVD.
Specific considerations in DCM with advanced heart failure
In patients with DCM and advanced HF, specific therapies, namely mechanical long-term support or HTx, must be considered [64]. In this setting, RV assessment is crucial, as it implies different approaches and profoundly changes the management of these patients.
In case of indications to left ventricular assist device (LVAD), acute RV failure post LVAD implantation occurs in 13–40% of patients, conferring important prognostic implications [65, 66].
Acute RV failure post LVAD implantation is defined by INTERMACS as need of an RVAD or requirement of inhaled nitric oxide or inotropic therapy for more than 1 week any time after LVAD implantation in the presence of symptoms and signs of persistent RVD, such as central venous pressure > 18 mmHg with a cardiac index < 2 L/min/m2 in the absence of elevated left atrial or pulmonary capillary wedge pressure (PCWP) (> 18 mmHg), cardiac tamponade, ventricular arrhythmias, or pneumothorax [67].
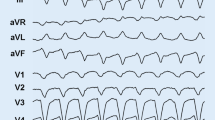
The mechanism of this phenomenon is not completely understood, but it is mostly related to the acute hemodynamic change post LVAD implantation (Fig. 3). Indeed, the increased RV preload due to the augmented venous return from the unloaded LV can further increase the physiologic burden on an RV that may already be dysfunctional pre-LVAD and can potentially exacerbate tricuspid regurgitation [68]. This mechanism is only partially balanced by the decreased RV afterload due to the reduction of LV filling pressures, while the possible structural changes in pulmonary vasculature require longer to develop [69]. At the same time, possible ineffective unloading of the LV under LVAD can also be detrimental for the RV and leads to RV failure [70]. An optimal hemodynamic balance is thus complicated in these patients, and fluid status must always be optimized and continuously monitored [12].
On the other hand, RV failure might develop even with a late onset (i.e., > 5 weeks since LVAD implantation) in patients supported by LVAD [71]. This condition has been reported in a various number of LVAD patients, ranging from 8 to 45% in previous observations [71,72,73,74], and leading to a poor prognosis [75]. The pathogenesis of late-onset RVF is multifactorial, and it is due to a complex interplay between intrinsic RV function and hemodynamic changes determined by LVAD support [72]. Indeed, while it is plausible that late RVF could occur in a greater percentage of patients with pre-existing underestimated RVD, suction from LVAD and leftward shift of the interventricular septum could induce changes in RV morphology resulting in RV impairment even in patients without pre-existing RVD [76, 77]. Furthermore, other important complications of LVAD such as aortic valve regurgitation and ventricular arrhythmias have been advocated in the progression of late RVD, with possible benefits of aortic valve replacement in patients with symptomatic aortic valve regurgitation [78, 79].
Based on the above considerations, it appears clear that one of the main determinants of RV failure post LVAD implantation is the pre-implant RV function. An adequate pre-implant RV evaluation, comprehensive of echocardiographic parameters such as RV free wall strain, RVFAC, and RV/LV size ratio, as well as some parameters evaluating left atrium and LV should be always performed to predict the possibility of RVF and to consider the possibility of biventricular instead of LV only support [68, 80, 81]. However, even though many specific multiparametric scores have been proposed in this setting, many other studies have found no predictors of RV failure, especially in cases of late onset [77]. Currently, the role of dobutamine stress echocardiography in selecting patients for LVAD is not well established, but it has been proven that a positive response to dobutamine myocardial stress in patients with LVAD and decreasing support might be useful to identify patients who could be weaned from LVAD [82].
Although the presence of RVD represents a marker of advanced disease prompting an HTx instead of LVAD, RV failure might be seen also in patient post HTx, representing one of the major outcome determinants [83]. In these patients, the presence of high PVR and pulmonary artery pressure pre-transplant lead to pressure overload of the donor RV and, therefore, to RV failure [84]. Other factors that may contribute to RVD post-surgery might be inadequate or prolonged hypothermic preservation, ischemic RV injury on cardiopulmonary bypass, and the change in contractile pattern of RV post cardiotomy [85].
