Abstract
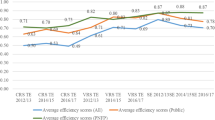
Efficiency analysis is crucial in healthcare to optimise resource allocation and enhance patient outcomes. However, the prompt adaptation of inputs can be hindered by adjustment costs, which impact Long-Run Technical Efficiency (LRTE). To bridge this gap in healthcare literature, this research employs a Bayesian Dynamic Stochastic Frontier Model to estimate parameters and explore healthcare efficiency dynamics over time. The study reveals the LRTE for New Zealand District Health Boards (DHBs) as 0.76, indicating around 32% more input utilisation due to adjustment costs. Most DHBs exhibit consistent short-run operational efficiency, with the national Short-Run Technical Efficiency (SRTE) very close to the LRTE. Among the tertiary providers, Auckland and Capital & Coast DHBs operate below the LRTE level, setting them apart from other tertiary providers. Similarly, Tairawhiti and West Coast DHBs also fall below the LRTE level, as indicated by their SRTE scores, potentially influenced by their unique healthcare settings and resource challenges. This research brings a new perspective to policy discussions by incorporating the temporal dynamics of decision-making and considering adjustment costs. It underscores the need to balance short-term and long-term technical efficiency, underlining their collective significance in fostering a sustainable and efficient healthcare system in New Zealand.
Similar content being viewed by others
Data availability
The data used in this manuscript is confidential and will not be deposited.
Notes
The Treasury [1] uses the Consumer Price Index to inflate the 1996 nominal dollar value to the 2016 real dollar value.
It is acknowledged that other factors may contribute to high adjustment costs; however, in this paper, policy and infrastructural issues have been used to motivate the estimation of efficiency under a dynamic system.
One FTE refers to 40 h of labour per week and is calculated based on accrual. However, working more than 40 h is only counted as one FTE. For more information on the calculation of FTEs, please refer to the Nationwide Service Framework [45].
A substantial correlation (close to 0.97) is observed between the FTEs of various labour groups.
It is recognised that employees may only sometimes be paid at their marginal product rate when a unionised workforce is prevalent. Nonetheless, given the limited availability of detailed compensation data, it is reasonable to make this assumption in the context of this research.
The price of any labour group can be used as a weighting factor.
The price index for various goods and services can be accessed at Statistics New Zealand [53].
For more information, refer to The Australian Institute of Health and Welfare [54].
The purchase unit is a classification system used to measure and quantify a healthcare service. For more information refer to Ministry of Health [56].
The relative inefficiency factor of a parameter is computed by using the formula \(1+2{\sum }_{\varphi =1}^{\infty }g\left(\varphi \right),\) where \(g\left(\varphi \right)\) is the sample autocorrelation of the draws on the parameter at lag \(\varphi\).
The LRTE corresponds to the expected value of LRTE calculated as \({\left[1+exp\left\{{\omega }_{j}/(1-{\rho }_{j})\right\}\right]}^{-1}\), where \(j\) indicates the \(j\) th draw from the posterior density.
DHBs with the same average efficiency scores and CVs are assigned the same ranking. On the other hand, a DHB with a low CV but the same average efficiency compared to its counterpart is given a high ranking. A low CV indicates low variability in efficiency signifying consistent performance.
References
The Treasury. Health Projections and Policy Options for the 2013 Long-term Fiscal Statement.2012. Available from: https://treasury.govt.nz/publications/ltfp/affording-our-future-statement-new-zealands-long-term-fiscal-position-html#section-5
The Treasury. Vote Health - Health Sector - Estimates 2017/2018 2017 [Available from: https://treasury.govt.nz/publications/vote-health-health-sector-estimates-2017-2018-html
The Treasury. District health board financial performance to 2016 and 2017 Plans 2017 [Available from: https://treasury.govt.nz/sites/default/files/2017-05/dhb-performance-feb17.pdf
Controller and Auditor-General. District health boards’ response to asset management requirements since 2009 2016 [Available from: https://www.oag.govt.nz/2016/dhbs-assets/docs/dhbs-assets.pdf
Controller and Auditor-General. Health sector: Results of the 2016/17 audits 2018 [Available from: https://oag.parliament.nz/2018/health-sector-audits/docs/health-sector-audits.pdf
Bentley TG, Effros RM, Palar K, Keeler EB (2008) Waste in the U.S. Health care system: a conceptual framework. Milbank Q 86(4):629–59
Rosko MD (2001) Cost efficiency of US hospitals: a stochastic frontier approach. Health Econ 10(6):539–551
Zuckerman S, Hadley J, Iezzoni L (1994) Measuring hospital efficiency with frontier cost functions. J Health Econ 13(3):255–280
Eisner R, Strotz RH, Post GR (1963).Determinants of business investment. In Commission on Money and Credit, Impacts of Monetary Policy. Prentice-Hall, New Jersey, pp 59–337.
