Abstract
Background
Family history of colorectal cancer (CRC) is used to stratify individuals into risk categories which determine timing of initial screening and ongoing CRC surveillance. Evidence for long-term CRC risk following a normal index colonoscopy in family history populations is limited.
Aims
To assess the incidence of advanced neoplasia and associated risk factors in a population undergoing surveillance colonoscopies due to family history of CRC.
Methods
Surveillance colonoscopy findings were examined in 425 individuals with a family history of CRC, a normal index colonoscopy and a minimum of 10 years of follow-up colonoscopies. Advanced neoplasia risk was determined for three CRC family history categories (near-average, medium and high-risk), accounting for demographics and time after the first colonoscopy.
Results
The median follow-up was 13.5 years (IQR 11.5–16.0), with an incidence of advanced neoplasia of 14.35% (61/425). The number of affected relatives and age of CRC diagnosis in the youngest relative did not predict the risk of advanced neoplasia (p > 0.05), with no significant differences in advanced neoplasia incidence between the family history categories (p = 0.16). Patients ≥ 60 years showed a fourfold (HR 4.14, 95% CI 1.33–12.89) higher advanced neoplasia risk during surveillance than those < 40 years at index colonoscopy. With each subsequent negative colonoscopy, the risk of advanced neoplasia at ongoing surveillance was reduced.
Conclusions
The incidence of advanced neoplasia was low (14.35%), regardless of the family history risk category, with older age being the main risk for advanced neoplasia. Delaying onset of colonoscopy or lengthening surveillance intervals could be a more efficient use of resources in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most commonly diagnosed cancer in Australia, and the second-leading cause of cancer-related death [1]. Colonoscopy can detect and remove adenomatous polyps (the precursor lesions for the majority of CRC), preventing the development of CRC or allowing its detection at an earlier stage [2,3,4,5].
Family history is a risk factor for CRC [6,7,8], with the degree of risk considered to depend on the number of first-degree and second-degree relatives with CRC and the age at which the relative was diagnosed [9,10,11]. The Australian National Health and Medical Research Council (NHMRC) have developed screening guidelines to detect CRC in family history populations, stratified into risk categories in which the likelihood of detecting cancer or preinvasive lesions (advanced adenomas) is enough to justify more frequent surveillance than the average-risk population without a family history of CRC [12]. Table 1 summarizes the family history risk categories, the associated family history characteristics, degree of risk and surveillance recommendations in Australia. Individuals in the ‘near-average’ risk category are considered at or slightly above the average population risk for developing CRC, corresponding to a 5–10% lifetime risk if no screening [12, 13]. Individuals in the ‘moderate risk’ category are approximately 3–6 times the average population risk; a 15–30% lifetime risk [12, 13]. Those in the ‘high-risk’ category are approximately 7–10 times the average CRC risk; a 30–40% lifetime risk [12, 13].
Average-risk individuals with an adenoma detected on index colonoscopy have higher rates of advanced neoplasia (AN; CRC or advanced adenoma) on subsequent surveillance colonoscopy [14, 15]. International evidence has shown that for average-risk individuals, a normal colonoscopy corresponds with a lower lifetime risk of developing CRC [14,15,16,17,18,19,20]. However, evidence is limited for CRC risk following a normal index colonoscopy in individuals who are considered at increased risk from family history.
This study aimed to determine the incidence of AN during surveillance of an Australian cohort with a family history of CRC, where the index colonoscopy had no neoplasia found. We also investigated the risk factors for CRC and pre-invasive lesions in this cohort. In doing so, the study aimed to validate the recommendations related to the need for colonoscopy surveillance with the different family history classifications.
Methods
A retrospective cohort study was employed using data from the Southern Co-operative Program for the Prevention of Colorectal Cancer (SCOOP) database [21], a hospital-based surveillance program whereby individuals with findings of colorectal neoplasia undergo organized colonoscopy surveillance following Australian guidelines [12]. A subset of this program includes those with a family history of CRC, where individuals considered to be at higher-than-average risk were invited to participate in colonoscopy surveillance.
