Abstract
Background
Insights into (poly)phenol exposure represent a modifiable factor that may modulate inflammation in chronic pancreatitis (CP), yet intake is poorly characterized and methods for assessment are underdeveloped.
Aims
The aims are to develop and test a method for estimating (poly)phenol intake from a 90-day food frequency questionnaire (FFQ) using the Phenol-Explorer database and determine associations with dietary patterns in CP patients versus controls via analysis of previously collected cross-sectional data.
Methods
Fifty-two CP patients and 48 controls were recruited from an ambulatory clinic at a large, academic institution. To assess the feasibility of the proposed methodology for estimating dietary (poly)phenol exposure, a retrospective analysis of FFQ data was completed. Mann–Whitney U tests were used to compare (poly)phenol intake by group; Spearman correlations and multivariable-adjusted log-linear associations were used to compare (poly)phenol intakes with dietary scores within the sample.
Results
Estimation of (poly)phenol intake from FFQs was feasible and produced estimates within a range of intake previously reported. Total (poly)phenol intake was significantly lower in CP vs controls (463 vs. 567mg/1000kcal; p = 0.041). In adjusted analyses, higher total (poly)phenol intake was associated with higher HEI-2015 (r = 0.34, p < 0.001), aMED (r = 0.22, p = 0.007), EDIH (r = 0.29, p < 0.001), and EDIP scores (r = 0.35, p < 0.001), representing higher overall diet quality and lower insulinemic and anti-inflammatory dietary potentials, respectively.
Conclusions
Using enhanced methods to derive total (poly)phenol intake from an FFQ is feasible. Those with CP have lower total (poly)phenol intake and less favorable dietary pattern indices, thus supporting future tailored dietary intervention studies in this population.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic pancreatitis (CP) is a disease characterized by chronic inflammation and irreversible fibrosis of the pancreatic parenchyma. The lifetime prevalence of disease-related complications (e.g., diabetes mellitus, exocrine pancreatic insufficiency, osteopathy) with metabolic and nutritional consequences is extremely high in CP [1,2,3]. Moreover, symptoms, such as abdominal pain and nausea, may further interfere with dietary intake contributing to additional nutritional compromise and potential loss of endocrine and exocrine function requiring medical management and aggressive nutritional interventions [1,2,3,4]. The chronic inflammation and dysfunctional glycemic control present in CP leads to the development and severity of malnutrition often detected in this patient population, contributing to more frequent hospitalizations, increased length of stay, and reduced survival [1,2,3]. With a variety of medical complications such as abdominal pain, diabetes mellitus, and altered bone metabolism, helping patients manage their CP is a significant challenge facing medical and dietetic professionals [1, 2, 5]. Identification of interventions that can be used to reduce inflammation and slow disease progression is needed.
Optimizing dietary intake is believed to be essential to the successful management of CP. Current standard of care includes pancreatic enzyme replacement therapy (PERT), reduction of dietary fat, and elimination of alcohol [1,2,3, 6]. However, these therapies have limited success, and there is a need to enhance medical treatment to reduce the recurring exacerbations in CP that increase severity of malnutrition and the associated sequelae of the disease [1, 2].
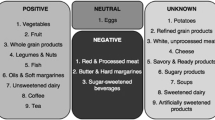
Many studies report that patients with CP have suboptimal dietary intake and poor diet quality [3, 6]. Because of the inflammatory nature of CP [7], understanding characteristics of the diet that may reduce inflammation could provide insight into dietary interventions to reverse or delay CP progression. (Poly)phenols are hypothesized to have anti-inflammatory properties and are abundantly found in plant-derived foods and beverages [8]. Therefore, estimation of dietary (poly)phenol intake in those with CP may provide an opportunity to further understand and modulate food sources of (poly)phenols in the diet with the ultimate goal of reducing inflammation and overall disease progression. However, estimating (poly)phenol intake is difficult, as (poly)phenol content of foods and beverages is not routinely included in food composition databases [9]. Therefore, detailed and improved methods are needed to help clinicians and researchers better assess dietary intake of these bioactive phytochemicals. Replicable methods will allow for comparable data between studies and ultimately aid in elucidating the impact of (poly)phenol-rich foods on chronic inflammatory conditions such as CP.
Food frequency questionnaires (FFQ) are dietary assessment tools that measure habitual intake by querying participants on their typical portion size and frequency of intake of a finite list of foods and beverages over a specific period (e.g., the previous 90 days). FFQs are commonly used in human nutrition studies because they are cost-effective, typically self-administered, and their output can be utilized to quantify usual intake of dietary patterns, foods, nutrients, and bioactives. However, FFQs have been subjected to scrutiny due to the reliance on self-reported estimates of portion sizes. To improve the accuracy of participant responses, FFQs with added food and portion size graphics, graphical FFQs, have been designed to provide a more accurate presentation of portion sizes [10]. Further, computerized versions of graphical FFQs allow for complex skip algorithms to reduce participant burden and remove the risk of missed questions and multiple marks present on paper forms [10].
