Abstract
Background
It is projected that the elderly population will continue to increase. Many will develop chronic conditions such as dementia.
Aims
Our aims are to describe the utilization of colonoscopy among patients with dementia and compare outcomes in those with and without dementia.
Methods
This population-based analysis utilized the National Inpatient Sample (NIS) during 2019. Patients with dementia over the age of 60 years receiving colonoscopy were identified utilizing ICD-10 codes. Logistic regression was used for propensity score matching between the comparison groups. A Greedy one-to-one matching algorithm was utilized along with standardized mean differences to assess balance. Mcnemar test, signed rank sum, and paired t-test were used to compare the outcomes.
Results
Initially, 50,692 patients without dementia were compared with 4323 patients with dementia. Patients with dementia were more likely to be female, older, less likely White, had lower income, and more likely to be on Medicare. In the matched comparison (4176 in each group), complication analysis showed that patients with dementia did not have higher colonoscopy-related complications. They did have higher rates of other complications including renal/AKI (p = 0.0042), pulmonary/pneumonia (p = 0.003), cerebrovascular accidents (p = 0.0063), and sepsis (< 0.0001). Patients with dementia were also less likely to have routine discharges (< 0.0001), had longer hospital stays (< 0.0001), and higher hospital costs (< 0.0001).
Conclusions
Elderly patients with dementia have similar colonoscopy-related complications as patients without dementia. However, they do have higher complications in general. The decision whether to perform colonoscopy in this patient population is multifactorial. A careful assessment of a dementia patient’s history can help with this decision.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Colonoscopy is a common procedure used both diagnostically for colon cancer screening and therapeutically for acute gastrointestinal bleeding. Though generally considered safe, as with any invasive procedure, complications of bowel preparation, the procedure itself, and the sedation do occur and are all increased in older patients. Therefore, patient selection is particularly important taking into account potential benefits, risk factors, and patient preference.
Dementia describes a clinical syndrome that includes cognitive decline with resulting reduction in functional status. Specific pathologies include Alzheimer’s disease, Lewy Body, and vascular dementia. Manifestations and outcomes vary depending on the diagnosis and patients with dementia can represent a challenging patient population [1]. Hospitalized elderly patients with dementia have higher financial burden than those without dementia [2, 3]. As hospital charges soar in this population, it becomes even more prudent to investigate the clinical tendencies, outcomes, and predictors of various procedures for inpatients. For common gastroenterology procedures, besides the direct risks of the procedure itself and the associated anesthesia, risks can go beyond that in the dementia population. With regard to colonoscopy specifically, previous research has shown that dementia is associated with less likelihood to utilize colorectal cancer screening, less likelihood to know that Medicare covers it, missed colonoscopy appointments, and suboptimal bowl preparation [4, 5].
Previous studies in hospitalized patients with dementia have generally demonstrated worse outcomes. In a study by Ijaz et al., patients with dementia admitted for heart failure or acute myocardial infarction were found to have significantly higher inpatient mortality and longer hospital lengths of stay (LOS) [6]. Similarly, Baral et al. found that patients with atrial fibrillation and dementia had greater risk of in-hospital mortality while also lower likelihood of undergoing cardiac procedures [7]. With regard to discharge disposition, patients with dementia also appear to fare worse. Lin et al. utilized a national database to evaluate for several common admission diagnoses and found patients with dementia with enteritis, gastrointestinal (GI) bleed, congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), pneumonia, and arrhythmia were less likely to be discharged to home [8]. Gastrointestinal bleeding patients specifically had an 82% reduction in likelihood in home discharge (aOR 0.18, 95% CI 0.18–0.19). This is compounded by the fact that the elderly and those with dementia face an increased risk of both upper and lower gastrointestinal disorders [3].
With the increasing age of the population, gastroenterologists increasingly face the challenges of performing procedures in patients with dementia [3]. Specifically, gastroenterologists are often plagued with the dilemma of whether or not to perform colonoscopy in this patient population. However, research on performing this common procedure in the inpatient setting is lacking, and more evidence is necessary to guide clinicians performing it. In this study, we evaluate the outcomes of patients diagnosed with dementia undergoing colonoscopy in the inpatient setting utilizing the National Inpatient Sample (NIS), the largest all-payer database of inpatient care publicly available in the United States. In addition to contributing to the already existing body of knowledge on hospitalized patients with dementia, this study will assist with clinical decision-making on those who may need a colonoscopy. We hypothesize that patients with dementia will serve as a challenge for the gastroenterologist performing this procedure because of higher likelihood of worse clinical outcomes. We will identify a potential problem in elderly patients and find ways toward better outcomes in this population.
