Abstract
Elevated blood pressure and hypertension have been associated with increased risk of atrial fibrillation in a number of epidemiological studies, however, the strength of the association has differed between studies. We conducted a systematic review and meta-analysis of the association between blood pressure and hypertension and atrial fibrillation. PubMed and Embase databases were searched for studies of hypertension and blood pressure and atrial fibrillation up to June 6th 2022. Cohort studies reporting adjusted relative risk (RR) estimates and 95% confidence intervals (CIs) of atrial fibrillation associated with hypertension or blood pressure were included. A random effects model was used to estimate summary RRs. Sixty eight cohort studies were included in the meta-analysis. The summary RR was 1.50 (95% CI: 1.42–1.58, I2 = 98.1%, n = 56 studies) for people with hypertension compared to those without hypertension (1,080,611 cases, 30,539,230 participants), 1.18 (95% CI: 1.16–1.21, I2 = 65.9%, n = 37 studies) per 20 mmHg increase in systolic blood pressure (346,471 cases, 14,569,396 participants), and 1.07 (95% CI: 1.03–1.11, I2 = 91.5%, n = 22 studies) per 10 mmHg increase in diastolic blood pressure (332,867 cases, 14,354,980 participants). There was evidence of a nonlinear association between diastolic blood pressure and atrial fibrillation with a steeper increase in risk at lower levels of diastolic blood pressure, but for systolic blood pressure the association appeared to be linear. For both systolic and diastolic blood pressure, the risk increased even within the normal range of blood pressure and persons at the high end of systolic and diastolic blood pressure around 180/110 mmHg had a 1.8–2.3 fold higher risk of atrial fibrillation compared to those with a blood pressure of 90/60 mmHg. These results suggest that elevated blood pressure and hypertension increases the risk of atrial fibrillation and there is some increase in risk even within the normal range of systolic and diastolic blood pressure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrial fibrillation presents a considerable public health burden and is the most common type of arrhythmia affecting around 1–2% of the general population, increasing to around 10% of persons by 80 years of age [1]. Five million incident cases were diagnosed worldwide in 2010 [2] and the prevalence of atrial fibrillation has been estimated at 33 million in 2015 [3]. In the USA the prevalence of atrial fibrillation has been projected to increase from 2.3 million in 1996–1997 to 5.6 million by 2050 [4]. Patients with atrial fibrillation are at increased risk of a number of complications, most notably stroke, heart failure, dementia and all-cause mortality [5, 6]. Several risk factors for atrial fibrillation have been established including age, sex, diabetes, coronary heart disease, heart failure, smoking, alcohol, obesity, low physical activity and possibly high intensity physical activity [7,8,9,10,11,12,13,14,15].
Elevated blood pressure is the leading cause of death and disability-adjusted life-years (DALYs) globally with 10.4 million deaths and 218 million DALYs attributable to elevated systolic blood pressure in 2017 according to the Global Burden of Disease Study [16]. Although elevated blood pressure is an established risk factor for several cardiovascular diseases, data regarding blood pressure and risk of atrial fibrillation have to our knowledge not been summarized in a meta-analysis. A large number of cohort studies have investigated the association between hypertension and the risk of atrial fibrillation [7,8,9, 17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65], and most of these found an increased risk [7, 8, 17,18,19,20,21,22, 24,25,26,27,28,29,30,31, 33, 34, 36,37,38,39,40,41,42,43,44,45,46,47,48,49, 51,52,53,54,55,56,57,58,59,60,61,62, 64, 65], with few studies reporting no association [9, 23, 32, 35, 50, 63], however, the strength of the association has differed considerably between studies with reported relative risks reported ranging from 0.93 to 2.85 [7,8,9, 17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]. In addition, several studies have investigated the association between systolic [8, 18, 20, 29, 33, 34, 39, 41, 42, 44, 46, 51, 55, 63, 65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80] or diastolic [8, 29, 33, 39, 41, 44, 46, 51, 55, 67,68,69,70, 72,73,74, 79, 81] blood pressure and risk of atrial fibrillation with most studies reporting increased risk for increasing systolic blood pressure [18, 20, 29, 34, 39, 41, 44, 46, 51, 55, 65,66,67,68,69,70,71,72, 74,75,76,77,78,79,80], while results have been more mixed for diastolic blood pressure with some showing an increased risk [39, 44, 51, 55, 67,68,69, 72, 79, 82] but other studies showing no association [8, 29, 33, 46, 70, 73, 74, 81], or even reduced risk [41, 77] with higher diastolic blood pressure.
Establishing whether hypertension and elevated blood pressure increases the risk of atrial fibrillation would be important from a preventive point of view as it is a risk factor that could be modified by diet, physical activity, weight control and pharmaceutical drugs [83]. In addition it would be useful to better characterize the strength and shape of the dose–response relationship between blood pressure and atrial fibrillation to clarify whether the association is dose-dependent or if there are threshold effects. We conducted a systematic review and meta-analysis of cohort studies on hypertension and blood pressure in relation to the risk of atrial fibrillation to clarify the strength and shape of the dose–response relationship, and to identify potential sources of heterogeneity in the results.
Material and methods
Search strategy and inclusion criteria
We searched Pubmed, and Embase databases up to June 9th 2022 for eligible studies. The search strategy is provided in the Supplementary Text. We followed standard criteria for conducting and reporting meta-analyses [84]. In addition, we searched the reference lists of the identified publications for further studies.
Study selection
We included published retrospective and prospective cohort studies and nested case–control studies within cohorts that investigated the association between blood pressure or hypertension and the risk of atrial fibrillation (any type). Retrospective case–control studies were excluded because of their potential for recall bias and selection bias and cross-sectional studies were excluded because of difficulties in establishing cause and effect relationships. Estimates of the relative risk adjusted for at least one confounding factor had to be available with the 95% confidence intervals (CIs) in the publication. Conference abstracts, grey literature and non-English publications were not included. When multiple publications were available from the same study, the study with the largest number of cases was used in general. However, overlapping publications were used in specific subgroup analyses by sex or ethnicity, when the article used for the main analysis did not report such stratified analyses. Overlapping publications that reported risk estimates in three categories or more were also used for the nonlinear dose–response analyses (as the nonlinear analysis requires categorical data) if the article included in the main analysis only reported risk estimates on a continuous scale. A list of the excluded studies can be found in Supplementary Table 1. DA, YMS, EK and TF did the study selection in duplicate and any disagreements were resolved by discussion.
