Abstract
Introduction
Abdominal aortic calcifications (AAC) are incidentally found on medical imaging and useful cardiovascular burden approximations. The Morphomic Aortic Calcification Score (MAC) leverages automated deep learning methods to quantify and score AACs. While associations of AAC and non-alcoholic fatty liver disease (NAFLD) have been described, relationships of AAC with other liver diseases and clinical outcome are sparse. This study’s purpose was to evaluate AAC and liver-related death in a cohort of Veterans with chronic liver disease (CLD).
Methods
We utilized the VISN 10 CLD cohort, a regional cohort of Veterans with the three forms of CLD: NAFLD, hepatitis C (HCV), alcohol-associated (ETOH), seen between 2008 and 2014, with abdominal CT scans (n = 3604). Associations between MAC and cirrhosis development, liver decompensation, liver-related death, and overall death were evaluated with Cox proportional hazard models.
Results
The full cohort demonstrated strong associations of MAC and cirrhosis after adjustment: HR 2.13 (95% CI 1.63, 2.78), decompensation HR 2.19 (95% CI 1.60, 3.02), liver-related death HR 2.13 (95% CI 1.46, 3.11), and overall death HR 1.47 (95% CI 1.27, 1.71). These associations seemed to be driven by the non-NAFLD groups for decompensation and liver-related death [HR 2.80 (95% CI 1.52, 5.17; HR 2.34 (95% CI 1.14, 4.83), respectively].
Discussion
MAC was strongly and independently associated with cirrhosis, liver decompensation, liver-related death, and overall death. Surprisingly, stratification results demonstrated comparable or stronger associations among those with non-NAFLD etiology. These findings suggest abdominal aortic calcification may predict liver disease severity and clinical outcomes in patients with CLD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic liver diseases (CLD) are estimated to affect 1.5 billion people worldwide [1, 2]. Causally, 59% of CLDs are attributed to non-alcoholic fatty liver disease (NAFLD), 9% to hepatitis C virus (HCV), and 2% to alcohol-related liver disease (ETOH) [2,3,4]. Comorbid occurrences of hepatic manifestation and cardiovascular conditions are prevalent; those with CLD have higher cardiovascular disease (CVD) burden than the general population [5, 6]. The strongest risk factors for NAFLD and CVD include insulin resistance, diabetes, obesity, and metabolic syndrome [7,8,9,10,11].
Abdominal aortic calcifications (AAC) were previously considered incidental findings from medical imaging. AAC has recently gained clinical interest as a strong independent predictor of incident CVD and related events [12,13,14,15,16]. Previous research has demonstrated strong associations of AAC with standard cardiovascular risk scores, stronger predictive ability of AAC for cardiovascular events than Framingham Risk Scores, evidence supporting the approximation of coronary calcification scores from AAC, and demonstration of AAC additively improving cardiovascular risk classification [15, 17,18,19,20,21]. Computer tomography (CT) scans can be opportunistically leveraged for surveillance purposes, capturing calcification measurements in anyone who already has a scan and contextualizing calcification burden among the general population [22, 23]. The Morphomics Analysis Group has developed the Morphomic Aortic Calcification Score (MAC) to identify those with elevated AAC [18, 21].
While the relationship of AAC and NAFLD has been described, evidence supporting the associations of AAC with other liver diseases and clinical outcomes is relatively sparse and may be overlooked [6]. The liver is a central organ supporting homeostasis, metabolism, immunity, digestion, and detoxification [24, 25]. Modification of lipid and glucose metabolism are common factors of both cardiovascular disease and liver disease [26,27,28,29]. While similar, the causal direction of effect of CLD and other metabolic diseases is difficult to discern and likely bidirectional [30,31,32,33]. While the pathogenic mechanism is not well understood, the associations between CLD and CVD are of clinical importance: for example, the treatment of HCV results in improved all-cause mortality including CVD-related outcomes [33,34,35].
The purpose of this study was to evaluate the association of AAC and liver-related clinical outcomes in a large cohort of Veterans with CLD. We sought to evaluate the effects of elevated aortic calcification and clinically relevant events when stratified by NAFLD classifications. Understanding the clinical effects of AAC and NAFLD may further assist clinicians in identifying those who may benefit from intervention or treatment.
Methods
Study Cohort
This study retrospectively utilizes the Veterans Integrated Services Network (VISN) 10 liver disease cohort [36]. Encounters occurred within the VISN 10 regional Veterans Health Administration network and the Danville, Illinois facility. Participants had an inpatient or outpatient encounter and a liver disease diagnosis between 1/1/2008 and 12/31/2014 and had an abdominal CT within 90 days of the diagnosis code. The cohort was restricted to include those with the three main liver disease diagnoses (HCV, NAFLD, and ETOH). HCV was defined as any positive HCV viral load during the study period. Patients with alcoholic liver disease were identified using ICD-9 codes for alcohol-related diseases or positive AUDIT-C scores (3 for female and 4 for male) in the absence HCV virus or ICD codes for other liver diseases (see supplementary tables). NAFLD was defined based on the absence of HCV virus, ETOH codes or positive alcohol use disorders identification test (AUDIT-C) and International Statistical Classification of Disease and Related Health Problem (ICD) codes for other liver diseases. Participants were excluded if mortality occurred within 180 days of the CT, had liver transplant or hepatocellular carcinoma at entry to cohort. Due to MAC score depending on the presence of abdominal CT scans, participants without observable imaging at the L3 and L4 vertebral level were removed from the analysis (N = 4616, n = 3604, removed 1008). See Fig. 1 for a flowchart describing the selection procedure and study design.