Hamermesh DS, Pfann GA (1996) Adjustment Costs in factor demand. J Econ Lit 34(3):1264–1292
Penrose E (1995) The theory of the growth of the Firm, 3rd edn. Oxford University Press, Oxford, p 296
Treadway AB (1971) The rational multivariate flexible accelerator. Econometrica 39(5):845–855
Jiang N, Andrews A (2020) Efficiency of New Zealand’s District Health Boards at providing hospital services: A stochastic frontier analysis. J Prod Anal 53(1):53–68
Tsionas EG (2006) Inference in dynamic stochastic frontier models. J Appl Economet 21(5):669–676
Ministry of Health. District health boards 2020 [Available from: http://www.health.govt.nz/new-zealand-health-system/key-health-sector-organisations-and-people/district-health-boards
Ministry of Health. Population-based Funding Formula Review 2015 [Available from: https://www.health.govt.nz/system/files/documents/publications/population-based-funding-formula-review-2015-technical-report-mar2016.pdf
Afonso A, St. Aubyn M (2011) Assessing health efficiency across countries with a two-step and bootstrap analysis. Appl Econ Lett 18(15):1427–30
Aletras V, Kontodimopoulos N, Zagouldoudis A, Niakas D (2007) The short-term effect on technical and scale efficiency of establishing regional health systems and general management in Greek NHS hospitals. Health Policy 83(2):236–245
Mitropoulos P, Talias ΜA, Mitropoulos I (2015) Combining stochastic DEA with Bayesian analysis to obtain statistical properties of the efficiency scores: An application to Greek public hospitals. Eur J Oper Res 243(1):302–311
Andrews A, Emvalomatis G (2024) Efficiency measurement in healthcare: the foundations, variables, and models – a narrative literature review. Economics 18(1):20220062. https://doi.org/10.1515/econ-2022-0062
Rosko MD, Mutter RL (2008) Stochastic frontier analysis of hospital inefficiency. Med Care Res Rev 65(2):131–166
Hamidi S (2016) Measuring efficiency of governmental hospitals in Palestine using stochastic frontier analysis. Cost Eff Resour Allocation 14(1):3
Colombi R, Martini G, Vittadini G (2017) Determinants of transient and persistent hospital efficiency: The case of Italy. Health Econ 26(S2):5–22
Aghlmand S, Feizollahzadeh S, Fathi B, Yusefzadeh H, Alinejhad M (2022) The stochastic frontier analysis technique in measuring the technical and economic efficiency of hospital diagnostic laboratories: a case study in Iran. Cost Eff Resour Allocation 20(1):65
Van den Broeck J, Koop G, Osiewalski J, Steel MFJ (1994) Stochastic frontier models: A Bayesian perspective. J Econ 61(2):273–303
Koop G, Steel M, Osiewalski J (1995) Posterior analysis of stochastic frontier models using Gibbs sampling. Comput Statistics 10(10):353–373
Koop G, Osiewalski J, Steel MFJ (1997) Bayesian efficiency analysis through individual effects: Hospital cost frontiers. J Econ 76(1):77–105
Ahn SC, Sickles RC (2000) Estimation of long-run inefficiency levels: a dynamic frontier approach. Economet Rev 19(4):461–492
Desli E, Ray SC, Kumbhakar SC (2003) A dynamic stochastic frontier production model with time-varying efficiency. Appl Econ Lett 10(10):623–626
Khalaf L, Saunders CJ, editors (2016) Dynamic technical efficiency. Productivity and Efficiency Analysis; Springer
Emvalomatis G (2012) Adjustment and unobserved heterogeneity in dynamic stochastic frontier models. J Prod Anal 37(1):7–16
Emvalomatis G, Stefanou SE, Oude LA (2011) Estimation of stochastic frontier models with fixed effects through Monte Carlo Maximum likelihood. J Probab Stat 2011:568457