Data extraction
The following data were extracted from each study: The first author’s last name, publication year, country where the study was conducted, study period, sample size, number of cases and participants, exposure (hypertension, systolic blood pressure, or diastolic blood pressure), subgroup (e.g. sex, race), relative risks (RRs) and 95% CIs for hypertension versus no hypertension or for increments in systolic or diastolic blood pressure and variables adjusted for in the analysis. DA did the data extraction and it was checked for accuracy by YMS.
Statistical methods
We calculated summary RRs (95% CIs) of atrial fibrillation for participants with hypertension compared with participants without hypertension and for systolic and diastolic blood pressure using the random-effects model by DerSimonian and Laird [85] which takes into account both within and between study variation (heterogeneity). The average of the natural logarithm of the RRs was estimated and the RR from each study was weighted by the inverse of its variance. Linear dose–response analyses were conducted per 20 mmHg for systolic blood pressure and per 10 mmHg for diastolic blood pressure (consistent with previous studies [86,87,88]) using the method of Greenland and Longnecker [89]. For studies that reported blood pressure by ranges we estimated the midpoint for each category by calculating the average of the upper and lower cut-off points. For open-ended categories we used the width of the adjacent interval to estimate an upper or lower cut-off value for the extreme category. Fractional polynomial models were used to investigate a potential nonlinear association between systolic and diastolic blood pressure and risk of atrial fibrillation [90]. A log-likelihood test was used to test for nonlinearity [91].
Heterogeneity between studies was evaluated using Q and I2 statistics [92]. I2 is an estimate of how much of the heterogeneity that is due to between study variation rather than chance. I2-values of 25%, 50% and 75% indicates low, moderate and high heterogeneity respectively. We conducted main analyses (all studies combined) and stratified by study characteristics such as sample size, number of cases, whether prevalent cases were excluded or not, geographic location, study quality and by adjustment for confounding factors to investigate potential sources of heterogeneity and we used meta-regression analyses to test for differences in summary estimates between subgroups. Study quality was assessed using the Newcastle Ottawa scale which rates studies according to selection, comparability and outcome assessment with a score range from 0 to 9 [93].
Publication bias was assessed using Egger’s test [94] and by inspection of funnel plots. The statistical analyses were conducted using the software package Stata, version 13.1 software (StataCorp, Texas, US).
Results
From a total of 32,876 records that were identified by the search we included a total of 69 publications [7,8,9, 17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82] with data from 68 cohort studies (two of these were nested case–control studies within cohort studies [21, 66]) in the systematic review and meta-analysis of hypertension and blood pressure and atrial fibrillation (Fig. 1). Five of these publications were identified from separate searches on other risk factors for atrial fibrillation [9, 21, 32, 34, 42]. Each of two publications reported results from two studies combined [73, 81], and another publication reported results from six studies combined [65]. Two publications [42, 75] reported results from two separate studies each and one publication reported results from five separate studies [29], two of which were included in the main analysis (the other three were surpassed by more recent publications, but results of two of these duplicate studies were included in subgroup analyses by ethnicity). Twenty six studies (23 publications) [18, 20, 21, 25, 27,28,29,30, 33, 36, 42, 43, 48, 54, 64, 65, 69, 71,72,73, 75, 76, 78] were from Europe, twenty studies (25 publications) [7, 17, 19, 22, 24, 26, 29, 31, 34, 37, 40, 41, 45,46,47, 52, 53, 56, 59, 67, 68, 70, 74, 77, 81] were from North America, nineteen studies (19 publications) [23, 32, 35, 38, 39, 44, 49,50,51, 55, 57, 60,61,62,63, 66, 79, 80, 82] were from Asia, and three studies (3 publications) [8, 9, 58] were from Australia.
Fifty six cohort studies (52 publications, 52 risk estimates) [7,8,9, 17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65] were included in the analysis of hypertension and atrial fibrillation risk including 1,080,611 cases and 30,539,230 participants (Fig. 1, Table 1). Data on hypertension and atrial fibrillation by ethnicity [29, 59] and sex [25] from three studies (ARIC, REGARDS, and Malmö Diet and Cancer Study) were only included in the respective subgroup analyses as the publications overlapped with more recent publications from the same studies which were used for the main analysis [27, 45, 56]. The summary relative risk for persons with hypertension compared to persons without hypertension was 1.50 (95% CI: 1.42–1.58, I2 = 98.1%, pheterogeneity < 0.0001) (Fig. 2). There was no evidence of publication bias neither with Egger’s test (p = 0.74) or by inspection of the funnel plot (Supplementary Fig. 1). The summary RR ranged from 1.47 (95% CI: 1.42–1.52) when excluding the study by Zoller et al. [30] to 1.51 (95% CI: 1.43–1.59) when excluding the study by Sano et al. [53] (Supplementary Fig. 2).
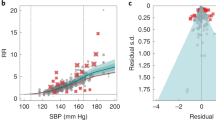
Thirty seven cohort studies (28 publications, 31 risk estimates) [8, 18, 20, 29, 33, 34, 39, 41, 42, 44, 46, 51, 55, 63, 65,66,67, 69,70,71,72,73,74,75, 77,78,79,80] (347,813 cases, 14,565,763 participants) were included in the analysis of systolic blood pressure and atrial fibrillation (Table 2). The summary RR was 1.19 (95% CI: 1.16–1.21, I2 = 68.4%, pheterogeneity < 0.0001) per 20 mmHg increment (Fig. 3a). There was no evidence of publication bias with Egger's test (p = 0.46), but some indication of asymmetry in the funnel plot (Supplementary Fig. 3a). When using the trim and fill method, eight studies were added, but the results were similar, summary RR = 1.17 (95% CI: 1.14–1.19) (Supplementary Fig. 4). The summary RR ranged from 1.18 (95% CI: 1.16–1.20) when the Atherosclerosis Risk in Communities Study [77] was excluded to 1.20 (95% CI: 1.18–1.22) when a pooled analysis [65] was excluded (Supplementary Fig. 5). Ten cohort studies [18, 34, 39, 55, 67,68,69, 76, 79, 80] were included in the nonlinear dose–response analysis. Although the test for nonlinearity was significant, pnonlinearity < 0.0001, the association was approximately linear, and there was a dose-dependent increase in risk with increasing systolic blood pressure from a systolic blood pressure level of 90 mmHg and above (Fig. 3b).
