Abstract
Background
Acute pancreatitis is the most common gastrointestinal cause of hospital admissions in the United States of which biliary or gallstone disease is the most common inciting factor.
Aim
Estimate the effects of frailty on burden, costs, and causes for hospitalization in patients with acute biliary pancreatitis.
Methods
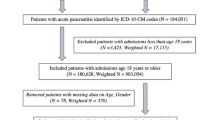
We analysed the Nationwide Readmission Database from 2016 to 2019 for patients with acute biliary pancreatitis. Patients were categorized into two groups, frail and non-frail, based on the Hospital Frailty Risk Score. Logistic and Cox regression were used to predict the impact of frailty on 30-day readmission, length of stay, mortality, and costs.
Results
162,202 index hospitalizations with acute biliary pancreatitis without cholangitis were identified, of whom 59.2% (n = 96,045) were female and 22.49% (n = 36,475) were classified as frail. Readmissions within 30 days were higher among frail patients (12.58% vs 7.09%, P < 0.001) compared to non-frail patients, respectively. Regression modeling showed that frail patients had higher odds of readmission (OR 1.32; 95% CI 1.24–1.42, P < 0.001), longer lengths of stay (8.18 days vs 4.11 days), and higher average costs of hospitalization ($21,511 vs $12,261) compared to non-frail patients, respectively. Cox regression showed that frail patients had a higher risk of mortality (HR 5.43; 95% Cl 4.06–7.29, P < 0.001) compared to non-frail patients, respectively.
Conclusions
Frailty is independently associated with higher mortality and burden of healthcare utilization in patients with acute biliary pancreatitis. We suggest using the Hospital Frailty Risk Score as part of the treatment algorithm in patients with acute biliary pancreatitis.


Similar content being viewed by others
References
Cho SK, Huh JH, Yoo JS et al. HOMA-estimated insulin resistance as an independent prognostic factor in patients with acute pancreatitis. Sci Rep. 2019;9:14894.
Crockett SD, Wani S, Gardner TB et al. American gastroenterological association institute guideline on initial management of acute pancreatitis. Gastroenterology. 2018;154:1096–1101.
Yang AL, McNabb-Baltar J. Hypertriglyceridemia and acute pancreatitis. Pancreatology. 2020;20:795–800.
Petrov MS, Yadav D. Global epidemiology and holistic prevention of pancreatitis. Nat Rev Gastroenterol Hepatol. 2019;16:175–184.
Cho JH, Kim TN, Kim SB. Comparison of clinical course and outcome of acute pancreatitis according to the two main etiologies: Alcohol and gallstone. BMC Gastroenterol. 2015;15:87.
Forsmark CE, Vege SS, Wilcox CM. Acute pancreatitis. N Engl J Med. 2016;375:1972–1981.
Marta K, Lazarescu AM, Farkas N, Mátrai P, Cazacu I, Ottoffy M, Habon T, Erőss B, Vincze A, Veres G, Czako L. Aging and comorbidities in acute pancreatitis I: a meta-analysis and systematic review based on 194,702 patients. Frontiers in physiology. 2019;10:328.
Garg SK, Sarvepalli S, Campbell JP, Obaitan I, Singh D, Bazerbachi F, Singh R, Sanaka MR. Incidence, admission rates, and predictors, and economic burden of adult emergency visits for acute pancreatitis. Journal of clinical gastroenterology. 2019;53(3):220–225.
Gilbert T, Neuburger J, Kraindler J et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: An observational study. Lancet 2018;391:1775–1782.
Wleklik M, Uchmanowicz I, Jankowska EA et al. Multidimensional approach to frailty. Front Psychol 2020;11:564.
Bagshaw SM, Stelfox HT, McDermid RC et al. Association between frailty and short- and long-term outcomes among critically ill patients: A multicenter prospective cohort study. CMAJ 2014;186:95–102.
Chen X, Mao G, Leng SX. Frailty syndrome: An overview. Clin Interv Aging 2014;9:433–441.
Walston J, Buta B, Xue QL. Frailty Screening and Interventions: Considerations for Clinical Practice. Clin Geriatr Med 2018;34:25–38.
HCUP Nationwide Readmissions Database (NRD). Healthcare Cost and Utilization Project (HCUP). 2019. Agency for Healthcare Research and Quality, Rockville, MD. https://www.hcup-us.ahrq.gov/nrdoverview.jsp.
Moore BJ, White S, Washington R, Coenen N, Elixhauser A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: The AHRQ Elixhauser Comorbidity index. Med Care 2017;55:698–705.
Quan H, Sundararajan V, Halfon P et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130–1139.
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care 2009;47:626–633.
Malik AH, Yandrapalli S, Zaid S et al. Impact of Frailty on Mortality, Readmissions, and Resource Utilization After TAVI. Am J Cardiol 2020;127:120–127.
Li C. Little’s test of missing completely at random. Stata J 2013;13:795–809.
Royston P. Multiple imputation of missing values. Stata J 2004;4:227–241.
Clegg A, Bates C, Young J et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age ageing 2016;45:353–360.
Funding
None.
Author information
Authors and Affiliations
Contributions
DR conceived and designed the study. JH, AA collected data. DR and JH conducted data analysis. DR drafted the manuscript. JM and DGA revised the manuscript for intellectual content. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Douglas G. Adler is a consultant for Boston Scientific and Micro Tech. All other authors have no relevant conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ramai, D., Heaton, J., Abomhya, A. et al. Frailty Is Independently Associated with Higher Mortality and Readmissions in Patients with Acute Biliary Pancreatitis: A Nationwide Inpatient Study. Dig Dis Sci 68, 2196–2203 (2023). https://doi.org/10.1007/s10620-023-07830-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-07830-7