Abstract
Purpose. Lisavanbulin (BAL101553) is the prodrug of avanbulin (BAL27862), a microtubule-destabilizing agent. The goal of this study (NCT02895360) was to characterize the safety, tolerability and antitumor activity of lisavanbulin administered as a 48-hour intravenous (IV) infusion at the recommended Phase 2 dose (RP2D) of 70 mg/m2. Results from the Phase 1 dose-escalation portion of the study identifying the RP2D have been previously reported. Here, we present the findings from the Phase 2a portion of this study. Methods. This multi-center, open-label study included patients with ovarian, fallopian-tube, or primary peritoneal cancer that was either platinum-resistant or refractory (11 patients), or with first recurrence of glioblastoma (12 patients). Lisavanbulin was administered as a 48-hour IV infusion on Days 1, 8, and 15 of a 28-day cycle. Results. Lisavanbulin was well tolerated in both patient cohorts. Thirteen patients (56.5%) developed 49 adverse events assessed as related to study treatment. The majority were mild or moderate; four were grade 3/4. Sixteen SAEs were reported in nine patients (39.1%), with none considered related to study treatment. No AEs led to permanent treatment discontinuation. Three patients in the ovarian cancer cohort had stable disease with lesion size reductions after two cycles of treatment; in the glioblastoma cohort, one patient showed partial response with a > 90% glioblastoma area reduction as best response, and one patient had stable disease after eight cycles of treatment. Conclusion. This study demonstrated a favorable safety and tolerability profile of 48-hour continuous IV infusion of lisavanbulin in patients with solid extracranial tumors or glioblastoma. Clinicaltrials.gov registration: NCT02895360.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Microtubule-targeting agents (MTAs) are among the most effective cytotoxic chemotherapy agents, and affect microtubule dynamics either as microtubule-destabilizers (such as the vinca-alkaloids) or microtubule stabilizers (such as the taxanes and azaepothilone B) [1]. Despite the initial sensitivity of many tumors to tubulin-targeting therapy, the development of primary or acquired resistance remains a major challenge [2, 3]. There is a need for novel microtubule-inhibitory agents that can overcome these resistance mechanisms and improve treatment outcomes.
Lisavanbulin (BAL101553; PubChem CID: 45,259,014) is the water-soluble lysine pro-drug of avanbulin (BAL27862; PubChem CID: 11,176,685) [4, 5]. Avanbulin is a potent inhibitor of tumor cell growth due to its ability to bind to tubulin heterodimers at the colchicine-binding site, thereby inhibiting microtubule assembly and resulting in activation of the spindle assembly checkpoint, an event required for anti-tumor activity [5, 6]. The mechanism of action of lisavanbulin extends beyond its ability to target tumor cell proliferation, also affecting the tumor microenvironment by reducing tumor microvasculature [7, 8].
Avanbulin showed activity in a number of in vitro and in vivo tumor models resistant to other microtubule-targeting agents [9,10,11,12]. One clinical study has been completed (CDI-CS-001), investigating lisavanbulin administered as a 2-hour infusion in patients with solid tumors who had failed standard anti-cancer therapy, or for whom no effective standard therapy was available. The recommended Phase 2 dose (RP2D) of 30 mg/m2 in that study was well-tolerated and showed encouraging anti-tumor activity [13]. The observed dose-limiting toxicities were related to lisavanbulin’s effects on the vascular system, which occurred at peak serum concentrations (Cmax) [13]. Conversely, the anti-proliferative effects of lisavanbulin were directly correlated to drug exposure (AUC) [4], suggesting that longer exposure at lower doses would result in maximal efficacy.
Study CDI-CS-003, a single-agent, open-label, Phase 1/2a study performed in two parts, aimed to reconcile these aspects of lisavanbulin’s pharmacokinetics through the use of an extended 48-hour IV infusion to maximize exposure while minimizing vascular toxicity. Part 1 of the study (previously reported) was a Phase 1 dose-escalation portion to determine the maximum tolerated dose (MTD) in patients with advanced/recurrent solid tumors [14] and to assess oral bioavailability. No DLTs were reported at the 30 mg/m2 or 45 mg/m2 doses. One DLT (grade 3 hypotension) was observed at the 70 mg/m2 dose [14]. Results from Part 1 of the study indicated that lisavanbulin was well tolerated at doses up to 70 mg/m2, and that the MTD (RP2D) for the 48-hour infusion was 70 mg/m2. When administered as a continuous 48 h infusion, higher exposures of the active metabolite avanbulin were achieved (compared to a 2-hour infusion at the RP2D), without significant vascular toxicity [14].
