Abstract
Background
Pediatric Inflammatory Bowel Disease (IBD) imposes significant healthcare costs and strains emergency services. This study aimed to identify factors associated with unplanned healthcare usage among children with IBD in a rural, medically underserved region in the southeastern United States.
Methods
In this retrospective cohort study, we analyzed children (<18 years) with moderate or severe IBD followed at an academic pediatric gastroenterology clinic between 2016 and 2021. Each planned visit was treated as a separate observation, and patients were followed after each planned visit until the occurrence of the earliest unplanned healthcare event, until the next planned visit, or until censoring.
Results
In our analysis of 471 planned visits from 70 children with IBD, we observed 84 (18%) unplanned visits within 12 months, with 39 of these visits related to IBD. Unplanned visits occurred at a median interval of 39 days, predominantly to the emergency department (ED). Multivariate Cox proportional hazards analysis revealed a higher hazard of unplanned visits among female patients, individuals with elevated C-reactive protein levels and anemia, those covered by Medicaid insurance, and those residing closer to the clinic.
Conclusions
This study elucidates the challenges faced by children with IBD in rural settings. By identifying factors associated with unplanned healthcare utilization, we can better pinpoint patients who may benefit from targeted interventions to reduce such visits.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
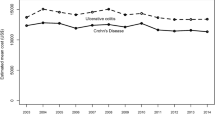
Inflammatory bowel disease (IBD) encompasses chronic, inflammatory disorders affecting the gastrointestinal tract, including ulcerative colitis and Crohn’s disease. The incidence of pediatric IBD in North America ranges from 2.4 to 15.4 per 100,000 person-years and is steadily increasing [1]. These conditions commonly manifest during adolescence and incur significant healthcare expenditure due to the complex nature of their management. The annual healthcare costs of IBD in the United States are estimated to range between 14 and 30 billion dollars, [2] with unplanned healthcare visits, such as emergency department (ED) visits and hospitalizations serving as important cost drivers [3,4,5,6,7]. Unplanned healthcare utilization among children with IBD is not only associated with reduced quality of life, [6] but also imposes substantial out-of-pocket expenses, [8] and exacerbates the strain on already overwhelmed emergency departments. Children with IBD have significantly higher healthcare costs and utilization compared to adults, possibly due to the increased severity of disease in children compared with adults [6].
Patients with IBD often seek care in the ED during periods of uncontrolled disease activity, known as flares. In this population, specific symptoms and use of certain medications can serve as indicators of disease activity and impact the likelihood of unplanned healthcare visits. For example, among adult patients with IBD, those experiencing fatigue and abdominal pain tend to utilize health services more frequently [9]. In children with IBD, higher ED utilization has been linked to increased primary care physician visits in the preceding year and longer travel distances to the gastroenterologist [10]. Furthermore, factors such as female sex, younger age, Medicaid insurance (in comparison to commercial insurance), and rural residence have been associated with more frequent ED visits or hospitalizations in individuals with IBD [6, 9, 11].
Unplanned visits among patients with IBD are more prevalent in rural compared to urban areas in Canada, [11] yet the determinants of such visits among rural children with IBD remain poorly understood. This knowledge gap is partly due to the predominance of data from urban centers in the pediatric literature [10, 12]. Moreover, existing research on healthcare utilization among patients with IBD has centered on adults; [4, 9, 13] employing cross-sectional study designs that assess predictors of unplanned visits at a single time point [6, 10, 11]. This approach hinders examining whether symptomatic improvement or changes in disease progression could influence the risk of unplanned healthcare visits. Consequently, we conducted a longitudinal study to ascertain the clinical and socioeconomic factors associated with unplanned healthcare utilization among children diagnosed with moderate-to-severe IBD residing in a rural, medically underserved region in the southeastern United States.