Study Measures
Cirrhosis, decompensated cirrhosis, diabetes mellitus, hypertension, and peripheral vascular disease was defined based off ICD-9 or ICD-10 codes (provided in supplemental information). Death was obtained from SPatient table found in the Veterans Affairs’ Corporate Data Warehouse (VA CDA) [37]. The “Vital Status” file was used for verification and validation. Outcomes were conditionally dependent on ICD-9 or ICD-10 codes and accumulated time after the CT date [38]. For the outcome of hepatic decompensation, we utilized the codes previously described and validated in the VA CDA with the exclusion of the codes for esophageal varices without bleed (ICD 9- 456.21) [38]. Survival time was based on introduction to study or first diagnosed outcome or censoring. Accumulated time was calculated for each specific outcome (accumulated days-to-death, hepatic decompensation days, cirrhosis days). Death hazard was modeled as presence of death outcome, and time-to-death. Hepatic decompensation (outcome) was defined as presence of decompensation and time-to-hepatic decompensation development. Cirrhosis (outcome) was defined as presence of cirrhosis and time-to-cirrhotic development. Liver-related death was defined as the presence of decompensated outcome prior to time-to-death. Those with baseline cirrhosis or decompensation were excluded from the development of cirrhosis or decompensation.
Aortic calcification biomarkers were measured using Analytic Morphomics [21, 22, 39]. MAC score conceptualization and operationalization are described elsewhere [18, 21,22,23]. Briefly, the central aortic lumen zone was identified on each CT slice between the L1 and L4 vertebral levels. Dynamic thresholding was used to identify calcification regions and to control for measurement confounding created by contrast phase [22]. Morphological regions with pixel values five standard deviations above the reference were classified as calcification [21, 22]. AAC was conceptualized as the percentage of the aortic wall obfuscated by calcification. A binary MAC score is useful to identify those with clinically elevated calcification levels: those with calcification greater than 4.21% of the aortic wall relative to the L3 and L4 levels were considered elevated [18]. The threshold of 4.21% was chosen to maximize the sensitivity and probability of discovering those with elevated calcium burden [21, 23].
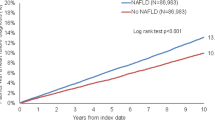
Descriptive statistics were performed to report differences among cohort participants with the three different CLD diagnoses. Logistic regression was used to evaluate the odds of clinical comorbidities among all cohort participants with elevated and normal MAC scores. Logistic regression was also performed to establish an association of aortic calcification with clinical comorbidities for adjustment in the Cox proportional hazard models. Cox proportional hazard was used to estimate the hazard of each clinical outcome among participants with elevated and normal MAC scores. Proportional hazards assumptions were verified through graphical inspection Figs. 2 and 3 displays Kaplan-Meier curves reflecting survival probability for each clinical outcome. Hazard ratios for all participants are reported, as well as stratification by NAFLD (n = 2513) and non-NAFLD (n = 1091). Logistic regression models were adjusted for age and sex. Cox proportional hazard ratios were adjusted for age, sex, body mass index (BMI), peripheral vascular disease, congestive heart failure, hypertension, and diabetes.
A sensitivity analysis was performed to evaluate the relationship of hepatic steatosis severity on aortic calcification and the clinical outcomes investigated in this study. Participants with ETOH liver disease were removed from consideration as ETOH would have a different causal mechanism of hepatic steatosis. Severity of hepatic steatosis was classified based on prior classification determined using MRI PDFF [40]. Those with a median value below 57 HU were categorized as normal levels (n = 234), a median 42–57 HU were mildly elevated levels (n = 618), a median 18–42 were moderately elevated levels (n = 378), and those under 18 HU were severely elevated levels (n = 52) Due to sample size and prevalence of outcomes steatosis factors were condensed into those of lower (n = 852) and higher (n = 430) steatosis severity.
Analysis was performed with R version 4.12 [41]. Figures were generated with ggplot2 [42]. Where appropriate, statistical significance was set to α = 0.05.
Results
Table 1 reports baseline descriptive statistics for the three groups used in the analysis (NAFLD, HCV, ETOH). Mean patient age at CT was 62.70 (SD 12.64) for NAFLD, 57.04 (SD 7.02) for HCV, and 57.45 (SD 11.22) for ETOH. The cohort was mostly white (76%) and male (93%). Mean BMI was 30.81 (SD 6.65) for NAFLD, 27.32 (SD 5.77) for HCV, and 28.38 (SD 6.48) for ETOH. Most groups were significantly different regarding clinical comorbidities and outcomes.