In both post LVAD and post HTx, patients with RVF might need an inotropic treatment to support the hemodynamic status due to the failing RV, with dobutamine, milrinone, and levosimendan as the most used agents, possibly associated with vasodilators such phosphodiesterase type-5-inhibitors to ensure a reduction of PVR and RV afterload [86,87,88]. In some refractory cases, the implementation of RV-specific mechanical supports should be considered [89].
Future perspectives
Although our knowledge on RV pathophysiology and our capability of its assessment have grown up in the last decades, many fascinating targets could be addressed in the next future.
It is plausible that CMR will be progressively more available, and its constant implementation, along with speckle tracking techniques in the routine assessment of RV, will probably contribute to a give real estimation of the RVD in DCM, helping clinicians in the prognostic stratification and therapeutical management.
At the moment, no specific therapies are present for RVD and the most important therapeutical step is to ensure an optimal hemodynamic status concurrently with the constant implementation of drugs for LV systolic dysfunction.
Progresses in the genetics field led us to study some specific therapies for some genetic etiologies such as LMNA and PLN [90,91,92]. Hopefully these therapies might change the natural history of these entities, and can directly counteract the cardiomyopathic process in both ventricles, representing an important alternative where the usual GDMT fails to improve symptoms and functional performance.
Finally, the advent of percutaneous correction of tricuspid regurgitation might represent a possible therapeutic target for some DCM patients where RVD could be the result of chronic volume overload which cannot be properly addressed by medical treatment [93].
Conclusions
The importance of the RV function in patients affected by DCM is pivotal. Progresses in cardiac imaging showed that the prevalence is high in DCM in distinct phases of the disease, with many possible pathogenetic mechanisms. At the moment, specific treatments for RVD are still lacking and further research is advocated to implement pharmacotherapies with a precise target on RV.
Availability of data and material
Not applicable.
Change history
22 July 2022
The original version of this paper was updated to add funding note.
References
Pinto YM, Elliott PM, Arbustini E et al (2016) Proposal for a revised definition of dilated cardiomyopathy, hypokinetic non-dilated cardiomyopathy, and its implications for clinical practice: a position statement of the ESC working group on myocardial and pericardial diseases. Eur Heart J 37(23). https://doi.org/10.1093/eurheartj/ehv727
Gulati A, Ismail TF, Jabbour A et al (2013) The prevalence and prognostic significance of right ventricular systolic dysfunction in nonischemic dilated cardiomyopathy. Circulation 128(15). https://doi.org/10.1161/CIRCULATIONAHA.113.002518
Merlo M, Gobbo M, Stolfo D et al (2016) The prognostic impact of the evolution of RV function in idiopathic DCM. JACC Cardiovasc Imaging 9(9). https://doi.org/10.1016/j.jcmg.2016.01.027
Liu T, Gao Y, Wang H et al (2021) Association between right ventricular strain and outcomes in patients with dilated cardiomyopathy. Heart 107(15). https://doi.org/10.1136/heartjnl-2020-317949
Pueschner A, Chattranukulchai P, Heitner JF et al (2017) The prevalence, correlates, and impact on cardiac mortality of right ventricular dysfunction in nonischemic cardiomyopathy. JACC Cardiovasc Imaging 10(10). https://doi.org/10.1016/j.jcmg.2017.06.013