Twenty three cohort studies (19 publications, 21 risk estimates) [8, 29, 33, 39, 41, 44, 46, 51, 55, 67, 69, 70, 72,73,74, 77, 79, 81, 82] (333,901 cases, 14,387,470 participants) were included in the analysis of diastolic blood pressure and atrial fibrillation. The summary RR was 1.06 (95% CI: 1.02–1.10, I2 = 92.1%, pheterogeneity < 0.0001) per 10 mmHg increment (Fig. 3c). There was no evidence of publication bias with Egger's test (p = 0.55) or by inspection of the funnel plot (Supplementary Fig. 6). The summary RR ranged from 1.05 (95% CI: 1.00–1.10) when excluding the UK GPRD study [72] to 1.07 (95% CI: 1.03–1.11) when excluding a study at Vanderbilt University [41] (Supplementary Fig. 7). Six cohort studies [39, 55, 67,68,69, 79] were included in the nonlinear dose–response analysis of diastolic blood pressure and atrial fibrillation. There was evidence of nonlinearity (pnonlinearity < 0.0001) with a slightly steeper increase in risk at lower levels of diastolic blood pressure than at higher levels, however, there was an increased risk from a diastolic blood pressure level of around 60 mmHg (Fig. 3d).
Subgroup and sensitivity analyses
There were positive associations between hypertension and risk of atrial fibrillation across all subgroup analyses defined by sex, duration of follow-up, geographic location, number of cases, whether prevalent cases were excluded or not, study quality and adjustment for confounding (and in some cases potentially mediating) factors (including age, education, alcohol, smoking, BMI, physical activity, diabetes, hyperlipidemia, coronary heart disease, heart failure, valvular heart disease, left ventricular hypertrophy, and kidney disease), although the number of studies was small in some subgroups (Table 3). With meta-regression analyses there was some indication of heterogeneity between some subgroups for hypertension, with a stronger association among European studies than studies from the other geographic locations (p = 0.02), and a weaker association among studies with adjustment for smoking (p = 0.03) when compared to those without such adjustment. Further subgroup analyses by ethnicity showed summary RRs of 1.53 (95% CI: 1.29–1.80, I2 = 70.4%, n = 5) for Caucasians [26, 29, 45, 59] and 1.35 (95% CI: 1.16–1.59, I2 = 7.5%, n = 6) for African Americans [26, 29, 45, 46, 59] with no significant heterogeneity between subgroups (p = 0.77) (Supplementary Fig. 8).
There was evidence of heterogeneity in the subgroup analysis of systolic blood pressure and atrial fibrillation when stratified by adjustment for education (p = 0.03) and physical activity (p = 0.04) with stronger associations among studies with compared to without such adjustments, however, relatively few studies made such adjustments. For diastolic blood pressure there was heterogeneity in analyses stratified by sex (p = 0.009) and by adjustment for BMI or obesity (p = 0.04), coronary heart disease (p = 0.01), and heart failure (p = 0.009). However, the association was weaker in studies of both sexes combined than in studies among either men or women, and there was no heterogeneity when comparing men with women (and excluding studies in both sexes combined) (Table 3). There was no association in studies that adjusted for BMI or obesity, coronary heart disease, or heart failure, but a positive association in studies that did not make such adjustments (Table 3).
Mean (median) study quality scores were 7.7 (8.0) for the analysis of hypertension, 7.8 (8.0) for systolic blood pressure, and 7.8 (8.0) for diastolic blood pressure.
Discussion
This meta-analysis of cohort studies suggests that persons with hypertension have a 50% increase in the relative risk of developing atrial fibrillation compared to persons without hypertension. There was a 19% increase in the relative risk of atrial fibrillation per 20 mmHg increase in systolic blood pressure and 6% increase in relative risk per 10 mmHg of diastolic blood pressure. Although the test for nonlinearity was significant both for systolic and diastolic blood pressure in relation to atrial fibrillation, the association with systolic blood pressure appeared to be approximately linear, while the association for diastolic blood pressure was nonlinear with a slightly steeper increase in risk at lower levels than at higher levels of diastolic blood pressure. However, there was an increased risk even within what is considered the normal blood pressure range and the lowest risk was observed at a systolic and diastolic blood pressure of 90/60 mmHg, respectively, while there was a 1.8–2.3 fold increase in risk at the high end of systolic and diastolic blood pressure around 180/110 mmHg. Positive associations were observed both in men and women, and among European, American, Asian and Australian studies, however, data from other regions are lacking. In the few studies that reported results stratified by ethnicity, there was a positive association between hypertension and atrial fibrillation among both Caucasians and African Americans. Our findings of an increased risk of atrial fibrillation with higher systolic and diastolic blood pressure are partly consistent with several recent Mendelian Randomization (MR) studies [95,96,97], as well as a randomized open-label trial which found a 54% reduction in risk of new-onset atrial fibrillation among participants allocated to tight vs usual blood systolic blood pressure control (target of < 130 mmHg and < 140 mmHg, respectively) [98], suggesting a possible causal relation between elevated blood pressure and atrial fibrillation. The MR studies reported stronger associations between blood pressure and atrial fibrillation when compared to the current analysis with 17–19% vs. 9% increases in risk of atrial fibrillation per 10 mmHg increase in systolic blood pressure and 25–29% vs. 6% increases in risk of atrial fibrillation per 10 mmHg increase in diastolic blood pressure, respectively. The stronger associations observed in the MR studies could be due to a stronger impact of lifelong elevated blood pressure that may be better captured in the MR studies, and potential overadjustment for intermediate risk factors in some of the observational studies. We did not observe significant differences in the association between hypertension or blood pressure and atrial fibrillation by sex, in contrast to what has been previously observed for cardiovascular disease incidence [99], but consistent with that observed for stroke [100] and cardiovascular disease mortality [99]. This suggests that for the prevention of atrial fibrillation, blood pressure lowering may be equally important among men and women.