FFQs are the best dietary assessment tool to measure habitual intake. However, they often group similar foods with a comparable micronutrient and macronutrient profile to minimize participant burden. For example, an FFQ may query participants on frequency of intake of “berries” rather than several questions on individual types of berries. However, when translating FFQ data into intakes of specific dietary components such as (poly)phenols, deconstruction of food group categories into individual foods would improve accuracy of the dietary assessment. Further, mixed dishes with multiple ingredients must be deconstructed into individual ingredients to calculate total (poly)phenol content for the item. Therefore, quantitating (poly)phenol intake from a FFQ requires multiple steps and decisions that must be reported in detail for replication [11].
In the present study, our primary goal was to develop and report in detail methods for derivation of (poly)phenol intake using data collected from a computerized web based graphical FFQ. With this methodology, estimations of habitual (poly)phenol intake and specific (poly)phenol subclasses could be quantified and compared between CP participants and controls. We then determined whether (poly)phenol intake was associated with existing dietary indices that could be targets for improving diet quality in future research. These indices include the Healthy Eating Index (HEI), alternative Mediterranean dietary score (aMED), Empirical Dietary Inflammatory Pattern (EDIP), and Empirical Dietary Index for Hyperinsulinemia (EDIH).
Experimental Methods
Study Design
The current study is a cross-sectional analysis of previously collected data from cases with CP and controls without CP at a large midwestern academic medical center. Data collection included electronic medical record (EMR) review (pancreatic disease characteristics, laboratory parameters, medication use), standard anthropometric measurements, a computerized web-based graphical FFQ with a recall period of 90 days (VioScreen™, Viocare Inc., Princeton, NJ), and a standardized health questionnaire [6]. To assess the feasibility of the proposed methodology for estimating dietary (poly)phenol exposure, a retrospective analysis of FFQ data was completed. This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the Institutional Review Board at the Ohio State University Wexner Medical Center (2020H0287). Written, informed consent was obtained from all subjects/patients. Recruitment and eligibility criteria for the primary analysis have been previously published and include those diagnoses with CP without concurrent gastrointestinal illnesses and were ≥ 18 years of age [6]. The diagnosis of CP was confirmed by a gastroenterologist, using published diagnostic guidelines from the American Pancreatic Association [12].
Derivation of an Enhanced Method to Estimate (Poly)Phenol Intake from FFQ Data (Fig. 1)
To quantitate (poly)phenol intake from FFQ output, a database containing (poly)phenol content in each FFQ item was built in Microsoft Excel. First, a list was compiled of all reported FFQ items which included foods, beverages, mixed dishes (i.e., items with more than 1 ingredient such as “coleslaw” or “pizza”), and all the individual foods included within FFQ groups. Foods of animal origin with presumed negligible (poly)phenol content were removed from the list. Mixed dishes were deconstructed into their single ingredient foods by matching to a US representative recipe in the Food Commodity Intake Database (FCID) that was selected by a registered dietitian nutritionist (RDN), which was accessed electronically (https://fcid.foodrisk.org/recipes/). Then, all items on the list were assigned matches with foods and beverages within the most comprehensive (poly)phenol database, the Phenol-Explorer database (PED, http://phenol-explorer.eu/) version 3.6 [13] while following a previously established series of steps (Fig. 1) [14, 15].
Content values in the PED are estimated using a variety of experimental methods and values to include in the database were chosen based on the appropriate method for the food matrix and/or (poly)phenol subclass following previously published methods [15,16,17]. For our database, (poly)phenol values calculated via chromatography without previous hydrolysis were selected for use. However, there were several exceptions [15,16,17]. For example, chromatography after hydrolysis was used for assessment of lignans in all items, ellagic acid in walnuts, hydroxycinnamic acids in cereal and cereal products, legumes, peanut products, soy and soy products, and olives [15]. Total anthocyanins were determined via pH differential method when available. If pH differential method was not available in the PED, anthocyanin content was calculated as the sum of individual anthocyanins via chromatography without hydrolysis [18]. If this method was unavailable, (poly)phenol content was not calculated. (Poly)phenol values were maintained in their original form for estimation and not translated to aglycone equivalents if presented in conjugate form in the PED, as this is the form they are typically found in nature. Additionally, other research groups commonly report intake values summed without aglycone equivalent translation, which will allow for comparison between cohorts [15, 19,20,21,22,23,24,25,26]. Retention factors were not applied to content values, as it is recommended that retention factors are specific for each food, (poly)phenol, and process, and this is not discernable from FFQs which typically provide data on generic processes (e.g., “cooked”) [27].