Becker MAJ, van der Lingen ALCJ, Wubben M et al (2021) Characteristics and prognostic value of right ventricular (dys)function in patients with non-ischaemic dilated cardiomyopathy assessed with cardiac magnetic resonance imaging. ESC Heart Failure 8(2). https://doi.org/10.1002/ehf2.13072
Vîjîiac A, Onciul S, Guzu C et al (2021) The prognostic value of right ventricular longitudinal strain and 3D ejection fraction in patients with dilated cardiomyopathy. Int J Card Imaging 37(11). https://doi.org/10.1007/s10554-021-02322-z
la Vecchia L, Zanolla L, Varotto L et al (2001) Reduced right ventricular ejection fraction as a marker for idiopathic dilated cardiomyopathy compared with ischemic left ventricular dysfunction. Am Heart J 142(1). https://doi.org/10.1067/mhj.2001.116071
Venner C, Selton-Suty C, Huttin O, Erpelding ML, Aliot E, Juillière Y (2016) Right ventricular dysfunction in patients with idiopathic dilated cardiomyopathy: prognostic value and predictive factors. Arch Cardiovasc Dis 109(4). https://doi.org/10.1016/j.acvd.2015.10.006
Manca P, Cannatà A, Nuzzi V et al (2021) Prevalence and evolution of right ventricular dysfunction among different genetic backgrounds in dilated cardiomyopathy. Can J Cardiol (Published online). https://doi.org/10.1016/j.cjca.2021.06.024
Gerges M, Gerges C, Pistritto AM et al (2015) Pulmonary hypertension in heart failure epidemiology, right ventricular function, and survival. Am J Respir Crit Care Med 192(10). https://doi.org/10.1164/rccm.201503-0529OC
Raina A, Meeran T (2018) Right ventricular dysfunction and its contribution to morbidity and mortality in left ventricular heart failure. Curr Heart Fail Rep 15(2). https://doi.org/10.1007/s11897-018-0378-8
Voelkel NF, Quaife RA, Leinwand LA et al (2006) Right ventricular function and failure: report of a National Heart, Lung, and Blood Institute working group on cellular and molecular mechanisms of right heart failure. Circulation 114(17). https://doi.org/10.1161/CIRCULATIONAHA.106.632208
Cipriani A, Bauce B, de Lazzari M et al (2020) Arrhythmogenic right ventricular cardiomyopathy: characterization of left ventricular phenotype and differential diagnosis with dilated cardiomyopathy. J Am Heart Assoc 9(5). https://doi.org/10.1161/JAHA.119.014628
Corrado D, Basso C, Judge DP (2017) Arrhythmogenic cardiomyopathy. Circ Res 121(7). https://doi.org/10.1161/CIRCRESAHA.117.309345
Klima UP, Guerrero JL, Vlahakes GJ (1999) Myocardial perfusion and right ventricular function. Ann Thorac Cardiovasc Surg (2)
Cavigli L, Focardi M, Cameli M, Mandoli GE, Mondillo S, D’Ascenzi F (2020) The right ventricle in “left-sided” cardiomyopathies: the dark side of the moon. Trends in Cardiovascular Medicine Published online. https://doi.org/10.1016/j.tcm.2020.10.003
Boxt LM (1999) Radiology of the right ventricle. Radiol Clin N Am 37(2). https://doi.org/10.1016/S0033-8389(05)70100-7
Haddad F, Hunt SA, Rosenthal DN, Murphy DJ (2008) Right ventricular function in cardiovascular disease, part I: anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation 117(11). https://doi.org/10.1161/CIRCULATIONAHA.107.653576
Schneider M, Aschauer S, Mascherbauer J et al (2019) Echocardiographic assessment of right ventricular function: current clinical practice. Int J Card Imaging 35(1). https://doi.org/10.1007/s10554-018-1428-8
Kaul S, Tei C, Hopkins JM, Shah PM (1984) Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J 107(3). https://doi.org/10.1016/0002-8703(84)90095-4
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the European association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging 16(3). https://doi.org/10.1093/ehjci/jev014