The work reported here is from Part 2 of study CDI-CS-003, a Phase 2a expansion portion to further characterize the safety and tolerability of lisavanbulin at the MTD of 70 mg/m2, performed in two parallel cohorts of patients with platinum-resistant/refractory ovarian, fallopian tube, or primary peritoneal cancer or glioblastoma at first recurrence. The selection of patients with ovarian cancer was supported by a complete response seen in a patient with ovarian cancer in Phase 1, the activity of avanbulin in taxane- and vinca-alkaloid-resistant ovarian cancer cell and xenograft models [10, 11], and the utility of microtubule-targeting drugs in this indication.
Patients with glioblastoma were not included in Phase 1, but daily oral administration of lisavanbulin was already under investigation as a monotherapy in patients with recurrent glioblastoma in study CDI-CS-002 (NCT02490800 [15]), and in combination with radiotherapy in patients with newly diagnosed glioblastoma in study CDI-CS-004 (NCT03250299). Lisavanbulin demonstrated excellent brain penetration and significant extension of survival alone or in combination with radiotherapy using a panel of glioblastoma patient-derived xenografts [16].
Methods
Study design
This was an open-label, multi-center Phase 1/2a study (NCT02895360) conducted between August 2016 and August 2020; results from the completed Phase 2a portion of the study are reported here. The Independent Ethics Committees of the six study sites, and relevant authorities in Switzerland, approved the study protocol. All patients provided written informed consent prior to study participation.
Objectives
The objectives of the Phase 2a portion of the study were to evaluate the safety, tolerability, and anti-tumor activity of lisavanbulin when administered as a 48-hour infusion at the RP2D in two patient populations of special interest.
Patients
The study population comprised adult patients (≥ 18 years) with either histologically-confirmed ovarian, fallopian-tube, or primary peritoneal cancer that was platinum-resistant or refractory (the ‘ovarian cancer cohort’), or with histologically-confirmed glioblastoma at first recurrence (the ‘glioblastoma cohort’). Key inclusion criteria were life expectancy ≥ 12 weeks, acceptable organ and marrow function within 15 days prior to starting study drug, Eastern Cooperative Oncology Group (ECOG) performance status ≤ 1 (the ovarian cancer cohort) or ≤ 2 (the glioblastoma cohort), and at least one site of measurable disease as defined by RECIST version 1.1 (ovarian cancer) or RANO criteria (glioblastoma). Glioblastoma patients who were being treated with steroids had to be on a stable or decreasing dose. Patients were excluded if they had received chemotherapy, radiotherapy, immunotherapy, or any investigational agents within 4 weeks (6 weeks for nitrosoureas or mitomycin C, 12 weeks for radiotherapy of glioblastoma) prior to receiving the study drug. Other exclusion criteria were the presence of peripheral neuropathy ≥ CTCAE grade 2, systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg, and combination treatment with more than two anti-hypertensive medications. Patients with significant cardiac disease or abnormalities, and those with a history of cerebral hemorrhage, cerebral aneurysm, ischemic stroke, or a history of transient ischemic attack within 24 months prior to screening, were also excluded.
Study treatment
All patients received lisavanbulin administered as a 48-hour IV infusion at 70 mg/m2 on Days 1, 8, and 15 of a 28-day treatment cycle, administered via an elastomeric pump (Baxter pump models 2C4711K or 2C1009KP/2C4009K) using an implantable venous access system. All patients were scheduled to receive two treatment cycles. Those with objective response or stable disease were permitted to continue additional treatment cycles beyond cycle 2, until the occurrence of progressive disease or unacceptable toxicity, or until other discontinuation criteria were met.
Efficacy assessments
Tumor assessments by radiological examination (computed tomography / magnetic resonance imaging scans) and cancer antigen 125 monitoring (in ovarian cancer patients) were performed at screening and end of study, and within the 7 days prior to completion of every even-numbered cycle, before administration of the next cycle of lisavanbulin. Tumor response was evaluated according to RECIST v1.1 (ovarian cancer) or RANO criteria (glioblastoma). Complete response or partial response had to be present for at least 4 weeks to be assessed as confirmed. Each lesion measured at baseline was to be measured throughout the study by the same method of assessment and the same technique, to facilitate consistent assessments and comparisons. Tumor growth was expressed as the change from baseline in the sum/products of the perpendicular diameters for either the target lesion or all measurable enhancing lesions.