Several biological pathways could explain an increased risk of atrial fibrillation in patients with hypertension. Elevated blood pressure increases the risk of coronary heart disease and heart failure [101], conditions that predisposes to atrial fibrillation [29, 34, 47, 48]. Hypertension induces structural remodelling of the left atrium with excessive fibroblast proliferation, and fibroblasts can switch and proliferate to myofibroblasts which have a higher profibrotic potential and also contribute to collagen accumulation [102]. Epidemiological studies have shown that elevated blood pressure predisposes to left ventricular hypertrophy [103,104,105,106], which again increases the risk of atrial fibrillation [17, 20, 29, 34, 41, 51]. It also stimulates apoptosis and inflammation of the cardiomyocytes, leading to fibrosis and left ventricular hypertrophy. Activation of the renin–angiotensin–aldosterone system and autonomic dysregulation are major factors behind these changes. Long-term hypertension can through ventricular thickening, left ventricular hypertrophy and impaired left ventricular systolic-diastolic function increase atrial pressure, ultimately leading to atrial stretch, enlargement and deterioration of atrial contraction [102]. Dysregulation of the autonomic nervous system may also contribute to the development of atrial fibrillation and it has been shown that both sympathetic and parasympathetic overactivation may trigger atrial fibrillation [102].
The present systematic review and meta-analysis has some limitations that need to be discussed. Persons with hypertension often have less healthy lifestyles than persons without hypertension, including higher BMI, less physical activity and they may be more likely to smoke. Several of the included studies adjusted for the most important confounding factors and the results persisted across most subgroup analyses, and we found little evidence of heterogeneity between these subgroups. However, we cannot exclude the possibility that residual confounding could partly explain the results. There was very high heterogeneity in the analyses of hypertension and diastolic blood pressure and moderately high heterogeneity in the analysis of systolic blood pressure and this persisted in many of the subgroup analyses, but there was lower heterogeneity in studies with a longer duration of follow-up. The heterogeneity observed appeared to be more driven by differences in the effect sizes rather than differences in the direction of the association, as all except one study found positive associations between hypertension or systolic blood pressure and atrial fibrillation. Since the studies only had one baseline assessment of hypertension status or blood pressure, regression dilution bias could have attenuated the association between hypertension or blood pressure and risk of atrial fibrillation. Some participants with high blood pressure at baseline may have undergone subsequent treatment for high blood pressure with pharmaceutical medications or lifestyle changes, which would have lowered their blood pressure, but any such effects would most likely have led to conservative estimates of the associations between hypertension and blood pressure and risk of atrial fibrillation. Some of the included studies may also have over-adjusted by including hypertension status and blood pressure in the same models, adjusting rather than stratifying for blood pressure treatment, and/or by adjusting for potentially intermediary conditions such as coronary heart disease, heart failure, valvular heart disease, and left ventricular hypertrophy in the multivariable models. Any further studies might want to adjust for potential confounders and mediators separately to evaluate the impact of both on the observed associations.
Strengths of the present meta-analysis include (1) the cohort design of the included studies (which avoids recall bias and reduces the potential for selection bias), (2) the detailed subgroup and sensitivity analyses, (3) the very large sample size with 14.3–30.5 million participants and 333,000 to 1,080,000 cases providing a more robust estimate of the association between blood pressure and hypertension and risk of atrial fibrillation than most individual studies, and (4) the detailed dose–response analyses. Our findings have important clinical and public health implications as the number of people with hypertension worldwide increased from 594 million in 1975 to 1.13 billion in 2015, mainly due to population growth and ageing, but also due to lifestyle factors [107]. This increase in the number of people with hypertension may at least have partly contributed to increased rates of atrial fibrillation. Routine screening for hypertension and lifestyle interventions to reduce blood pressure that emphasize healthy diets, physical activity, weight control and proper pharmaceutical treatment of hypertension may therefore also reduce the risk of atrial fibrillation as well as other cardiovascular complications.
Conclusion
In conclusion, this meta-analysis suggests that people with hypertension have a 50% increase in the relative risk of developing atrial fibrillation compared to those without hypertension. Increasing systolic and diastolic blood pressure even within the normal range was associated with increased risk and at the high end was associated with a twofold increase in risk. These results strongly support a role of elevated blood pressure in the development of atrial fibrillation.
References
Kannel WB, Wolf PA, Benjamin EJ, Levy D. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol. 1998;82(8A):2N-9N.
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum RF, Kim YH, McAnulty JH Jr, Zheng ZJ, Forouzanfar MH, Naghavi M, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014;129(8):837–47.
GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–602.
Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285(18):2370–5.
Odutayo A, Wong CX, Hsiao AJ, Hopewell S, Altman DG, Emdin CA. Atrial fibrillation and risks of cardiovascular disease, renal disease, and death: systematic review and meta-analysis. BMJ. 2016;6(354):i4482.
Liu DS, Chen J, Jian WM, Zhang GR, Liu ZR. The association of atrial fibrillation and dementia incidence: a meta-analysis of prospective cohort studies. J Geriatr Cardiol. 2019;16(3):298–306.
Conen D, Glynn RJ, Sandhu RK, Tedrow UB, Albert CM. Risk factors for incident atrial fibrillation with and without left atrial enlargement in women. Int J Cardiol. 2013;168(3):1894–9.
Knuiman M, Briffa T, Divitini M, Chew D, Eikelboom J, McQuillan B, Hung J. A cohort study examination of established and emerging risk factors for atrial fibrillation: the Busselton Health Study. Eur J Epidemiol. 2014;29(3):181–90.
Diouf I, Magliano DJ, Carrington MJ, Stewart S, Shaw JE. Prevalence, incidence, risk factors and treatment of atrial fibrillation in Australia: the Australian Diabetes, Obesity and Lifestyle (AusDiab) longitudinal, population cohort study. Int J Cardiol. 2016;15(205):127–32.
Aune D, Feng T, Schlesinger S, Janszky I, Norat T, Riboli E. Diabetes mellitus, blood glucose and the risk of atrial fibrillation: a systematic review and meta-analysis of cohort studies. J Diabetes Complicat. 2018;32(5):501–11.
Aune D, Schlesinger S, Norat T, Riboli E. Tobacco smoking and the risk of atrial fibrillation: a systematic review and meta-analysis of prospective studies. Eur J Prev Cardiol. 2018;25(13):1437–51.
