Abstract
Understanding the drivers of student dropout from higher education has been a policy concern for several decades. However, the contributing role of certain factors—including student mental health—remains poorly understood. Furthermore, existing studies linking student mental health and university dropout are limited in both methodology and scope—for example, they often rely on small and/or non-representative samples or subjective measures, and focus almost exclusively on main effects. This paper overcomes many of these shortcomings by leveraging unique linked administrative data on the full population of domestic students commencing undergraduate studies at Australian universities between 2012 and 2015 (n = 652,139). Using these data, we document that approximately 15% of students drop out of university within their first academic year. Critically, students receiving treatment for mental health problems are 4.3 (adjusted) to 8.3 (unadjusted) percentage points more likely to drop out of higher education. This association remains in the presence of an encompassing set of potential confounds, and is remarkably uniform across segments of the student population determined by individual, family, and programme characteristics. Altogether, our findings call for increased policy efforts to improve student mental health and to buffer against its deleterious effects on retention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Student dropout from higher education (HE) has been a policy concern for several decades. This issue has become more salient as HE systems expanded substantially and more students from diverse backgrounds entered university (Marginson, 2016), including in Australia—the country of focus for this study (Productivity Commission, 2019). Mirroring policy interest, academic research on student dropout from HE has a long tradition. Despite numerous studies considering individual student attributes and institutional characteristics contributing to early departure (see, e.g. Pascarella & Terenzini, 2005), some factors remain underexplored. In this study, we focus on one such factor, namely student mental health. Failure to consider student mental health in studies of HE dropout is a major omission, given evidence of a high and increasing prevalence of mental health problems among youth. Globally, about 20% of adolescents suffer from mental health problems (World Health Organization, 2020). Furthermore, HE students have been identified as a high-risk population due to the stress associated with their educational transitions and HE studies (Barden et al., 2019). In Australia, one-third of respondents to the 2016 National Tertiary Student Wellbeing Survey reported experiencing mental health problems (Rickwood et al., 2017).
Previous research has documented adverse impacts of mental health problems on students’ capability and motivation to learn (see, e.g. Bowman et al., 2020; Markoulakis & Kirsh, 2013). Studies have also linked mental health problems with lower school grades (McLeod et al., 2012), an increased likelihood of school dropout (Leach & Butterworth, 2012), and a decreased likelihood of commencing (McLeod & Kaiser, 2004) and completing (Kessler et al., 1995) university studies. However, studies linking mental health to student dropout from HE, specifically, are comparatively less common. Furthermore, the existing body of work is affected by methodological and scope limitations. For example, many such studies are based on small and/or non-representative samples or self-reported measures. Furthermore, most available studies examine only the “main effects”, thereby assuming that the influence of mental health status on dropout from HE is uniform across different student groups. Considering interactive effects between mental health status and other characteristics is important, as it can help identify segments of the student population that may require targeted support. Third, a vast majority of the available evidence comes from the USA. This limits the generalisability of the reported findings to countries with different education and health systems.
This paper seeks to overcome the shortcomings of previous studies and to offer a comprehensive and robust account of the associations between student mental health and dropout from HE in Australia. To accomplish this, we leverage a unique administrative dataset obtained through a partnership with the Australian Government Department of Education, Skill and Employment. These data encompass the full population of domestic students commencing undergraduate studies at Australian universities between 2012 and 2015 (n = 652,139) and allow us to examine whether students treated for mental health problems are more prone than others to first-year dropout. Furthermore, the richness of the data at hand allows us to examine whether the estimated effects of mental health problems on HE dropout vary across segments of the student population.Footnote 1
Literature review
Individual and organisational predictors of HE dropout
Research on dropout from HE can be divided into four strands. The first strand focuses on ascertaining the contributing role of students’ background characteristics, including their gender (Severiens & Dam, 2012), social class (Aina, 2013), and other markers of a disadvantaged background (Li & Carroll, 2020). A second strand of research is devoted to investigating the role of intra-individual traits, attitudes, and dispositions, such as learning strategies (Van Bragt et al., 2011), student experience (Shcheglova et al., 2020), or programme expectations (Zając & Komendant-Brodowska, 2019). A third strand focuses on institutional-level predictors, including universities’ “selectivity” (Shamsuddin, 2016) and expenditure, tuition, and staffing patterns (Gansemer-Topf et al., 2018). Finally, some studies have evaluated concrete policy changes, including the provision of financial aid to students (Santelices et al., 2016).
Overall, this body of scholarly work demonstrates that the precursors of HE dropout lie at both the individual and institutional levels. However, as noted before, a potentially important factor shaping students’ experiences and outcomes—mental health—has received surprisingly little attention. In the next section, we discuss theoretical reasons why we should expect a relationship between student mental health and HE dropout.
Mental health and student dropout from HE: theorising the links
To conceptualise the role of mental health in influencing HE retention, we draw on two seminal frameworks theorising student success in HE: Astin’s theory of student involvement (1984), commonly known as the “I-E-O model”, and Tinto’s theory of HE student departure. Astin’s, (1984) I-E-O theory posits that higher education success can be understood as the combined function of three sets of elements, such that students’ inputs (I) (e.g. their socio-demographic and background characteristics, and pre-university experiences) and environments (E) (e.g. their university experiences) exert an influence over their cognitive, emotional, and behavioural outcomes (O) (e.g. their post-graduation knowledge, attitudes, and beliefs). Astin further argues that student involvement is a key “mediating mechanism” (1984: 520) that connects students’ inputs to their outputs. Within this context, Astin defines student involvement as “the amount of physical and psychological energy that the student devotes to the academic experience” such that “a highly involved student is one who, for example, devotes considerable energy to studying, spends much time on campus, participates actively in student organisations, and interacts frequently with faculty members and other students” (Astin, 1984: 518).