The PED content values are reported in mg/100 g fresh weight for foods or mg/100 mL for beverages. The Food Data Central (https://fdc.nal.usda.gov/) database was used to convert (poly)phenol content data in beverages from milliliters to gram weight. To determine (poly)phenol content of each FFQ item, the gram weight was multiplied by the (poly)phenol content in mg/100 g. To calculate total (poly)phenol and subclass (e.g., flavonoid) content values for each FFQ item, individual (poly)phenols were summed.
To determine the (poly)phenol content of an FFQ group of items, the (poly)phenol content of the individual foods comprising the group were calculated from the PED individually. Then, a weighted estimate for each group of foods was calculated using consumption data from the nationally representative 2005–2018 National Health and Nutrition Examination Survey (NHANES) to determine the proportional intakes of each individual food to the total intakes for the FFQ group. Weighted averages were determined using the Individual Foods Files NHANES 2005–2018 for adults over the age of twenty years. The aggregated gram intakes were computed for each unique Food and Nutrient Database for Dietary Studies (FNDDS) food code. The total intake for each individual food item (g) were divided by the intake of the FFQ group (g) to determine the proportional contribution of each food to the group’s (poly)phenol content. (Poly)phenol content values for each food were determined, then weights were applied to estimate the total (poly)phenol content of the FFQ group. For example, in NHANES, strawberries accounted for 58% of the total intakes of berries, and thus the (poly)phenol content of strawberries was used to account for 58% of the total (poly)phenol content for the FFQ group “berries such as strawberries and blueberries.” NHANES data was also utilized to calculate a weighted average for items which had several matches in the PED. However, some items which had detailed varieties in the PED were not differentiated in the NHANES dietary intake data and therefore all varieties from the PED were assumed to have equal contribution to the dietary assessment group. For example, each variety of beer in the PED was assumed to have equal contribution to the FFQ group “beer (all types)” due to the lack of adequate differentiation between beers in the FNDDS (Fig. 1).
In addition to summation of individual (poly)phenol compounds to calculate polyphenol content of FFQ items, a separate analysis was also conducted using PED values measured via the Folin assay. The Folin assay is a spectrophotometric assay used to determine a crude estimate of total phenolic compounds and these data were used to compare with the computed summed values.
All data entered in the database were checked for quality assurance by two research assistants. Participant daily (poly)phenol intake estimations were calculated by summing (poly)phenol content values for all reported FFQ items.
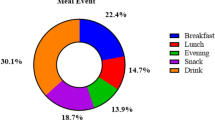
Assessment of Dietary Patterns
Dietary patterns were assessed via two a-priori methods and two empirical hypothesis-oriented approaches. HEI-2015 and the aMED scores were tabulated following previously published methods [6, 28, 29]. The inflammatory and insulinemic potentials of the diet were assessed via EDIP and EDIH scores, respectively [30, 31]. The EDIP score assigns weighted values to daily intakes of different food groups classified as proinflammatory (e.g., processed meat, fish other than dark-meat fish) or anti-inflammatory (e.g., tea, coffee, beer, wine, green-leafy vegetables, pizza), based on plasma CRP, IL6, and TNFα-R concentrations [30]. The EDIH is derived from dietary and biomarker data which weights food groups according to insulinemic potential as defined by fasting plasma C-peptide [31]. In previous studies, both scores were calculated such that higher scores were indicative of more pro-inflammatory or hyperinsulinemic dietary patterns. However, to ease comparisons with HEI-2015 and aMED, the scores were inverted so that higher overall EDIP and EDIH scores represented dietary patterns with more anti-inflammatory or lower insulinemic dietary potential, respectively.
Statistical Analyses
In the present study, median daily total (poly)phenol intake as well as median daily (poly)phenol intake of each of the five (poly)phenol subclasses as identified in the PED were calculated [16, 17]. Intakes of (poly)phenols and (poly)phenol subclasses (expressed as mg per 1000 kcal/day) as well as energy-adjusted dietary index scores (HEI-2015, aMED, EDIH and EDIP) were summarized by medians and interquartile ranges (IQR), and Mann–Whitney U tests were used to compare intakes between CP cases and controls. Foods and food groups contributing to total (poly)phenol intake were summarized as percentages of total (poly)phenol intake in each group. Spearman’s rank correlations were used to determine correlations between (poly)phenol intake and each dietary pattern score among the full cohort. The relationships between (poly)phenol intake and dietary pattern indices were further evaluated using log-linear regression models that adjusted for predefined confounders (diagnosis, age, gender, BMI, and total energy intake). Because of the high contribution of coffee to total (poly)phenol intake, all analyses were conducted both with and without inclusion of coffee. Data were also analyzed to determine the top five food contributors to (poly)phenol intake.
Subgroup analyses were done comparing intake of (poly)phenols and (poly)phenol subclasses between the CP and control groups when stratified by BMI classification (underweight- BMI < 18.5kg/m2, normal weight- BMI ≥ 18.5–24.9 kg/m2, overweight- BMI ≥ 25–29.9 kg/m2, and obese- ≥ 30kg/m2). Analyses were conducted with SAS 9.4 (SAS Institute, Cary, NC).