Methods
This study utilized the Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample (NIS) during the year 2019. This database is sponsored by the Agency for Healthcare Research and Quality (AHQR). The NIS is the largest all-payer database of hospitalized patients in the United States with a large sample size allowing ideal analysis of association and comparisons between various conditions and procedures. This study was approved by the Cleveland Clinic Institutional Review Board (IRB) as an exempt study.
Patients aged ≥ 60 years who had received a colonoscopy identified via International Classification of Diseases, tenth edition, clinical modification (ICD-10-CM) procedure codes were included in the study. The following ICD-10-CM codes were used for colonoscopy: 0DJD8ZZ, 0DJD3ZZ, 0DJD4ZZ, 0DJD7ZZ, 0DJD8ZZ, 0DBE8ZX, 0DBF8ZX, 0DBG8ZX, 0DBH8ZX, 0DBK8ZX, 0DBL8ZX, 0DBM8ZX, and 0DBN8ZX. The presence of dementia as a comorbidity (along with other identifiable comorbidities) was identified using Elixhauser Comorbidity Software administered by AHRQ.
Patient and hospital characteristics were collected for each hospitalization. Hospitalizations records were divided into 2 groups: elderly patients (i.e., ≥ 60 years) without dementia and elderly patients with dementia. Demographic and clinical data were compared between the 2 groups. Factors and variables analyzed included sex, race, type of insurance coverage, hospital type, discharge disposition, length of stay, mortality, and comorbidities (see Table 1, 2, 3, 4).
Categorical variables are described by frequencies and percentages. Continuous measures are described by means and standard deviations or medians and interquartile range as appropriate depending on their distribution. In terms of group matching, propensity score matching was used to correct for effects of the uneven features of the clinical outcomes between those with dementia versus without dementia. Logistic regression model was used to estimate propensity scores. Greedy one-to-one algorithm was used where each patient in the dementia group was matched to a patient in the non-dementia group with the closest propensity score. Baseline variables considered to be potentially associated with dementia diagnosis and outcomes of interest were included in the propensity score model, including demographics, comorbidities, and hospital characteristics as listed in Table 1. Standardized mean differences were used to assess the balance of characteristics post-matching with a standardized mean difference less than 0.1 considered to represent covariate balance. To compare the outcomes between matched groups, dependent sample statistical methods were used: McNemar test for categorical variables and a signed rank sum test or paired t-tests for continuous variables. Multivariable regression analyses were used to assess the effect of patient factors –age, sex, race/ethnicity, hospital region, and status on length of stay, type of discharge, and hospital charges. All tests were 2-sided. A p < 0.05 was considered statistically significant. Analyses were performed using SAS Software (Version 9.4, Cary, NC).
Results
A total of 55,015 elderly patients over the age of 60 years who underwent colonoscopy in 2019 were included. Of these, 4323 had a diagnosis of dementia and 50,692 did not have a diagnosis of dementia (Table 1). The mean age of the dementia cohort was 80.08 years and those without dementia was 73.69 years.
Females made up 59.6% of those with dementia and 53.9% of those without dementia. Whites made up 67.1% of those with dementia and 72.6% of those without dementia. Blacks with dementia were more likely to receive a colonoscopy than those without (18.3% vs. 14.3%). Obese patients with dementia (9.23%) had a lower percentage of colonoscopy versus those without dementia (16.6%). In terms of urgency of the procedure, those with dementia (95.39%) were more likely to have received a colonoscopy on an emergent basis than those without dementia (87.7%); conversely, there was a higher likelihood of receiving a colonoscopy on an elective basis in those without dementia (12.3% vs 4.61%). There was a lower likelihood for those with private insurance and with dementia (4.8%) to receive colonoscopy compared to those without dementia (13.6%) and same insurance. Correspondingly, a patient who is on Medicare and has dementia (91.2%) is more likely to get a colonoscopy than a patient without dementia on Medicare (78.9%).
