Abstract
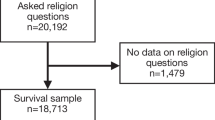
Research suggests a protective effect of religious service attendance on various health outcomes. However, most research has been done in religious societies, raising the question of whether these associations are also prominent in secular cultures. Here we examine mortality and hospitalisations by religious service attendance among men and women in a secular society. We performed a cohort study including 2987 Danes aged 40+ interviewed in SHARE from 2004 to 2007 and followed up in the Danish registries until 2018. We used Cox regressions and negative binomial regressions to examine associations, including interactions with sex and adjusting for age, wave, socioeconomic factors, lifestyle factors, body mass index, and history of diseases. Overall, 5.0% of men and 6.6% of women reported that they had taken part in a religious organisation within the last month. Among 848 deaths, we found lower mortality for people who attended religious services (hazard ratio (HR) 0.70; 95% CI 0.50–0.99). There was evidence for an association among women (HR 0.56; 95% CI 0.35–0.89), but not among men (HR 0.95; 95% CI 0.59–1.53). In contrast, regarding hospital admissions (n = 12,010), we found lower hospitalisation rates among men who attended religious services (incidence rate ratio (IRR) 0.67; 95% CI 0.45–0.98), whereas no association was found among women (IRR 0.95; 95% CI 0.70–1.29). Sensitivity analyses with E-values were moderately robust. Our results contribute to the limited literature on possible health benefits of religious service attendance in secular societies, demonstrating lower mortality among women and fewer hospitalisations among men.


Similar content being viewed by others
Data availability
SHARE data is free of charge for scientific use globally http://www.share-project.org/data-access.html.
Code availability
Not applicable.
References
Koenig HG, King DE, Carson VB. Handbook of religion and health. Oxford: Oxford University Press; 2012. p. 317.
Kim ES, VanderWeele TJ. Mediators of the association between religious service attendance and mortality. Am J Epidemiol. 2019;188(1):96–101.
Chen Y, Kim ES, VanderWeele TJ. Religious-service attendance and subsequent health and well-being throughout adulthood: evidence from three prospective cohorts. Int J Epidemiol. 2021;49(6):2030–40.
Oksuzyan A, Juel K, Vaupel JW, Christensen K. Men: good health and high mortality. Sex differences in health and aging. Aging Clin Exp Res. 2008;20(2):91–102.
Zuckerman P. Society without God: what the least religious nations can tell us about contentment. New York: New York University Press; 2008.
Hvidtjorn D, Hjelmborg J, Skytthe A, Christensen K, Hvidt NC. Religiousness and religious coping in a secular society: the gender perspective. J Relig Health. 2014;53(5):1329–41.
Olga S. Religion, self-rated health, and mortality: whether religiosity delays death depends on the cultural context. Soc Psychol Personal Sci. 2015;6(8):911–22.
Musick MA, House JS, Williams DR. Attendance at religious services and mortality in a national sample. J Health Soc Behav. 2004;45(2):198–213.
Hummer RA, Rogers RG, Nam CB, Ellison CG. Religious involvement and U.S. adult mortality. Demography. 1999;36(2):273–85.
Strawbridge WJ, Cohen RD, Shema SJ, Kaplan GA. Frequent attendance at religious services and mortality over 28 years. Am J Public Health. 1997;87(6):957–61.
Chida Y, Steptoe A, Powell LH. Religiosity/spirituality and mortality. A systematic quantitative review. Psychother Psychosom. 2009;78(2):81–90.
Li S, Stampfer MJ, Williams DR, VanderWeele TJ. Association of religious service attendance with mortality among women. JAMA Intern Med. 2016;176(6):777–85.
La Cour P, Avlund K, Schultz-Larsen K. Religion and survival in a secular region. A twenty year follow-up of 734 Danish adults born in 1914. Soc Sci Med (1982). 2006;62(1):157–64.
Teinonen T, Vahlberg T, Isoaho R, Kivela SL. Religious attendance and 12-year survival in older persons. Age Ageing. 2005;34(4):406–9.
VanderWeele TJ. Religion and health in Europe: cultures, countries, context. Eur J Epidemiol. 2017;32(10):857–61.