Results
Study Population
Estimating dietary (poly)phenol intake using the described methodology supports estimates of (poly)phenol intake in other US populations [26]. The study population included 52 cases with CP and 48 controls. As previously described, the mean age was 52 ± 14 years with 67% male [6]. The mean BMI in the CP group was lower than controls, due to the lack of matching for this variable (24 vs. 31 mg/kg2, p < 0.001) [6].
(Poly)Phenol Intake
Estimates of median daily energy-adjusted (poly)phenol intake were significantly lower in the CP cohort compared to controls (Fig. 2). Total (poly)phenol intake remained significantly lower among those with CP when estimates were calculated excluding coffee (Fig. 3). Similarly, the same three (poly)phenol subclasses were found to be suboptimal in those with CP (e.g., flavonoids, stilbenes, and lignans). Further assessment of BMI as a continuous variable and the association with total polyphenol between groups was not significant suggesting BMI is not significantly associated with total polyphenol intake (p = 0.284; supplemental Table 1).
Energy-adjusted total (poly)phenol and (poly)phenol subclass intake between those with (n = 52) and without chronic pancreatitis (n = 48). Diamonds represent means, bars represent medians, boxes represent interquartile ranges that extent to the minimum and maximum, and outliers are represented by circles. *p-value ≤ 0.05; **p-value ≤ 0.01; ***p-value ≤ 0.001; not significant (NS) is defined as p-value > 0.05
Energy-adjusted total (poly)phenol excluding coffee consumption and (poly)phenol subclass intake between those with (n = 52) and without chronic pancreatitis (n = 48). Diamonds represent means, bars represent medians, boxes represent interquartile ranges that extent to the minimum and maximum, and outliers are represented by circles. *p-value ≤ 0.05; **p-value ≤ 0.01; ***p-value ≤ 0.001; not significant (NS) is defined as p-value > 0.05
In addition to total (poly)phenol intake, intake of three of the five (poly)phenol classes was significantly different between groups. The CP group had significantly lower intake of flavonoids, lignans and stilbenes. The Folin assay showed median total (poly)phenol intake per day was nearly 1.7-fold greater than the median calculated from the combination of other analytical methods among all participants (Supplementary Table 2).
“Coffee (not including lattes or mochas)” was the primary contributor to total (poly)phenol and phenolic acid intake in both the CP and control groups (Table 1). Among both groups, tea was the top contributor to flavonoid intake, broccoli was the major contributor to lignan intake, and red wine contributed most to stilbene intake. The top contributor to other (poly)phenol intake in the CP group was pizza, while the primary contributor to other (poly)phenols in the control group was 100% whole grain breads.
Correlation of (Poly)Phenol and Dietary Intake Patterns
Though the mean EDIH score was more than 2.7 times higher in controls compared to CP patients, the difference was not statistically significant. However, the EDIP score was significantly (> 8 times) higher in controls compared to those with CP (p = 0.052) (Table 2). In the overall sample, total (poly)phenol intake was associated with all dietary pattern scores included in the analysis (Table 3). When controlling for age, gender, BMI, and caloric intake, these relationships remained statistically significant (Table 4). While EDIH scores were not statistically significantly different in both groups, a weak positive association was observed between EDIH scores and total (poly)phenol intake in those with CP, but not controls; whereas EDIP scores were significantly different among both groups and weak positive correlations were observed when stratified by disease state (Supplemental Table 3).
Subgroup Analyses
Participants with CP who were categorized as overweight and obese had lower daily intake of total (poly)phenols (excluding (poly)phenols from coffee beverages) than those in the overweight and obese categories in the control group (Table 5). Those with CP who were normal weight also reported lower daily intake of flavonoids and stilbenes (data not shown). Lower intake of lignans were reported among participants with CP categorized as overweight or obese when compared to controls within these BMI categories, and there were no differences when assessed with and without coffee consumption (data not shown).
Discussion
We present an enhanced and feasible method for estimating dietary (poly)phenol intake using a computerized web-based graphical FFQ that can be administered in the clinic and coupled to the PED. Using this methodology, we estimated (poly)phenol intake in CP compared to healthy controls and described the relationship between (poly)phenol intake and common indices used to define dietary quality and patterns of intake and compare these findings between patients with CP and a control sample. Our findings suggest those with CP report lower intake of total (poly)phenols and several subclasses of (poly)phenols when compared to healthy controls, identifying key differences in typical dietary intake that may provide insight into potential targets for those designing (poly)phenol-rich dietary pattern interventions aimed at modulating inflammatory pathways in those with CP [32,33,34]. Additionally, there was a correlation between polyphenol intake and empirical dietary indices that are associated with biomarkers of insulinemic and inflammatory pathways. Collectively, these results identify opportunities for further investigation into dietary interventions that would increase (poly)phenol exposure in CP, which could potentially alter the inflammatory state and disease course. Polyphenol-rich dietary interventions could potentially impact the spectrum of symptoms related to CP without the side effects of pharmacotherapy, though future clinical testing is required. However, we have completed an important step in understanding (poly)phenol intake in this population.