Mean and median aortic attenuation were not significantly different among the three groups. Mean total abdominal calcium volume at the L3 vertebral level was 633.59 mm3 (SD 965.16) for NAFLD participants, 691 mm3 (SD 979.12) for HCV, and 468.82 mm3 (SD 730) for ETOH participants. Mean wall percent calcification was 16.71 (SD 21.34) for NAFL, 13.38 (SD 17.87) for HCV, and 18.19 (SD 18.19), and 18.19 (SD 21.18) for ETOH participants. Elevated MAC scores were most prevalent in the ETOH group (~ 63%), followed by the NAFLD group (~ 58%) and the HCV group (~ 55%).
Table 2 reports odds ratios between the MAC scores and presence of clinical comorbidities in the full cohort. Significant unadjusted associations were observed for all clinical comorbidities (Cirrhosis, Decompensated Cirrhosis, Diabetes Mellitus, Hypertension, Congestive Heart Failure). After adjustment for age, significant associations were observed between MAC and the clinical comorbidities in all instances. After adjustment for age and sex, significant associations were observed between MAC and cirrhosis [OR 2.34 (95% CI 1.79, 3.08)], decompensated cirrhosis [OR 3.04 (1.93, 4.94)], diabetes mellitus [OR 1.23 (95% CI 1.05, 2.14)], hypertension [OR 1.47 (1.03, 2.14)], peripheral vascular disease [OR 1.92 (95% CI 1.54, 2.52)], and congestive heart failure [OR 1.39 (95% CI 1.07, 1.83)].
Table 3 reports the relevant clinical events and contributed days for each CLD group observed during the study period. Significant differences were observed for all groups across observed events and contributed time. The maximum contributed study days for any participant was 4015. Overall death was observed at the highest proportion for the ETOH group (37.9%) and the least for the NAFLD group (29.6%). Decompensation was the most prevalent in the HCV group (16.4%) and least prevalent in the NAFLD group (3.5%). Cirrhosis was the most prevalent in the HCV group (43.1%) and lowest in the NAFLD group (9.8%). Liver-related death was most prevalent in the HCV group (13.2%) and lowest in the NAFLD group (2.4%). Median contribution days were highest for the HCV group for death [median 2232 IQR (1583, 3320)] and hepatic decompensation [median 2160 IQR (1526, 3183)], while the NAFLD group had the most contributed days the cirrhosis [median 1922 IQR (1367, 2617)] and liver-related death [median 1250 IQR (448,1945)].
Table 4 reports hazards ratios of elevated MAC score and clinical outcomes stratified by chronic liver disease status in the CLD Cohort. Cirrhosis development was significantly associated with MAC across the different strata, except for HCV status. Associations remained statistically significant after adjustment in the full cohort, the NAFLD and non-NAFLD (HCV+ETOH) groups (See Fig. 4), HRs 2.13 (1.63, 2.78), 2.19 (95% CI 1.41, 3.41), 2.05 (95% CI 1.28, 3.28), respectively. Hepatic decompensation development significantly increased with elevated MAC in the fulld cohort, HR 2.19 (95% CI 1.60, 3.02). This relationship seemed driven by the non-NAFLD group, (HCV + ETOH) HR 2.80 (95% CI 1.52, 5.17), more than the NAFLD group HR 1.32 (95% CI 0.79, 2.20). Similar findings were observed with liver-related death and MAC, HR 2.13 (95% CI 1.46, 3.11) for the full cohort, and for HCV + ETOH, HR 2.34 (95% CI 1.14, 4.83). Overall death was associated with MAC in the full cohort, HR 1.47 (95% CI 1.27, 1.71), for NAFLD HR 1.34 (95% CI 1.11, 1.61) and HCV + ETOH 1.67 (95% CI 1.19, 2.36).
Table 5 reports hazard ratios for MAC score and clinical outcomes stratified by hepatic steatosis severity. Among participants with lower steatosis severity (normal or mild rated liver density) having elevated aortic calcification resulted in increased hazard regarding cirrhosis HR 2.01 (95% CI 1.13, 3.53) and overall death HR 2.41 (95% CI 1.79, 3.23). Those with higher steatosis severity and elevated aortic calcification had higher hazards for all clinical outcomes: cirrhosis HR 3.04 (95% CI 1.33, 6.93), decompensation HR 3.67 (95% CI 1.40, 9.61), liver-related death HR 6.88 (1.59, 29.67) and HR 3.28 (95% CI 1.93, 5.57).
Discussion
We evaluated the relationship of a novel aortic wall percent calcification score (MAC), with comorbidities and chronic liver disease-related outcomes in a cohort of veterans. MAC was found to be independently associated with cirrhosis, decompensation, liver-related death, and overall death after adjustment for age, sex, and common clinical comorbidities. After stratification by NAFLD status, the relationship of MAC with decompensation and liver-related death in patients with NAFLD was attenuated, while the relationship of MAC with cirrhosis and overall death remained significant. In those with HCV and ETOH, associations of elevated MAC with cirrhosis, decompensation, liver-related death, and overall death remained after multiple adjustment, although this appears to be driven by ETOH. After limiting to those without ETOH, elevated steatosis severity had greater hazard magnitude for cirrhosis, decompensation, liver-related death, and overall death.
