Abstract
Background and Aims
Pancreaticobiliary diseases are common in the elderly. To this end, frailty represents a state of vulnerability that should be considered when assessing the risks and benefits of therapeutic endoscopic procedures. We aim to determine the rate of readmissions and clinical outcomes using the validated Hospital Frailty Risk Score in patients undergoing endoscopic retrograde cholangiopancreatography (ERCP).
Methods
Using the National Readmissions Database, we identified patients with an admission diagnosis of cholangitis with obstructive stone from 2016 to 2019. Patients were determined to be of low frailty risk with a score of < 5, while patients of medium to high frailty risk had a score of > 5.
Results
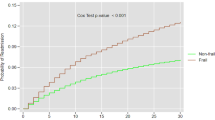
During the study period, 5751 patients were identified with acute cholangitis with obstructing stone. Mean age of index admissions was 69.4 years and 51.8% were female. From the total cohort, 5119 (89.2%) patients underwent therapeutic ERCP, 38.0% (n = 1947) of whom were regarded as frail (risk score > 5). Following ERCP, frail patients had a less but statistically insignificant readmission rate compared to non-frail patients (2.76% vs 4.05%, p = 0.450). However, compared to non-frail patients, frail patients experienced higher post-ERCP complications (6.20% vs 14.63%, p < 0.001). Frail patients were more likely to have longer lengths of stay, higher hospital cost, and mortality risk.
Conclusion
ERCP is not a risk factor for readmission among frail patients. However, frail patients are at higher risk for procedure-related complications, healthcare utilization, and mortality.

Similar content being viewed by others
References
Facciorusso A, Ramai D, Gkolfakis P et al. Comparative efficacy of different methods for difficult biliary cannulation in ERCP: A Systematic review and network meta-analysis. Gastrointest Endosc 2022;95:60–71.
Day LW, Lin L, Somsouk M. Adverse events in older patients undergoing ERCP: A systematic review and meta-analysis. Endosc Int Open 2014;2:28–36.
Finkelmeier F, Tal A, Ajouaou M et al. ERCP in elderly patients: Increased risk of sedation adverse events but low frequency of post-ERCP pancreatitis. Gastrointest Endosc 2015;82:1051–1059.
Gilbert T, Neuburger J, Kraindler J et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: An observational study. Lancet 2018;391:1775–1782.
Wleklik M, Uchmanowicz I, Jankowska EA et al. Multidimensional approach to frailty. Front Psychol 2020;11:564.
Bagshaw SM, Stelfox HT, McDermid RC et al. Association between frailty and short- and long-term outcomes among critically ill patients: A multicenter prospective cohort study. CMAJ 2014;186:95–102.
Stefanaki C, Pervanidou P, Boschiero D, Chrousos GP. Chronic stress and body composition disorders: implications for health and disease. Hormones. 2018;17:33–43.
Chen X, Mao G, Leng SX. Frailty syndrome: An overview. Clin Interv Aging 2014;9:433–441.
Walston J, Buta B, Xue QL. Frailty screening and interventions: Considerations for clinical practice. Clin Geriatr Med 2018;34:25–38.
HCUP Nationwide Readmissions Database (NRD). Healthcare Cost and Utilization Project (HCUP). 2019. Agency for Healthcare Research and Quality, Rockville, MD. https://www.hcup-us.ahrq.gov/nrdoverview.jsp.
Moore BJ, White S, Washington R, Coenen N, Elixhauser A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: The AHRQ Elixhauser Comorbidity index. Med Care 2017;55:698–705.
Quan H, Sundararajan V, Halfon P et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130–1139.
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care 2009;47:626–633.
Malik AH, Yandrapalli S, Zaid S et al. Impact of frailty on mortality, readmissions, and resource utilization after TAVI. Am J Cardiol 2020;127:120–127.
Li C. Little’s test of missing completely at random. Stata J 2013;13:795–809.
Royston P. Multiple imputation of missing values. Stata J 2004;4:227–241.
Facciorusso A, Amato A, Crinò SF et al. Definition of a hospital volume threshold to optimize outcomes after drainage of pancreatic fluid collections with lumen-apposing metal stents: A nationwide cohort study. Gastrointest Endosc 2022;95:1158–1172.
Loperfido S, Angelini G, Benedetti G et al. Major early complications from diagnostic and therapeutic ERCP: A prospective multicenter study. Gastrointest Endosc 1998;48:1–10.
Keswani RN, Qumseya BJ, O’Dwyer LC, Wani S. Association between Endoscopist and center endoscopic retrograde cholangiopancreatography volume with procedure success and adverse outcomes: A systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2017;15:1866–1875.
Parikh MP, Garg R, Chittajallu V et al. Trends and risk factors for 30-day readmissions in patients with acute cholangitis: Analysis from the national readmission database. Surg Endosc 2021;35:223–231.
Jeurnink SM, Poley JW, Steyerberg EW, Kuipers EJ, Siersema PD. ERCP as an outpatient treatment: A review. Gastrointest Endosc 2008;68:118–123.
Nelson DB. Infectious disease complications of GI endoscopy: Part I, endogenous infections. Gastrointest Endosc 2003;57:546–556.
Lam SK, Tsui JK, Chan PK et al. How often does bacteraemia occur following endoscopic retrograde cholangiopancreatography (ERCP)? Endoscopy 1977;9:231–234.
Parker HW, Geenen JE, Bjork JT et al. A prospective analysis of fever and bacteremia following ERCP. Gastrointest Endosc 1979;25:102–103.
Siegel JH, Berger SA, Sable RA et al. Low incidence of bacteremia following endoscopic retrograde cholangiopancreatography (ERCP). Am J Gastroenterol 1979;71:465–468.
ASGE Standards of Practice Committee, Khashab MA, Chithadi KV et al. Antibiotic prophylaxis for GI endoscopy. Gastrointest Endosc 2015;81:81–89.
Thosani N, Zubarik RS, Kochar R et al. Prospective evaluation of bacteremia rates and infectious complications among patients undergoing single-operator choledochoscopy during ERCP. Endoscopy 2016;48:424–431.
Clegg A, Bates C, Young J et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age ageing 2016;45:353–360.
Funding
None.
Author information
Authors and Affiliations
Contributions
DR conceived and designed the study. AO, PG, and SC collected data. DR and JH conducted data analysis. DR drafted the manuscript. AT, MTB, CH, AR, and AF revised the manuscript for intellectual content. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Alessandro Repici is a consultant for Boston Scientific and Fuji. Daryl Ramai, Joseph Heaton, Andrew Ofosu, Paraskevas Gkolfakis, Saurabh Chandan, Alberto Tringali, Monique T. Barakat, Cesare Hassan, and Antonio Facciorusso have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ramai, D., Heaton, J., Ofosu, A. et al. Influence of Frailty in Patients Undergoing Endoscopic Retrograde Cholangiopancreatography for Biliary Stone Disease: A Nationwide Study. Dig Dis Sci 68, 3605–3613 (2023). https://doi.org/10.1007/s10620-023-08013-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-08013-0