Similarly, Tinto’s, (1993) theory of HE student departure stresses the importance of students’ interactions with academic and social systems within a HE institution for student outcomes, focusing on retention. Rewarding interactions with these systems result in students’ greater academic and social integration, thereby increasing their persistence and retention.
Here, we argue that—consistent with Astin’s theory—students’ pre-existing mental health can be thought of as an important student input, alongside other student traits (e.g. their gender, age, or “first-in-family” status). Specifically, poor mental health has the capacity to inhibit students’ ability to devote energy and efforts towards their academic experience, thereby decreasing the likelihood of student retention. Indeed, existing studies linking mental health to student outcomes suggest several mechanisms through which mental health problems can hamper student outcomes and increase the risk of dropout. Consistent with Tinto’s framework, these mechanisms operate through either (a) academic integration or (b) social integration.
On the one hand, academic integration can be affected by impairments in cognitive functioning associated with mental health problems. For example, mental health problems can lead to acute deficits in attention, information processing, decision-making, memory, and motivation (American Psychiatric Association (APA), 2013), which may in turn affect students’ capacity to learn and persist in their studies. Consistent with this, a recent review of the literature found that students who experienced depression and anxiety were more likely to have difficulties with processing speed, perceptual reasoning, and verbal comprehension, resulting in learning problems and suboptimal academic outcomes (Bowman et al., 2020). Although this review focused on high school students, these factors are also likely to affect the performance of university students.
On the other hand, mental health problems can also lead to students experiencing difficulties in social situations, with possible implications for their social integration within HE settings. For instance, mental health problems—including depressive symptoms and anxiety disorders—can result in low self-esteem, diminished motivation, anhedonia, and/or withdrawal from social situations (Markoulakis & Kirsh, 2013). An inability to perform in social situations may complicate students’ interactions with their peers, lecturers, tutors, and university administrators. Indeed, a literature review by Markoulakis & Kirsh (2013) indicated that university students with mental health problems faced both internal difficulties (e.g. physical, psychological, social) and external difficulties (e.g. structural issues, stigma) affecting their academic performance.
Altogether, combining Astin’s, (1984) I-E-O theory, Tinto’s, (1993) theory of student departure, and mental health scholarship leads us to expect mental health problems to negatively affect students’ HE retention.
Mental health and student dropout from HE: existing empirical evidence
Empirical evidence on the associations between mental health and overall student outcomes is largely consistent with these theoretical postulations. Most existing studies come from the USA and document adverse long-term effects of mental health problems on the attainment of educational milestones. For instance, using the US National Comorbidity Survey, Kessler et al., (1995) estimated that the odds of university dropout among individuals with pre-existing psychiatric disorders were 1.4 times (anxiety disorders) to 2.9 times greater (mood disorders) than for individuals without such disorders. These results have been replicated using more recent US samples (Breslau et al., 2008; Mojtabai et al., 2015).
Studies focusing exclusively on HE have reached similar conclusions, documenting adverse effects of mental health problems on student outcomes such as grade point average (GPA) and completion. These are mostly small-scale studies using samples drawn from a single institution (e.g. Eisenberg et al., 2009). However, some leverage relatively large survey datasets comprising ~ 5000 to ~ 16,000 responses, such as the 2001–2002 US National Epidemiologic Survey on Alcohol and Related Conditions (Hunt et al., 2010) or the US Beginning Postsecondary Students Longitudinal Study (Carroll et al., 2020).
The detrimental impact of mental health problems on educational attainment has also been observed in countries other than the USA. For example, Hjorth et al., (2016) used Danish data and Lee et al. (2009) compared results from 16 countries taking part in the World Mental Health Survey Initiative. In both studies, respondents with prior mental disorders were more likely to terminate their participation in HE prematurely. Finally, while most existing studies have found evidence of detrimental effects of mental health problems on HE dropout, others have not (e.g. Cvetkovski et al., 2018).
To our knowledge, however, administrative datasets capturing complete populations—which are both larger and more representative than these surveys—have not been used in this literature. In the next section, we explain how the present study makes use of these powerful data to expand on the existing literature, both in methodology and scope.
The present study: aims and contributions
Existing studies examining the links between student mental health and HE attrition are affected by several methodological and scope limitations. The current study seeks to address some of these shortcomings by leveraging unique administrative data covering the full population of domestic students commencing undergraduate studies at Australian universities between 2012 and 2015. These data feature both a large number of cases and objective measures for the focal constructs.
A key limitation of the majority of existing studies is that they rely on small samples, sometimes drawn from a single HE institution, limiting the generalisability of the conclusions drawn by these studies. Furthermore, this situation also creates a risk of analyses being under-powered. Small sample sizes can result in inflated standard errors and an enhanced risk of Type-II estimation errors (i.e. failing to observe a relationship in the sample that exists in the population). Using administrative data covering the entire population improves the external validity of the results and minimises estimation errors.
Our study also expands on the findings of larger, survey-based previous studies. First, most such studies rely on self-reported measures of mental health and educational outcomes, including HE dropout. Furthermore, some surveys used in previous studies rely on retrospective self-reports, which are prone to measurement error (e.g. due to recall issues) and social desirability biases (Martin, 2010). Objective measures, such as medical records capturing mental health treatment as leveraged in this study, are less likely to be affected by such issues.
Second, the scope of these previous studies has been limited. Specifically, this literature has limited itself to unveiling “main effects”, that is, identifying the overall effect of mental health status on HE dropout. This approach ignores that such an effect may not be uniform, but rather fluctuate across population groups. One barrier to examining effect heterogeneity in this literature has been a reliance on datasets that were too small to consider nuanced intersections, or datasets including only coarse information on relevant student and institutional characteristics. This applies also to many of the social surveys used in the larger, earlier studies in the field. Thanks to the volume and richness of our data, we are able to provide first-time evidence on whether and how the estimated impact of mental health problems on student dropout differs by student socioeconomic background and academic programme characteristics. As discussed below, any evidence of moderation by these factors can help tailor policies aimed at ameliorating negative impacts of mental health problems on student outcomes.