The consistent association of NAFLD with subclinical atherosclerosis and prevalent CVD is well established [7, 43,44,45,46]. While the findings of this study do support the relationship between NAFLD and atherosclerosis, it is surprising to see stronger hazard ratios among MAC and some clinical outcomes for the HCV and ETOH strata. Liver fibrosis has previously been associated with aortic calcification while cirrhosis has been reported to increase the risk of cardiovascular death regardless of etiology and stage of disease [47,48,49,50,51,52,53]. Both aortic calcification and liver fibrosis are causally influenced by inflammation, elevated oxidative stress, and accumulation of pro-inflammatory macrophages [47, 54, 55]. Vascular calcification approximates prolonged disease states of the medial or intimal wall and may explain the overarching relationship [14, 56, 57]. Further, inorganic pyrophosphate deficiencies are associated with pathologic calcification, dysregulation provides a potential encompassing mechanism for arterial calcification promotion [47, 58, 59]. An observational study of hepatic pyrophosphate deficiency reported inorganic pyrophosphate before and after liver transplantation; authors determined that promotion of arterial calcification in several arterial beds were attributed to inorganic pyrophosphate dysregulation via liver disease [47].
While studies examining the relationship of NAFLD and atherosclerosis are prevalent, relatively few studies examine this relationship in those with ETOH-related CLD [60]. A coronary imaging study of patients with end-stage renal disease (due to ETOH) demonstrated higher total prevalence of coronary calcification when compared to the prevalence of a matched cohort without CLD [61]. Further, higher risk of CVD-related mortality has been noted in those with ETOH related CLD than with NAFLD [62]. While stronger risk of atherosclerosis was reported for the ETOH than NAFLD strata, the authors thoughtfully point out that the ETOH group had more advanced states liver disease compared to NAFLD group [60]. Regardless, large cross-sectional study estimated that 10-year Framingham Risk Scores were similar in those with ETOH and NAFLD compared to those without liver disease [63].
Strong associations between HCV and atherosclerosis are reported in all outcomes but cirrhosis, even with adjustment for cardiovascular risk factors [33,34,35, 64]. Those with chronic HCV infection are susceptible to cardiovascular morbidities through inflammatory and lipid processes [65]. In large cohort studies, those with diagnosed HCV had higher all-cause mortality and diagnostic status was an independently associated with cerebrovascular death [33, 65,66,67,68]. However, this could be due to the high co-occurrence of type 2 diabetes, insulin resistance, and steatosis among those with chronic HCV infection and will require further evaluation [69,70,71,72].
Consistent associations between vitamin K deficiency and vascular calcification are reported in the literature [73,74,75,76]. Vitamin K deficiency is also commonly observed in patients with CLD, and some suggest a protective effect of vitamin K on CLD, particularly metabolic dysfunction-associated fatty liver disease [77,78,79,80,81]. The overlying relationship between vitamin K, atherosclerosis, and CLD may be due to shared risk factors, heterostasis, physical function, or indicative of disease state. Further epidemiologic and causal studies will be necessary to evaluate a common mechanism.
Despite the study population being scanned for indications outside of cardiovascular disease, we detected elevated atherosclerotic burden in more than 55% of the study population. For reference, AAC prevalence has been estimated at 29% in NHANES [82]. Previous studies have associated aortic calcification with cardiovascular disease, overall mortality, incident coronary heart disease, myocardial infarction, diabetes mellitus, and stroke [13, 16, 82, 82,83,84,85,86,87,88]. Unsurprisingly, the logistic regression results of this study indicated strong associations of MAC with diabetes mellitus, hypertension, peripheral vascular disease, and congestive heart failure.
This work has limitations. The cohort is limited to veterans, who have been noted to have higher rates of chronic liver disease relative to the general population [1, 89]. There may an additional selection bias as this cohort is limited to those with abdominal CT scan. Therefore, the results may not be generalizable, and magnitude of effect estimates could be biased away from the null. As the secondary data used in this study leverages patient encounters rather than the recruitment of participants, it is difficult to ascertain whether the patient was lost to follow-up before the study ended. As such, informative biases may exist inflating contribution time in non-censored observations. Finally, as this analysis is cross-sectional, causal inference is limited.
Nevertheless, this work highlights the comorbidity of elevated aortic calcification with NAFLD, HCV, and alcohol-related liver diseases in a large clinically relevant cohort. Future work should validate the direction and magnitude of the relationship between aortic calcification and non-NAFLD liver diseases. Such validation will contextualize comorbidity between atherosclerotic cardiovascular disease and chronic liver diseases and may be useful for the mitigation of cirrhosis, decompensation, liver-related death, and overall death in the clinical setting.