Methods
Sample Selection
This retrospective cohort study was approved by the local Institutional Review Board with a waiver of informed consent. We included patients under 18 years of age who were seen in our academic pediatric gastroenterology clinic between 2016 and 2021 and had moderate or severe IBD (based on use of immunomodulators or biologic medications) at any time during this period. The clinic is located near our health system’s main campus in Greenville, North Carolina, which includes the only children’s hospital and children’s ED in the 29-county region served by this health system. The hospital, ED, and outpatient clinics share the same electronic medical record (EMR). For eligible patients, we analyzed all planned pediatric gastroenterology visits to the outpatient clinic or the hospital (including planned telemedicine visits). Each planned visit to the clinic or hospital between 2016 and 2021 (defined as a regularly scheduled visit based on when the physician decided to follow up with the patient) was considered as a separate observation. We classified any “regular health maintenance visit” as a planned visit, and any “sick visit” (prompted by a change in symptoms) as an unplanned visit. Patients were excluded from the study if data on time-invariant characteristics (detailed below) were missing from their chart, and individual planned visits were excluded from the study if they occurred <6 months after first diagnosis of IBD, or if they did not involve the patient seeing a physician during that visit. Patients newly diagnosed with IBD often have higher rates of unplanned healthcare utilization, as it may take several months for them to achieve remission. Therefore, we decided to exclude planned visits occurring within the first 6 months after diagnosis.
Study Variables
Patients who met study inclusion criteria were followed after each planned clinic visit until the earliest unplanned healthcare visit; until they were known to have passed away, moved, or transferred care to another gastroenterology practice (whichever occurred earliest); or until 12 months have passed since their most recent planned clinic visit. If applicable, the next planned visit to the outpatient clinic or hospital was also considered as a censoring event. Follow-up data on unplanned visits after each planned visit were collected through June 2022. The primary outcome was unplanned healthcare utilization, defined as unplanned visits to the pediatric gastroenterology clinic, unplanned hospitalization, or ED visit in any facility for any reason. The secondary outcome was defined as unplanned health care visits specifically related to IBD. Data on hospitalizations, ED visits, and urgent care visits at outside facilities (including regional community hospitals that are part of the same academic health system) were collected if this information was recorded in the EMR.
Time-invariant independent variables included patient sex, race/ethnicity, age at the time of IBD diagnosis, and distance from the clinic (based on the ZIP code of the patient’s address). All other covariates were time-varying (assessed at the time of each planned visit), and included age at the time of the planned visit, history of IBD-related surgery, current body mass index (BMI) percentile, current symptoms (abdominal pain; diarrhea; blood in stool; nocturnal stooling; or fatigue), and current labs. For each planned visit, we queried the most recent labs obtained at that visit or up to 8 weeks prior: hemoglobin, platelets, albumin, Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP; classified as normal, <10; mild elevation, 10 to <50; moderate elevation, 50 to <100; or severe elevation, 100+). We also examined current medications (classified as infliximab, adalimumab, second-line biologics, immunomodulators; or other/none) and current insurance status (public, commercial, or self-pay) at the time of each planned visit. Second-line biologics referred to a second biologic medication (second anti-TNF agent, vedolizumab or ustekinumab) used after loss of response or primary failure of the initial anti-TNF agent.
Statistical Analysis
Data were summarized using medians and interquartile ranges (IQR) or counts and percentages at the time of the earliest and latest planned visit for each patient in the cohort. In bivariate analyses, we compared characteristics of planned visits based on whether each planned visit was followed by an unplanned visit, using rank-sum tests, Chi-square tests, or Fisher’s exact tests, as appropriate. The timing of unplanned visits after each planned visit was summarized using a Kaplan-Meier curve, and the hazard of an unplanned visit (for any reason) was modeled based on each covariate using unadjusted Cox proportional hazards regression. We then fit multivariable Cox regression models for each study outcome, including the covariates found to be statistically significant on univariate Cox regression analysis. Planned visits with incomplete data on the time-varying covariates selected for multivariable adjustment were excluded from the multivariable analysis. All Cox models included a shared frailty term at the patient level, to account for non-independence of multiple observations (planned visits) involving the same patient. Data analysis was completed in Stata/SE 16.1 (College Station, TX), and P<0.05 was considered statistically significant.