In addition, empirical evidence for countries other than the USA is scarce. As a result, it remains unclear whether findings for the USA may generalise to other country contexts, including Australia. In addition, the Australian HE context makes it an interesting case study. Australia has witnessed a considerable expansion of the HE sector in recent decades, coinciding with increased student dropout rates—particularly among students from disadvantaged backgrounds (Productivity Commission, 2019). At the same time, university students’ mental health has been largely absent from government policy (Orygen, 2017). As such, our results add a new case study to an emerging body of research aimed at establishing whether previous US findings operate in countries with different institutional environments.
In the next section, we describe the data and methods used in our empirical analyses.
Data and methods
Dataset and sample selection
We utilise a customised Multi-Agency Data Integration Project (MADIP) dataset that includes linked de-identified unit-level records from the Higher Education Information Management System (HEIMS), Medicare Benefits Schedule (MBS), Pharmaceutical Benefits Schedule (PBS), and Personal Income Tax (PIT) records. The Australian Bureau of Statistics (ABS) was responsible for linking the information across these datasets, achieving a high linkage rate. Mental health data are available for 97% of the in-scope population. For details about the standard MADIP dataset, including the linking methodology, see ABS, (2018).
The analytical dataset contained HE records on enrolments and background characteristics of all domestic undergraduate students commencing studies in Australian universities between 2012 and 2015. MBS and PBS comprise rich and accurate information on mental health-related services and medication provided to all Australian citizens and permanent residents through Medicare—a federally funded universal health system. In turn, the PIT data provide information on labour market activity. Overall, out of 657,777 observations drawn from HEIMS, less than 1% were excluded from the sample due to missing data on analytic variables, most often those derived from address records (0.6%). The final analytic dataset comprises 652,139 individuals—which amounts to 42 to 130 times the size of the samples used in earlier studies in the field (Carroll et al., 2020; Hunt et al., 2010).
Measures
Student dropout
Student dropout can occur at various levels (Tinto, 1993). Here, we focus on the most serious type of dropout—leaving the HE system entirely (as opposed to transferring to another programme or institution). We measure it by considering students’ enrolment status in the academic year following their commencement year. Students who had no record of enrolment at any HE institution in Australia at that point in time were deemed to have dropped out of HE. Nearly 15% of the sample—that is, 97,655 students—left HE after the first year.
Mental health treatment
The second key variable for our analyses is mental health treatment in the year preceding the commencement of an undergraduate degree. Since our interest is on the effects of mental health on HE outcomes, we deliberately choose to capture mental health treatment prior to commencing university. This allows for a clear temporal ordering of events and reduces the risk of bias due to reverse causation.
We follow previous research (see, e.g. Barr et al., 2020; Butterworth et al., 2021; Saxby et al., 2020) and use the MBS and PBS records on the use of mental health services and medication to derive our proxy measure for mental health status. The MBS records allow us to identify individuals who accessed mental health services provided by general practitioners, psychiatrists, clinical psychologists, other psychologists, and other allied health specialists as a part of the national medical system. The PBS records contain information on the following drug groups: antipsychotics, anxiolytics, hypnotics, sedatives, antidepressants, psychostimulants, attention deficit hyperactivity disorder agents, and nootropics. Our indicator of mental health treatment is a binary variable identifying individuals who accessed at least one mental health service (from the MBS) or who were prescribed at least one mental health-related medication (from the PBS). Using this measure, nearly 86,000 individuals, or approximately 13.1% of the sample, were observed to receive mental health treatment in the year before commencing their university studies.
Admittedly, this measure misses a small portion of mental health treatments, as MBS data do not include mental health support obtained outside of the system and PBS data do not include private prescriptions, over the counter medicines, and medicines supplied to public hospital inpatients. However, these “blind spots” are not large. The gaps in MBS data are mitigated by the universal nature of the Australian Medicare system (Department of Health, 2016) and prescriptions not included in PBS constitute only a small portion of all medicines prescribed in Australia (Australian Institute of Health and Welfare (AIHW), 2021).
While it is safe to assume that most people receiving mental health treatment require it because of their mental health problems, not everyone suffering from a mental health problem seeks treatment (Butterworth et al., 2021). Therefore, a limitation of our approach—shared with other studies using administrative data—is that it may undercount students experiencing mental health problems. Hence, our analyses may yield lower-bound estimates of the true effects of mental health problems on student dropout.
Control variables
Our models control for an encompassing set of student and programme characteristics known to affect HE outcomes in Australia (see, e.g. Tomaszewski et al., 2018). These include the following:
-
Background characteristics, such as gender, delayed entry (commencement at age 20 or higher), Indigenous status (yes/no), non-English-speaking background status (yes/no), being a first-generation student (i.e. none of the parents completed HE, yes/no), self-reported physical disability (yes/no), and coming from a regional area (yes/no)
-
Programme characteristics, including field of study, attendance mode (internal, external, or multi-modal), attendance type (full-time or part-time), and Tertiary Entrance Score (TES) (quartiles plus a “no score” category)Footnote 2
-
Labour-market engagement (not working; working; no information)
-
Commencement year (n = 4)
-
State-of-residence (n = 8) and institution (n = 41—statistics not shown for confidentiality reasons) fixed effects to account for any time-invariant state- or institution-specific factors potentially correlated with student mental health and student retention
In our cohort, 58.5% of students are female, 68.1% are first-generation, 2.2% identify as Indigenous, 6.1% have a physical disability, 7.9% come from a non-English-speaking background (NESB), 23.5% come from a regional area, and 41.1% experienced a delayed entry into HE. Nearly three-quarters (73.3%) work while they study. Internal mode of study (79.7%) and full-time attendance (85.0%) are typical, whereas Society and Culture (23.4% of students) and Health (18.4%) are the most popular fields of study. Table A1 in the Appendix presents summary statistics of all variables included in the analyses.