Data availability
Analyses were performed using data from Corporate Data Warehouse domains that are only available within a secure research environment behind the US Department of Veterans Affairs firewall. To comply with VA privacy and data security policies and regulatory constraints, only aggregate summary statistics and results of our analyses are permitted to be shared for publication. Restrictions are in place to maintain Veteran privacy and confidentiality. Access to these data can be granted to persons who are not employees of the VA; however, there is an official protocol that must be followed. Interested researchers can contact the VA Center for Clinical Management Research.
Abbreviations
- AAC:
-
Abdominal aortic calcification
- AUDIT-C:
-
Alcohol use disorders identification test
- CLD:
-
Chronic liver disease
- CT:
-
Computed tomography
- CVD:
-
Cardiovascular disease
- HCV:
-
Hepatitis C Virus
- ICD:
-
International Statistical Classification of Disease and Related Health Problem
- MAC:
-
Morphomic Aortic Calcification Score
- NAFLD:
-
Non-alcoholic fatty liver disease
- VISN:
-
Veterans Integrated Services Network
References
Moon AM, Singal AG, Tapper EB. Contemporary epidemiology of chronic liver disease and cirrhosis. Clin Gastroenterol Hepatol. 2020;18:2650–66.
Cheemerla S, Balakrishnan M. Global epidemiology of chronic liver disease. Clin Liver Dis. 2021;17:365–70.
GBD 2017 Cirrhosis Collaborators. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5:245–66.
Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70:151–71.
Weisberg IS, Jacobson IM. Cardiovascular diseases and the liver. Clin Liver Dis. 2011;15:1–20.
Chang WH, Mueller SH, Chung S-C, Foster GR, Lai AG. Increased burden of cardiovascular disease in people with liver disease: unequal geographical variations, risk factors and excess years of life lost. J Transl Med. 2022;20:2.
Targher G, Byrne CD, Tilg H. NAFLD and increased risk of cardiovascular disease: clinical associations, pathophysiological mechanisms and pharmacological implications. Gut. 2020;69:1691–705.
Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363:1341–50.
Adams LA, Anstee QM, Tilg H, Targher G. Non-alcoholic fatty liver disease and its relationship with cardiovascular disease and other extrahepatic diseases. Gut. 2017;66:1138–53.
National Guideline Centre (UK). Risk factors for NAFLD. National Institute for Health and Care Excellence (NICE); 2016. https://www.ncbi.nlm.nih.gov/books/NBK384735/
Lin A, Roth H, Anyane-Yeboa A, Rubin DT, Paul S. Prevalence of nonalcoholic fatty liver disease in patients with inflammatory bowel disease: a systematic review and meta-analysis. Inflamm Bowel Dis. 2020;27:947–55.
Criqui MH, Denenberg JO, Ix JH, McClelland RL, Wassel CL, Rifkin DE et al. Calcium density of coronary artery plaque and risk of incident cardiovascular events. JAMA. 2014;311:271–8.
Gonçalves FB, Voûte MT, Hoeks SE, Chonchol MB, Boersma EE, Stolker RJ et al. Calcification of the abdominal aorta as an independent predictor of cardiovascular events: a meta-analysis. Heart 2012;98:988–94.
Buijs RVC, Leemans EL, Greuter M, Tielliu IFJ, Zeebregts CJ, Willems TP. Quantification of abdominal aortic calcification: inherent measurement errors in current computed tomography imaging. PLoS ONE. 2018;13:e0193419.
Pickhardt PJ, Graffy PM, Zea R, Lee SJ, Liu J, Sandfort V et al. Automated CT biomarkers for opportunistic prediction of future cardiovascular events and mortality in an asymptomatic screening population: a retrospective cohort study. Lancet Digit Health. 2020;2:e192-200.
Bartstra JW, Mali WPTM, Spiering W, de Jong PA. Abdominal aortic calcification: from ancient friend to modern foe. Eur J Prev Cardiol. 2021;28:1386–91.
Summers RM, Elton DC, Lee S, Zhu Y, Liu J, Bagheri M et al. Atherosclerotic plaque burden on abdominal CT: automated assessment with deep learning on noncontrast and contrast-enhanced scans. Acad Radiol. 2021;28:1491–9.
Horbal SR, Rossman AH, Brown E, Shah NV, Ross BE, Bidulescu A et al. Morphomic calcification score from clinical CT scans: a proxy for coronary artery calcium. Clin Imaging. 2020;66:57–63.
Leow K, Szulc P, Schousboe JT, Kiel DP, Teixeira-Pinto A, Shaikh H et al. Prognostic value of abdominal aortic calcification: a systematic review and meta-analysis of observational studies. J Am Heart Assoc. 2021;10:e017205.
Kälsch H, Lehmann N, Möhlenkamp S, Hammer C, Mahabadi AA, Moebus S et al. Prevalence of thoracic aortic calcification and its relationship to cardiovascular risk factors and coronary calcification in an unselected population-based cohort: the Heinz Nixdorf Recall Study. Int J Cardiovasc Imaging. 2013;29:207–16.
Horbal SR, Derstine BA, Brown E, Su GL, Wang SC, Holcombe SA. Reference distributions of aortic calcification and association with Framingham risk score. Sci Rep. 2023;13:9421.