Results
Patient Characteristics
We initially identified 77 eligible patients with 523 planned visits during the study period. After excluding 7 patients due to missing or implausible data regarding their distance to the clinic, we retained 471 planned visits by 70 patients in the analysis. This included 34/36 male/female patients, 46% of whom identified as White, 44% Black, 6% Hispanic or Latino, and 3% as some other race or ethnicity. Median age at IBD diagnosis was 12 years (IQR: 10, 14), and patients lived at a median distance of 53 km (IQR: 22, 69) from the clinic. Table 1 summarizes the visit-specific characteristics, including the number of planned visits with missing data for each time-varying covariate.
Bivariate Analysis
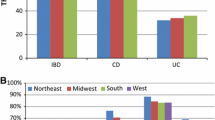
Of the total 471 planned visits, 84 (18%) were succeeded by an unplanned visit within 12 months, including 39 unplanned visits directly related to IBD. These unplanned visits typically occurred a median of 39 days after the last planned visit (IQR:14, 99) and predominantly involved visits to the emergency department (n=60), followed by hospitalizations (n=20) and unscheduled returns to the gastroenterology clinic (n=4). The Kaplan-Meier curves illustrating the time to any unplanned visit and time to IBD-related unplanned visit are depicted in Fig. 1. In our univariate Cox proportional hazards regression analysis of all-cause unplanned visits (Table 2), we observed a decreased hazard of unplanned visits among patients residing farther from the clinic, yet an increased hazard among those experiencing poor symptomatic control (e.g., abdominal pain, blood in stool) and displaying elevated inflammatory markers and thrombocytosis. Furthermore, unplanned visits were more prevalent among female patients, Hispanic and non-Hispanic Black patients, and patients covered by Medicaid insurance.
Multivariable Analysis
The multivariable model analyzing all-cause unplanned visits is shown in Table 3. We observed higher hazard of unplanned visits among female patients, those with higher CRP levels, and individuals residing closer to the clinic. Conversely, patients with commercial insurance exhibited a lower hazard for unplanned visits compared to those with Medicaid insurance. When applying the same multivariable model to examine the secondary outcome of IBD-related unplanned visits (Table 4), we found similar associations of the hazard of IBD-related unplanned visits with sex, distance from clinic, and CRP. Additionally, we found that anemia was associated with higher hazard of IBD-specific unplanned visits.
Discussion
The management of inflammatory bowel disease (IBD) in children presents notable challenges, particularly within rural settings. Our study aimed to pinpoint the clinical and socioeconomic factors predicting unplanned healthcare utilization among children with IBD receiving care at an academic center serving a predominantly rural area. We found that laboratory markers of inflammation, Medicaid insurance, and female sex, were associated with increased unplanned healthcare utilization. Interestingly, patients residing farther away from our clinic were less likely to experience unplanned health visits. These findings underscore the substantial impact of clinical and socioeconomic factors on the burden of IBD experienced by young patients, as well as the strain placed on healthcare systems in rural communities.
Our investigation revealed a significantly heightened likelihood of unplanned health visits among female patients, consistent with findings from previous studies [6, 14]. One study noted that female patients with IBD, when compared to male counterparts, reported lower quality of life, exhibited a higher prevalence of depression associated with IBD, and experienced increased disease activity [14]. Furthermore, IBD impacts the onset and regularity of women's menstrual cycles, with hormone fluctuations during the menstrual cycle known to influence IBD-related symptoms [15].
Patients covered by Medicaid insurance exhibited a higher frequency of unplanned visits compared to those with commercial insurance. This association has been documented among adults and children with IBD, and may stem from transportation obstacles, barriers to adherence to routine care, and other forms of hardship experienced by Medicaid-insured patients [6, 16, 17]. Medicaid-insured children with Crohn’s disease also have higher rates of repeat ED visits when compared to children with private insurance [16]. Children with public insurance may be more likely to use the ED for routine care, compared to those with commercial insurance, potentially due to factors such as convenience and the absence of copayments [18].