Ahrenfeldt LJ, Hvidt NC, Kjøller ST, Möller S, Lindahl-Jacobsen R. Religiousness and diseases in Europe: findings from SHARE. J Relig Health. 2019;58(6):1925–37.
Ahrenfeldt LJ, Möller S, Andersen-Ranberg K, Vitved AR, Lindahl-Jacobsen R, Hvidt NC. Religiousness and health in Europe. Eur J Epidemiol. 2017;32:1–9.
Opsahl T, Ahrenfeldt LJ, Moller S, Hvidt NC. Religiousness and depressive symptoms in Europeans: findings from the survey of health, ageing, and retirement in Europe. Public Health. 2019;175:111–9.
Ahrenfeldt LJ, Moller S, Hvidt NC, Lindahl-Jacobsen R. Religiousness and lifestyle among Europeans in SHARE. Public Health. 2018;165:74–81.
Herold SC, Hvidt NC, Möller S, Christensen K, Ahrenfeldt LJ. Is religiousness associated with better lifestyle and health among Danes? Findings from SHARE. J Relig Health. 2020;61:1621.
Ahrenfeldt LJ, Scheel-Hincke LL, Kjaergaard S, Moller S, Christensen K, Lindahl-Jacobsen R. Gender differences in cognitive function and grip strength: a cross-national comparison of four European regions. Eur J Pub Health. 2019;29(4):667–74.
Borsch-Supan A, Brandt M, Hunkler C, Kneip T, Korbmacher J, Malter F, et al. Data resource profile: the survey of health, ageing and retirement in Europe (SHARE). Int J Epidemiol. 2013;42(4):992–1001.
SHARE. REGLINK-SHAREDK 2021. http://www.share-project.org/special-data-sets/record-linkage-project/reglink-sharedk.html
Bergmann M, Kneip T, Luca GD, Scherpenzeel A. Survey participation in the Survey of Health, Ageing and Retirement in Europe (SHARE), Wave 1–7. Based on Release 7.0.0. 2019.
Thygesen LC, Daasnes C, Thaulow I, Bronnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Pub Health. 2011;39(7 Suppl):12–6.
Pedersen CB. The Danish civil registration system. Scand J Pub Health. 2011;39(7 Suppl):22–5.
Helweg-Larsen K. The Danish register of causes of death. Scand J Pub Health. 2011;39(7 Suppl):26–9.
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish national patient registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–90.
SHARE. Survey of Health, Ageing and Retirement in Europe. Release guide 7.1.0. http://www.share-project.org/fileadmin/pdf_documentation/SHARE_release_guide_7-1-1.pdf; 2020
Ariel L, Maya BM, Tyler JV. EVALUE: Stata module for conducting sensitivity analyses for unmeasured confounding in observational studies. S458592 ed: Boston College Department of Economics; 2019.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268–74.
VanderWeele TJ, Mathur MB, Chen Y. Outcome-Wide Longitudinal Designs for Causal Inference: A New Template for Empirical Studies. Stat Sci. 2020;35(3):437–66.
Ransome Y. Is investing in religious institutions a viable pathway to reduce mortality in the population? Soc Sci Med. 1982;2020(262):113106.
Pawlikowski J, Bialowolski P, Weziak-Bialowolska D, VanderWeele TJ. Religious service attendance, health behaviors and well-being-an outcome-wide longitudinal analysis. Eur J Public Health. 2019;29(6):1177–83.
Chen Y, Koh HK, Kawachi I, Botticelli M, VanderWeele TJ. Religious service attendance and deaths related to drugs, alcohol, and suicide among US Health Care professionals. JAMA Psychiat. 2020;77(7):737–44.
Spence ND, Farvid MS, Warner ET, VanderWeele TJ, Tworoger SS, Argentieri MA, et al. Religious service attendance, religious coping, and risk of hypertension in women participating in the nurses’ health study II. Am J Epidemiol. 2020;189(3):193–203.
Pawlikowski J, Bialowolski P, Weziak-Bialowolska D, VanderWeele TJ. Religious service attendance, health behaviors and well-being-an outcome-wide longitudinal analysis. Eur J Pub Health. 2019;29:1177.