Analytic approach
Our analyses involve a series of logistic regression models. For ease of interpretation, all model results are expressed as odds ratios (ORs) and average marginal effects (AMEs) calculated holding the covariates at their observed values. Our key aim is to analyse the associations between being treated for mental health problems and dropout from HE. Prior to doing so, we consider how mental health treatment is distributed across students and HE programmes. To accomplish this, we fit a model (Model 1) that takes the following form:
where T is a binary variable capturing mental health treatment; α is the model’s intercept; C is a set of control variables; U is a vector of institution fixed effects; S is a vector of location fixed effects; the βs are vectors of coefficients to be estimated; and e is the regression error.
We then move to examine the associations between mental health treatment as an explanatory variable and student dropout as an outcome. To do so, we first fit a base (i.e. unadjusted) model (Model 2) of the following form:
Here, the new term D is a binary variable capturing student dropout. In the next model (Model 3), we add student and programme characteristics. This adjusted model allows us to retrieve the effect of mental health on dropout net of possible confounds. This model takes the following form:
In the final model (Model 4), we test whether the relationship between being treated for mental health problems and student dropout differs across levels of the control variables. To accomplish this, we introduce interaction terms (T × C) between these variables, which results in the following model:
To assess the significance of differences in the effect of mental health across values of the explanatory variables in a way that is appropriate for logistic regression, we use the techniques described by Mize, (2019). Specifically, we evaluate the interaction effects in the predicted probability metric by using a Wald test to determine whether AMEs for being treated for mental health problems vary depending on the value of the independent variable with which it is interacted.
Empirical evidence
In this section, we present the results of our empirical analyses. We begin by examining the student- and programme-level predictors of mental health treatment. We then estimate the main effects of being treated for mental health problems on student dropout. We conclude the section by discussing potential interaction effects between mental health status and a range of student- and programme-level factors.
Predictors of mental health status among higher education students
The results (Model 1, Table 1) indicate that all of the considered student and programme characteristics are statistically significantly associated with mental health status. Receiving treatment for mental health problems was more common among Indigenous (OR = 1.15, p < 0.001; AME = 0.015) and part-time (OR = 1.37, p < 0.001; AME = 0.034) students, those with a physical disability (OR = 5.27, p < 0.001; AME = 0.261), and those who delayed entry into HE (OR = 1.90, p < 0.001; AME = 0.067). In contrast, it is less common among males (OR = 0.57, p < 0.001; AME = − 0.056), first-generation (OR = 0.93, p < 0.001; AME = − 0.007) and NESB students (OR = 0.44, p < 0.001; AME = − 0.067), students from regional areas (OR = 0.92, p < 0.001; AME = − 0.008), and students not working while studying (OR = 1.20, p < 0.001; AME = − 0.019). We also observed differences in the shares of students who received treatment for mental health problems across different fields and modes of study.
Based on the AMEs, the most at-risk groups were female students (5.6 percentage points [pp] more likely than male students to receive treatment for mental health problems), students with a delayed entry into university (6.7 pp more likely than students entering at normative ages), and students from English-speaking backgrounds (6.7 pp more likely than those from NESB). Yet the biggest difference of all was between students with and without a physical disability, with the latter being 26.1 pp more likely than the former to receive treatment for mental health problems. These results suggest that these groups, particularly students with a physical disability, may be differentially exposed to the potentially deleterious effects of mental health problems on student outcomes. It is to these that we now turn.
Mental health status and student dropout
Bivariate statistics suggest that students treated for mental health problems are at higher risk of dropping out of HE than their peers. Among students receiving mental health treatment, 22.2% left their studies in the first year, compared to just 13.9% of students not receiving mental health treatment (p < 0.05 in a t-test). Logistic regression analyses confirmed that students treated for mental health problems are indeed more likely to drop out. In the base model (Model 2, Table 1), the odds of student dropout are 1.77 time higher among students treated for mental health problems than their peers (OR = 1.77, p < 0.001; AME = 0.083). In the next model (Model 3, Table 1), which controls for an encompassing set of variables, the odds ratio for mental health treatment is smaller in magnitude but remains statistically significant (OR = 1.41, p < 0.001; AME = 0.043). The magnitude of the association is easier to grasp when the model results are transformed into predicted probabilities. Based on the second model, the predicted dropout rate for students receiving mental health treatment equals 18.6% which is 4.3 pp higher than that for students not receiving mental health treatment (of 14.3%). This suggests that approximately half (4.0 pp) of the bivariate association between mental health problems and student HE dropout was actually due to confounding. The higher dropout rate among students receiving mental health treatment translates into approximately 3700 additional students from our cohort, or 925 annually, dropping out of the HE system.
The results from Model 3 also indicate that all student characteristics except regional residence are associated with dropout from HE. The factors associated with increased odds of dropping out of HE included being Indigenous (OR = 1.49, p < 0.001; AME = 0.051), male (OR = 1.21, p < 0.001; AME = 0.022), a first-generation student (OR = 1.23, p < 0.001; AME = 0.023), delayed entry into HE (OR = 1.03, p < 0.01; AME = 0.003), and studying in external mode (OR = 1.16, p < 0.001; AME = 0.019) or part-time (OR = 2.47, p < 0.001; AME = 0.125). Meanwhile, the factors decreasing the odds of dropping out of HE included having a physical disability (OR = 0.78, p < 0.001; AME = − 0.026) and not engaging in paid work (OR = 0.84, p < 0.001; AME = − 0.020).Footnote 3 There were also statistically significant differences by field-of-study and TES.