Safety assessments
Safety and tolerability assessments included the recording of adverse events (AEs; evaluated according to CTCAE version 4.03), serious adverse events (SAEs), physical examinations, vital signs measurements, 12-lead electrocardiogram (ECG) assessments including heart rate, and PR, QRS, and QT intervals, clinical laboratory parameters, pregnancy testing, and ECOG performance status. Transthoracic echocardiography was performed at screening and at the end of the study. Concomitant medications were monitored throughout.
Statistical analysis
All patients who received at least one partial or complete dose of study drug were included in the full analysis population (FAP), and all of these patients who had at least one post-baseline safety assessment were included in the safety population. Separate efficacy-evaluable populations (EEPs) were defined for both cohorts. The EEPs were (1) all patients with progressive disease who had completed at least cycle 1 and who had at least one on-study tumor assessment or radiological assessment, and (2) patients with stable disease, partial response, or complete response at the end of cycle 2, who had received at least four doses of study drug in the first two cycles. The objective response rate was the proportion of patients responding, i.e., with a best observed objective response of complete or partial response. The disease control rate was the proportion of patients with controlled disease (complete or partial response or stable disease) after two and four treatment cycles, and at the end of treatment. Progression-free survival (PFS) was defined as the interval between the date of first infusion and the earliest date of objective disease progression, investigator-confirmed clinical progression, or death due to any cause. Percentages and 95% confidence intervals (CIs) were calculated. Background, demographic and safety data were analyzed using descriptive statistics or contingency tables. Safety assessments included the frequency of AEs and laboratory abnormalities in the safety population. Statistical analyses were performed using SAS® Version 9.3 or higher (SAS Institute, Cary, North Carolina, USA).
Results
Patient demographics and medical history
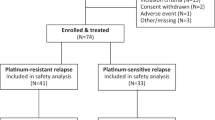
Twenty-three patients were enrolled at six study sites in Switzerland. There were 11 patients in the ovarian cancer cohort and 12 in the glioblastoma cohort, of whom eight (72.7%) and eight (66.7%), respectively, were included in the EEP. Nine patients in each cohort (81.8% and 75%, respectively) completed the follow-up period. The mean age of the FAP was 61.9 years, and all patients were Caucasian. A summary of the diagnosis and extent of cancer at screening for the FAP is shown in Table 1.
The mean (± SD) extent of exposure to lisavanbulin in the safety population was 84.1 (± 119.1) days. The mean exposure was similar in both cohorts (81.6 days vs. 86.5 days in the ovarian cancer and glioblastoma cohorts, respectively).
Six patients with ovarian cancer and one patient with glioblastoma had at least one dose adjustment. The mean (± SD) overall treatment compliance in the safety population was 98.3% (± 4.6), range 80.3–102.9%. This was similar across both cohorts (98.7% and 97.9% in the ovarian cancer and glioblastoma cohorts, respectively).
Tolerability and safety
Most patients (22/23 [95.7%]) reported at least one treatment-emergent AE. The most frequently-reported AEs were fatigue (10/23 patients, 43.5%), constipation (8/23, 34.8%), decreased appetite (7/23, 30.4%), and abdominal pain (6/23, 26.1%) (see Online Resource 2). One AE led to a dose reduction, but none led to treatment discontinuation. There were 16 SAEs reported by nine patients (39.1%), none of which were considered related to study treatment. No grade 5 toxicity occurred. Related AEs reported for patients in Phase 2a and in those treated at 70 mg/m2 in Phase 1 are summarized in Table 2. Apart from reported AEs, there were no significant changes or trends over time, in laboratory assessments, vital signs, ECG results, or echocardiographic assessments.
Efficacy
In the glioblastoma cohort, one patient had a confirmed partial response with a steady decrease in target lesion size to less than 10% over a treatment period of 16 cycles (see Online Resource 1). Another patient with stable disease as best response was treated for 10 cycles, corresponding to a disease control rate of 2/8 (25%) after eight cycles of treatment, and an objective response rate of 1/8 (12.5%) in the EEP of this cohort. In the ovarian cancer cohort, the best response was stable disease in three patients, corresponding to disease control rates of 3/8 (37.5%) after two cycles of treatment in the EEP. After four cycles, the disease control rate was 1/8 (12.5%) in the EEP. Reduction in the size of target lesions was observed in four patients with ovarian cancer and in three patients with glioblastoma.