In our cohort of elderly patients aged over 60 years, colonoscopy-related complications—colon perforations, bleeding, and splenic injury—occurred at about the same rate in the dementia versus the non-dementia comparison (Table 2). Non-procedure-related complications, however, were more common in patients with dementia compared to those without dementia including renal and/or acute kidney injury, pulmonary and/or pneumonia, cerebrovascular accident (CVA), and sepsis (all with significant p-values, p < 0.05).
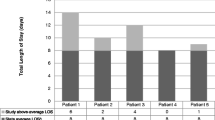
Patients with dementia versus non-dementia groups (Table 3) showed a significant increase in length of stay (LOS) and hospital charges. For instance, 28.1% of those with dementia had a routine discharge while 54.7% had such a discharge in those without dementia (p < 0.001). Those with dementia had a prolonged LOS when compared to those without dementia (6 days vs. 5 days, p < 0.0001). Finally, those with dementia incurred higher hospital charges with an estimated cost of $55,808 vs. $47,912 (p < 0.0001). No significant difference in in-hospital mortality was appreciated between the groups.
On multivariable regression (Table 4), patients with dementia were 69% less likely to have had a routine discharge as compared to non-dementia patients (OR 0.31, 95% CI [0.28–0.34]). Table 4 also indicates that when compared with those on private insurance, Medicare and Medicaid patients were less likely to have a routine discharge (OR 0.70, 95% CI [0.56–0.87] and OR 0.67, 95% CI [0.46–0.97], respectively). Medicaid patients were also more likely to have a longer LOS (RR 1.23, 99% CI [1.04–1.42]). Other pertinent findings included lower costs at rural hospitals (vs. teaching hospitals, RR 0.77, 95% CI [0.73–0.81]), lower likelihood of routine discharge at hospitals in the Northeast region (34% less likely than West coast hospital, OR 0.76, 95% CI[0.65–0.89])), but significantly lower charges (RR 0.77, 95% CI [0.70–0.83]). Southern states and Midwest states also had significantly less hospital charges than West coast hospitals (RR 0.59, 95% CI [0.55–0.65]) and RR 0.74, 95% CI [0.69–0.81], respectively).
Tables 5 and 6 summarize our literature review with regard to national studies analyzing dementia comorbidity on outcomes of various medical conditions and procedures [2, 6, 8,9,10,11,12,13,14,15,16,17] and with regard to its impacts on GI procedures specifically [5, 18,19,20,21,22,23,24].
Discussion
Utilizing the NIS database, we found 55,015 inpatient colonoscopies were performed in elderly patients over the age of 60 years, 4,323 of which in dementia patients. Compared to those without dementia, those with dementia receiving colonoscopy were overall older by an average of 7 years, had a higher percentage of females, had proportionately less Whites, were significantly less likely to be obese, less likely to have private insurance, and more likely to receive the procedure emergently. Black patients who have dementia are more likely to receive a colonoscopy than those Black patients without dementia. We found the number of complications from colonoscopy were similar in patients with and without dementia; however, we did note that other non-procedural related complications were higher in those with dementia. Outcomes analysis also indicated that patients with dementia also had worse LOS, charges, and discharge disposition.
This study also raises important questions about informed decision-making as demented patients are less likely to decide on their own and rely on others (family, friends, healthcare power of attorney, etc.) to make decisions on their behalf. Indeed, it is also possible that in such scenarios, the gastroenterologist is faced with the decision to perform the procedure on these patients versus not, and it seems that gastroenterologists in certain cases were more likely to opt for or recommend colonoscopy. For instance, we hypothesize that Black patients without dementia were more likely to decline colonoscopy (as they are likely the primary decision maker) due to certain biases or feelings about the procedure. Similarly, females with dementia probably have the same scenario when it comes to proper informed consent with their next of kin deciding on their behalf to consent for a colonoscopy procedure, as we find a smaller percentage among them without dementia undergoing colonoscopy. Again, the proceduralist/endoscopist decision-making process and/or their biases along with it should be taken into consideration when assessing these findings. Indeed, ethical considerations play an important role in these clinical situations. At the same time, well-balanced decision-making including providing relief for palliative reasons as occurs commonly this patient population is an important factor that proceduralists may contemplate.