Although comparisons across explanatory variables must be undertaken with a degree of caution, the estimated effect of receiving mental health treatment on the odds of dropout from HE (AME = 0.043) appears to be larger in magnitude than the analogous estimated effects for other variables which have received more attention in the literature—e.g. being male (AME = 0.022), being a first-generation student (AME = 0.023), coming from a regional area (AME = 0.002), and delayed entry into HE entry (AME = 0.003). This rough comparison underscores the importance of gaining a better understanding of the role of mental health on student retention.
We conducted multiple sensitivity analyses to establish the robustness of our main results to different specifications and analytic choices, including (i) alternative measures of mental health treatment (separating accessing a mental health service and being prescribed mental health medication), (ii) measuring mental health problems during the first year of studies (instead of the year before), (iii) alternative measures of student dropout (leaving the institution and leaving the education field), (iv) different specifications of the disability indicators, and (v) incorporation of “stop out” into the measurement of student dropout. Due to space constraints, their rationale and results for these analyses are discussed in more detail in the Appendix. Importantly though, across all sensitivity analyses, the results pertaining to our focal explanatory variable—being treated for mental health problems—were consistent with those of the main analyses presented here, which speaks of the robustness of our approach.
Associations between mental health status and student dropout: do they vary by student and programme characteristics?
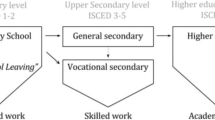
To ascertain whether and how student and/or programme characteristics moderate the relationship between receiving mental health treatment and dropout from HE, we turn to the results from the logistic regression model including interaction terms (Model 4). As explained in the methods section, we focus our discussion on differences in the AMEs on the mental health treatment across groups of students. Figure 1 presents the AMEs for the variables that involved statistically significant interactions (see Table A4 in the Appendix).
Average marginal effects of being treated for mental health problems on student dropout, by selected student characteristics. Notes: Data from customised MADIP dataset (2011–2016). AMEs based on the model results presented in Table A4 in the Appendix. N&Ph, Natural and Physical Sciences. Engi, Engineering and Related Technologies. Agr, Agriculture, Environmental and Related Studies. Edu, Education. M&C, Management and Commerce. S&C, Society and Culture. Arts, Creative Arts
There is some evidence of statistical moderation for gender, having a physical disability, coming from a regional area, being a first-generation student, attendance type and mode, and labour market activity. Specifically, being treated for mental health problems increased the estimated risk of dropout by a higher margin among students who come from regional areas (Diff = 0.84 pp, p < 0.01), are male (Diff = 0.66 pp, p < 0.05), study part-time (Diff = 1.50 pp, p < 0.001), and engage in paid work (Diff = 1.25 pp, p < 0.001). Meanwhile, being treated for mental health problems increased the estimated risk of dropout by a lower margin among students who had a physical disability (Diff = − 0.85 pp, p < 0.05), were a first-generation student (Diff = − 0.69 pp, p < 0.05), and studied in multi-modal mode (Diff = − 1.54 pp, p < 0.001) or external mode (Diff = − 1.69 pp, p < 0.01) rather than internal mode. Again, there were also some differences by field of study.
Although these interaction effects were statistically significant, none of them appeared to be substantive in their magnitude. In fact, differences in the estimated being treated for mental health problems on HE dropout across students with different characteristics and in different programmes were rarely greater than 2 percentage points. Therefore, we conclude that the effects of being treated for mental health problems are fairly uniform across groups of students.
Discussion and conclusion
In this paper, we have leveraged unique and powerful linked administrative data on an entire population of undergraduate students in Australia to offer comprehensive and robust evidence of the associations between students’ mental health status and dropout from HE. Following Astin’s, (1984) I-E-O theory and Tinto’s, (1993) model of student departure from HE, we expected to observe higher dropout rates among students treated for mental health problems. Consistent with this expectation, our main analysis demonstrated that being treated for mental health problems in the year preceding university commencement is associated with higher risk of HE dropout. The unadjusted difference in dropout rates was 8.3 pp (13.9% vs 22.2%). In regression models adjusted for an encompassing set of factors, the predicted dropout rate among students treated for mental health problems remained 4.3 pp higher than among other students. To further illustrate the magnitude and practical significance of this difference, we estimate that mental health issues result in roughly 3700 additional students from our cohort, or 925 annually, dropping out of the HE system.
These results were replicated across a range of sensitivity analyses and align with earlier studies highlighting the link between mental health and educational outcomes (e.g. Mojtabai et al., 2015), including dropout from HE (e.g. Hunt et al., 2010). Therefore, our study adds new evidence to a body of research documenting deleterious effects of mental health problems on students’ HE outcomes. Importantly, we reached the same conclusions as earlier studies (i) using administrative data with a different structure and properties and (ii) analysing a new context, Australia. The latter demonstrates that this association extends to countries other than the USA, where most previous research was conducted.
The unprecedented scale of our data allowed us to extend the analytic scope beyond the estimation of simple “main effects” of mental health status on student dropout. To this end, we assessed differences in the magnitude of the estimated impacts of being treated for mental health problems on HE dropout across students with different characteristics and in different programmes. To our knowledge, no previous empirical studies have explored this type of effect heterogeneity. In these analyses, we documented some evidence of statistical moderation. However, none of the estimated effects had a substantial magnitude, with group differences in such effects being always smaller than 2 pp. Therefore, our results can be read as indicating that the effects of mental health status are largely uniform across groups. More important, however, were differences in the share of HE students receiving mental health treatment by student- and programme-level characteristics. Specifically, our results corroborate previous findings that students who are female or of an English-speaking background, delayed-entry, or had a physical disability were overrepresented among students receiving mental health treatment. As a result, HE students with these characteristics are disproportionately affected by the negative impacts of mental health problems.