Larsson SC, Drca N, Wolk A. Alcohol consumption and risk of atrial fibrillation: a prospective study and dose-response meta-analysis. J Am Coll Cardiol. 2014;64(3):281–9.
Aune D, Sen A, Schlesinger S, Norat T, Janszky I, Romundstad P, Tonstad S, Riboli E, Vatten LJ. Body mass index, abdominal fatness, fat mass and the risk of atrial fibrillation: a systematic review and dose-response meta-analysis of prospective studies. Eur J Epidemiol 2017.
Tikkanen E, Gustafsson S, Ingelsson E. Associations of fitness, physical activity, strength, and genetic risk with cardiovascular disease: longitudinal analyses in the UK biobank study. Circulation. 2018;137(24):2583–91.
Thelle DS, Selmer R, Gjesdal K, Sakshaug S, Jugessur A, Graff-Iversen S, Tverdal A, Nystad W. Resting heart rate and physical activity as risk factors for lone atrial fibrillation: a prospective study of 309,540 men and women. Heart. 2013;99(23):1755–60.
GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1923–94.
Krahn AD, Manfreda J, Tate RB, Mathewson FA, Cuddy TE. The natural history of atrial fibrillation: incidence, risk factors, and prognosis in the Manitoba Follow-Up Study. Am J Med. 1995;98(5):476–84.
Wilhelmsen L, Rosengren A, Lappas G. Hospitalizations for atrial fibrillation in the general male population: morbidity and risk factors. J Intern Med. 2001;250(5):382–9.
Tsang TS, Barnes ME, Bailey KR, Leibson CL, Montgomery SC, Takemoto Y, Diamond PM, Marra MA, Gersh BJ, Wiebers DO, Petty GW, Seward JB. Left atrial volume: important risk marker of incident atrial fibrillation in 1655 older men and women. Mayo Clin Proc. 2001;76(5):467–75.
Friberg J, Buch P, Scharling H, Gadsbphioll N, Jensen GB. Rising rates of hospital admissions for atrial fibrillation. Epidemiology. 2003;14(6):666–72.
Ruigomez A, Johansson S, Wallander MA, Rodriguez LA. Incidence of chronic atrial fibrillation in general practice and its treatment pattern. J Clin Epidemiol. 2002;55(4):358–63.
Gami AS, Hodge DO, Herges RM, Olson EJ, Nykodym J, Kara T, Somers VK. Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J Am Coll Cardiol. 2007;49(5):565–71.
Kim HJ, Young KO, Sung J, Kim JH, Song YB, Lee W-S, Choi J-O, Shin D-H, Cho S-W, Choi JH, Hahn J-Y, Kim JS. Risk factors for predicting new-onset atrial fibrillation in persons who received health screening tests. Korean Circulat J. 2007;37(12):609–15.
Nichols GA, Reinier K, Chugh SS. Independent contribution of diabetes to increased prevalence and incidence of atrial fibrillation. Diabetes Care. 2009;32(10):1851–6.
Smith JG, Platonov PG, Hedblad B, Engstrom G, Melander O. Atrial fibrillation in the Malmo Diet and Cancer study: a study of occurrence, risk factors and diagnostic validity. Eur J Epidemiol. 2010;25(2):95–102.
Lipworth L, Okafor H, Mumma MT, Edwards TL, Roden DM, Blot WJ, Darbar D. Race-specific impact of atrial fibrillation risk factors in blacks and whites in the southern community cohort study. Am J Cardiol. 2012;110(11):1637–42.
Smith JG, Melander O, Sjogren M, Hedblad B, Engstrom G, Newton-Cheh C, Platonov PG. Genetic polymorphisms confer risk of atrial fibrillation in patients with heart failure: a population-based study. Eur J Heart Fail. 2013;15(3):250–7.
Nyrnes A, Mathiesen EB, Njolstad I, Wilsgaard T, Lochen ML. Palpitations are predictive of future atrial fibrillation. An 11-year follow-up of 22,815 men and women: the Tromso Study. Eur J Prev Cardiol. 2013;20(5):729–36.
Alonso A, Krijthe BP, Aspelund T, Stepas KA, Pencina MJ, Moser CB, Sinner MF, Sotoodehnia N, Fontes JD, Janssens AC, Kronmal RA, Magnani JW, et al. Simple risk model predicts incidence of atrial fibrillation in a racially and geographically diverse population: the CHARGE-AF consortium. J Am Heart Assoc. 2013;2(2):e000102.
Zoller B, Li X, Sundquist J, Sundquist K. Neighbourhood deprivation and hospitalization for atrial fibrillation in Sweden. Europace. 2013;15(8):1119–27.
Perez MV, Wang PJ, Larson JC, Soliman EZ, Limacher M, Rodriguez B, Klein L, Manson JE, Martin LW, Prineas R, Connelly S, Hlatky M, et al. Risk factors for atrial fibrillation and their population burden in postmenopausal women: the Women’s Health Initiative Observational Study. Heart. 2013;99(16):1173–8.
Sano F, Ohira T, Kitamura A, Imano H, Cui R, Kiyama M, Okada T, Yamagishi K, Sankai T, Tanigawa T, Kario K, Iso H. Heavy alcohol consumption and risk of atrial fibrillation. The Circulatory Risk in Communities Study (CIRCS). Circ J. 2014;78(4):955–61.
Pfister R, Bragelmann J, Michels G, Wareham NJ, Luben R, Khaw KT. Performance of the CHARGE-AF risk model for incident atrial fibrillation in the EPIC Norfolk cohort. Eur J Prev Cardiol. 2015;22(7):932–9.
Schnabel RB, Yin X, Gona P, Larson MG, Beiser AS, McManus DD, Newton-Cheh C, Lubitz SA, Magnani JW, Ellinor PT, Seshadri S, Wolf PA, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet. 2015;386(9989):154–62.
Suzuki H, Ohira T, Takeishi Y, Hosoya M, Yasumura S, Satoh H, Kawasaki Y, Takahashi A, Sakai A, Ohtsuru A, Kobashi G, Ozasa K, et al. Increased prevalence of atrial fibrillation after the Great East Japan Earthquake: results from the Fukushima health management survey. Int J Cardiol. 2015;1(198):102–5.