Holcombe SA, Horbal SR, Ross BE, Brown E, Derstine BA, Wang SC. Variation in aorta attenuation in contrast-enhanced CT and its implications for calcification thresholds. PLoS ONE. 2022;17:e0277111.
Horbal SR, Brown E, Derstine BA, Zhang P, Bidulescu A, Sullivan JA et al. A correction score to compare aortic calcification in contrast enhanced and non-contrast measurements from computed tomography scans. Clin Imaging. 2021;83:51–5.
Cheng ML, Nakib D, Perciani CT, MacParland SA. The immune niche of the liver. Clin Sci Lond Engl 1979. 2021;135:2445–66.
Kalra A, Yetiskul E, Wehrle CJ, Tuma F. Physiology, Liver. StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. http://www.ncbi.nlm.nih.gov/books/NBK535438/
Soppert J, Lehrke M, Marx N, Jankowski J, Noels H. Lipoproteins and lipids in cardiovascular disease: from mechanistic insights to therapeutic targeting. Adv Drug Deliv Rev. 2020;159:4–33.
Leong Darryl P, Joseph Philip G, McKee martin, Anand Sonia S, TeoKoon K, Schwalm Jon-David et al. Reducing the global burden of cardiovascular disease. Circ Res. 2017;121:695–710.
Bhat N, Mani A. Dysregulation of lipid and glucose metabolism in nonalcoholic fatty liver disease. Nutrients. 2023;15:2323.
Nagarajan SR, Cross E, Sanna F, Hodson L. Dysregulation of hepatic metabolism with obesity: factors influencing glucose and lipid metabolism. Proc Nutr Soc. 2022;81:1–11.
Muzica CM, Sfarti C, Trifan A et al. Nonalcoholic fatty liver disease and type 2 diabetes mellitus: a bidirectional relationship. Can J Gastroenterol Hepatol. 2020;2020:6638306.
Kasper P, Martin A, Lang S et al. NAFLD and cardiovascular diseases: a clinical review. Clin Res Cardiol. 2021;110:921–37.
Stahl EP, Dhindsa DS, Lee SK, Sandesara PB, Chalasani NP, Sperling LS. Nonalcoholic fatty liver disease and the heart: JACC state-of-the-art review. J Am Coll Cardiol. 2019;73:948–63.
Adinolfi LE, Zampino R, Restivo L, Lonardo A, Guerrera B, Marrone A et al. Chronic hepatitis C virus infection and atherosclerosis: Clinical impact and mechanisms. World J Gastroenterol WJG. 2014;20:3410–7.
Backus LI, Boothroyd DB, Phillips BR, Belperio P, Halloran J, Mole LA. A sustained virologic response reduces risk of all-cause mortality in patients with hepatitis C. Clin Gastroenterol Hepatol. 2011;9:509-516.e1.
Mostafa A, Mohamed MK, Saeed M et al. Hepatitis C infection and clearance: impact on atherosclerosis and cardiometabolic risk factors. Gut. 2010;59:1135–40.
Su GL, Zhang P, Belancourt PX, Youles B, Enchakalody B, Perumalswami P et al. Incorporation of quantitative imaging data using artificial intelligence improves risk prediction in veterans with liver disease. Hepatol Baltim Md. 2023. https://doi.org/10.1097/HEP.0000000000000750.
Health Services Research & Development. Corporate Data Warehouse (CDW) [Internet]. 2023 Jan [cited 2023 Jul 6]. https://www.hsrd.research.va.gov/for_researchers/cdw.cfm
Goldberg D, Lewis J, Halpern S, Weiner M, Lo Re V. Validation of three coding algorithms to identify patients with end-stage liver disease in an administrative database. Pharmacoepidemiol Drug Saf. 2012;21:765–9.
Englesbe MJ, Lee JS, He K et al. Analytic morphomics, core muscle size, and surgical outcomes. Ann Surg. 2012;256:255–61.
Graffy PM, Sandfort V, Summers RM, Pickhardt PJ. Automated liver fat quantification at nonenhanced abdominal CT for population-based steatosis assessment. Radiology. 2019;293:334–42.
R Core Team,. R: A Language and Environment for Statistical Computing. 2013Available from: http://www.R-project.org/
Wickham H. ggplot2: Elegant Graphics for Data Analysis. New York: Springer; 2016.
Zhou Y-Y, Zhou X-D, Wu S-J et al. Nonalcoholic fatty liver disease contributes to subclinical atherosclerosis: a systematic review and meta-analysis. Hepatol Commun. 2018;2:376–92.
Mantovani A, Ballestri S, Lonardo A, Targher G. Cardiovascular disease and myocardial abnormalities in nonalcoholic fatty liver disease. Dig Dis Sci. 2016;61:1246–67. https://doi.org/10.1007/s10620-016-4040-6
Jaruvongvanich V, Wirunsawanya K, Sanguankeo A, Upala S. Nonalcoholic fatty liver disease is associated with coronary artery calcification: a systematic review and meta-analysis. Dig Liver Dis. 2016;48:1410–7.
Oni ET, Agatston AS, Blaha MJ et al. A systematic review: burden and severity of subclinical cardiovascular disease among those with nonalcoholic fatty liver; should we care? Atherosclerosis. 2013;230:258–67.