Individuals in the SCOOP program with a family history of CRC, a normal or non-neoplastic finding on index colonoscopy, and at least 10 years of follow-up colonoscopies between the years 2000 (start of the study) -2019 (end of the study) were included. The study considered provisions to censor participants at the occurrence of loss to follow-up, death, or the completion of the study. Procedures were undertaken in public hospitals in South Australia including Flinders Medical Centre (Bedford Park, SA), Repatriation General Hospital (Daw Park, SA) and Noarlunga Hospital (Noarlunga Centre, SA). Colonoscopy dates, indications for colonoscopy, pathology findings, age, gender, CRC family history details (age at diagnosis, degree of kinship, number of affected relatives) and total colonoscopy follow-up time were recorded.
Cases were excluded if there was inadequate family history information to assign to a family history risk category, or if their index or final colonoscopy was of poor quality, incomplete, or with indeterminate pathology. Individuals with inflammatory bowel disease or known genetic cancer syndromes were also excluded. In a subgroup analysis of findings at the first follow-up colonoscopy, individuals with incomplete, poor quality and indeterminant findings on this procedure were excluded from the subgroup analysis, however, subsequent complete colonoscopies were included in the overall analysis.
Individuals were classified into risk categories according to the current NHMRC family history screening guidelines [12] as ‘near-average risk’ (Category 1), ‘moderately increased risk’ (Category 2) or ‘high-risk’ (Category 3) on the basis of their family history demographics (Table 1).
Colonoscopy reports were analysed for histologically confirmed AN, which included adenocarcinoma, advanced adenomas and high-risk sessile serrated lesions. Pathologies were classified with the following hierarchy: colorectal adenocarcinoma, advanced adenoma, non-advanced adenoma, non-neoplastic pathologies, and normal. Advanced adenoma included adenomas with size ≥ 10 mm, > 20% villosity or high-grade dysplasia. Cases with ≥ 5 small tubular adenomas were included as high-risk in keeping with current literature [22,23,24,25]. High-risk sessile serrated lesions (classified as those with size ≥ 10 mm, presence of dysplasia, or with synchronous conventional adenoma) were also included as AN in keeping with current guidelines [26]. Adenomas and sessile serrated lesions which were not classified as advanced were grouped as non-advanced. A normal colonoscopy was defined as a colonoscopy without any neoplastic finding. Non-neoplastic findings included benign polyps (such as hyperplastic polyps), diverticular disease and hemorrhoids.
The data were analysed using Stata 16 (Statacorp LP, College Station, Texas). Descriptive statistics were used to report patients’ demographic and clinical characteristics, and risk of AN were compared between family history risk categories, demographics of participant and family history characteristics using Chi-square, t-test and non-parametric Kruskal–Wallis tests as appropriate. Survival analysis of time-to-event data (time from baseline colonoscopy to AN diagnosis or end of study period) and multivariable logistic regression for binary outcome data were used to investigate AN risk. Hazard ratios (HR) and odds ratio (OR) with corresponding 95% confidence interval (CI) were calculated for AN amongst different demographic (age and gender) and family history risk categories. A P value < 0.05 was considered statistically significant. Ethics approval was obtained through the Southern Adelaide Clinical Human Research Ethics Committee, Reference Number 244.20.
Results
Characteristics of Participants
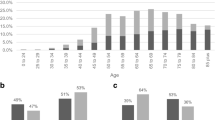
Overall, 425 patients were included in the final analysis (Supplemental Fig. 1); mean age at index colonoscopy was 49.4 years [standard deviation (SD) 9.4 years], and 64.7% (275/425) were female. Median time until the final follow-up colonoscopy during the study period was 13.5 years [interquartile range (IQR) 11.5–16.0 years] after the index colonoscopy, with a median of 4 colonoscopy procedures undertaken (range 2–10). All enrolled participants were closely monitored and followed up until the end of the designated study period. As shown in Table 2, nearly one third (30.6%, 130/425) of participants were classified as ‘near-average risk’ due to their family history, 59.8% (n = 254) as ‘moderate risk’ and 9.7% (n = 41) as ‘high-risk’. There was no significant difference in the gender proportions (p = 0.69) or the median follow up times (p = 0.25) when comparing the risk groups. Those in the high-risk group were younger at index colonoscopy (mean 46.2 years, SD 9.5 years) compared with those at moderate risk (mean 48.5 years, SD 10.0 years) and near-average risk (mean 52.1 years, SD 7.3 years) (p < 0.001) (Table 2).