The impact of obesity on receiving a colonoscopy is also demonstrated in our study. It is indicative that it influences decision-making by the gastroenterologist whether to perform the procedure or not, with obese patients without dementia being more favored to receive the procedure than those with obesity and dementia. This suggests that increasing comorbidities is a further hindrance on gastroenterologists to perform the procedure. At the same time, it potentially indicates patient preference with more obese patients without dementia opting for colonoscopy. Findings on the effects of insurance status on colonoscopy utilization is indicative that patients with dementia are more likely to get an index colonoscopy during hospitalization if they were on Medicare rather than private insurance when compared to their non-dementia counterparts. The cause for this is likely multifactorial; again, patient factors and physician factors are likely at play including decision-making by both parties, personal biases, and insurance reimbursement considerations.
In terms of specific complications related to colonoscopy, patients with dementia did not incur an increased risk of colonic perforation, post-colonoscopy bleeding, or splenic injury, suggesting that this comorbidity doesn’t result in altered colon anatomy that may put them at risk of such complications. From an endoscopist perspective, it also suggests that performing a colonoscopy on patients with dementia will not put them at a higher risk of procedure-related complications as may occur with other comorbidities. However, other more general complications such as CVA, pneumonia, sepsis, and AKI did occur at a higher rate among the dementia group indicating that proceeding with a colonoscopy in patients with this comorbidity should be done with caution. The overall picture of the patient’s pre-procedure clinical status should be considered including indication of the procedure, patient mental status, other comorbidities, laboratory and imaging findings, and social situation.
We also report significant outcomes regarding discharge disposition, LOS, and hospitalization charges. All these latter outcomes were significantly worse (i.e., less routine discharge, higher LOS, and higher charges) among patients with dementia. This goes along with other previous studies that reported on patients with dementia and its association with a poor prognosis during hospitalization, procedure utilization, and surgical operations. While we find that mortality rate is the same between our comparisons, we are unable to report on longer-term mortality rate following discharge, as these data are not available. We hypothesize that since approximately there was a 2:1 ratio of dementia versus non-dementia patients to have a non-routine discharge (i.e., not to home, and rather to acute rehab facility, skilled nursing facility, etc.), there is a high likelihood that more patients died at outside facilities shortly after the index hospitalization, implying a likely higher mortality among dementia patient than we find in our study. However, other previous studies have reported a similar trend in which there is greater rates of complications, longer lengths of stay, less likelihood of home discharge, and higher medical costs in patients with dementia while the mortality rate is insignificant comparatively [14, 22]. Some have highlighted the higher anesthetic risks in dementia as a possibility; there is a theoretically greater likelihood of post-procedure occurrence of delirium with sedation medications resulting in longer LOS, driving up medical costs [22]. Others also corroborated our findings in terms of procedure urgency with a higher likelihood of emergent/urgent procedures performed on patients with dementia [13].
Our data also suggest disparities based on insurance status, type of hospital, and geography. The finding that patients with private insurance are more likely to have a routine discharge is puzzling and is likely to be multifactorial in nature. Private insurance patients could possibly encounter more difficulties in obtaining authorization to be placed at skilled nursing facilities or acute rehab institutions and more likely settle on being taken care of at home with family members. Also possible, family members of such patients are more likely to provide support to them when compared to patients on Medicare or Medicaid. These patients may have been more likely to refuse placement at such long-term facilities and opted to be discharged home as well. Similar explanations could also account for the higher length of stay in elderly patients on Medicaid. Likely due to less resources and manpower, rural hospitals incurred less charges when compared to teaching hospitals, which have more resources, more likely to be located in urban areas, and more likely to spend on areas such as medical care. Finally, the disparities found based on geography are quite puzzling; these findings should be further investigated in future retrospective or prospective studies.