VanderWeele TJ, Yu J, Cozier YC, Wise L, Argentieri MA, Rosenberg L, et al. Attendance at religious services, prayer, religious coping, and religious/spiritual identity as predictors of all-cause mortality in the black women’s health study. Am J Epidemiol. 2017;185(7):515–22.
VanderWeele TJ, Li S, Tsai AC, Kawachi I. Association between religious service attendance and lower suicide rates among US women. JAMA Psychiat. 2016;73(8):845–51.
Strawbridge WJ, Cohen RD, Shema SJ. Comparative strength of association between religious attendance and survival. Int J Psychiatry Med. 2000;30(4):299–308.
Boussarsar M, Bouchoucha S. Dying at home: cultural and religious preferences. Intensive Care Med. 2006;32(11):1917–8.
Popper KR. The logic of scientific discovery. Hutchinson; 1959.
VanderWeele TJ, Balboni TA, Koh HK. Invited commentary: religious service attendance and implications for clinical care, community participation, and public health. Am J Epidemiol. 2022;191(1):31–5.
Stripp TK, Büssing A, Wehberg S, Andersen HS, Kørup AK, Pedersen HF, et al. Measuring spiritual needs in a secular society: validation and clinimetric properties of the Danish 20-item spiritual needs questionnaire. J Relig Health. 2022;61:3542.
Hvidt NC, Nielsen KT, Korup AK, Prinds C, Hansen DG, Viftrup DT, et al. What is spiritual care? Professional perspectives on the concept of spiritual care identified through group concept mapping. BMJ Open. 2020;10(12):e042142.
Stripp TK, Wehberg S, Büssing A, Andersen-Ranberg K, Jensen LH, Henriksen FL, et al. Protocol for EXICODE: the EXIstential health COhort DEnmark—a register and survey study of adult Danes. BMJ Open. 2022;12(6):e058257.
Acknowledgements
This paper uses data from SHARE Waves 1 and 2 (DOIs: https://doi.org/10.6103/SHARE.w1.600, https://doi.org/10.6103/SHARE.w2.600); see Börsch-Supan et al. for methodological details [22]. The European Commission has funded the SHARE data collection, DG RTD through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812), FP7 (SHARE-PREP: GA N°211909, SHARE-LEAP: GA N°227822, SHARE M4: GA N°261982, DASISH: GA N°283646) and Horizon 2020 (SHARE-DEV3: GA N°676536, SHARE-COHESION: GA N°870628, SERISS: GA N°654221, SSHOC: GA N°823782, SHARE-COVID19: GA N°101015924) and by DG Employment, Social Affairs & Inclusion through VS 2015/0195, VS 2016/0135, VS 2018/0285, VS 2019/0332, and VS 2020/0313. Furthermore, additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C, RAG052527A) and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Funding
This research was funded by Demography of Sex Differences in Health and Survival, grant number P01 AG031719 (LJA).
Author information
Authors and Affiliations
Contributions
LJA: Conceptualisation, Formal analysis, Investigation, Methodology, Project administration, Visualisation, Roles/Writing—original draft. SM: Formal analysis, Methodology NCH: Supervision TJV: Supervision TKS: Roles/Writing—editing and revisions, Formal analysis, Conceptualisation, Supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Ethics approval was handled by SHARE (Survey of Health, Aging, and retirement in Europe). See: A., Jürges, Hendrik. The Survey of Health, Aging, and Retirement in Europe – Methodology. MEA, 2005.
Consent to participate
Consent was obtained by SHARE (Survey of Health, Aging, and retirement in Europe). See: Börsch-Supan, A., Jürges, Hendrik. The Survey of Health, Aging, and Retirement in Europe – Methodology. MEA, 2005.
Consent for publication
Consent was obtained by SHARE (Survey of Health, Aging, and retirement in Europe). See: Börsch-Supan, A., Jürges, Hendrik. The Survey of Health, Aging, and Retirement in Europe – Methodology. MEA, 2005.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ahrenfeldt, L.J., Möller, S., Hvidt, N.C. et al. Effect of religious service attendance on mortality and hospitalisations among Danish men and women: longitudinal findings from REGLINK-SHAREDK. Eur J Epidemiol 38, 281–289 (2023). https://doi.org/10.1007/s10654-023-00964-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-023-00964-y