Effect of Family History Risk Categories on Development of AN
In this population with a family history of CRC and a normal index colonoscopy, the incidence of AN at any colonoscopy during the total follow-up period was 14.4% (n = 61/425).
At the first follow-up colonoscopy (n = 403; which was completed a median of 5.2 years (IQR 4.9–6.1) after the index colonoscopy), there was a trend for the near-average category to have a higher incidence of AN (9.6%, n = 12/125), compared with 5.0% (n = 12/240) for the moderate risk category and 5.3% (n = 2/38) for the high-risk category, although the difference was not significant (p = 0.22) (Table 3). This trend was also observed over the entire surveillance period: 19.2% (n = 25/130) of near-average risk patients developed AN throughout the surveillance period, compared with 12.2% (n = 31/254) of moderate risk patients and 12.2% (n = 5/41) for the high-risk patients (p = 0.16). There were no differences between the time until diagnosis of AN for the three risk categories, with median time until diagnosis of 12.4 years for the near-average category, 13.1 years for moderate risk and 11.8 years for high-risk (p = 0.07).
Patients in the high-risk category were younger at the time of the AN finding (59.3 years, SD 10.2) compared with the moderate risk category (61.9 years, SD 9.8) and near-average risk category (64.8 years, SD 7.9) (p = 0.001) (Table 3).
Effect of Family History Demographics on the Development of AN
In a multivariable analysis, the patient’s gender and family history risk category did not affect the risk of AN in the surveillance population (p > 0.05) (Table 4). However, patients aged ≥ 60 years showed a four-fold (HR 4.14, 95% CI 1.33–12.89) higher risk of AN at any time point compared with patients aged < 40 years (p = 0.01). When adjusted for age, gender and the number of preceding non-significant colonoscopies, the number of affected family members and the age of diagnosis of CRC in the youngest affected family member did not affect the risk of developing AN in the surveillance population at any follow-up time (p > 0.05) (Table 4).
Incidence of CRC
Only four individuals developed adenocarcinoma throughout the surveillance period (0.9%) (Supplemental Table 1). The median time to development of adenocarcinoma after the index and most recent colonoscopy was 9.5 years (IQR 5.6–13.0 years) and 4.9 years (IQR 4.37–6.6 years), respectively. Three of the individuals were in the moderate-risk category, and one was considered near-average risk. No individuals in the high-risk group developed adenocarcinoma. Two individuals developed adenocarcinoma on their first follow-up colonoscopy (stage II ascending colon tumor and stage I sigmoid colon tumor respectively), and one was diagnosed with a stage II sigmoid colon tumor on the second follow-up, following two non-significant adenomas excised from the transverse colon on their prior colonoscopy. The remaining case had a stage III ascending colon tumor on their third follow-up colonoscopy, with only melanosis coli on previous colonoscopies. According to the criteria established by the World Endoscopy Organization [27], two of the cancers were considered “interval cancers” as they were detected in the interval prior to the recommended surveillance colonoscopy. The other two cancers were detected after the planned surveillance interval. All cancers were detected after an adequate prior colonoscopy.
Effect of Surveillance Colonoscopies Without AN on the Subsequent Development of AN
Absence of AN at prior follow-up colonoscopy (i.e., a ‘negative’ colonoscopy) was associated with a lower risk for AN at ongoing surveillance. As shown in Table 5, the risk of developing AN at any time point was 92% lower (HR 0.08, 95% CI 0.04, 0.18) if the individual had undergone two follow-up colonoscopies without AN during the follow-up time compared with only one negative follow-up colonoscopy (p < 0.001). The hazard ratio for AN was reduced further with each subsequent negative colonoscopy: if the patient had undergone three negative colonoscopies, the risk was 99% lower (HR 0.01, 95% CI 0.01, 0.03) and after four negative colonoscopies the risk was 99.8% lower (HR 0.002, 95% CI 0.001, 0.005), compared with only one negative follow-up colonoscopy (p < 0.001).