Study limitations and implications for future research
Despite the importance of our findings, some study limitations must be acknowledged. These limitations point to opportunities for methodological refinement and further inquiry. First, as previously discussed, the mental health measures based on MBS and PBS data have “blind spots” (Australian Institute of Health and Welfare (AIHW), 2021), such as private prescriptions obtained outside the national health system. Mental health-related medication may also be part of ongoing therapy for some groups of people with neurological conditions but no mental health problems. While it is unclear whether and how these measure limitations might impact our findings, the advantageous properties of the administrative data justify their use. Second, the MBS and PBS do not provide a nuanced picture of whether individuals’ mental health issues are chronic or temporary, nor do they indicate the severity of the condition (e.g. through information on dosage). Future studies could benefit from a more nuanced operationalisation of mental health status. Third, the data do not capture instances where individuals do not seek professional support, or cannot access services or medications due to financial, cultural, or other barriers. As stated before, this may result in an undercount of students affected by mental health problems and underestimation of the effects of mental health problems on student dropout.
Furthermore, our study is—necessarily—targeted in its scope, focusing on just one student outcome. Gaining a holistic understanding of the impact of mental health on HE outcomes requires additional research examining its impact on other outcomes across the student life course, including access to HE, more complex student trajectories like “stop-out”, other markers of HE achievement, and post-graduation labour market performance (Bennett et al., 2015).
Implications for policy and practice
Investments in college education are expensive—for the student and the educational system. At the same time, university education has the potential to change an individual’s life course by enhancing capabilities, employment prospects, and salary level, as well as fostering social mobility. Therefore, barriers or risks to university success are important to understand—for the individual, educational systems, and society as a whole. Our results show that mental health conditions impart an identifiable risk to onward retention success in the first year of HE. These findings add to a body of literature demonstrating that the transition from secondary schooling to HE—including the first year of university—constitutes a vulnerable phase of late adolescence and emerging adulthood (Evans et al., 2018). They also resonate with scholarship encouraging identification, prevention, and intervention of mental health conditions early in their development and onset (Arango et al., 2018).
While our analyses are not designed to identify specific policy solutions to the challenges posed by student mental health problems, our findings raise some considerations that may guide future policy development. A key policy implication is the need to better integrate programmes targeting mental health and programmes targeting educational outcomes—including those aimed at preventing HE dropout. In Australia, there is increasing recognition that addressing the mental health of secondary and tertiary students is a policy priority (e.g. Australian Government, 2021). Both the secondary school and HE sectors feature programmes aimed at preventing students developing mental health issues, or at improving student mental health more generally (Headspace, 2021; Orygen, 2017). Such programmes operate across educational sectors and jurisdictions, and many of them are run in collaboration by schools and universities. However, they are typically implemented independently of other programmes designed to target educational outcomes (such as maintaining school engagement, assisting student decision-making regarding HE, and preventing student dropout).
Our findings suggest the need for a comprehensive policy framework that enables successful intervention through early identification and remediation of mental health problems among young people completing secondary education. Some first steps may include campaigns aimed at raising awareness among secondary school students, parents, and educators, and increasing the availability of school-based, on-demand mental health screening services for students facing the school to university transition. A more radical direction would be to normalise students taking time off until they feel “ready, mental health wise” to successfully transition to higher education—e.g. by noting this option in school counselling and career pathway sessions. Intervening remedially among individuals who already accessed higher education should be another policy pillar. Such remedial policies should lay a solid framework for providing students experiencing mental health issues with enhanced HE supports (e.g. free mental health counselling or dedicated tutoring sessions) and/or offering them viable alternatives to dropping out (e.g. accessing extended periods of mental health leave or giving mental health problems greater consideration as extenuating circumstances for academic participation and performance). Future studies aimed specifically at assessing the relative merits of these different policy options are sorely needed, and any future interventions should be rigorously trialled before implementation.
Our analyses further demonstrated that, while the association between mental health status and student dropout from HE is relatively homogenous across segments of the student population, the share of students impacted by mental health problems is not. Indeed, female students, delayed-entry students, and, most importantly, students with a physical disability are disproportionately more likely to be treated for mental health problems. These groups are among those identified within the equity initiatives of the Australian Government. As such, they are the focus of existing equity and diversity programmes within the secondary school and HE sectors targeting student access and success (Bennett et al, 2015). It follows that, to be successful, mental health programmes in the Australian HE sector must keep the needs of these groups at the forefront.
To conclude, this study has generated unique evidence on the distribution and impacts of mental health problems among HE students. Our results serve to elevate claims that further research and policy attention are required to fully understand the role of mental health as a factor structuring educational equity and success, and how we can intervene to address this significant issue (e.g. Australian Institute of Health and Welfare (AIHW), 2014; Brett, 2016).
Data availability
The results of these studies are based, in part, on tax data supplied by the ATO to the ABS under the Taxation Administration Act 1953, which requires that such data is only used for the purpose of administering the Census and Statistics Act 1905. Any discussion of data limitations or weaknesses is in the context of using the data for statistical purposes, and is not related to the ability of the data to support the ATO's core operational requirements. Legislative requirements to ensure privacy and secrecy of these data have been followed. For access to MADIP data under Section 16A of the ABS Act 1975 or enabled by section 15 of the Census and Statistics (Information Release and Access) Determination 2018, source data are de-identified and so data about specific individuals has not been viewed in conducting this analysis. In accordance with the Census and Statistics Act 1905, results have been treated where necessary to ensure that they are not likely to enable identification of a particular person or organisation. The data cannot be shared.
Notes
A cautionary note on terminology is due here. The operationalisation of “mental-health status” varies across studies. For example, a mental-health problem may refer to the presence of a diagnosed mental disorder, high levels of self-reported psychological distress, or self-identified depressive symptoms. When reviewing the scholarly evidence, we take an encompassing approach and consider studies focusing on these and other operationalisations of mental health. In doing so, we recognise that these studies may be based on mental health measures that differ in nature, duration, and severity.