(Poly)phenol intake in a US-based population of patients with CP is lower than controls and thus is associated with an inflammatory dietary pattern. Published data from large epidemiologic cohorts have demonstrated significant variation in (poly)phenol intake, with estimates ranging from 400–1500 mg/day [15, 35]. Some of these differences may be due to the dietary assessment method employed, while others may be directly influenced by cultural differences within each population. Huang et al. estimated (poly)phenol intake at 884 mg per 1000 kcal/day when assessed by 24-h recall in approximately 10,000 U.S. adults in 2013–2016 as part of NHANES [26]. This value is somewhat greater than findings in this study, potentially due to their inclusion of the Folin assay, which likely contributed to overestimation of (poly)phenol intake because the assay is not specific for phenolic compounds [26]. Energy-adjusted total (poly)phenol intake among those with CP may also be lower than Huang et al.’s estimations of the general US population (e.g., 884 mg/day) due to self-restriction of both total energy intake and intake of (poly)phenol-rich foods in order to minimize meal-related gastrointestinal symptoms such as fruits and vegetables which are relatively rich in fiber and (poly)phenols [6, 11, 36, 37]. Energy adjustment of (poly)phenol intake is a superior method of estimating exposure within this population due to the variation in energy intakes observed between those with differing levels of disease severity [38].
Coffee is identified as the major contributor to total (poly)phenol intake in both groups within this study, indicating a potential dietary target to increase (poly)phenol consumption that would be relatively easy to implement in patients who can tolerate coffee intake [24, 35]. In addition, significant differences in intakes of (poly)phenols from the flavonoid, lignan, and stilbene subclasses may relate to the typical food and beverage sources that are uncommon or more difficult to tolerate in CP. Lignans are present in foods such as flaxseeds, legumes, fruits, and vegetables, while stilbenes are predominantly found in wines, berries, and grapes. Fiber content is high in many lignan-rich foods, which may explain the lower intake since dietary fiber has been shown to contribute to an increase in fecal weight and fecal fat and may be self-restricted in CP due to gastrointestinal discomfort [37]. Designing interventions to improve tolerance to these foods may increase intake of these (poly)phenol subclasses while simultaneously improving diet quality. Additionally, though flavonoid intakes appeared to be similar in both groups when coffee beverages were included in dietary estimates, flavonoid intake from other sources was significantly lower in CP, indicating that the high concentration of (poly)phenols in coffee may mask poorer diet quality in relation to dietary flavonoids.
Greater reported intakes of several food groups comprised of (poly)phenol-rich foods, such as whole-grain products, fruits, vegetables, and legumes result in higher HEI and aMED scores [29, 39]. Therefore, the positive correlation between (poly)phenol intake and HEI and aMED scores was expected. Previous research from independent cohorts suggests that those with greater diet quality exhibit higher (poly)phenol intake and higher fiber intake [26, 40, 41]. For the first time, we demonstrate a significant association between the EDIP and EDIH scores with total (poly)phenol intake, indicating that consumption of (poly)phenol-containing foods may directly influence not only diet quality, but measurable biological indicators of dietary inflammatory or insulinemic potential. Together, these results support further investigation of the role of (poly)phenol-rich dietary interventions to modulate inflammation in CP.
Dietary interventions to modulate inflammatory pathways in CP could dramatically alter patient outcomes and lead to a shift in standard of nutrition care within this population. As such, further study of food-based approaches to reduce inflammation are of significant interest to our group and others [22, 42,43,44,45]. To accurately design clinical trials aimed at delivering a (poly)phenol-rich food product, dietary exposure must be quantified and controlled to ensure that interval changes are due to the intervention delivered. Data reported within this CP cohort will therefore inform the development of a low-(poly)phenol control diet tailored to those with CP as constructed in other (poly)phenol-rich food interventions [22, 32, 42,43,44,45]. Perhaps more importantly, the identification of typical (poly)phenol-rich foods sources consumed and tolerated by those with CP will allow researchers to target these foods as well as those that are not regularly consumed to enhance (poly)phenol exposure and improve dietary patterns.