Discussion
Within this Australian population undergoing colonoscopy surveillance due to family history of CRC, there was no significant difference in the development of AN between the family history risk groups after a normal index colonoscopy. Our data also suggested that the number and age of affected relatives did not impact on AN risk. Age ≥ 60 years at index colonoscopy was the only significant risk factor for future development of AN. With each subsequent colonoscopy without advanced findings, the proportion of those who went on to develop AN became increasingly lower, suggesting that negative good quality surveillance colonoscopies predict a lower lifetime CRC risk, even in those at higher risk due to family history.
Family history has long been considered a risk factor for CRC and is currently used in screening guidelines to stratify individuals into risk categories warranting more intensive screening than the average population [6, 10,11,12, 18, 28, 29]. The Australian guidelines were based on international cohort studies [9, 29,30,31,32,33,34] and had not been validated with Australian data. In addition, there was little evidence whether there was enduring risk of AN following colonoscopies with no advanced findings in family history populations.
Our findings correspond with similar studies, revealing little evidence in clinical practice that family history risk categories correlate with AN risk. A 2017 outcome study of an Irish CRC surveillance program found that the extent of family history was not a significant contributor to AN risk at surveillance colonoscopy, with age > 50 years identified as the only significant risk factor [34]. Another study of individuals with one first-degree relative < 50 years with CRC or two first-degree relatives at any age found that advanced adenoma at index colonoscopy was associated with subsequent metachronous advanced adenoma, however the type of family history was not [35]. Our study expands on these studies by analyzing a cohort with a normal index colonoscopy, which we would expect to have a lower lifetime risk than those with adenomas on index colonoscopy.
In our population, the incidence of AN decreased when patients had undergone follow-up colonoscopies after normal or non-advanced findings on prior colonoscopies. There is convincing international evidence in average-risk individuals that a normal index colonoscopy reduces the future risk of CRC. Lee et al. [16] demonstrated that a normal colonoscopy conferred a 46% lower risk of CRC, and an 88% lower risk of cancer-related death for > 12 years, when compared with an unscreened cohort. Similarly, Nishihara et al. [19] found that CRC risk persistently decreased after a normal colonoscopy, with a hazard ratio of 0.35 for < 3 years to 0.65 at > 15 years. Morelli et al. [17] found that low-risk findings (no advanced adenoma or < 3 non-advanced adenomas) on index colonoscopy and normal/low-risk findings at first surveillance colonoscopy conferred only a 3.8% incidence of AN on second surveillance colonoscopy, compared with a 15.4% incidence of AN at second surveillance colonoscopy in those with a low-risk index colonoscopy but with AN on first surveillance.
The data regarding enduring risk following normal colonoscopies in high-risk family history populations is more limited, but the available studies correspond with our findings. One study of family history surveillance demonstrated that absence of adenomas and advanced adenomas at index colonoscopy was predictive of a normal follow-up surveillance period [36]. In a population cohort of 7515 individuals from Utah, Samadder et al. [18] demonstrated that patients with a first-degree relative with CRC had a significantly lower than expected incidence of CRC for only the first 5 years after a negative index colonoscopy (standardized incidence ratio 0.39, 95% CI 0.13–0.64), however it was noted that the Utah population has low rates of smoking and drinking, which could make this cohort less generalizable to other populations. Conversely, a study by Lieberman et al. [37], that included the assessment of 6535 individuals undergoing colonoscopy for an indication of family history, found no increased risk for CRC for 10 years after normal index colonoscopy. However, types of family history were not detailed and could have included any family history of CRC or polyps, and not limited to first degree relatives under 60 years at diagnosis. Despite these two large studies, there is still uncertainty about how long the risk of CRC remains reduced after a negative colonoscopy in people with a family history, based on limited available evidence in well characterized family history populations.”