TES is based on tertiary entrance ranks, such as the Australian Tertiary Admission Rank (ATAR), with higher numbers indicating greater levels of achievement. Many students enter HE through alternative pathways and hence do not have a TES. Since these students tend to be mature age and/or come from disadvantage social backgrounds, we expect students with no TES to exhibit comparatively higher dropout rates.
While the finding that students with a physical disability are less likely to drop out is counterintuitive, this pattern was also apparent in both bivariate associations and regression models excluding mental health treatment from the covariates. This suggests that the negative coefficient on disability is not driven by collinearity between disability and mental health, or any other variable in the model. It might instead reflect the fact that students with a disability are less likely to access HE (Tomaszewski et al., 2018) and, as a result, those who enter HE may be particularly committed and persistent in their studies.
References
ABS. (2018). 1700.0—Microdata: Multi-Agency Data Integration Project, Australia. https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/1700.0Main+Features1Australia. Retrieved 20 December 2021.
Aina, C. (2013). Parental background and university dropout in Italy. Higher Education, 65(4).
American Psychiatric Association (APA). (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association.
Arango, C., Díaz-Caneja, C. M., McGorry, P. D., Rapoport, J., Sommer, I. E., Vorstman, J. A., McDaid, D., Marín, O., Serrano-Drozdowskyj, E., Freedman, R., & Carpenter, W. (2018). Preventive strategies for mental health. The Lancet Psychiatry, 5(7), 591–604. https://doi.org/10.1016/S2215-0366(18)30057-9
Astin, A. W. (1984). Student involvement: A developmental theory for higher education. Journal of College Student Personnel, 25(4), 297–308.
Australian Government. (2021). Australia's Youth Policy Framework. https://apo.org.au/sites/default/files/resource-files/2021-08/apo-nid314287.pdf
Australian Institute of Health and Welfare (AIHW). (2014). Towards a performance measurement framework for equity in higher education. AIHW.
Australian Institute of Health and Welfare (AIHW). (2021). Mental health services in Australia. AIHW. https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia/report-contents/mental-health-related-prescriptions/data-source-and-key-concepts. Retrieved 20 December 2021.
Barden, N., & Caleb, R. (Eds.). (2019). Student mental health and wellbeing in higher education: A practical guide. Sage.
Barr, M., Welberry, H., Finch, J., & Blunden, L. A. (2020). Using multiple administrative health datasets to identify a mental illness cohort. International Journal of Population Data Science, 5(5). https://doi.org/10.23889/ijpds.v5i5.1563
Bennett, A., Naylor, R., Mellor, K., Brett, M., Gore, J., Harvey, A., Munn, B., James, R., Smith, M., & Whitty, G. (2015). The critical interventions framework part 2: Equity initiatives in Australian higher education: A review of evidence of impact.
Bowman, S., McKinstry, C., Howie, L., & McGorry, P. (2020). Expanding the search for emerging mental ill health to safeguard student potential and vocational success in high school: A narrative review. Early Intervention in Psychiatry, 14(6), 655–676.
Breslau, J., Lane, M., Sampson, N., & Kessler, R. C. (2008). Mental disorders and subsequent educational attainment in a US national sample. Journal of Psychiatric Research, 42(9), 708–716.
Brett, M. (2016). Disability and Australian higher education: Policy drivers for increasing participation. In A. Harvey, C. Burnheim, & M. Brett (Eds.), Student Equity in Australian Higher Education: Twenty-five years of A Fair Chance for All (pp. 87–108). Springer Singapore.
Butterworth, P., de New, S. C., Schilling, C., Saxby, K., Petrie, D., & Wong, C. (2021). Dynamics of mental health and healthcare use among children and young adults. Australian Economic Review, 54(1), 130–142.
Carroll, J. M., Pattison, E., Muller, C., & Sutton, A. (2020). Barriers to bachelor’s degree completion among college students with a disability. Sociological Perspectives, 63(5), 809–832.
Cvetkovski, S., Jorm, A. F., & Mackinnon, A. J. (2018). Student psychological distress and degree dropout or completion: A discrete-time, competing risks survival analysis. Higher Education Research & Development, 37(3), 484–498.
Department of Health. (2016). What is the MBS and Medicare? http://www.msac.gov.au/internet/msac/publishing.nsf/Content/factsheet-03#:~:text=MSAC%20is%20independent%20of%20the%20Government%20and%2C%20while,is%20a%20key%20component%20of%20the%20Medicare%20system. Retrieved 20 December 2021.
Eisenberg, D., Golberstein, E., & Hunt, J. B. (2009). Mental health and academic success in college. The B.E. Journal of Economic Analysis & Policy, 9(1). https://doi.org/10.2202/1935-1682.2191
Evans, D., Borriello, G. A., & Field, A. P. (2018). A review of the academic and psychological impact of the transition to secondary education. Frontiers in Psychology, 9, 1482. https://doi.org/10.3389/fpsyg.2018.01482
Gansemer-Topf, A. M., Downey, J., Thompson, K., & Genschel, U. (2018). Did the recession impact student success? Relationships of finances, staffing and institutional type on retention. Research in Higher Education, 59(2), 174–197.
Headspace. (2021). Helping young people get through challenging times. Headspace year in review 2020 - 2021. Headspace National Youth Mental Health Foundation. https://headspace.org.au/assets/Reports/headspace-Year-in-Review-2020-2021.pdf
Hjorth, C. F., Bilgrav, L., Frandsen, L. S., Overgaard, C., Torp-Pedersen, C., Nielsen, B., & Bøggild, H. (2016). Mental health and school dropout across educational levels and genders: A 4.8-year follow-up study. BMC Public Health, 16(1), 1–12.
Hunt, J., Eisenberg, D., & Kilbourne, A. M. (2010). Consequences of receipt of a psychiatric diagnosis for completion of college. Psychiatric Services, 61(4), 6.