IBD is characterized by periods of remission and flare-ups. Elevated ESR and CRP levels are often associated with active inflammation, particularly in Crohn’s disease. In our multivariable analysis, CRP values greater than 10 mg/L predicted a higher hazard of all-cause and IBD-related unplanned visits. Other studies have analyzed the utility of biomarkers such as CRP and fecal calprotectin in IBD, and similarly found CRP to be a good predictor of disease activity and complications in IBD [19,20,21]. We were unable to analyze calprotectin due to missing data from the majority of planned visits (399 of 471 planned visits included in the analysis). In contrast to prior research, [4] we did not find that presence of specific symptoms during office visits predicted future ED visits or hospitalizations. We also found that lower hemoglobin was associated with higher hazard of IBD-related unplanned healthcare utilization. Similarly, a study of adults with Crohn’s disease found that anemia, tachycardia and elevated alkaline phosphatase were independently associated with ED returns within 30 days [13].
Patients residing at a greater distance from our healthcare institution exhibited a reduced likelihood of experiencing unplanned visits. This could be due to the inconvenience of traveling long distances, limited access to transportation or seeking care at urgent care center or ED affiliated with other health systems. In addition, patients living farther away may have preferentially utilized other modalities such as phone calls or online messages to connect with their gastroenterologist which may have prevented ED visits [22]. Other studies have found that patients with IBD in rural settings have a higher likelihood of ED and urgent care visits and are less likely to visit their gastroenterologist compared to those living in urban areas [10, 11, 23].
The study has certain limitations, most notably the inability to capture data on urgent care and ED visits at other nearby health systems which may not have been recorded. In addition, we did not record certain forms of healthcare utilization, such as phone calls and online messages to the clinic staff, which utilize significant resources and have been shown to occur at a high frequency in children with active IBD [22]. Our study was completed at a single center and had a small sample size, which may limit generalizability. Since this was a retrospective study, we did not have data available to calculate disease activity indices which incorporate clinical, laboratory and endoscopic parameters at a given point in time. The number of unique patients in our study was limited, although our analysis of each planned visit as a separate observation improved statistical power for detecting differences in unplanned visits based on time-varying measures.
Conclusions
This research has revealed some of the challenges faced by the rural pediatric population living with IBD which contribute to unplanned healthcare utilization. We found that severity of disease, Medicaid insurance, and female sex correlated with higher unplanned healthcare utilization. The results of this study suggest that patients with an elevated risk profile may require closer monitoring to mitigate the likelihood of emergency department visits or hospitalizations. However, our study did not support expectations from prior research that patients living further away from the clinic would have a higher risk of unplanned visits. In rural areas, drivers of unplanned visits stem from factors such as limited access to specialized healthcare services, reduced disease awareness, and potential disparities in treatment options. By addressing these specific challenges to healthcare access in rural areas, healthcare providers and policymakers can work towards ensuring equitable access to care and enhancing the well-being of this vulnerable population, thereby reducing the burden on healthcare systems.
Data availability
Data is provided within the manuscript or supplementary information files
References
Kuenzig ME, Fung SG, Marderfeld L et al. Twenty-first century trends in the global epidemiology of pediatric-onset inflammatory bowel disease: systematic review. Gastroenterology. 2022;162:1147-1159.e4.
Mehta F. Report: economic implications of inflammatory bowel disease and its management. Am J Manag Care. 2016;22:s51–s60.
Pant C, Deshpande A, Fraga-Lovejoy C et al. Emergency department visits related to inflammatory bowel disease: results from nationwide emergency department sample. J Pediatr Gastroenterol Nutr. 2015;61:282–284.
Nguyen NH, Zhang X, Long MD et al. Patient-reported outcomes and risk of hospitalization and readmission in patients with inflammatory bowel diseases. Dig Dis Sci. 2022;67:2039–2048. https://doi.org/10.1007/s10620-021-07082-3.
Sin AT, Damman JL, Ziring DA et al. Out-of-pocket cost burden in pediatric inflammatory bowel disease: a cross-sectional cohort analysis. Inflamm Bowel Dis. 2015;21:1368–1377.
Kappelman MD, Porter CQ, Galanko JA, et al. Utilization of healthcare resources by U.S. children and adults with inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:62-68
El-Matary W, Kuenzig ME, Singh H et al. Disease-associated costs in children with inflammatory bowel disease: a systematic review. Inflamm Bowel Dis. 2020;26:206–215.