Rudski LG, Lai WW, Afilalo J et al (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography. Endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23(7). https://doi.org/10.1016/j.echo.2010.05.010
Unsworth B, Casula RP, Yadav H et al (2013) Contrasting effect of different cardiothoracic operations on echocardiographic right ventricular long axis velocities, and implications for interpretation of post-operative values. Int J Cardiol 165(1). https://doi.org/10.1016/j.ijcard.2011.08.031
Spruijt OA, di Pasqua MC, Bogaard HJ (2017) Serial assessment of right ventricular systolic function in patients with precapillary pulmonary hypertension using simple echocardiographic parameters: a comparison with cardiac magnetic resonance imaging. J Cardiol 69(1). https://doi.org/10.1016/j.jjcc.2016.02.019
Anavekar NS, Gerson D, Skali H, Kwong RY, Kent Yucel E, Solomon SD (2007) Two-dimensional assessment of right ventricular function: an echocardiographic-MRI correlative study. Echocardiography 24(5). https://doi.org/10.1111/j.1540-8175.2007.00424.x
Smolarek D, Gruchała M, Sobiczewski W (2017) Echocardiographic evaluation of right ventricular systolic function: the traditional and innovative approach. Cardiol J 24(5). https://doi.org/10.5603/CJ.a2017.0051
Champion HC, Michelakis ED, Hassoun PM (2009) Comprehensive invasive and noninvasive approach to the right ventricle-pulmonary circulation unit state of the art and clinical and research implications. Circulation 120(11). https://doi.org/10.1161/CIRCULATIONAHA.106.674028
Lopez-Candales A, Hernandez-Suarez DF (2016) Strain imaging echocardiography: what imaging cardiologists should know. Curr Cardiol Rev 13(2). https://doi.org/10.2174/1573403x12666161028122649
Sanz J, Conroy J, Narula J (2012) Imaging of the right ventricle. Cardiol Clin 30(2). https://doi.org/10.1016/j.ccl.2012.03.001
Nuzzi V, Castrichini M, Collini V et al (2021) Impaired right ventricular longitudinal strain without pulmonary hypertension in patients who have recovered from COVID-19. Circ Cardiovasc Imaging. https://doi.org/10.1161/CIRCIMAGING.120.012166
Focardi M, Cameli M, Carbone SF et al (2015) Traditional and innovative echocardiographic parameters for the analysis of right ventricular performance in comparison with cardiac magnetic resonance. Eur Heart J Cardiovasc Imaging 16(1). https://doi.org/10.1093/ehjci/jeu156
Seo J, Jung IH, Park JH et al (2019) The prognostic value of 2D strain in assessment of the right ventricle in patients with dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging 20(9). https://doi.org/10.1093/ehjci/jez015
Carluccio E, Biagioli P, Alunni G et al (2018) Prognostic value of right ventricular dysfunction in heart failure with reduced ejection fraction: superiority of longitudinal strain over tricuspid annular plane systolic excursion. Circ Cardiovasc Imaging 11(1). https://doi.org/10.1161/CIRCIMAGING.117.006894
Vijiiac A, Onciul S, Guzu C et al (2021) Forgotten no more - the role of right ventricular dysfunction in heart failure with reduced ejection fraction: an echocardiographic perspective. Diagnostics 11(3). https://doi.org/10.3390/diagnostics11030548
Leibundgut G, Rohner A, Grize L et al (2010) Dynamic assessment of right ventricular volumes and function by real-time three-dimensional echocardiography: a comparison study with magnetic resonance imaging in 100 adult patients. J Am Soc Echocardiog 23(2). https://doi.org/10.1016/j.echo.2009.11.016
Sugeng L, Mor-Avi V, Weinert L et al (2010) Multimodality comparison of quantitative volumetric analysis of the right ventricle. JACC: Cardiovasc Imaging 3(1). https://doi.org/10.1016/j.jcmg.2009.09.017