Other recent studies have also suggested that patients with dementia undergoing procedures have worse outcomes when compared to non-dementia patients. One example of this is demonstrated by Shah et al. when evaluating outcomes after vascular surgery [13]. Their study found patients with dementia to have higher likelihood of 30 and 90-day mortality, longer hospital LOS, and lower likelihood of discharge to home. Similar results in terms of LOS and hospital discharge have also been found in patients with dementia undergoing spine fusion [14]. A study by Beydoun et al. evaluated trends in hospitalized Alzheimer’s patients with dementia among a variety of commonly performed procedures. Notably, in patients undergoing respiratory or GI procedures, grouped together in their analysis, they report increased cost of hospital stay, increased length of stay, and higher mortality risk [11].
Although colonoscopy is generally considered a minor and safe procedure, patient safety and procedure benefit must still be assessed. Two major factors to consider are ability to tolerate bowel prep and risk for adverse outcomes or complications. In the dementia population, there is a paucity of evidence regarding the safety profile of these patients when undergoing colonoscopy. Inadequate bowel preparation can result in colonoscopy cancelation or lead to prolonged procedure time, increased risk for complications, and suboptimal visualization. Several studies demonstrate dementia as being one of the strongest associations of predictors of inadequate bowel preparation for colonoscopy [18, 19, 24]. Patients with cognitive impairment may have significant barriers to completing a bowel preparation regimen, including impaired ability to swallow and intolerance of the large volume of fluid. Given these challenges, some suggest strategies including clear liquids or low-residue diet in the days prior to procedure or even direct administration of preparation through esophagogastroduodenoscope or nasogastric tube [25].
Proper evaluation and consideration of patient fit for colonoscopy is very important, especially given recent population-level and epidemiologic data. In a recent study by Lv and colleagues, colorectal cancer screening utilization in older adults increased from 86.4% to 88.96% from 2015 to 2018; however, those with Alzheimer’s or other related dementias were significantly less likely to undergo screening [5]. On the other hand, a recent study evaluated utilization of colonoscopy during 2018–2019 in screening-eligible patients and found no statistically significant difference in utilization rate between those with cognitive impairment and those without [23]. As colonoscopy is performed more frequently in older patients and in patients with dementia, a comprehensive understanding of patient safety and benefit must be established. Along with the previous findings mentioned, our study will help further develop guidelines, policies, and protocols that will give better solutions to this clinical dilemma. It is hoped that this will provide greater impetus to educate physicians of all specialties on the growing elderly population, particularly with circumstances in which an intervention is contemplated, and for governing bodies to incentivize and fund programs that specialize in the care of the elderly.
While the analysis of NIS data provides a large sample size with ample statistical power, limitations of using such administrative databases exist. The limitations of this database include the inability to assess clinical attributes such as adequacy of bowel preparation, medications used, laboratory findings, long-term follow-up after discharge, and readmissions if they occurred. In addition, the lack of tracking of readmissions means that a particular readmitted patient may be unknowingly counted more than once in the analysis. Also, mortality soon after discharge such as 30-day mortality cannot be assessed and thus patients who were regarded as hospice or with end-of-life care, as happens with increasing age and complex comorbidities, were not reported. Similarly, coexisting polypharmacy and frailty indicators which are common in this patient population were difficult to determine and thus not assessed. The coding used to identify the patients with dementia may underestimate or overestimate the prevalence of dementia as clinicians may underdiagnose some patients while wrongfully designating others as having the condition. Along the same lines, coding errors may and do occur in real-world settings when entering ICD-10 codes in the electronic medical record (EMR). The severity of dementia is unable to be defined or evaluated in this study, which is important since cognitive impairment is diagnosed based on a spectrum of disorders. Thus, determining the degree of dementia severity (for instance, using the Functional Assessment Screening Tool [FAST]) can be crucial to providing proper patient care, making sound decisions on performing procedures, and determination of prognosis. It is also relevant to distinguish between patient preference and family preferences regarding receiving interventions such as colonoscopy, both of which were not retrievable. Reporting of the type of anesthesia used is also a limitation, as this can impact post-procedure delirium and, in return, clinical outcomes. In addition, this study may not be generalizable to younger patients with dementia, as younger patients are less likely to have chronic conditions, have different comorbidities all together, and overall would be expected to be healthier. Particularly, young-onset dementia not only has adult neurodegenerative conditions as etiology, but also late-onset forms of childhood neurodegenerative conditions (mitochondrial disorders, lysosomal storage disease, etc.) and reversible causes as well [26]. On the other hand, our study may be generalizable to other higher-risk populations afflicted by chronic neuropsychiatric conditions such as traumatic brain injury, debilitated cerebrovascular disease, cerebral palsy, Parkinson’s disease, and multiple sclerosis (specifically end-stage).
