Abstract
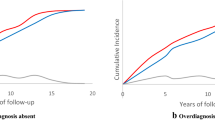
After the introduction of the prostate specific antigen (PSA) test in the 1980s, a sharp increase in the incidence rate of prostate cancer was seen in the United States. The age-specific incidence patterns exhibited remarkable shifts to younger ages, and declining rates were observed at old ages. Similar trends were seen in Norway. We investigate whether these features could, in combination with PSA testing, be explained by a varying degree of susceptibility to prostate cancer in the populations. We analyzed incidence data from the United States’ Surveillance, Epidemiology, and End Results program for 1973–2010, comprising 511,027 prostate cancers in men ≥40 years old, and Norwegian national incidence data for 1953–2011, comprising 113,837 prostate cancers in men ≥50 years old. We developed a frailty model where only a proportion of the population could develop prostate cancer, and where the increased risk of diagnosis due to the massive use of PSA testing was modelled by encompassing this heterogeneity in risk. The frailty model fits the observed data well, and captures the changing age-specific incidence patterns across birth cohorts. The susceptible proportion of men is \(39.9\,\%\,\left( {95\,\%\,{\text{CI}}\, 38.2, 41.6\,\% } \right)\) in the United States and \(30.4\,\%\, \left( {95\,\%\, {\text{CI}} \,28.9, 32.0\,\% } \right)\) in Norway. Cumulative incidence rates at old age are unchanged across birth cohort exposed to PSA testing at younger and younger ages. The peaking cohort-specific age-incidence curves of prostate cancer may be explained by the underlying heterogeneity in prostate cancer risk. The introduction of the PSA test has led to a larger number of diagnosed men. However, no more cases are being diagnosed in total in birth cohorts exposed to the PSA era at younger and younger ages, even though they are diagnosed at younger ages. Together with the earlier peak in the age-incidence curves for younger cohorts, and the strong familial association of the cancer, this constitutes convincing evidence that the PSA test has led to a higher proportion, and an earlier timing, of diagnoses in a limited pool of susceptible individuals.






Similar content being viewed by others
References
Mucci LA, Signorello LB, Adami H-O. Prostate Cancer. In: Adami H-O, Hunter D, Trichopoulos D, editors. Textbook of cancer epidemiology. Oxford: Oxford University Press Inc.; 2008. p. 517–54.
Hsing AW, Devesa SS. Trends and patterns of prostate cancer: What do they suggest? Epidemiol Rev. 2001;23(1):3–13.
Cancer in Norway 2013 - Cancer incidence, mortality, survival and prevalence in Norway. Oslo: Cancer Registry of Norway; 2015.
Aalen OO, Valberg M, Grotmol T, Tretli S. Understanding variation in disease risk: the elusive concept of frailty. Int J Epidemiol. 2014. doi:10.1093/ije/dyu192.
Aalen OO, Borgan Ø, Gjessing HK. Survival and event history analysis: a process point of view. New York: Springer; 2008.
Duchateau L, Janssen P. The frailty model. New York: Springer; 2008.
Wienke A. Frailty models in survival analysis. Boca Raton: Chapman and Hall/CRC; 2011.
Aalen OO, Tretli S. Analyzing incidence of testis cancer by means of a frailty model. Cancer Causes Control. 1999;10(4):285–92.
Svensson E, Moger TA, Tretli S, Aalen OO, Grotmol T. Frailty modelling of colorectal cancer incidence in Norway: indications that individual heterogeneity in risk is related to birth cohort. Eur J Epidemiol. 2006;21(8):587–93. doi:10.1007/s10654-006-9043-8.
Valberg M, Grotmol T, Tretli S, Veierød MB, Devesa SS, Aalen OO. Frailty modeling of age-incidence curves of osteosarcoma and Ewing sarcoma among individuals younger than 40 years. Stat Med. 2012;31(28):3731–47.
Haugen M, Bray F, Grotmol T, Tretli S, Aalen OO, Moger TA. Frailty modeling of bimodal age-incidence curves of nasopharyngeal carcinoma in low-risk populations. Biostatistics. 2009;10(3):501–14. doi:10.1093/biostatistics/kxp007.