Shimada YJ, Shiota M, Siegel RJ, Shiota T (2010) Accuracy of right ventricular volumes and function determined by three-dimensional echocardiography in comparison with magnetic resonance imaging: a meta-analysis study. J Am Soc Echocardiog 23(9). https://doi.org/10.1016/j.echo.2010.06.029
Sechtem U, Pflugfelder PW, Gould RG, Cassidy MM, Higgins CB (1987) Measurement of right and left ventricular volumes in healthy individuals with cine MR imaging. Radiology 163(3). https://doi.org/10.1148/radiology.163.3.3575717
Rominger MB, Bachmann GF, Geuer M et al (1999) Accuracy of right- and left-ventricular heart volume and left-ventricular muscle mass determinations by cine MRI in breath-hold technique. Rofo Fortschritte auf dem Gebiet der Rontgenstrahlen und der bildgebenden Verfahren 170(1). https://doi.org/10.1055/s-2007-1011007
Csecs I, Czimbalmos C, Suhai FI et al (2018) Left and right ventricular parameters corrected with threshold-based quantification method in a normal cohort analyzed by three independent observers with various training-degree. Int J Cardiovasc Imaging 34(7). https://doi.org/10.1007/s10554-018-1322-4
Luijnenburg SE, Robbers-Visser D, Moelker A, Vliegen HW, Mulder BJM, Helbing WA (2010) Intra-observer and interobserver variability of biventricular function, volumes and mass in patients with congenital heart disease measured by CMR imaging. Int J Cardiovasc Imaging 26(1). https://doi.org/10.1007/s10554-009-9501-y
Grothues F, Moon JC, Bellenger NG, Smith GS, Klein HU, Pennell DJ (2004) Interstudy reproducibility of right ventricular volumes, function, and mass with cardiovascular magnetic resonance. Am Heart J 147(2). https://doi.org/10.1016/j.ahj.2003.10.005
Gopal AS, Chukwu EO, Iwuchukwu CJ et al (2007) Normal values of right ventricular size and function by real-time 3-dimensional echocardiography: comparison with cardiac magnetic resonance imaging. J Am Soc Echocardiog 20(5). https://doi.org/10.1016/j.echo.2006.10.027
Rominger MB, Bachmann GF, Pabst W, Rau WS (1999) Right ventricular volumes and ejection fraction with fast cine MR imaging in breath-hold technique: applicability, normal values from 52 volunteers, and evaluation of 325 adult cardiac patients. J Magn Reson Imaging 10(6). https://doi.org/10.1002/(SICI)1522-2586(199912)10:6<908::AID-JMRI2>3.0.CO;2-2
Francone M, Carbone I, Agati L et al (2011) Utility of T2-weighted short-tau inversion recovery (STIR) sequences in cardiac MRI: an overview of clinical applications in ischaemic and non-ischaemic heart disease. Radiol Med 116(1). https://doi.org/10.1007/s11547-010-0594-0
Grigoratos C, Pantano A, Meschisi M et al (2020) Clinical importance of late gadolinium enhancement at right ventricular insertion points in otherwise normal hearts. Int J Card Imaging 36(5). https://doi.org/10.1007/s10554-020-01783-y
Yi JE, Park J, Lee HJ et al (2018) Prognostic implications of late gadolinium enhancement at the right ventricular insertion point in patients with non-ischemic dilated cardiomyopathy: a multicenter retrospective cohort study. PLoS One 13(11). https://doi.org/10.1371/journal.pone.0208100
Grosse-Wortmann L, Macgowan CK, Vidarsson L, Yoo SJ (2008) Late gadolinium enhancement of the right ventricular myocardium: is it really different from the left ? J Cardiovasc Magn Reson 10(1). https://doi.org/10.1186/1532-429X-10-20
Manca P, Nuzzi V, Cannatà A, Merlo M, Sinagra G (2021) Contemporary etiology and prognosis of dilated non-ischemic cardiomyopathy. Minerva Cardiology and Angiology Published online. https://doi.org/10.23736/s2724-5683.21.05736-7