Strengths and Limitations
Calculating (poly)phenol content values for individual FFQ food categories remains a significant challenge, yet the methodological framework employed within this study improves confidence in estimates [20, 46]. The inclusion of mixed dishes, appropriate analytical methods in the PED, and using US dietary data to improve the accuracy of assessments enhance polyphenol assessment from FFQ data. However, limitations of dietary analysis from FFQ may have over- or underestimated serving sizes or excluded foods due to inaccurate recall or individual perception [10, 47]. Validation of this dietary information against diet records would enhance confidence. Furthermore, (poly)phenols were added to the database as presented in the PED and were not converted to their aglycone form, as is published by others in the literature[21, 23, 26, 48]. Therefore, our findings are comparable to many other cohorts that also present (poly)phenol intakes in this fashion [21, 23, 26, 48]. However, the reader should understand that intake values presented for (poly)phenols include the weight of their conjugates for some (poly)phenols. Future work in our group will expand the database to include aglycone equivalents to present intake values in both forms. Lastly, differences in BMI between CP and controls may have influenced analyses, though we accounted for this by adjusting for BMI in the log-linear regression analyses both as a continuous and a categorical variable. Future investigations of larger samples will assist in determining the impact of BMI and other factors such as age, sex, socioeconomic status, and smoking on (poly)phenol estimates and the relationship to dietary pattern indices [49]. Despite these limitations, both groups had intake estimates that are comparable to previously reported populations, increasing confidence in our results [21, 23, 25, 48].
Conclusion
We demonstrated an enhanced method for estimating (poly)phenol intake using an established FFQ. Using this method, we report reduced consumption of total (poly)phenols and several (poly)phenol subclasses in patients with CP. Assessment of the (poly)phenol content and the inflammatory and insulinemic potential of the diet as well as associations between these factors among those with CP may inform the design of future dietary pattern intervention studies in CP. Results will provide evidence that can be used by RDNs to formulate recommendations for specific dietary modifications with the goal of minimizing the inflammatory potential of the diet in CP and other inflammatory conditions [8, 50].
References
Hart PA, Conwell DL. Chronic pancreatitis: managing a difficult disease. Am J Gastroenterol. 2020;115:49–55.
Ramsey ML, Conwell DL, Hart PA. Complications of chronic pancreatitis. Dig Dis Sci. 2017;62:1745–1750.
O’Brien SJ, Omer E. Chronic pancreatitis and nutrition therapy. Nutr Clin Pract. 2019;34:S13–S26.
Gupte A, Goede D, Tuite R, Forsmark CE. Chronic pancreatitis. BMJ. 2018;361:k2126.
Petrov MS, Yadav D. Global epidemiology and holistic prevention of pancreatitis. Nat Rev Gastroenterol Hepatol. 2019;16:175–184.
Roberts KM, Golian P, Nahikian-Nelms M, Hinton A, Madril P, Basch K et al. Does the healthy eating index and Mediterranean diet score identify the nutritional adequacy of dietary patterns in chronic pancreatitis? Dig Dis Sci. 2019;64:2318–2326.
Komar HM, Hart PA, Cruz-Monserrate Z, Conwell DL, Lesinski GB. Local and systemic expression of immunomodulatory factors in chronic pancreatitis. Pancreas. 2017;46:986–993.
Shapiro H, Singer P, Halpern Z, Bruck R. Polyphenols in the treatment of inflammatory bowel disease and acute pancreatitis. Gut. 2007;56:426–435.
Neveu V, Perez-Jimenez J, Vos F, Crespy V, du Chaffaut L, Mennen L et al. Phenol-Explorer: an online comprehensive database on polyphenol contents in foods. Database 2010;2010:bap024.
Kristal AR, Kolar AS, Fisher JL, Plascak JJ, Stumbo PJ, Weiss R et al. Evaluation of web-based, self-administered, graphical food frequency questionnaire. J Acad Nutr Diet. 2014;114:613–621.
Ribichini E, Stigliano S, Rossi S, Zaccari P, Sacchi MC, Bruno G et al. Role of fibre in nutritional management of pancreatic diseases. Nutrients. 2019;11:2219.
Conwell DL, Lee LS, Yadav D, Longnecker DS, Miller FH, Mortele KJ et al. American pancreatic association practice guidelines in chronic pancreatitis: evidence-based report on diagnostic guidelines. Pancreas. 2014;43:1143–1162.
[Cited Jan 1, 2020]. Available from: http://phenol-explorer.eu/.
Kennedy AJ. The Assessment of Polyphenols in Ulcerative Colitis. Columbus: The Ohio State University; 2019.
Zamora-Ros R, Knaze V, Rothwell JA, Hemon B, Moskal A, Overvad K et al. Dietary polyphenol intake in Europe: the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Eur J Nutr. 2016;55:1359–1375.
Knaze V, Rothwell JA, Zamora-Ros R, Moskal A, Kyro C, Jakszyn P et al. A new food-composition database for 437 polyphenols in 19,899 raw and prepared foods used to estimate polyphenol intakes in adults from 10 European countries. Am J Clin Nutr. 2018;108:517–524.
Perez-Jimenez J, Fezeu L, Touvier M, Arnault N, Manach C, Hercberg S et al. Dietary intake of 337 polyphenols in French adults. Am J Clin Nutr. 2011;93:1220–1228.