Kessler, R. C., Foster, C. L., Saunders, W. B., & Stang, P. E. (1995). Social consequences of psychiatric disorders, I: Educational attainment. American Journal of Psychiatry, 152(7), 1026–1032.
Leach, L. S., & Butterworth, P. (2012). The effect of early onset common mental disorders on educational attainment in Australia. Psychiatry Research, 199(1), 51–57.
Lee, S., Tsang, A., Breslau, J., Aguilar-Gaxiola, S., Angermeyer, M., Borges, G., Bromet, E., Bruffaerts, R., De Girolamo, G., & Fayyad, J. (2009). Mental disorders and termination of education in high-income and low-and middle-income countries: Epidemiological study. The British Journal of Psychiatry, 194(5), 411–417.
Li, I. W., & Carroll, D. R. (2020). Factors influencing dropout and academic performance: An Australian higher education equity perspective. Journal of Higher Education Policy and Management, 42(1), 14–30.
Marginson, S. (2016). High participation systems of higher education. The Journal of Higher Education, 87(2), 243–271.
Markoulakis, R., & Kirsh, B. (2013). Difficulties for university students with mental health problems: A critical interpretive synthesis. The Review of Higher Education, 37(1), 77–100.
Martin, J. (2010). Stigma and student mental health in higher education. Higher Education Research & Development, 29(3), 259–274.
McLeod, J. D., & Kaiser, K. (2004). Childhood emotional and behavioral problems and educational attainment. American Sociological Review, 69(5), 636–658.
McLeod, J. D., Uemura, R., & Rohrman, S. (2012). Adolescent mental health, behavior problems, and academic achievement. Journal of Health and Social Behavior, 53(4), 482–497.
Mize, T. (2019). Best practices for estimating, interpreting, and presenting nonlinear interaction effects. Sociological Science, 6, 81–117. https://doi.org/10.15195/v6.a4
Mojtabai, R., Stuart, E. A., Hwang, I., Eaton, W. W., Sampson, N., & Kessler, R. C. (2015). Long-term effects of mental disorders on educational attainment in the National Comorbidity Survey ten-year follow-up. Social Psychiatry and Psychiatric Epidemiology, 50(10), 1577–1591.
Orygen. (2017). Under the radar. The mental health of Australian university students. Orygen, The National Centre of Excellence in Youth Mental Health. https://www.orygen.org.au/Orygen-Institute/Policy-Reports/Under-the-radar/Orygen-Under_the_radar_report?ext=
Pascarella, E. T., & Terenzini, P. T. (2005). How college affects students: A third decade of research (vol. 2). Jossey-Bass.
Productivity Commission. (2019). The demand driven university system: A mixed report card. The Productivity Commission. https://www.pc.gov.au/research/completed/university-report-card/university-report-card.pdf
Rickwood, D., Telford, N., O’Sullivan, S., Crisp, D., & Magyar, R. (2017). National tertiary student wellbeing survey 2016. National Youth Mental Health Foundation. https://headspace.org.au/assets/Uploads/headspace-NUS-Publication-Digital.pdf
Santelices, M. V., Catalán, X., Kruger, D., & Horn, C. (2016). Determinants of persistence and the role of financial aid: Lessons from Chile. Higher Education, 71(3), 323–342.
Saxby, K., de New, S. C., & Petrie, D. (2020). Structural stigma and sexual orientation disparities in healthcare use: Evidence from Australian Census-linked-administrative data. Social Science & Medicine, 255. https://doi.org/10.1016/j.socscimed.2020.113027
Severiens, S., & ten Dam, G. (2012). Leaving college: A gender comparison in male and female-dominated programs. Research in Higher Education, 53(4), 453–470.
Shamsuddin, S. (2016). Berkeley or bust? Estimating the causal effect of college selectivity on bachelor’s degree completion. Research in Higher Education, 57(7), 795–822.
Shcheglova, I., Gorbunova, E., & Chirikov, I. (2020). The role of the first-year experience in student attrition. Quality in Higher Education, 26(3), 307–322.
Tinto, V. (1993). Leaving college: Rethinking the causes and cures of student attrition. The University of Chicago Press.
Tomaszewski, W., Kubler, M., Perales, F., Western, M., Rampino, T., & Xiang, N. (2018). Review of identified equity groups. The University of Queensland. https://espace.library.uq.edu.au/view/UQ:bd8a044
Van Bragt, C. A. C., Bakx, A. W. E. A., Bergen, T. C. M., & Croon, M. A. (2011). Looking for students’ personal characteristics predicting study outcome. Higher Education, 61(1), 59–75.
World Health Organization. (2020). Adolescent mental health. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health. Retrieved 20 December 2021.
Zając, T. Z., & Komendant-Brodowska, A. (2019). Premeditated, dismissed and disenchanted: Higher education dropouts in Poland. Tertiary Education and Management, 25(1), 1–16.
Acknowledgements
We are grateful to NCSEHE for its financial support. The research builds on a previous study funded through a collaborative partnership between the Australian Research Council Centre of Excellence for Children and Families over the Life Course (project number CE140100027) and the Australian Government Department of Education and Training. We would like to acknowledge guidance on the data properties from staff at the Australian Government Department of Education and Training (especially Luke Hendrickson and Marc Wigzell) and the Australian Bureau of Statistics. The study uses data from a customised Multi-Agency Data Integration Project dataset provided by the Australian Bureau of Statistics through the Australian Government Department of Education and Training.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This study was supported by the National Centre for Student Equity in Higher Education (NCSEHE) through its 2020 Research Grants Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval for the research was granted by The University of Queensland’s Office of Research Ethics (project number 2020002372).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zając, T., Perales, F., Tomaszewski, W. et al. Student mental health and dropout from higher education: an analysis of Australian administrative data. High Educ 87, 325–343 (2024). https://doi.org/10.1007/s10734-023-01009-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10734-023-01009-9