Merlo M, Cannatà A, Pio Loco C et al (2020) Contemporary survival trends and aetiological characterization in non-ischaemic dilated cardiomyopathy. Eur J Heart Fail 22(7). https://doi.org/10.1002/ejhf.1914
Merlo M, Cannatà A, Gobbo M, Stolfo D, Elliott PM, Sinagra G (2018) Evolving concepts in dilated cardiomyopathy. Eur J Heart Fail 20(2). https://doi.org/10.1002/ejhf.1103
Merlo M, Pyxaras SA, Pinamonti B, Barbati G, di Lenarda A, Sinagra G (2011) Prevalence and prognostic significance of left ventricular reverse remodeling in dilated cardiomyopathy receiving tailored medical treatment. J Am Coll Cardiol 57(13). https://doi.org/10.1016/j.jacc.2010.11.030
Cannata A, Manca P, Nuzzi V et al (2020) Sex-specific prognostic implications in dilated cardiomyopathy after left ventricular reverse remodeling. J Clin Med Res 9(8). https://doi.org/10.3390/jcm9082426
Rao SD, Adusumalli S, Mazurek JA (2020) Pulmonary hypertension in heart failure patients. Card Fail Rev 6. https://doi.org/10.15420/cfr.2019.09
Alpendurada F, Guha K, Sharma R et al (2011) Right ventricular dysfunction is a predictor of non-response and clinical outcome following cardiac resynchronization therapy. J Cardiovasc Magn Reson 13(1). https://doi.org/10.1186/1532-429X-13-68
Manca P, Cossa S, Matta G et al (2020) Right ventricular function assessed by cardiac magnetic resonance predicts the response to resynchronization therapy. J Cardiovasc Med 21(4). https://doi.org/10.2459/JCM.0000000000000931
Spieker M, Marpert J, Afzal S et al (2021) Right ventricular dysfunction assessed by cardiovascular magnetic resonance is associated with poor outcome in patients undergoing transcatheter mitral valve repair. PLoS One 16(1 January). https://doi.org/10.1371/journal.pone.0245637
Kaneko H, Neuss M, Weissenborn J, Butter C (2016) Prognostic significance of right ventricular dysfunction in patients with functional mitral regurgitation undergoing MitraClip. Am J Cardiol 118(11). https://doi.org/10.1016/j.amjcard.2016.08.054
di Mauro M, Calafiore AM, Penco M, Romano S, di Giammarco G, Gallina S (2007) Mitral valve repair for dilated cardiomyopathy: predictive role of right ventricular dysfunction. Eur Heart J 28(20). https://doi.org/10.1093/eurheartj/ehm375
Ghio S, Recusani F, Klersy C et al (2000) Prognostic usefulness of the tricuspid annular plane systolic excursion in patients with congestive heart failure secondary to idiopathic or ischemic dilated cardiomyopathy. Am J Card Imaging 85(7). https://doi.org/10.1016/S0002-9149(99)00877-2
Nagata Y, Wu VCC, Kado Y et al (2017) Prognostic value of right ventricular ejection fraction assessed by transthoracic 3D echocardiography. Circ Cardiovasc Imaging 10(2). https://doi.org/10.1161/CIRCIMAGING.116.005384
Cittar M, Cipriani A, Merlo M et al (2021) Prognostic significance of feature-tracking right ventricular global longitudinal strain in non-ischemic dilated cardiomyopathy. Frontiers in Cardiovascular Medicine 8. https://doi.org/10.3389/fcvm.2021.765274
Potapov EV, Antonides C, Crespo-Leiro MG et al (2019) 2019 EACTS Expert Consensus on long-term mechanical circulatory support. Eur J Cardiothorac Surg 56(2). https://doi.org/10.1093/ejcts/ezz098
Drakos SG, Janicki L, Horne BD et al (2010) Risk factors predictive of right ventricular failure after left ventricular assist device implantation. Am J Card Imaging 105(7). https://doi.org/10.1016/j.amjcard.2009.11.026
Patlolla B, Beygui R, Haddad F (2013) Right-ventricular failure following left ventricle assist device implantation. Curr Opin Cardiol 28(2). https://doi.org/10.1097/HCO.0b013e32835dd12c