Ballou S, Hirsch W, Singh P et al. Emergency department utilization for inflammatory bowel disease in the United States from 2006 to 2014. Aliment Pharmacol Ther. 2018;47:913–921.
Bogale K, Maheshwari P, Kang M, et al. Symptoms associated with healthcare resource utilization in the setting of inflammatory bowel disease. Sci Rep. 2022;12:10577. Published Jun 22 2022
Michel HK, Noll RB, Siripong N, Kim SC. Patterns of primary, specialty, urgent care, and emergency department care in children with inflammatory bowel diseases. J Pediatr Gastroenterol Nutr. 2020;71:e28–e34.
Benchimol EI, Kuenzig ME, Bernstein CN et al. Rural and urban disparities in the care of Canadian patients with inflammatory bowel disease: a population-based study. Clin Epidemiol. 2018;10:1613–1626.
Dheri AK, Kuenzig ME, Mack DR et al. Shifting health care use from hospitalisations and surgeries to outpatient visits in children with inflammatory bowel disease: a population-based cohort study from ontario. Canada J Crohns Colitis. 2021;15:1991–2000.
Mahajna H, Barash Y, Ungar B et al. Prediction of recurrent emergency department visits among patients with crohn’s disease: a retrospective study. J Clin Med. 2020;9:3651.
Greuter T, Manser C, Pittet V, et al.; on behalf of Swiss IBDnet, an official working group of the swiss society of gastroenterology. Gender differences in inflammatory bowel disease. Digestion. 2020;101 Suppl 1:98-104
Rosenblatt E, Kane S. Sex-specific issues in inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2015;11:592–601.
Dotson JL, Kappelman MD, Bricker J et al. multicenter evaluation of emergency department treatment for children and adolescents with Crohn’s Disease according to race/ethnicity and insurance payor status. Inflamm Bowel Dis. 2019;25:194–203.
Axelrad JE, Sharma R, Laszkowska M et al. Increased healthcare utilization by patients with inflammatory bowel disease covered by medicaid at a tertiary care center. Inflamm Bowel Dis. 2019;25:1711–1717.
Schlichting LE, Rogers ML, Gjelsvik A et al. Pediatric emergency department utilization and reliance by insurance coverage in the United States. Acad Emerg Med. 2017;24:1483–1490.
Li T, Qian Y, Bai T, Li J. Prediction of complications in inflammatory bowel disease using routine blood parameters at diagnosis. Ann Transl Med. 2022;10:185. https://doi.org/10.21037/atm-22-123.
Vermeire S, Van Assche G, Rutgeerts P. Laboratory markers in IBD: useful, magic, or unnecessary toys? Gut. 2006;55:426–31.
Huh G, Yoon H, Choi YJ, et al. Trends in emergency department visits and hospitalization rates for inflammatory bowel disease in the era of biologics. PLoS One. 2019 Jan 16;14(1):e0210703. Erratum in: PLoS One. 2019 May 7;14:e0216768
Wojtowicz AA, Plevinsky JM, Poulopoulos N et al. Examining predictors of healthcare utilization in youth with inflammatory bowel disease. Eur J Gastroenterol Hepatol. 2016;28:469–74.
Xu F, Carlson SA, Liu Y, Greenlund KJ. Urban-rural differences in health care utilization for inflammatory bowel disease in the USA, 2017. Dig Dis Sci. 2022;67:3601–3611. https://doi.org/10.1007/s10620-021-07264-z.
Funding
Open access funding provided by the Carolinas Consortium.
Author information
Authors and Affiliations
Contributions
CG: study design, data collection and writing up of the first draft of the paper RS: data collection and writing up of the first draft of the paper DT: study design, data collection, data analysis, editing draft manuscript CM: study design, data collection, editing draft manuscript
Corresponding author
Ethics declarations
Conflicts of interest
No funding sources, financial disclosures, or conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gray, C., Shakir, R., Tumin, D. et al. Predictors of Unplanned Health Care Utilization Among Children with Inflammatory Bowel Disease in a Rural Region of the Southeastern US. Dig Dis Sci (2024). https://doi.org/10.1007/s10620-024-08619-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10620-024-08619-y