In this national inpatient study, we found elderly patients with dementia receiving colonoscopy have similar colonoscopy-related complications as patients without dementia. However, patients with dementia do have higher complications in general and they should be aware that kidney injury, pneumonia, CVA, and sepsis can be catastrophic. Major outcomes such as discharge disposition, LOS, and hospital costs were also worse in dementia cohort. We also report on significant interesting findings and implications on demographic, socioeconomic, and hospital-level characteristics among patients with dementia undergoing colonoscopy. Our original hypothesis is therefore supported by these findings, though not to the full extent. Knowledge of the findings identified will allow for more thorough counseling of patients and their families and will enhance readiness for the procedure. Accordingly, as now more than ever gastroenterologists face the challenges of performing procedures on the elderly dementia population, the decision whether to perform colonoscopy in this patient population is multifactorial. A thorough assessment of a dementia patient’s history can help with this decision as well as careful assessment of ethical and palliative measures. The interplay between physician, patient, and family (i.e., healthcare power of attorney, surrogate, etc.) in decision-making is also of significance particularly for suitable patient selection. Future investigations in this area are required given limited data available on this specific patient population, particularly with regard to long-term clinical outcomes, the need to augment their medical care, better elucidate the effect of socioeconomic factors, including palliative and ethical implications.
Data availability
The data utilized in this study is from the National (Nationwide) Inpatient Sample (NIS) developed by the Healthcare Cost and Utilization Project (HCUP): https://hcup-us.ahrq.gov/nisoverview.jsp. The specific data that was extracted and analyzed is provided within the text of the manuscript as well as the provided tables.
References
Gale SA, Acar D, Daffner KR. Dementia. Am J Med. 2018;131:1161–1169.
Anderson TS, Marcantonio ER, McCarthy EP, Herzig SJ. National trends in potentially preventable hospitalizations of older adults with dementia. J Am Geriatr Soc. 2020;68:2240–2248.
Olaiya B, Adler DG. Adverse events after inpatient colonoscopy in octogenarians: results from the national inpatient sample (1998–2013). J Clin Gastroenterol. 2020;54:813–818.
Arias F, Riverso M, Levy SA et al. Pilot study: neurocognitive disorders and colonoscopy in older adults. Anesth Analg. 2019;129:e89–e93.
Lv G, Wang X, Jiang X, Li M, Lu K. Impact of Alzheimer’s disease and related dementias on colorectal cancer screening utilization, knowledge, and associated health disparities. Front Pharmacol. 2022;13:872702.
Ijaz SH, Minhas AMK, Ghoneem A et al. Association of dementia with in-hospital outcomes in primary heart failure and acute myocardial infarction hospitalizations. Prog Cardiovasc Dis. 2022;73:24–31.
Baral N, Mitchell JD, Aggarwal NT et al. Sex-based disparities and in-hospital outcomes of patients hospitalized with atrial fibrillation with and without dementia. Am Heart J Plus 2023;26:100266.
Lin RY, Scanlan BC, Liao W, Nguyen TP. Disproportionate effects of dementia on hospital discharge disposition in common hospitalization categories. J Hosp Med. 2015;10:586–591.
Alshekhlee A, Li CC, Chuang SY et al. Does dementia increase risk of thrombolysis?: a case-control study. Neurology. 2011;76:1575–1580.
Beydoun MA, Gamaldo AA, Beydoun HA et al. Trends, predictors, and outcomes of healthcare resources used in patients hospitalized with Alzheimer’s disease with at least one procedure: the nationwide inpatient sample. J Alzheimers Dis. 2017;57:813–824.
Gupta A, McKeever TM, Hutchinson JP, Bolton CE. Impact of coexisting dementia on inpatient outcomes for patients admitted with a COPD exacerbation. Int J Chron Obstruct Pulmon Dis. 2022;17:535–544.