All study patients experienced disease progression. The six-month PFS rates in the ovarian cancer and glioblastoma cohorts were 9.1% and 16.7%, respectively. Kaplan-Meier curves for PFS are shown in Fig. 1. The median time to disease progression was similar in both cohorts (54.0 and 49.0 days for the ovarian cancer and glioblastoma cohorts, respectively). In the overall EEP, the six-month PFS rates were 12.5% and 25%, with median times to death or disease progression of 55.5 and 51.5 days in the ovarian cancer and glioblastoma cohorts, respectively.
Discussion
Lisavanbulin is a water-soluble lysine prodrug of the active synthetic small molecule avanbulin, which can be administered intravenously in the absence of solubilizing excipients, and has high oral bioavailability. Study CDI-CS-001 showed that the RP2D of 30 mg/m2 was well-tolerated and had encouraging anti-tumor activity [13]. However, the observed dose-limiting toxicities of lisavanbulin were related to its effects on the vascular system, which occurred at peak serum concentrations (Cmax), whereas its anti-proliferative effects were related to drug exposure (AUC) [13]. The goal of this study was therefore to test the safety, tolerability, and anti-tumor efficacy of lisavanbulin using a 48-hour IV infusion.
When administered as a 48-hour IV infusion, the RP2D was determined to be 70 mg/m2 in the Phase 1 portion of this study [14]. Administration of lisavanbulin in this manner resulted in a higher dose intensity and higher cumulative exposure to the active moiety avanbulin, while mitigating the vascular toxicity observed with the 2-hour infusion [14]. The corresponding mean Cmax values were lower with the 48-hour infusion (144 vs. 267 ng/mL for the 2-hour infusion), resulting in a four-fold higher AUC/Cmax ratio (60 vs. 14, respectively) [14]. In the Phase 1 portion of the study, dose-limiting toxicities comprised grade 3 hypotension in one patient treated at 70 mg/m2, grade 3 hyponatremia in one patient at 90 mg/m2, and grade 2 hallucination, ataxia, and dysarthria with grade 3 neutropenia in another patient treated at 90 mg/m2 [14]. The only corresponding event of the same grade during the Phase 2a portion of the study was a case of grade 2 hallucination leading to dose reduction in a patient with ovarian cancer. Grade 3/4 events were reported in three patients with ovarian cancer and in one with glioblastoma. Two patients experienced grade 3 hypertension; one patient with pre-existing hypertension had self-limiting grade 3 episodes in cycle 1; another patient with hypertension borderline to grade 2 at baseline required initiation of antihypertensive medication in cycle 12. The interpretation of one event of grade 4 decrease in lymphocyte counts requires some caution, as it only occurred 12 days after the last infusion had ended; such events were rarely observed with lisavanbulin, and when seen were of low grades. The case of grade 3 increase in aspartate aminotransferase would be classified as grade 1 per CTCAE version 5.0 due to elevated baseline values. Overall, the safety profile of lisavanbulin appears consistent in patients with solid tumors, ovarian cancer, and glioblastoma treated at the RP2D. When comparing the percentage of patients affected by related AEs (89%, 81%, and 33%; Table 2), the tolerance to lisavanbulin appears to slightly favor patients with glioblastoma. Treatment compliance was high in both Phase 2a cohorts. Compared with study CDI-CS-001, the percentages of patients affected by related adverse events appear similar across system organ classes at RP2D levels (CDI-CS-001: 30 mg/m2, CDI-CS-003: 70 mg/m2) but for gastrointestinal, nervous system, and vascular disorders, these percentages were significantly lower than those observed in study CDI-CS-001 at dose levels of 45–80 mg/m2 (see Online Resource 3).
Signals of efficacy were observed following treatment with lisavanbulin as a 48-hour IV infusion. In the ovarian cancer cohort, three patients had best response of stable disease, with lesion size reductions after two cycles of treatment (EEP). In the glioblastoma cohort, one patient with partial response was treated for 16 cycles, and one patient with stable disease as best response was treated for 10 cycles, corresponding to a disease control rate of 25% after eight cycles of treatment, and an objective response rate of 12.5% in the EEP.