Nystrom PK, Carlsson AC, Leander K, De FU, Hellenius ML, Gigante B. Obesity, metabolic syndrome and risk of atrial fibrillation: a Swedish, prospective cohort study. PLoS One. 2015;10(5):e0127111.
Qureshi WT, Alirhayim Z, Blaha MJ, Juraschek SP, Keteyian SJ, Brawner CA, Al-Mallah MH. Cardiorespiratory fitness and risk of incident atrial fibrillation: results from the henry ford exercise testing (FIT) project. Circulation. 2015;131(21):1827–34.
Guo Y, Tian Y, Wang H, Si Q, Wang Y, Lip GYH. Prevalence, incidence, and lifetime risk of atrial fibrillation in China: new insights into the global burden of atrial fibrillation. Chest. 2015;147(1):109–19.
Kokubo Y, Watanabe M, Higashiyama A, Nakao YM, Kobayashi T, Watanabe T, Okamura T, Okayama A, Miyamoto Y. Interaction of blood pressure and body mass index with risk of incident atrial fibrillation in a Japanese Urban Cohort: the suita study. Am J Hypertens. 2015;28(11):1355–61.
Chyou JY, Hunter TD, Mollenkopf SA, Turakhia MP, Reynolds MR. Individual and combined risk factors for incident atrial fibrillation and incident stroke: an analysis of 3 million at-risk US patients. J Am Heart Assoc. 2015;4(7):e001723.
Kolek MJ, Graves AJ, Xu M, Bian A, Teixeira PL, Shoemaker MB, Parvez B, Xu H, Heckbert SR, Ellinor PT, Benjamin EJ, Alonso A, et al. Evaluation of a prediction model for the development of atrial fibrillation in a repository of electronic medical records. JAMA Cardiol. 2016;1(9):1007–13.
Svennberg E, Lindahl B, Berglund L, Eggers KM, Venge P, Zethelius B, Rosenqvist M, Lind L, Hijazi Z. NT-proBNP is a powerful predictor for incident atrial fibrillation—Validation of a multimarker approach. Int J Cardiol. 2016;15(223):74–81.
Hobbelt AH, Siland JE, Geelhoed B, Van der HP, Hillege HL, Van GI, Rienstra M. Clinical, biomarker, and genetic predictors of specific types of atrial fibrillation in a community-based cohort: data of the PREVEND study. Europace. 2017;19(2):226–32.
Ding L, Li J, Wang C, Li X, Su Q, Zhang G, Xue F. Incidence of atrial fibrillation and its risk prediction model based on a prospective urban Han Chinese cohort. J Hum Hypertens. 2017;31(9):574–9.
Ogunmoroti O, Michos ED, Aronis KN, Salami JA, Blankstein R, Virani SS, Spatz ES, Allen NB, Rana JS, Blumenthal RS, Veledar E, Szklo M, et al. Life’s simple 7 and the risk of atrial fibrillation: the multi-ethnic study of atherosclerosis. Atherosclerosis. 2018;275:174–81.
Austin TR, Wiggins KL, Blackshear C, Yang Y, Benjamin EJ, Curtis LH, Sotoodehnia N, Correa A, Heckbert SR. Atrial fibrillation in an African-American cohort: the Jackson heart study. Clin Cardiol. 2018;41(8):1049–54.
Aronson D, Shalev V, Katz R, Chodick G, Mutlak D. Risk score for prediction of 10-year atrial fibrillation: a community-based study. Thromb Haemost. 2018;118(9):1556–63.
Khurshid S, Choi SH, Weng LC, Wang EY, Trinquart L, Benjamin EJ, Ellinor PT, Lubitz SA. Frequency of cardiac rhythm abnormalities in a half million adults. Circ Arrhythm Electrophysiol. 2018;11(7):e006273.
Kim YG, Choi KJ, Han S, Hwang KW, Kwon CH, Park GM, Won KB, Ann SH, Kim J, Kim SJ, Lee SG, Nam GB, et al. Metabolic syndrome and the risk of new-onset atrial fibrillation in middle-aged East Asian men. Circ J. 2018;82(7):1763–9.
Kodani E, Kaneko T, Fujii H, Nakamura H, Sasabe H, Tamura Y, Shimizu W. Prevalence and incidence of atrial fibrillation in the general population based on national health insurance special health checkups- TAMA MED project-AF. Circ J. 2019;83(3):524–31.
Hamada R, Muto S. Simple risk model and score for predicting of incident atrial fibrillation in Japanese. J Cardiol. 2019;73(1):65–72.
Bose A, O’Neal WT, Wu C, McClure LA, Judd SE, Howard VJ, Howard G, Soliman EZ. Sex differences in risk factors for incident atrial fibrillation (from the reasons for geographic and racial differences in stroke [REGARDS] study). Am J Cardiol. 2019;123(9):1453–7.
Hulme OL, Khurshid S, Weng LC, Anderson CD, Wang EY, Ashburner JM, Ko D, McManus DD, Benjamin EJ, Ellinor PT, Trinquart L, Lubitz SA. Development and validation of a prediction model for atrial fibrillation using electronic health records. JACC Clin Electrophysiol. 2019;5(11):1331–41.
Feng T, Vegard M, Strand LB, Laugsand LE, Morkedal B, Aune D, Vatten L, Ellekjaer H, Loennechen JP, Mukamal K, Janszky I. Metabolically healthy obesity and risk for atrial fibrillation: the HUNT study. Obesity (Silver Spring). 2019;27(2):332–8.
Kim YG, Han KD, Choi JI, Yung BK, Kim DY, Oh SK, Lee KN, Shim J, Kim JS, Kim YH. Impact of the duration and degree of hypertension and body weight on new-onset atrial fibrillation: a nationwide population-based study. Hypertension. 2019;74(5):e45–51.
Rattani A, Claxton JS, Ali MK, Chen LY, Soliman EZ, Alvaro A. Association and impact of hypertension defined using the 2017 AHA/ACC guidelines on the risk of atrial fibrillation in The Atherosclerosis Risk in Communities study. BMC Cardiovasc Disord. 2019;19(1):262.
Koshiyama M, Tamaki K, Ohsawa M. Age-specific incidence rates of atrial fibrillation and risk factors for the future development of atrial fibrillation in the Japanese general population. J Cardiol 2020.