Plaza M, Domínguez-Rodríguez G, Castro-Puyana M, Marina ML. Polyphenols analysis and related challenges. In: G CM, ed. Elsevier; 2018; 177–232.
Zamora-Ros R, Cayssials V, Jenab M, Rothwell JA, Fedirko V, Aleksandrova K et al. Dietary intake of total polyphenol and polyphenol classes and the risk of colorectal cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Eur J Epidemiol. 2018;33:1063–1075.
Xu Y, Le Sayec M, Roberts C, Hein S, Rodriguez-Mateos A, Gibson R. Dietary assessment methods to estimate (poly)phenol Intake in epidemiological studies: a systematic review. Adv Nutr. 2021;12:1781–1801.
Wang ZJ, Ohnaka K, Morita M, Toyomura K, Kono S, Ueki T et al. Dietary polyphenols and colorectal cancer risk: the Fukuoka colorectal cancer study. World J Gastroenterol. 2013;19:2683–2690.
Vetrani C, Vitale M, Bozzetto L, Della Pepa G, Cocozza S, Costabile G et al. Association between different dietary polyphenol subclasses and the improvement in cardiometabolic risk factors: evidence from a randomized controlled clinical trial. Acta Diabetol. 2018;55:149–153.
Tresserra-Rimbau A, Medina-Remon A, Perez-Jimenez J, Martinez-Gonzalez MA, Covas MI, Corella D et al. Dietary intake and major food sources of polyphenols in a Spanish population at high cardiovascular risk: the PREDIMED study. Nutr Metab Cardiovasc Dis. 2013;23:953–959.
Burkholder-Cooley N, Rajaram S, Haddad E, Fraser GE, Jaceldo-Siegl K. Comparison of polyphenol intakes according to distinct dietary patterns and food sources in the Adventist Health Study-2 cohort. Br J Nutr. 2016;115:2162–2169.
Grosso G, Stepaniak U, Topor-Madry R, Szafraniec K, Pajak A. Estimated dietary intake and major food sources of polyphenols in the Polish arm of the HAPIEE study. Nutrition. 2014;30:1398–1403.
Huang Q, Braffett BH, Simmens SJ, Young HA, Ogden CL. Dietary polyphenol intake in US adults and 10-year trends: 2007–2016. J Acad Nutr Diet. 2020;120:1821–1833.
Rothwell JA, Urpi-Sarda M, Boto-Ordonez M, Llorach R, Farran-Codina A, Barupal DK et al. Systematic analysis of the polyphenol metabolome using the phenol-explorer database. Mol Nutr Food Res. 2016;60:203–211.
Panagiotakos DB, Pitsavos C, Arvaniti F, Stefanadis C. Adherence to the Mediterranean food pattern predicts the prevalence of hypertension, hypercholesterolemia, diabetes and obesity, among healthy adults; the accuracy of the MedDietScore. Prev Med. 2007;44:335–340.
Guenther PM, Reedy J, Krebs-Smith SM. Development of the healthy eating index-2005. J Am Diet Assoc. 2008;108:1896–1901.
Tabung FK, Smith-Warner SA, Chavarro JE, Wu K, Fuchs CS, Hu FB et al. Development and validation of an empirical dietary inflammatory index. J Nutr. 2016;146:1560–1570.
Tabung FK, Wang W, Fung TT, Hu FB, Smith-Warner SA, Chavarro JE et al. Development and validation of empirical indices to assess the insulinaemic potential of diet and lifestyle. Br J Nutr. 2016;116:1787–1798.
Roberts KM, Grainger EM, Thomas-Ahner JM, Hinton A, Gu J, Riedl K et al. Dose-dependent increases in ellagitannin metabolites as biomarkers of intake in humans consuming standardized black raspberry food products designed for clinical trials. Mol Nutr Food Res. 2020;64:e1900800.
Knobloch TJ, Ryan NM, Bruschweiler-Li L, Wang C, Bernier MC, Somogyi A et al. Metabolic regulation of glycolysis and AMP activated protein kinase pathways during Black Raspberry-mediated oral cancer chemoprevention. Metabolites. 2019;9:140.
Gu J, Thomas-Ahner JM, Riedl KM, Bailey MT, Vodovotz Y, Schwartz SJ et al. Dietary Black Raspberries impact the colonic microbiome and phytochemical metabolites in mice. Mol Nutr Food Res. 2019;63:e1800636.
Burkholder-Cooley NM, Rajaram SS, Haddad EH, Oda K, Fraser GE, Jaceldo-Siegl K. Validating polyphenol intake estimates from a food-frequency questionnaire by using repeated 24-h dietary recalls and a unique method-of-triads approach with 2 biomarkers. Am J Clin Nutr. 2017;105:685–694.