Galán JE, Veiga H, Wiper MP (2015) Dynamic effects in inefficiency: Evidence from the Colombian banking sector. Eur J Oper Res 240(2):562–571
Skevas I, Emvalomatis G, Brümmer B (2018) Heterogeneity of long-run technical efficiency of German dairy farms: A Bayesian approach*. J Agric Econ 69(1):58–75
Jacobs R, Smith PC, Street A (2006) Measuring efficiency in health care: analytic techniques and health policy. Cambridge University Press, Cambridge, United Kingdom
Kumbhakar SC, Wang H-J (2005) Estimation of growth convergence using a stochastic production frontier approach. Econ Lett 88(3):300–305
Knopf E. History of Efficiency Measurement by the New Zealand Health SectorPost 2000 2017 [22]. Available from: https://www.productivity.govt.nz/assets/Documents/31af48f5ed/History-of-efficiency-measurement-by-the-health-sector-Knopf-v2.pdf
Kumbhakar SC, Wang H-J, Horncastle AP (2015) A practitioner’s guide to stochastic frontier analysis using Stata: Cambridge University Press
Farrell MJ (1957) The measurement of productive efficiency. J Royal Stat Soc Ser A (General) 120(3):253–290
Christensen LR, Jorgenson D, Lau LJ (1973) Transcendental logarithmic production frontiers. Rev Econ Stat 55(1):28–45
Intriligator MD, Bodkin RG, Hsiao C (1978) Econometric models, techniques, and applications. Prentice-Hall, New Jersey, NJ
Coelli TJ, Rao DSP, O’Donnell CJ, Battese GE (2005) An introduction to efficiency and productivity analysis. New York, NY: Springer Science & Business Media. 163–4
Hollingsworth B, Peacock S (2008) Efficiency measurement in health and health care. Routledge, New York, NY
Worthington AC (2004) Frontier efficiency measurement in health care: A review of empirical techniques and selected applications. Med Care Res Rev 61(2):135–170
Nationwide Service Framework Library. Measuring Staff Resources - Counting ‘FTEs’ 2016 [Available from: https://nsfl.health.govt.nz/accountability/financial-standards-and-guidelines/measuring-staff-resources-counting-ftes
Aletras V, Kontodimopoulos N, Zagouldoudis A, Niakas D (2007) The short-term effect on technical and scale efficiency of establishing regional health systems and general management in Greek NHS hospitals. Health Policy 83(2–3):236–245
Herr A (2008) Cost and technical efficiency of German hospitals: does ownership matter? Health Econ 17(9):1057–1071
Asmild M, Hollingsworth B, Birch S (2013) The scale of hospital production in different settings: one size does not fit all. J Prod Anal 40(2):197–206
Chattopadhyay S, Ray SC (1996) Technical, scale, and size efficiency in nursing home care: A nonparametric analysis of Connecticut homes. Health Econ 5(4):363–373
Grosskopf S, Valdmanis V (1993) Evaluating hospital performance with case-mix-adjusted outputs. Med Care 31(6):525–532
Hu H-H, Qi Q, Yang C-H (2012) Analysis of hospital technical efficiency in China: Effect of health insurance reform. China Econ Rev 23(4):865–877
Valdmanis V (1992) Sensitivity analysis for DEA models: An empirical example using public vs. NFP hospitals. J Public Econ 48(2):185–205
Statistics New Zealand. Infoshare 2019 [Available from: http://archive.stats.govt.nz/infoshare/
The Australian Institute of Health and Welfare. Australian refined diagnosis-related groups (AR-DRG) data cubes 2019 [Available from: https://www.aihw.gov.au/reports/hospitals/ar-drg-data-cubes/contents/data-cubes
Ministry of Health. Weighted Inlier Equivalent Separations 2019 [Available from: https://www.health.govt.nz/nz-health-statistics/data-references/weighted-inlier-equivalent-separations