Laurain A, Rubera I, Razzouk-Cadet M et al. Arterial calcifications in patients with liver cirrhosis are linked to hepatic deficiency of pyrophosphate production restored by liver transplantation. Biomedicines. 2022;10:1496.
Dogan S, Celikbilek M, Yilmaz YK et al. Association between liver fibrosis and coronary heart disease risk in patients with nonalcoholic fatty liver disease. Eur J Gastroenterol Hepatol. 2015;27:298–304.
Ishiba H, Sumida Y, Kataoka S et al. Association of coronary artery calcification with liver fibrosis in Japanese patients with non-alcoholic fatty liver disease. Hepatol Res. 2016;46:1107–17.
You SC, Kim KJ, Kim SU et al. Hepatic fibrosis assessed using transient elastography independently associated with coronary artery calcification. J Gastroenterol Hepatol. 2015;30:1536–42.
Kazankov K, Munk K, Øvrehus KA et al. High burden of coronary atherosclerosis in patients with cirrhosis. Eur J Clin Invest. 2017;47:565–73.
Sørensen HT, Thulstrup AM, Mellemkjar L et al. Long-term survival and cause-specific mortality in patients with cirrhosis of the liver: a nationwide cohort study in Denmark. J Clin Epidemiol. 2003;56:88–93.
Jepsen P, Vilstrup H, Lash TL. Development and validation of a comorbidity scoring system for patients with cirrhosis. Gastroenterology. 2014;146:147–56.
Durham AL, Speer MY, Scatena M, Giachelli CM, Shanahan CM. Role of smooth muscle cells in vascular calcification: implications in atherosclerosis and arterial stiffness. Cardiovasc Res. 2018;114:590–600.
Parola M, Pinzani M. Liver fibrosis: pathophysiology, pathogenetic targets and clinical issues. Mol Aspects Med. 2019;65:37–55.
Doherty TM, Fitzpatrick LA, Inoue D et al. Molecular, endocrine, and genetic mechanisms of arterial calcification. Endocr Rev. 2004;25:629–72.
Abedin M, Tintut Y, Demer LL. Vascular calcification. Arterioscler Thromb Vasc Biol. 2004;24:1161–70.
Orriss IR, Arnett TR, Russell RGG. Pyrophosphate: a key inhibitor of mineralisation. Curr Opin Pharmacol. 2016;28:57–68.
Ralph D, van de Wetering K, Uitto J, Li Q. Inorganic pyrophosphate deficiency syndromes and potential treatments for pathologic tissue calcification. Am J Pathol. 2022;192:762–70.
Chang Y, Ryu S, Sung K-C et al. Alcoholic and non-alcoholic fatty liver disease and associations with coronary artery calcification: evidence from the Kangbuk Samsung Health Study. Gut. 2019;68:1667–75.
Steinkohl F, Barbieri F, Senoner T et al. Coronary atherosclerosis profile in patients with end-stage liver disease prior to liver transplantation due to alcoholic fatty liver: a coronary CTA study. Eur Radiol. 2021;31:494–503.
Wild SH, Walker JJ, Morling JR et al. Cardiovascular disease, cancer, and mortality among people with type 2 diabetes and alcoholic or nonalcoholic fatty liver disease hospital admission. Diabetes Care. 2017;41:341–7.
Kim HJ, Kim JH, Choe WH, Kwon SY, Lee CH. Alcoholic fatty liver disease elevates estimated coronary heart disease risk to levels comparable with those of nonalcoholic fatty liver disease in the Korean population: a cross-sectional study. Clin Mol Hepatol. 2014;20:154–61.
Olubamwo OO, Aregbesola AO, Miettola J, Kauhanen J, Tuomainen T-P. Hepatitis C and risk of coronary atherosclerosis—a systematic review. Public Health. 2016;138:12–25.
Broker M, Frager SZ, Patel NS, Lebovics E, Frishman WH. The inflammatory relationship between hepatitis C virus with coronary and carotid atherosclerosis. Cardiol Rev. 2021;29:178–83.
Lee M-H, Yang H-I, Lu S-N et al. Chronic hepatitis C virus infection increases mortality from hepatic and extrahepatic diseases: a community-based long-term prospective study. J Infect Dis. 2012;206:469–77.
Lee M-H, Yang H-I, Wang C-H et al. Hepatitis C virus infection and increased risk of cerebrovascular disease. Stroke. 2010;41:2894–900.
HeHuang, Kang R, Zhao Z. Hepatitis C virus infection and risk of stroke: a systematic review and meta-analysis. PLoS ONE. 2013;8:e81305.
Petta S, Macaluso FS, Craxì A. Cardiovascular diseases and HCV infection: a simple association or more? Gut. 2014;63:369–75.
Negro F, Alaei M. Hepatitis C virus and type 2 diabetes. World J Gastroenterol WJG. 2009;15:1537–47.
Petta S, Cammà C, Di Marco V et al. Insulin resistance and diabetes increase fibrosis in the liver of patients with genotype 1 HCV infection. Am J Gastroenterol. 2008;103:1136–44.