Abbas SS, Majeed T, Nair BR, Forder P, Weaver N, Byles J. Burden of atrial fibrillation and stroke risk among octagenarian and nonagenarian women in Australia. Ann Epidemiol. 2020;44:31–7.
O'Neal WT, Judd SE, Limdi NA, McIntyre WF, Kleindorfer DO, Cushman M, Howard VJ, Howard G, Soliman EZ. Differential Impact of Risk Factors in Blacks and Whites in the Development of Atrial Fibrillation: the Reasons for Geographic And Racial Differences in Stroke (REGARDS) Study. J Racial Ethn Health Disparities 2016.
Chao TF, Chiang CE, Chen TJ, Liao JN, Tuan TC, Chen SA. Clinical risk score for the prediction of incident atrial fibrillation: derivation in 7220654 Taiwan patients With 438930 Incident atrial fibrillations during a 16-year follow-up. J Am Heart Assoc. 2021;10(17):e020194.
Ninomiya Y, Kawasoe S, Kubozono T, Tokushige A, Ichiki H, Miyahara H, Tokushige K, Ohishi M. Sex-specific relationship between abdominal obesity and new-onset atrial fibrillation in the general Japanese population. Heart Vessels. 2021;36(12):1879–84.
Matsuoka S, Kaneko H, Okada A, Morita K, Itoh H, Michihata N, Jo T, Takeda N, Morita H, Fujiu K, Nakamura S, Node K, et al. Age modified relationship between modifiable risk factors and the risk of atrial fibrillation. Circ Arrhythm Electrophysiol. 2022;15(1):e010409.
Shapkina M, Ryabikov A, Mazdorova E, Titarenko A, Avdeeva E, Mazurenko E, Shcherbakova L, Pikhart H, Bobak M, Malyutina S. The determinants of the 13-year risk of incident atrial fibrillation in a Russian population cohort of middle and elderly age. J Pers Med. 2022;12(1):122.
Schnabel RB, Witt H, Walker J, Ludwig M, Geelhoed B, Kossack N, Schild M, Miller R, Kirchhof P. Machine learning-based identification of risk-factor signatures for undiagnosed atrial fibrillation in primary prevention and post-stroke in clinical practice. Eur Heart J Qual Care Clin Outcomes 2022.
Camen S, Csengeri D, Geelhoed B, Niiranen T, Gianfagna F, Vishram-Nielsen JK, Costanzo S, Søderberg S, Vartiainen E, Borschel CS, Donati MB, Lochen ML, et al. Risk factors, subsequent disease onset, and prognostic impact of myocardial infarction and atrial fibrillation. J Am Heart Assoc. 2022;11(7):e024299.
Minami M, Kobayashi Y, Toyokawa S, Inoue K, Takeshita Y. Risk factors for new-onset atrial fibrillation during routine medical checkups of Japanese male workers. Int Heart J. 2009;50(4):457–64.
Conen D, Tedrow UB, Koplan BA, Glynn RJ, Buring JE, Albert CM. Influence of systolic and diastolic blood pressure on the risk of incident atrial fibrillation in women. Circulation. 2009;119(16):2146–52.
Chamberlain AM, Agarwal SK, Folsom AR, Soliman EZ, Chambless LE, Crow R, Ambrose M, Alonso A. A clinical risk score for atrial fibrillation in a biracial prospective cohort (from the Atherosclerosis Risk in Communities [ARIC] study). Am J Cardiol. 2011;107(1):85–91.
Grundvold I, Skretteberg PT, Liestol K, Erikssen G, Kjeldsen SE, Arnesen H, Erikssen J, Bodegard J. Upper normal blood pressures predict incident atrial fibrillation in healthy middle-aged men: a 35-year follow-up study. Hypertension. 2012;59(2):198–204.
Roetker NS, Chen LY, Heckbert SR, Nazarian S, Soliman EZ, Bluemke DA, Lima JA, Alonso A. Relation of systolic, diastolic, and pulse pressures and aortic distensibility with atrial fibrillation (from the Multi-Ethnic Study of Atherosclerosis). Am J Cardiol. 2014;114(4):587–92.
Perkiomaki JS, Nortamo S, Ylitalo A, Kesaniemi A, Ukkola O, Huikuri HV. Ambulatory blood pressure characteristics and long-term risk for atrial fibrillation. Am J Hypertens. 2017;30(3):264–70.
Emdin CA, Anderson SG, Salimi-Khorshidi G, Woodward M, MacMahon S, Dwyer T, Rahimi K. Usual blood pressure, atrial fibrillation and vascular risk: evidence from 4.3 million adults. Int J Epidemiol. 2017;46(1):162–72.
Tikhonoff V, Kuznetsova T, Thijs L, Cauwenberghs N, Stolarz-Skrzypek K, Seidlerova J, Malyutina S, Gilis-Malinowska N, Swierblewska E, Kawecka-Jaszcz K, Filipovsky J, Narkiewicz K, et al. Ambulatory blood pressure and long-term risk for atrial fibrillation. Heart. 2018;104(15):1263–70.
Matsumoto K, Jin Z, Homma S, Elkind MSV, Schwartz JE, Rundek T, Mannina C, Ito K, Sacco RL, Di Tullio MR. Office, central and ambulatory blood pressure for predicting incident atrial fibrillation in older adults. J Hypertens. 2021;39(1):46–52.
Wong JA, Conen D, Healey JS, Johnson LSB. Modifiable risk factors predict incident atrial fibrillation and heart failure. Open Heart. 2020;7(1):e001092.
Espnes H, Ball J, Løchen ML, Wilsgaard T, Njølstad I, Mathiesen EB, Gerdts E, Sharashova E. Sex-Specific associations between blood pressure and risk of atrial fibrillation subtypes in the Tromsø study. J Clin Med. 2021;10(7):1514.
Liao LZ, Wen XY, Zhang SZ, Li WD, Zhuang XD. Hypertension and atrial fibrillation: a study on epidemiology and mendelian randomization causality. Front Cardiovasc Med. 2021;8:644405.
Lind L, Ingelsson M, Sundstrom J, Arnlov J. Impact of risk factors for major cardiovascular diseases: a comparison of life-time observational and Mendelian randomisation findings. Open Heart. 2021;8(2):e001735.