Grotmol T, Bray F, Holte H, Haugen M, Kunz L, Tretli S, et al. Frailty modeling of the bimodal age-incidence of Hodgkin lymphoma in the Nordic countries. Cancer Epidemiol Biomark Prev. 2011;20(7):1350–7. doi:10.1158/1055-9965.epi-10-1014.
Il’yasova D, Siamakpour-Reihani S, Akushevich I, Akushevich L, Spector N, Schildkraut J. What can we learn from the age- and race/ethnicity- specific rates of inflammatory breast carcinoma? Breast Cancer Res Treat. 2011;130(2):691–7.
Kravchenko J, Akushevich I, Seewaldt V, Abernethy A, Lyerly HK. Breast cancer as heterogeneous disease: contributing factors and carcinogenesis mechanisms. Breast Cancer Res Treat. 2011;128(2):483–93. doi:10.1007/s10549-011-1347-z.
Soto-Ortiz L, Brody JP. Similarities in the age-specific incidence of colon and testicular cancers. PLoS One. 2013;8(6):e66694. doi:10.1371/journal.pone.0066694.
Campisi J, Andersen JK, Kapahi P, Melov S. Cellular senescence: a link between cancer and age-related degenerative disease? Semin Cancer Biol. 2011;21(6):354–9. doi:10.1016/j.semcancer.2011.09.001.
Kong Y, Cui H, Ramkumar C, Zhang H. Regulation of senescence in cancer and aging. J Aging Res. 2011;2011:15. doi:10.4061/2011/963172.
Soto-Ortiz LF, Brody JP. Lifetime-independent risk of a second primary cancer in artificial populations subjected to frailty and cell senescence effects. Adv Stud Biol. 2015;7(4):179–202. doi:10.12988/asb.2015.514.
SEER 9 Regs Research Data, Nov 2012 Sub (1973–2010) (Katrina/Rita Population Adjustment)—Linked to county attributes—Total US, 1969–2011 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, released April 2013, based on the November 2012 submission.
Bray F, Parkin DM. Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer. 2009;45(5):747–55. doi:10.1016/j.ejca.2008.11.032.
Parkin DM, Bray F. Evaluation of data quality in the cancer registry: principles and methods Part II Completeness. Eur J Cancer. 2009;45(5):756–64. doi:10.1016/j.ejca.2008.11.033.
Larsen IK, Småstuen M, Johannesen TB, Langmark F, Parkin DM, Bray F, et al. Data quality at the Cancer Registry of Norway: an overview of comparability, completeness, validity and timeliness. Eur J Cancer. 2009;45(7):1218–31. doi:10.1016/j.ejca.2008.10.037.
Welch HG, Albertsen PC. Prostate cancer diagnosis and treatment after the introduction of prostate-specific antigen screening: 1986–2005. J Natl Cancer Inst. 2009;101(19):1325–9. doi:10.1093/jnci/djp278.
Fosså SD, Eri LM, Skovlund E, Tveter K, Vatten L. No randomised trial of prostate cancer screening in Norway. Lancet Oncol. 2001;2(12):741–5. doi:10.1016/S1470-2045(01)00588-5.
Fosså SD, Høisæter PÅ. Screening for prostate cancer in Norway. Nor J Epidemiol. 2001;11(2):147–52.
Legler J, Feuer E, Potosky A, Merrill R, Kramer B. The role of prostate-specific antigen (PSA) testing patterns in the recent prostate cancer incidence declinein the United States. Cancer Causes Control. 1998;9(5):519–27. doi:10.1023/A:1008805718310.
Howard DH, Tangka FK, Guy GP, Ekwueme DU, Lipscomb J. Prostate cancer screening in men ages 75 and older fell by 8 percentage points after Task Force recommendation. Health Aff (Millwood). 2013;32(3):596–602.
Sirovich BE, Schwartz LM, Woloshin S. Screening men for prostate and colorectal cancer in the United States: does practice reflect the evidence? JAMA. 2003;289(11):1414–20.
Drazer MW, Huo D, Schonberg MA, Razmaria A, Eggener SE. Population-based patterns and predictors of prostate-specific antigen screening among older men in the United States. J Clin Oncol. 2011;29(13):1736–43.
Armitage P, Doll R. The age distribution of cancer and a multi-stage theory of carcinogenesis. Br J Cancer. 1954;8:1–12. doi:10.1038/bjc.1954.1.