Petta S, Amato M, Cabibi D et al. Visceral adiposity index is associated with histological findings and high viral load in patients with chronic hepatitis C due to genotype 1. Hepatol Baltim Md. 2010;52:1543–52.
Bellinge JW, Dalgaard F, Murray K et al. Vitamin K intake and atherosclerotic cardiovascular disease in the Danish diet cancer and health study. J Am Heart Assoc. 2021;10:e020551.
Chen H-G, Sheng L-T, Zhang Y-B et al. Association of vitamin K with cardiovascular events and all-cause mortality: a systematic review and meta-analysis. Eur J Nutr. 2019;58:2191–205.
van Ballegooijen AJ, Beulens JW. The role of vitamin K status in cardiovascular health: evidence from observational and clinical studies. Curr Nutr Rep. 2017;6:197–205.
Bleizgys A. Zinc, magnesium and vitamin K supplementation in vitamin D deficiency: pathophysiological background and implications for clinical practice. Nutrients. 2024;16:834.
Dowd P, Ham SW, Naganathan S, Hershline R. The mechanism of action of vitamin K. Annu Rev Nutr. 1995;15:419–40.
Ferland G. The discovery of vitamin K and its clinical applications. Ann Nutr Metab. 2012;61:213–8.
Wang X, Zhang W, Huang J, Li H, Gao J. The relationship between vitamin K and metabolic dysfunction-associated fatty liver disease among the United States population: National Health and Nutrition Examination Survey 2017–2018. Front Nutr. 2023;10:1086477.
Smith CB, Hennessey EK, Crossey CD, Crannage AJ. Impact of vitamin K administration on elevated international normalized ratio in chronic liver disease. Clin Appl Thromb. 2023;29:10760296231164642.
Schurgers LJ, Barreto DV, Barreto FC et al. The circulating inactive form of matrix gla protein is a surrogate marker for vascular calcification in chronic kidney disease: a preliminary report. Clin J Am Soc Nephrol CJASN. 2010;5:568–75.
Rahman EU, Chobufo MD, Farah F et al. Prevalence and risk factors for the development of abdominal aortic calcification among the US population: NHANES study. Arch Med Sci Atheroscler Dis. 2021;6:e95-101.
Hoffman DJ, Wang Z, Gallagher D, Heymsfield SB. Comparison of visceral adipose tissue mass in adult African Americans and whites. Obes Res. 2005;13:66–74.
O’Connor SD, Graffy PM, Zea R, Pickhardt PJ. Does nonenhanced CT-based quantification of abdominal aortic calcification outperform the framingham risk score in predicting cardiovascular events in asymptomatic adults? Radiology. 2019;290:108–15.
van der Meer IM, Bots ML, Hofman A, Iglesias del Sol A, van der Kuip DAM, Witteman JCM. Predictive value of noninvasive measures of atherosclerosis for incident myocardial infarction. Circulation. 2004;109:1089–94.
Levitzky YS, Cupples LA, Murabito JM et al. Prediction of intermittent claudication, ischemic stroke, and other cardiovascular disease by detection of abdominal aortic calcific deposits by plain lumbar radiographs. Am J Cardiol. 2008;101:326–31.
Chen H-C, Wang W-T, Hsi C-N et al. Abdominal aortic calcification score can predict future coronary artery disease in hemodialysis patients: a 5-year prospective cohort study. BMC Nephrol. 2018;19:313.
Bendix EF, Johansen E, Ringgaard T, Wolder M, Starup-Linde J. Diabetes and abdominal aortic calcification—a systematic review. Curr Osteoporos Rep. 2018;16:42–57.
Beste LA, Leipertz SL, Green PK, Dominitz JA, Ross D, Ioannou GN. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US veterans, 2001–2013. Gastroenterology. 2015;149:1471–1482.
Funding
No specific funding mechanism supported the work presented in this article.
Author information
Authors and Affiliations
Contributions
Conceptualization SRH, AES, SCW, GLS; Methodology PXB, SRH, PZ, SAH; Formal Analysis and Investigation SRH, PXB, PZ, GLS; Writing—original draft preparation SRH; Writing—review and editing SRH, PXB, PZ, SAH, SS, SCW, AES, SCW, GLS; Resources: PXB, SAH, SS, SCW, GLS. All authors commented, reviewed, and provided impactful edits to the manuscript.
Corresponding author
Ethics declarations
Competing interests
Authors declare no potential conflicts of interest.
Ethical approval
This study was approved by the Institutional Review Boards at VA Ann Arbor Healthcare System Research’s (IRB-2018-1136) and the University of Michigan (HUM-0028846).
Consent for publication
All authors have read this manuscript and consented for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Horbal, S.R., Belancourt, P.X., Zhang, P. et al. Independent Associations of Aortic Calcification with Cirrhosis and Liver Related Mortality in Veterans with Chronic Liver Disease. Dig Dis Sci 69, 2681–2690 (2024). https://doi.org/10.1007/s10620-024-08450-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-024-08450-5