Giger U, Stanga Z, DeLegge MH. Management of chronic pancreatitis. Nutr Clin Pract. 2004;19(1):37–49.
Dutta SK, Hlasko J. Dietary fiber in pancreatic disease: effect of high fiber diet on fat malabsorption in pancreatic insufficiency and in vitro study of the interaction of dietary fiber with pancreatic enzymes. Am J Clin Nutr. 1985;41:517–525.
Naska A, Lagiou A, Lagiou P. Dietary assessment methods in epidemiological research: current state of the art and future prospects. F1000Res. 2017;6:926.
Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009;119:1093–1100.
Bakirhan H, Pehlivan M, Uyar Cankay T, Kocak M. Migraine severity, disability, and duration: is a good diet quality, high intake of phytochemicals and polyphenols important? Front Nutr. 2022;9:1041907.
Vitale M, Della Pepa G, Costabile G, Bozzetto L, Cipriano P, Signorini S et al. Association between diet quality and index of non-alcoholic steatohepatitis in a large population of people with type 2 diabetes: data from the TOSCA.IT study. Nutrients. 2022;14:5339.
Roberts KM, Grainger EM, Thomas-Ahner JM, Hinton A, Gu J, Riedl KM et al. Application of a low polyphenol or low ellagitannin dietary intervention and its impact on ellagitannin metabolism in men. Mol Nutr Food Res. 2017. https://doi.org/10.1002/mnfr.201600224.
Ahn-Jarvis J, Lombardo E, Cruz-Monserrate Z, Badi N, Crowe O, Kaul S et al. Reduction of inflammation in chronic pancreatitis using a soy bread intervention: a feasibility study. Pancreatology. 2020;20:852–859.
Stoner GD, Sardo C, Apseloff G, Mullet D, Wargo W, Pound V et al. Pharmacokinetics of anthocyanins and ellagic acid in healthy volunteers fed freeze-dried black raspberries daily for 7 days. J Clin Pharmacol. 2005;45(10):1153–1164.
Gonzalez-Sarrias A, Gimenez-Bastida JA, Garcia-Conesa MT, Gomez-Sanchez MB, Garcia-Talavera NV, Gil-Izquierdo A et al. Occurrence of urolithins, gut microbiota ellagic acid metabolites and proliferation markers expression response in the human prostate gland upon consumption of walnuts and pomegranate juice. Mol Nutr Food Res. 2010;54:311–322.
Hill EB, Kennedy AJ, Roberts KM, Riedl KM, Grainger EM, Clinton SK. Considerations for use of the phenol-explorer database to estimate dietary (poly)phenol Intake. J Acad Nutr Diet. 2021;121:833–834.
Arija V, Abellana R, Ribot B, Ramon JM. Biases and adjustments in nutritional assessments from dietary questionnaires. Nutr Hosp. 2015;31:113–118.
Sohrab G, Hosseinpour-Niazi S, Hejazi J, Yuzbashian E, Mirmiran P, Azizi F. Dietary polyphenols and metabolic syndrome among Iranian adults. Int J Food Sci Nutr. 2013;64:661–667.
Tabung FK, Satija A, Fung TT, Clinton SK, Giovannucci EL. Long-term change in both dietary insulinemic and inflammatory potential is associated with weight gain in adult women and men. J Nutr. 2019;149:804–815.
Verhaegh BP, Reijven PL, Prins MH, Brouns JH, Masclee AA, Keulemans YC. Nutritional status in patients with chronic pancreatitis. Eur J Clin Nutr. 2013;67:1271–1276.
Acknowledgments
Liya Swaminathan and Gretchen Murray are thanked for their support in the quality assurance and checking of data. Additionally, Andrew Siprelle and Amber DeLozier are thanked for their recommendations in spreadsheet development and technology.
Funding
The project described was supported by Award Number UL1TR001070 from the National Center for Advancing Translational Sciences and TL1TR002735 from the Center for Clinical and Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
KS wrote the first draft and developed (poly)phenol intake calculation methodology. PM, MNN, KMR, and PH collected all original data. AH completed all statistical analyses. KS, AK, EH, EG, and KMR developed methodology for food frequency questionnaire (poly)phenol estimates. PM, PH, MNN and KMR designed the original clinical trial. FKT and NS developed the methodology for EDIP and EDIH scores. CT calculated weighted food intakes according to FNDDS data. All authors reviewed and commented on the final draft of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
PM is a consultant for Viocare™. KMR and EG have an invention disclosure for a software invention that The Ohio State University is protecting with a copyright.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Emily B. Hill is now a post-doctoral researcher at University of Colorado Anschutz Medical Campus.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Siprelle, K., Kennedy, A.J., Hill, E.B. et al. An Improved Assessment Method to Estimate (Poly)phenol Intake in Adults with Chronic Pancreatitis. Dig Dis Sci 69, 2996–3007 (2024). https://doi.org/10.1007/s10620-024-08417-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-024-08417-6