In a Phase 1 study with continuous daily oral administration of lisavanbulin, two of 28 patients with recurrent or progressive glioblastoma or high-grade glioma achieved long-lasting objective responses (CDI-CS-002, NCT02490800 [15]). Notably, the tumor tissues of both patients showed strong end-binding protein 1 (EB1) expression as assessed by immunohistochemistry staining. This observation is supported by earlier data in orthotopic glioblastoma mouse models suggesting that EB1 expression could be a response-predictive biomarker of lisavanbulin in glioblastoma [17, 18]. The rather low prevalence of high EB1 expression seen in archival tissue samples of various tumor types [19] could explain heterogeneous responses seen with lisavanbulin when used in unselected patient populations. The Phase 2a portion of study CDI-CS-002 was therefore designed to determine the objective response rate of daily oral administration of lisavanbulin (25 mg per day) in patients whose glioblastoma tissue had high EB1 expression [20]. While oral administration has obvious advantages, data generated in this study support the safe use of lisavanbulin as a 48-hour continuous infusion, which may gain additional significance if response-predictive biomarkers of lisavanbulin show high prevalence in pediatric indications.
Conclusion
This study demonstrated that a 48-hour continuous IV infusion of lisavanbulin had a better tolerability profile than the 2-hour infusion. The favorable safety profile was confirmed for patients with solid tumors, including glioblastoma.
References
Čermák V, Dostál V, Jelínek M et al (2020) Microtubule-targeting agents and their impact on cancer treatment. Eur J Cell Biol 99. https://doi.org/10.1016/j.ejcb.2020.151075
Das T, Anand U, Pandey SK et al (2021) Therapeutic strategies to overcome taxane resistance in cancer. Drug Resist Updates 55:100754. https://doi.org/10.1016/J.DRUP.2021.100754
Mosca L, Ilari A, Fazi F et al (2021) Taxanes in cancer treatment: activity, chemoresistance and its overcoming. Drug Resist Updates 54. https://doi.org/10.1016/J.DRUP.2020.100742
Pohlmann J, Bachmann F, Schmitt-Hoffmann A et al (2011) Abstract 1347: BAL101553: an optimized prodrug of the microtubule destabilizer BAL27862 with superior antitumor activity. Cancer Res 71:1347. https://doi.org/10.1158/1538-7445.AM2011-1347
Prota AE, Danel F, Bachmann F et al (2014) The novel microtubule-destabilizing drug BAL27862 binds to the colchicine site of tubulin with distinct effects on microtubule organization. J Mol Biol 426:1848–1860. https://doi.org/10.1016/J.JMB.2014.02.005
Bachmann F, Burger K, Lane H (2015) Abstract 3789: BAL101553 (prodrug of BAL27862): the spindle assembly checkpoint is required for anticancer activity. Cancer Res 75:3789. https://doi.org/10.1158/1538-7445.AM2015-3789
Sharma A, Bachmann F, Broggini-Tenzer A et al (2017) The novel tubulin-binding, tumor checkpoint controller BAL101553 has differential effects on tumor vascularization with IV and oral dosing and provides superior anti-tumor activity in combination with bevacizumab. Cancer Res 77. https://doi.org/10.1158/1538-7445.AM2017-LB-151. LB-151-LB-151
Bachmann F, Lane H (2012) 421 dual mechanism of action of the Novel Microtubule-targeting drug BAL27862 (active Moiety of the Prodrug BAL101553): targeting Tumor and Vascular cells. Eur J Cancer 48:128. https://doi.org/10.1016/S0959-8049(12)72219-0
Bachmann F, Burger K, Duran GE et al (2014) Abstract 831: BAL101553 (prodrug of BAL27862): a unique microtubule destabilizer active against drug refractory breast cancers alone and in combination with trastuzumab. Cancer Res 74:831. https://doi.org/10.1158/1538-7445.AM2014-831
Duran GE, Lane H, Bachmann F, Sikic BI (2010) In vitro activity of the novel tubulin active agent BAL27862 in MDR1(+) and MDR1(-) human breast and ovarian cancer variants selected for resistance to taxanes. Cancer Res 70. https://doi.org/10.1158/1538-7445.AM10-4412