Lagu T, Zilberberg MD, Tjia J et al. Dementia and outcomes of mechanical ventilation. J Am Geriatr Soc. 2016;64:e63–e66.
Shah SK, Jin G, Reich AJ et al. Dementia is associated with increased mortality and poor patient-centered outcomes after vascular surgery. J Vasc Surg. 2020;71:1685-1690.e2.
Sharma M, Dietz N, Scott V, Wang D, Ugiliweneza B, Boakye M. Trends and outcomes in patients with dementia undergoing spine fusions: a matched nationwide inpatient sample analysis. World Neurosurg. 2023;169:e164–e170.
Sherzai A, Ovbiagele B, Sherzai D. Time trends and characteristics of prevalent dementia among patients hospitalized for stroke in the United States. J Stroke Cerebrovasc Dis. 2018;27:1447–1457.
Sherzai D, Losey T, Vega S, Sherzai A. Seizures and dementia in the elderly: nationwide Inpatient Sample 1999–2008. Epilepsy Behav. 2014;36:53–56.
Sherzai D, Sherzai A, Lui K et al. The association between diabetes and dementia among elderly individuals: a nationwide inpatient sample analysis. J Geriatr Psychiatry Neurol. 2016;29:120–125.
Agrawal R, Majeed M, Attar BM et al. Predictors of poor bowel preparations and colonoscopy cancellations in inpatient colonoscopies, a single center retrospective study. Transl Gastroenterol Hepatol. 2022;7:4.
Gandhi K, Tofani C, Sokach C et al. Patient characteristics associated with quality of colonoscopy preparation: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2018;16:357-369.e10.
Iida T, Kaneto H, Wagatsuma K et al. Efficacy and safety of endoscopic procedures for common bile duct stones in patients aged 85 years or older: a retrospective study. PLoS ONE. 2018;13:e0190665.
Kitagawa K, Mitoro A, Ozutsumi T et al. Comparison of the efficacy and safety between palliative biliary stent placement and duct clearance among elderly patients with choledocholithiasis: a propensity score-matched analysis. BMC Gastroenterol. 2021;21:369.
Murata A, Mayumi T, Muramatsu K, Ohtani M, Matsuda S. Effect of dementia on outcomes of elderly patients with hemorrhagic peptic ulcer disease based on a national administrative database. Aging Clin Exp Res. 2015;27:717–725.
Yang S, Bian J, George TJ et al. The association between cognitive impairment and breast and colorectal cancer screening utilization. BMC Cancer. 2021;21:539.
Yee R, Manoharan S, Hall C, Hayashi A. Optimizing bowel preparation for colonoscopy: what are the predictors of an inadequate preparation? Am J Surg. 2015;209:787–792.
Lim YJ, Hong SJ. What is the best strategy for successful bowel preparation under special conditions? World J Gastroenterol. 2014;20:2741–2745.
Kuruppu DK, Matthews BR. Young-onset dementia. Semin Neurol. 2013;33:365–385.
Acknowledgments
The authors acknowledge that there isn’t any grants or financial support to declare with regard to publication of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Faris Shweikeh and Gordon Hong. The first draft of the manuscript was written by Faris Shweikeh and Gordon Hong and all authors commented on the previous versions of the manuscript. Primary conception and design: Faris Shweikeh. Acquisition of Data: Faris Shweikeh and Gordon Hong. Analysis and interpretation of the data: All authors. Critically revising the article: Anthony Lembo, Matthew Hoscheit, Mohamad Mouchli, and Kathleen Rogers. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest with regard to the publication of this article.
Ethical approval
The authors declare that this research is performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its subsequent amendments. Institutional Review Board (IRB) approval was obtained through the Cleveland Clinic IRB review board, and it was approved with an exempt status.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Results of this study were presented in abstract form at the 2023 Ohio Gastroenterology Society Annual Meeting in Westerville, OH, USA, on September 9th, 2023.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Shweikeh, F., Hong, G., Rogers, K. et al. Colonoscopy Utilization in Elderly Patients with Dementia: Characteristics, Complications, and Charges in a National Matched-Cohort Analysis. Dig Dis Sci 69, 1613–1625 (2024). https://doi.org/10.1007/s10620-024-08363-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-024-08363-3