The low incidence of AN in the current audit suggests that surveillance intervals in individuals with a family history of CRC may be too frequent following an index colonoscopy without neoplasia. In average-risk individuals with normal or non-advanced findings on index colonoscopy, there is high-quality evidence that repeat colonoscopy can be deferred until 10 years after the index procedure [14, 16, 18,19,20]. This is reflected in the Australian post-polypectomy guidelines which suggest extending to 10-year colonoscopy after low-risk findings [1–2 small (< 10 mm) tubular adenomas without high-grade dysplasia] [26]. However, the optimal surveillance intervals in family history populations is less established. The Australian guidelines recommend CRC screening with FIT biennially from age 40, then 5-yearly colonoscopy from age 50 for moderate-risk individuals (Category 2), and biennial FIT from age 35 with 5-yearly colonoscopy from age 45 for high-risk individuals (Category 3) [12]. The 5-year surveillance interval was based on international evidence that family history did not affect the risk of AN within 5 years of polypectomy [38,39,40]. However, these studies did not investigate the significance of a normal index colonoscopy. Our Australian data, in conjunction with international data, suggest that a normal index colonoscopy is a negative predictor for future AN and that family history plays a less significant role in CRC risk than previously believed. We therefore propose that the risk after a normal colonoscopy is low enough to warrant extension to 10-year surveillance intervals, as would be suggested for the average-risk population, or even that they be taken off colonoscopic surveillance and continue with biennial FIT.
Additionally, given that age ≥ 60 years was the most significant risk factor in our population, we suggest a role for delaying the age of colonoscopy surveillance to age 60 years, regardless of the extent of family history. Also of note is that previous Australian guidelines recommended screening 10 years younger than the age of the youngest relative at CRC diagnosis, but the updated guidelines removed this recommendation due to lack of evidence [12]. Our study has shown that the age of CRC diagnosis in first- and second-degree relatives does not affect CRC risk, therefore supporting that this not be used as an indicator of the age to begin screening.
There are several study limitations. This study relies on self-reported family history details and are not verified with patient records. Therefore, some ages may have been inaccurately reported, leading to possible risk category misclassification. Our analysis is retrospective and limited to those undergoing follow-up, meaning that those who exited the surveillance program early are not accounted for. This may have introduced a small healthy person bias, as only including individuals who have been undergoing surveillance colonoscopies for a minimum of 10 years could have limited the cohort to a healthier population. Due to the 20-year surveillance period of this study, the cohort covers different guidelines depending on when surveillance was commenced. Furthermore, there are likely other risk factors in the cohort that are unaccounted for, including ethnicity, medications, environment, and modifiable risk factors such as diet, smoking, metabolic syndrome, and sedentary lifestyle. Recent studies have proposed that these factors should be considered in addition to family history when planning the starting age for screening colonoscopy, to provide a personalized and precision risk-based approach [41, 42]. Additionally, there is no true control group (i.e., those without a family history of colorectal cancer) in our study. However, the ‘near-average group’ have a very similar risk to the average Australian population [12]. The strength of this study is that the population comes from a large, long-term, well-recorded surveillance program.
Conclusions
Overall, these results suggest that family history may not pose as significant a risk of AN as previously thought and that regular colonoscopies may not be required, particularly if an individual has had at least one normal colonoscopy. Extending surveillance intervals to 10 years while providing regular FIT could be a more efficient use of resources in this population. Consideration of more personalized screening based on family history, age and findings at previous colonoscopy may be a direction for the future of CRC screening in Australia.
References
Australian Institute of Health and Welfare. Cancer in Australia 2019. Canberra: AIHW; 2019. Available at: https://www.aihw.gov.au/reports/cancer/cancer-in-australia-2019 Accessed November 19 2021.
Winawer SJ, Zauber AG, Ho MN et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N. Engl. J. Med. 1993;329:1977–1981.
Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M. Protection from colorectal cancer after colonoscopy: a population-based, case-control study. Ann. Intern. Med. 2011;154:22–30.
Kahi CJ. Reviewing the evidence that polypectomy prevents cancer. Gastrointest. Endosc. Clin. N. Am. 2019;29:577–585.
Kahi CJ, Imperiale TF, Juliar BE, Rex DK. Effect of screening colonoscopy on colorectal cancer incidence and mortality. Clin. Gastroenterol. Hepatol. 2009;7:770–775.
Johns LE, Houlston RS. A systematic review and meta-analysis of familial colorectal cancer risk. Am. J. Gastroenterol. 2001;96:2992–3003.