Esteve M-A, Honore S, Mckay N et al (2010) Abstract 1977: BAL27862: a unique microtubule-targeted drug that suppresses microtubule dynamics, severs microtubules, and overcomes Bcl-2- and tubulin subtype-related drug resistance. Cancer Res. https://doi.org/10.1158/1538-7445.AM10-1977. 70:1977
Sharma A, Broggini-Tenzer A, Vuong V et al (2017) The novel microtubule targeting agent BAL101553 in combination with radiotherapy in treatment-refractory tumor models. Radiother Oncol 124:433–438. https://doi.org/10.1016/j.radonc.2017.07.024
Kristeleit R, Evans J, Molife LR et al (2020) Phase 1/2a trial of intravenous BAL101553, a novel controller of the spindle assembly checkpoint, in advanced solid tumours. Br J Cancer 123:1360–1369. https://doi.org/10.1038/S41416-020-1010-8
Joerger M, Stathis A, Metaxas Y et al (2020) A phase 1 study of BAL101553, a novel tumor checkpoint controller targeting microtubules, administered as 48-h infusion in adult patients with advanced solid tumors. Investig New Drugs 38:1067–1076. https://doi.org/10.1007/s10637-019-00850-z
Tiu C, Tzankov A, Plummer R et al (2020) 382P the potential utility of end-binding protein 1 (EB1) as response-predictive biomarker for lisavanbulin: final results from a phase I study of lisavanbulin (BAL101553) in adult patients with recurrent glioblastoma (GBM). Ann Oncol 31:S404. https://doi.org/10.1016/J.ANNONC.2020.08.491
Burgenske DM, Talele S, Pokorny JL et al (2022) Preclinical modeling in glioblastoma patient-derived xenograft (GBM PDX) xenografts to guide clinical development of lisavanbulin - a novel tumor checkpoint controller targeting microtubules. Neurooncology 24:384–395. https://doi.org/10.1093/neuonc/noab162
Bergès R, Tchoghandjian A, Honoré S et al (2016) The novel tubulin-binding checkpoint activator BAL101553 inhibits EB1-dependent migration and invasion and promotes differentiation of glioblastoma stem-like cells. Mol Cancer Ther 15:2740–2749. https://doi.org/10.1158/1535-7163.MCT-16-0252
Bergès R, Tchoghandjian A, Sergé A et al (2020) EB1-dependent long survival of glioblastoma-grafted mice with the oral tubulin-binder BAL101553 is associated with inhibition of tumor angiogenesis. Oncotarget 11:759–774. https://doi.org/10.18632/oncotarget.27374
Skowronska M, Tiu CD, Tzankov A et al (2021) Expression of end-binding protein 1 (EB1), a potential response-predictive biomarker for lisavanbulin, in glioblastoma and various other solid tumor types. J Clin Oncol 39:3118. https://doi.org/10.1200/JCO.2021.39.15_suppl.3118
Tiu CD, Derby S, Haris NM et al (2021) The potential utility of end-binding protein 1 (EB1) as response-predictive biomarker for lisavanbulin: a phase 2 study of lisavanbulin (BAL101553) in adult patients with recurrent glioblastoma. J Clin Oncol 39:TPS2068–TPS2068. https://doi.org/10.1200/JCO.2021.39.15_suppl.TPS2068
Acknowledgements
We thank the patients and their families for their participation in this study, and the staff from the SAKK Coordinating Center.
Funding
The work was supported by Basilea Pharmaceutica International Ltd, Allschwil.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Markus Joerger, Thomas Hundsberger, Anastasios Stathis, Roger von Moos, Simon Haefliger, Andreas Hottinger, and Patrick Roth. The first draft of the manuscript was written by Thomas Kaindl, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
MJ, TH, SH, RvM, AH, PR, and AS report no conflict of interest in relation to the current study. TK, ME, MM, and HL are employees of Basilea Pharmaceutica International Ltd, Allschwil.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committees, and with the Declaration of Helsinki or comparable ethical standards.
Informed consent
Written informed consent was obtained from all patients included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Joerger, M., Hundsberger, T., Haefliger, S. et al. Safety and anti-tumor activity of lisavanbulin administered as 48-hour infusion in patients with ovarian cancer or recurrent glioblastoma: a phase 2a study. Invest New Drugs 41, 267–275 (2023). https://doi.org/10.1007/s10637-023-01336-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-023-01336-9