Kirklin JK, Naftel DC, Stevenson LW et al (2008) INTERMACS database for durable devices for circulatory support: first annual report. J Heart Lung Transplant 27(10). https://doi.org/10.1016/j.healun.2008.07.021
Vivo RP, Cordero-Reyes AM, Qamar U et al (2013) Increased right-to-left ventricle diameter ratio is a strong predictor of right ventricular failure after left ventricular assist device. J Heart Lung Transpalant 32(8). https://doi.org/10.1016/j.healun.2013.05.016
Gulati G, Ruthazer R, Denofrio D, Vest AR, Kent D, Kiernan MS (2021) Understanding longitudinal changes in pulmonary vascular resistance after left ventricular assist device implantation. J Card Fail 27(5). https://doi.org/10.1016/j.cardfail.2021.01.004
Leung CC, Moondra V, Catherwood E, Andrus BW (2010) Prevalence and risk factors of pulmonary hypertension in patients with elevated pulmonary venous pressure and preserved ejection fraction. Am J Cardiol 106(2). https://doi.org/10.1016/j.amjcard.2010.02.039
Takeda K, Takayama H, Colombo PC et al (2015) Incidence and clinical significance of late right heart failure during continuous-flow left ventricular assist device support. J Heart Lung Transplant 34(8). https://doi.org/10.1016/j.healun.2015.03.011
Kapelios CJ, Charitos C, Kaldara E et al (2015) Late-onset right ventricular dysfunction after mechanical support by a continuous-flow left ventricular assist device. J Heart Lung Transplant 34(12). https://doi.org/10.1016/j.healun.2015.05.024
Ruiz-Cano MJ, Ramazyan L, Schramm R et al (2021) Clinical implications of late-onset right ventricular failure after implantation of a continuous-flow left ventricular assist device as bridge to transplantation. Eur J Cardiothorac Surg 60(1). https://doi.org/10.1093/ejcts/ezab114
Imamura T, Kinugawa K, Kato N et al (2014) Late-onset right ventricular failure in patients with preoperative small left ventricle after implantation of continuous flow left ventricular assist device. Circulation J 78(3). https://doi.org/10.1253/circj.CJ-13-1201
Kurihara C, Critsinelis AC, Kawabori M et al (2018) Frequency and consequences of right-sided heart failure after continuous-flow left ventricular assist device implantation. Am J Cardiol 121(3). https://doi.org/10.1016/j.amjcard.2017.10.022
Sack KL, Dabiri Y, Franz T, Solomon SD, Burkhoff D, Guccione JM (2018) Investigating the role of interventricular interdependence in development of right heart dysfunction during LVAD support: a patient-specific methods-based approach. Front Physiol 9(May). https://doi.org/10.3389/fphys.2018.00520
Rich JD, Gosev I, Patel CB et al (2017) The incidence, risk factors, and outcomes associated with late right-sided heart failure in patients supported with an axial-flow left ventricular assist device. J Heart Lung Transplant 36(1). https://doi.org/10.1016/j.healun.2016.08.010
Gopinathannair R, Cornwell WK, Dukes JW et al (2019) Device therapy and arrhythmia management in left ventricular assist device recipients: a scientific statement from the American Heart Association. Circulation 139(20). https://doi.org/10.1161/CIR.0000000000000673
Cowger J, Rao V, Massey T et al (2015) Comprehensive review and suggested strategies for the detection and management of aortic insufficiency in patients with a continuous-flow left ventricular assist device. J Heart Lung Transplant 34(2). https://doi.org/10.1016/j.healun.2014.09.045
Neyer J, Arsanjani R, Moriguchi J, Siegel R, Kobashigawa J (2016) Echocardiographic parameters associated with right ventricular failure after left ventricular assist device: a review. J Heart Lung Transplant 35(3). https://doi.org/10.1016/j.healun.2015.12.018