Ministry of Health. About purchase units 2018 [Available from: https://nsfl.health.govt.nz/purchase-units/about-purchase-units
Ministry of Health. 2017/18 DHB Hospital Caseload Monitoring Report 2018 [updated March, 2018. Available from: https://www.health.govt.nz/system/files/documents/pages/cmr_report_1718_summary_may.pdf
Friesner D, Mittelhammer R, Rosenman R (2013) Inferring the incidence of industry inefficiency from DEA estimates. Eur J Oper Res 224(2):414–424
Mutter RL, Rosko MD, Wong HS (2008) Measuring hospital inefficiency: The effects of controlling for quality and patient burden of illness. Health Serv Res 43(6):1992–2013
Tanner MA, Wong WH (1987) The calculation of posterior distributions by data augmentation. J Am Stat Assoc 82(398):528–540
Allsopp L. Investigating Health Technology Diffusion in New Zealand - How Does it Spread and Who Stands to Gain? 2006 [Available from: https://treasury.govt.nz/publications/wp/investigating-health-technology-diffusion-new-zealand-how-does-it-spread-and-who-stands-gain-wp-06
Ministry of Health. DHB Sector Financial Reports 2017–18 2018 [Available from: https://www.health.govt.nz/new-zealand-health-system/key-health-sector-organisations-and-people/district-health-boards/accountability-and-funding/summary-financial-reports/dhb-sector-financial-reports-2017-18
Ministry of Health. Population of Tairawhiti DHB 2019 [Available from: https://www.health.govt.nz/new-zealand-health-system/my-dhb/tairawhiti-dhb/population-tairawhiti-dhb
Robson B, Purdie G, Simmonds S, Waa A, Faulkner R, Rameka R. Tairāwhiti District Health Board Māori Health Profile 2015 2015 [Available from: https://www.otago.ac.nz/wellington/otago152495.pdf
Färe R, Grosskopf S, Valdmanis V (1989) Capacity, competiton and efficiency in hospitals: A nonparametric approach. J Prod Anal 1(2):123–138
Health Workforce New Zealand. Health of the Health Workforce 2015 2015 [Available from: https://www.health.govt.nz/system/files/documents/publications/health-of-health-workforce-2015-feb16_0.pdf
West Coast District Health Board. West Coast physio shortages result in changes 2017 [Available from: https://www.wcdhb.health.nz/media-release/west-coast-physio-shortages-result/
West Coast District Health Board. West Coast Health System Quality Accounts 2014 [Available from: https://www.hqsc.govt.nz/assets/Health-Quality-Evaluation/PR/QA-2014-West-Coast-DHB.pdf
West Coast District Health Board. Annual Report 2013/14 2014 [Available from: https://www.wcdhb.health.nz/wp-content/uploads/ann_report_2014.pdf
West Coast District Health Board. Annual Report 2014/15 2015 [Available from: https://www.wcdhb.health.nz/wp-content/uploads/ann_report_2015.pdf
West Coast District Health Board. Annual Report 2015/16 2016 [Available from: https://www.wcdhb.health.nz/wp-content/uploads/ann_report_2016.pdf
West Coast District Health Board. Annual Report 2017/18 2018 [Available from: https://www.wcdhb.health.nz/about-us/document-library/annual-report-2017-2018/.
West Coast District Health Board. Quality Accounts 2018 2018 [Available from: https://www.wcdhb.health.nz/wp-content/uploads/Focus-on-People-2018-E-Version.pdf
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
None required.
Competing interests
The authors report there are no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Andrews, A., Emvalomatis, G. Do adjustment costs constrain public healthcare providers’ technical efficiency? Evidence from the New Zealand Public Healthcare System. Health Care Manag Sci (2024). https://doi.org/10.1007/s10729-024-09668-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10729-024-09668-5