Taylor DP, Burt RW, Williams MS, Haug PJ, Cannon-Albright LA. Population-based family history-specific risks for colorectal cancer: a constellation approach. Gastroenterology. 2010;138:877–885.
Benhamiche-Bouvier AM, Lejeune C, Jouve JL, Manfredi S, Bonithon-Kopp C, Faivre J. Family history and risk of colorectal cancer: implications for screening programmes. J. Med. Screen. 2000;7:136–140.
Taylor DP, Stoddard GJ, Burt RW et al. How well does family history predict who will get colorectal cancer? Implications for cancer screening and counseling. Genet. Med. 2011;13:385–391.
Henrikson N, Webber E, Goddard K et al. Family history and the natural history of colorectal cancer: systematic review. Genet. Med. 2015;17:702–712.
Sandhu MS, Luben R, Khaw KT. Prevalence and family history of colorectal cancer: implications for screening. J. Med. Screen. 2001;8:69–72.
Cancer Council Australia, Colorectal Cancer Guidelines Working Party. Clinical practice guidelines for the prevention, early detection and management of colorectal cancer. 2017. Available at: https://wiki.cancer.org.au/australia/Guidelines:Colorectal_cancer Accessed August 29 2021.
Jenkins MA, Ait Ouakrim D, Boussioutas A et al. Revised Australian national guidelines for colorectal cancer screening: family history. Med. J. Aust. 2018;209:455–460.
Gupta S, Lieberman D, Anderson JC et al. Recommendations for follow-up after colonoscopy and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastrointest. Endosc. 2020;9:463–485.
Duvvuri A, Chandrasekar VT, Srinivasan S et al. Risk of colorectal cancer and cancer related mortality after detection of low-risk or high-risk adenomas, compared with no adenoma, at index colonoscopy: a systematic review and meta-analysis. Gastroenterology. 2021;160:1986–1996.
Lee JK, Jensen CD, Levin TR et al. Long-term risk of colorectal cancer and related deaths after a colonoscopy with normal findings. JAMA Intern. Med. 2019;179:153–160.
Morelli MS, Glowinski EA, Juluri R, Johnson CS, Imperiale TF. Yield of the second surveillance colonoscopy based on the results of the index and first surveillance colonoscopies. Endoscopy. 2013;45:821–826.
Samadder NJ, Pappas L, Boucherr KM et al. Long-term colorectal cancer incidence after negative colonoscopy in the state of Utah: the effect of family history. Am. J. Gastroenterol. 2017;112:1439–1447.
Nishihara R, Wu K, Lochhead P et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N. Engl. J. Med. 2013;369:1095–1105.
Brenner H, Altenhofen L, Stock C, Hoffmeister M. Incidence of colorectal adenomas: birth cohort analysis among 4.3 million participants of screening colonoscopy. Cancer Epidemiol. Biomark. Prev. 2014;23:1920–1927.
Bampton PA, Sandford JJ, Young GP. Applying evidence-based guidelines improves use of colonoscopy resources in patients with a moderate risk of colorectal neoplasia. Med. J. Aust. 2002;176:155–157.
Park SK, Song YS, Jung YS et al. Do surveillance intervals in patients with more than five adenomas at index colonoscopy be shorter than those in patients with three to four adenomas? A Korean Association for the Study of Intestinal Disease study. J. Gastroenterol. Hepatol. 2017;32:1026–1031.
Vemulapalli KC, Rex DK. Risk of advanced lesions at first follow-up colonoscopy in high-risk groups as defined by the United Kingdom post-polypectomy surveillance guideline: data from a single U.S. center. Gastrointest. Endosc. 2014;80:299–306.
Rutter MD, East J, Rees CJ et al. British Society of Gastroenterology/Association of Coloproctology of Great Britain and Ireland/Public Health England post-polypectomy and post-colorectal cancer resection surveillance guidelines. Gut. 2020;69:201–223.
Pérez-Cuadrado-Robles E, Torrella-Cortés E, Bebia-Conesa P et al. Intermediate-risk patients with three to four small adenomas should be considered low risk for colorectal cancer screening. Dig. Endosc. 2016;28:450–455.