Kato TS, Farr M, Schulze PC et al (2012) Usefulness of two-dimensional echocardiographic parameters of the left side of the heart to predict right ventricular failure after left ventricular assist device implantation. Am J Cardiol 109(2). https://doi.org/10.1016/j.amjcard.2011.08.040
Khan T, Delgado RM, Radovancevic B et al (2003) Dobutamine stress echocardiography predicts myocardial improvement in patients supported by left ventricular assist devices (LVADs): Hemodynamic and histologic evidence of improvement before LVAD explantation. J Heart Lung Transplant 22(2). https://doi.org/10.1016/S1053-2498(02)00485-0
Stobierska-Dzierzek B, Awad H, Michler RE (2001) The evolving management of acute right-sided heart failure in cardiac transplant recipients. J Am Coll Cardiol 38(4). https://doi.org/10.1016/S0735-1097(01)01486-3
Kirklin JK, Naftel DC, Kirklin JW, Blackstone EH, White-Williams C, Bourge RC (1988) Pulmonary vascular resistance and the risk of heart transplantation. J Heart Transplant 7(5)
Carrier M, Blaise G, Bélisle S et al (1999) Nitric oxide inhalation in the treatment of primary graft failure following heart transplantation. J Heart Lung Transplant 18(7). https://doi.org/10.1016/S1053-2498(99)00025-X
Haddad F, Doyle R, Murphy DJ, Hunt SA (2008) Right ventricular function in cardiovascular disease, part II: pathophysiology, clinical importance, and management of right ventricular failure. Circulation 117(13). https://doi.org/10.1161/CIRCULATIONAHA.107.653584
Raina A, Vaidya A, Gertz ZM, Susan Chambers, Forfia PR (2013) Marked changes in right ventricular contractile pattern after cardiothoracic surgery: implications for post-surgical assessment of right ventricular function. J Heart Lung Transplant 32(8). https://doi.org/10.1016/j.healun.2013.05.004
Hansen MS, Andersen A, Nielsen-Kudsk JE (2018) Levosimendan in pulmonary hypertension and right heart failure. Pulm Circ 8(3). https://doi.org/10.1177/2045894018790905
Saito S, Sakaguchi T, Miyagawa S et al (2011) Biventricular support using implantable continuous-flow ventricular assist devices. J Heart Lung Transplant 30(4). https://doi.org/10.1016/j.healun.2010.11.013
Repetti GG, Toepfer CN, Seidman JG, Seidman CE (2019) Novel therapies for prevention and early treatment of cardiomyopathies: now and in the future. Circ Res 124(11). https://doi.org/10.1161/CIRCRESAHA.119.313569
Grote Beverborg N, Später D, Knöll R et al (2021) Phospholamban antisense oligonucleotides improve cardiac function in murine cardiomyopathy. Nat Commun 12(1). https://doi.org/10.1038/s41467-021-25439-0
Chai RJ, Werner H, Li PY et al (2021) Disrupting the LINC complex by AAV mediated gene transduction prevents progression of Lamin induced cardiomyopathy. Nat Commun 12(1). https://doi.org/10.1038/s41467-021-24849-4
Besler C, Seeburger J, Thiele H, Lurz P (2018) Treatment options for severe functional tricuspid regurgitation: indications, techniques and current challenges. e-Journal of Cardiology Practice 16(31)
Acknowledgements
The authors acknowledge Cassa di Risparmio di Trieste (CRT) Foundation for the continuous support in research.
Funding
Open access funding provided by Università degli Studi di Trieste within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Not applicable.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Manca, P., Nuzzi, V., Cannatà, A. et al. The right ventricular involvement in dilated cardiomyopathy: prevalence and prognostic implications of the often-neglected child. Heart Fail Rev 27, 1795–1805 (2022). https://doi.org/10.1007/s10741-022-10229-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-022-10229-7