Potosky AL, Kessier L, Gridley G, Brown CC, Horm JW. Rise in prostatic cancer incidence associated with increased use of transurethral resection. J Natl Cancer Inst. 1990;82(20):1624–8. doi:10.1093/jnci/82.20.1624.
Kvåle R, Auvinen A, Adami H-O, Klint Å, Hernes E, Møller B, et al. Interpreting trends in prostate cancer incidence and mortality in the five nordic countries. J Natl Cancer Inst. 2007;99(24):1881–7. doi:10.1093/jnci/djm249.
Wolf A, Wender RC, Etzioni RB, Thompson IM, D’Amico AV, Volk RJ, et al. American Cancer Society guideline for the early detection of prostate cancer: update 2010. CA Cancer J Clin. 2010;60(2):70–98.
Smith RA, Cokkinides V, Brooks D, Saslow D, Shah M, Brawley OW. Cancer screening in the United States, 2011. CA Cancer J Clin. 2011;61(1):8–30. doi:10.3322/caac.20096.
Doll R. Cancer incidence in five continents: A Technical Report. Berlin, Germany: Springer-Verlag (for UICC); 1966.
Eeles R, Goh C, Castro E, Bancroft E, Guy M, Olama AAA, et al. The genetic epidemiology of prostate cancer and its clinical implications. Nat Rev Urol. 2014;11(1):18–31. doi:10.1038/nrurol.2013.266.
Hemminki K. Familial risk and familial survival in prostate cancer. World J Urol. 2012;30(2):143–8. doi:10.1007/s00345-011-0801-1.
Aly M, Wiklund F, Grönberg H. Early detection of prostate cancer with emphasis on genetic markers. Acta Oncol. 2011;50(sup1):18–23. doi:10.3109/0284186X.2010.529824.
Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst. 2010;102(9):605–13. doi:10.1093/jnci/djq099.
Jahn JL, Giovannucci EL, Stampfer MJ. The high prevalence of undiagnosed prostate cancer at autopsy: implications for epidemiology and treatment of prostate cancer in the Prostate-specific Antigen-era. Int J Cancer. 2015;137(12):2795–802. doi:10.1002/ijc.29408.
Zhou CK, Check DP, Lortet-Tieulent J, Laversanne M, Jemal A, Ferlay J, et al. Prostate cancer incidence in 43 populations worldwide: an analysis of time trends overall and by age group. Int J Cancer. 2016;138(6):1388–400.
Bray F, Kohler B, Ferlay J. Data comparability and quality. In: Forman D, Bray F, Brewster DH, GombeMbalawa C, Kohler B, Piñeros M, et al., editors. Cancer incidence in five continents, vol. 10. Lyon: International Agency for Research on Cancer; 2013. p. 89–106.
Jemal A, Fedewa SA, Ma J, Siegel R, Lin CC, Brawley O, et al. Prostate cancer incidence and PSA testing patterns in relation to USPSTF screening recommendations. JAMA. 2015;314(19):2054–61. doi:10.1001/jama.2015.14905.
Etzioni R, Berry KM, Legler JM, Shaw P. Prostate-specific antigen testing in black and white men: an analysis of medicare claims from 1991–1998. Urology. 2002;59(2):251–5. doi:10.1016/S0090-4295(01)01516-3.
Hoffman RM, Couper MP, Zikmund-Fisher BJ, Levin CA, McNaughton-Collins M, Helitzer DL, et al. Prostate cancer screening decisions: results from the national survey of medical decisions (decisions study). Arch Intern Med. 2009;169(17):1611–8. doi:10.1001/archinternmed.2009.262.
Skovlund E, Fosså SD. PSA analyses in three Norwegian counties in 1999. Tidsskr Nor Laegeforen. 2000;120:2539–41.
NORDCAN: Cancer incidence, mortality, prevalence and survival in the nordic countries, version 7.1 (09.07.2015) (database on the Internet). Association of the Nordic Cancer Registries. http://www.ancr.nu/. Accessed: 9 Sept 2015.
Funding
This work was supported by the Norwegian Cancer Society, Grant Number 4493570.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Valberg, M., Grotmol, T., Tretli, S. et al. Prostate-specific antigen testing for prostate cancer: Depleting a limited pool of susceptible individuals?. Eur J Epidemiol 32, 511–520 (2017). https://doi.org/10.1007/s10654-016-0185-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-016-0185-z