Cancer Council Australia, Colorectal Cancer Guidelines Working Party. Clinical practice guidelines for surveillance colonoscopy. 2018. Available at: https://wiki.cancer.org.au/australia/Guidelines:Colorectal_cancer/Colonoscopy_surveillance Accessed August 14 2021.
Rutter MD, Beintaris I, Valori R et al. World endoscopy organization consensus statements on post-colonoscopy and post-imaging colorectal cancer. Gastroenterology. 2018;155:909–925.
Hall NR, Bishop DT, Stephenson BM, Finan PJ. Hereditary susceptibility to colorectal cancer. Relatives of early onset cases are particularly at risk. Dis. Colon Rectum. 1996;39:739–743.
Schoen RE, Razzak A, Yu KJ et al. Incidence and mortality of colorectal cancer in individuals with a family history of colorectal cancer. Gastroenterology. 2015;149:1438–1445.
Bass AJ, Meyerhardt JA, Chan JA, Giovannucci EL, Fuchs CS. Family history and survival after colorectal cancer diagnosis. Cancer. 2008;112:1222–1229.
Murphy G, Shu XO, Gao YT et al. Family cancer history affecting risk of colorectal cancer in a prospective cohort of Chinese women. Cancer Causes Control. 2009;20:1517–1521.
Leu M, Reilly M, Czene K. Evaluation of bias in familial risk estimates: a study of common cancers using Swedish population-based registers. J. Natl. Cancer Inst. 2008;100:1318–1325.
Stefansson T, Moller PH, Sigurdsson F, Steingrimsson E, Eldon BJ. Familial risk of colon and rectal cancer in Iceland: evidence for different etiologic factors? Int. J. Cancer. 2006;119:304–308.
Wei EK, Giovannucci E, Wu K et al. Comparison of risk factors for colon and rectal cancer. Int. J. Cancer. 2004;108:433–442.
Hennink SD, van der Meulen-de Jong AE, Wolterbeek R et al. Randomized comparison of surveillance intervals in familial colorectal cancer. J. Clin. Oncol. 2015;33:4188–4193.
Walshe M, Moran R, Boyle M et al. High-risk family colorectal cancer screening service in Ireland: critical review of clinical outcomes. Cancer Epidemiol. 2017;50:30–38.
Lieberman DA, Holub JL, Morris CD, Logan J, Williams JL, Carney P. Low rate of large polyps (>9 mm) within 10 years after an adequate baseline colonoscopy with no polyps. Gastroenterology. 2014;147:343–350.
Chung SJ, Kim YS, Yang SY et al. Five-year risk for advanced colorectal neoplasia after initial colonoscopy according to the baseline risk stratification: a prospective study in 2452 asymptomatic Koreans. Gut. 2011;60:1537–1543.
Park SK, Hwang SW, Kim KO et al. Risk of advanced colorectal neoplasm in patients with more than 10 adenomas on index colonoscopy: a Korean Association for the Study of Intestinal Diseases (KASID) study. J. Gastroenterol. Hepatol. 2017;32:803–808.
Anderson JC, Baron JA, Ahnen DJ et al. Factors associated with shorter colonoscopy surveillance intervals for patients with low-risk colorectal adenomas and effects on outcome. Gastroenterology. 2017;152:1933–1943.
Jeon J, Du M, Schoen RE, Hoffmeister M et al. Determining risk of colorectal cancer and starting age of screening based on lifestyle, environmental, and genetic factors. Colorectal transdisciplinary study and genetics and epidemiology of colorectal cancer consortium. Gastroenterology. 2018;154:2152–2164.
Kastrinos F, Kupfer SS, Gupta S. Colorectal cancer risk assessment and precision approaches to screening: brave new world or worlds apart? Gastroenterology. 2023;164:812–827.
Acknowledgments
We acknowledge all clinicians participating in the SCOOP program and the patients undergoing surveillance.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no personal, professional or financial conflicts of interest relevant to the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Barnett, M.I., Wassie, M.M., Cock, C. et al. Low Incidence of Colorectal Advanced Neoplasia During Surveillance in Individuals with a Family History of Colorectal Cancer. Dig Dis Sci 68, 4243–4251 (2023). https://doi.org/10.1007/s10620-023-08053-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-08053-6