Hata J, Nagata T, Sakata S, Oishi E, Furuta Y, Hirakawa Y, Honda T, Yoshida D, Kitazono T, Ninomiya T. Risk prediction model for incident atrial fibrillation in a general Japanese population - The Hisayama study. Circ J. 2021;85(8):1373–82.
Son MK, Song DS, Lee K, Park HY. Lower number of modifiable risk factors was associated with reduced atrial fibrillation incidence in an 18-year prospective cohort study. Sci Rep. 2022;12(1):9207.
Mitchell GF, Vasan RS, Keyes MJ, Parise H, Wang TJ, Larson MG, D’Agostino RB Sr, Kannel WB, Levy D, Benjamin EJ. Pulse pressure and risk of new-onset atrial fibrillation. JAMA. 2007;297(7):709–15.
Igarashi Y, Nochioka K, Sakata Y, Tamai T, Ohkouchi S, Irokawa T, Ogawa H, Hayashi H, Fujihashi T, Yamanaka S, Shiroto T, Miyata S, et al. Risk prediction for new-onset atrial fibrillation using the Minnesota code electrocardiography classification system. Int J Cardiol Heart Vasc. 2021;34:100762.
Forman JP, Stampfer MJ, Curhan GC. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA. 2009;302(4):401–11.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–13.
Kobeissi E, Hibino M, Pan H, Aune D. Blood pressure, hypertension and the risk of abdominal aortic aneurysms: a systematic review and meta-analysis of cohort studies. Eur J Epidemiol. 2019;34(6):547–55.
Pan H, Hibino M, Kobeissi E, Aune D. Blood pressure, hypertension and the risk of sudden cardiac death: a systematic review and meta-analysis of cohort studies. Eur J Epidemiol. 2020;35(5):443–54.
Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. 1992;135(11):1301–9.
Royston P. A strategy for modelling the effect of a continuous covariate in medicine and epidemiology. Stat Med. 2000;19(14):1831–47.
Bagnardi V, Zambon A, Quatto P, Corrao G. Flexible meta-regression functions for modeling aggregate dose-response data, with an application to alcohol and mortality. Am J Epidemiol. 2004;159(11):1077–86.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Wells G, Shea B, O'Connell D., Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. https://www.ohri.ca//programs/clinical_epidemiology/oxford.asp, Accessed 20 May 2022.
Egger M, Davey SG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Nazarzadeh M, Pinho-Gomes AC, Bidel Z, Canoy D, Dehghan A, Smith BK, Bennett DA, Smith GD, Rahimi K. Genetic susceptibility, elevated blood pressure, and risk of atrial fibrillation: a Mendelian randomization study. Genome Med. 2021;13(1):38.
Georgiopoulos G, Ntritsos G, Stamatelopoulos K, Tsioufis C, Aimo A, Masi S, Evangelou E. The relationship between blood pressure and risk of atrial fibrillation: a Mendelian randomization study. Eur J Prev Cardiol 2021.
Hyman MC, Levin MG, Gill D, Walker VM, Georgakis MK, Davies NM, Marchlinski FE, Damrauer SM. Genetically predicted blood pressure and risk of atrial fibrillation. Hypertension. 2021;77(2):376–82.
Verdecchia P, Staessen JA, Angeli F, De SG, Achilli A, Ganau A, Mureddu G, Pede S, Maggioni AP, Lucci D, Reboldi G. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): an open-label randomised trial. Lancet. 2009;374(9689):525–33.
Wei YC, George NI, Chang CW, Hicks KA. Assessing sex differences in the risk of cardiovascular disease and mortality per increment in systolic blood pressure: a systematic review and meta-analysis of follow-up studies in the United States. PLoS ONE. 2017;12(1):e0170218.
Peters SA, Huxley RR, Woodward M. Comparison of the sex-specific associations between systolic blood pressure and the risk of cardiovascular disease: a systematic review and meta-analysis of 124 cohort studies, including 1.2 million individuals. Stroke. 2013;44(9):2394–401.
Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, White IR, Caulfield MJ, Deanfield JE, Smeeth L, Williams B, Hingorani A, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014;383(9932):1899–911.
Gumprecht J, Domek M, Lip GYH, Shantsila A. Invited review: hypertension and atrial fibrillation: epidemiology, pathophysiology, and implications for management. J Hum Hypertens. 2019;33(12):824–36.
McNiece KL, Gupta-Malhotra M, Samuels J, Bell C, Garcia K, Poffenbarger T, Sorof JM, Portman RJ. Left ventricular hypertrophy in hypertensive adolescents: analysis of risk by 2004 National high blood pressure education program working group staging criteria. Hypertension. 2007;50(2):392–5.
Soliman EZ, Byington RP, Bigger JT, Evans G, Okin PM, Goff DC Jr, Chen H. Effect of intensive blood pressure lowering on left ventricular hypertrophy in patients with diabetes mellitus: action to control cardiovascular risk in diabetes blood pressure trial. Hypertension. 2015;66(6):1123–9.
Mosterd A, D’Agostino RB, Silbershatz H, Sytkowski PA, Kannel WB, Grobbee DE, Levy D. Trends in the prevalence of hypertension, antihypertensive therapy, and left ventricular hypertrophy from 1950 to 1989. N Engl J Med. 1999;340(16):1221–7.
Cao X, Broughton ST, Waits GS, Nguyen T, Li Y, Soliman EZ. Interrelations between hypertension and electrocardiographic left ventricular hypertrophy and their associations with cardiovascular mortality. Am J Cardiol. 2019;123(2):274–83.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet 2017; 389(10064):37–55.
Acknowledgements
DA designed the research, conducted the literature search and analyses and wrote the first draft of the manuscript. DA, YMS, EK, and TF did the literature screening. All authors interpreted the data, revised the subsequent drafts for important intellectual content, read and approved the final manuscript. This work has been supported by funding from the South-East Regional Health Authority of Norway (DA), Norwegian Heart and Lung Association (TF), and Liaison Committee for Education, Research and Innovation in Central Norway (TF). The authors declare that there is no duality of interest associated with this manuscript. D. Aune takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have not disclosed any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aune, D., Mahamat-Saleh, Y., Kobeissi, E. et al. Blood pressure, hypertension and the risk of atrial fibrillation: a systematic review and meta-analysis of cohort studies. Eur J Epidemiol 38, 145–178 (2023). https://doi.org/10.1007/s10654-022-00914-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-022-00914-0