Abstract
Introduction
Chronic inflammatory conditions of the pouch are common after ileal pouch-anal anastomosis (IPAA) for ulcerative colitis (UC).
Aims
We aimed to investigate the relationship between acute pouchitis within 180 days of the final stage of IPAA surgery (very early pouchitis) and the future development of chronic antibiotic dependent pouchitis (CADP) and Crohn’s-like disease of the pouch (CLDP).
Methods
We performed a retrospective cohort study, evaluating patients who underwent proctocolectomy with IPAA between January 1, 2004 and December 31, 2016. Multivariable logistic regression was used to evaluate the relationship between very early pouchitis and the development of CADP and CLDP.
Results
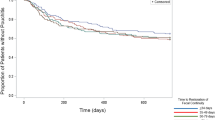
Among 626 patients undergoing IPAA for UC, 137 (22%) developed very early pouchitis, 75 (12%) developed CADP, and 59 (9%) developed CLDP in a median follow-up of 5.18 years (interquartile range 0.94–10.8 years). Very early pouchitis was associated with a significant increase in the odds of developing CADP (adjusted odds ratio [aOR3.65, 95% CI 2.19–6.10) as was primary sclerosing cholangitis (aOR 3.97, 95% CI 1.44–11.0). Very early pouchitis was associated with increased odds for developing CLDP (aOR 2.77, 95% CI 1.54–4.98) along with a family history of inflammatory bowel disease (aOR 2.10, 95% CI 1.11–3.96).
Conclusion
In this cohort, very early pouchitis was associated with an increased risk of developing CADP and CLDP. These findings highlight very early pouchitis as a unique risk factor for chronic inflammatory conditions of the pouch and the need for future studies evaluating potential strategies for secondary prophylaxis strategies in this population.

Similar content being viewed by others
References
Tsai L, Ma C, Dulai PS et al. Contemporary risk of surgery in patients with ulcerative colitis and crohn’s disease: a meta-analysis of population-based cohorts. Clin Gastroenterol Hepatol 2021;19:2031–2045.e2011.
Frolkis AD, Dykeman J, Negron ME et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology 2013;145:996–1006.
Magro F, Gionchetti P, Eliakim R et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: Definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and Ileo-anal pouch disorders. J Crohns Colitis 2017;11:649–670.
Ross H, Steele SR, Varma M et al. Practice parameters for the surgical treatment of ulcerative colitis. Dis Colon Rectum 2014;57:5–22.
Fumery M, Singh S, Dulai PS et al. Natural history of adult ulcerative colitis in population-based cohorts: a systematic review. Clin Gastroenterol Hepatol 2018;16:e343.
Fazio VW, Kiran RP, Remzi FH et al. Ileal pouch anal anastomosis: analysis of outcome and quality of life in 3707 patients. Ann Surg 2013;257:679–685.
Delaney CP, Fazio VW, Remzi FH et al. Prospective, age-related analysis of surgical results, functional outcome, and quality of life after ileal pouch-anal anastomosis. Ann Surg 2003;238:221–228.
Gionchetti P, Rizzello F, Helwig U et al. Prophylaxis of pouchitis onset with probiotic therapy: a double-blind, placebo-controlled trial. Gastroenterology 2003;124:1202–1209.
Lightner AL, Mathis KL, Dozois EJ et al. Results at up to 30 years after ileal pouch-anal anastomosis for chronic ulcerative colitis. Inflamm Bowel Dis 2017;23:781–790.
Barnes EL, Herfarth HH, Sandler RS et al. Pouch-related symptoms and quality of life in patients with ileal pouch-anal anastomosis. Inflamm Bowel Dis 2017;23:1218–1224.
Quinn KP, Raffals LE. An update on the medical management of inflammatory pouch complications. Am J Gastroenterol 2020;115:1439–1450.
Barnes EL, Lightner AL, Regueiro M. Peri-operative and post-operative management of patients with crohn’s disease and ulcerative colitis. Clin Gastroenterol Hepatol 2020;18:1356–1366.
Barnes EL, Kochar B, Jessup HR, Herfarth HH. The incidence and definition of crohn’s disease of the pouch: a systematic review and meta-analysis. Inflamm Bowel Dis 2019;25:1474–1480.
Yu CS, Pemberton JH, Larson D. Ileal pouch-anal anastomosis in patients with indeterminate colitis: long-term results. Dis Colon Rectum 2000;43:1487–1496.
Tulchinsky H, Hawley PR, Nicholls J. Long-term failure after restorative proctocolectomy for ulcerative colitis. Ann Surg 2003;238:229–234.
Alsafi Z, Snell A, Segal JP. Prevalence of “pouch failure” of the ileoanal pouch in ulcerative colitis: a systematic review and meta-analysis. Int J Colorectal Dis 2022;37:357–364.
Barnes EL, Holubar SD, Herfarth HH. Systematic review and meta-analysis of outcomes after ileal pouch-anal anastomosis in primary sclerosing cholangitis-ulcerative colitis. J Crohns Colitis 2021;15:1272–1278.
Wasmuth HH, Tranø G, Endreseth BH et al. Primary sclerosing cholangitis and extraintestinal manifestations in patients with ulcerative colitis and ileal pouch-anal anastomosis. J Gastrointest Surg: Official J Soc Surg Aliment Tract 2010;14:1099–1104.
Hata K, Okada S, Shinagawa T et al. Meta-analysis of the association of extraintestinal manifestations with the development of pouchitis in patients with ulcerative colitis. BJS Open 2019;3:436–444.
Shen B, Fazio VW, Remzi FH et al. Risk factors for diseases of ileal pouch-anal anastomosis after restorative proctocolectomy for ulcerative colitis. Clin Gastroenterol Hepatol 2006;4:81–89 quiz 82-83.
Kayal M, Kohler D, Plietz M et al. Early pouchitis is associated with crohn’s disease-like pouch inflammation in patients with ulcerative colitis. Inflamm Bowel Dis 2022;28:1821–1825.
Shen B, Achkar JP, Connor JT et al. Modified pouchitis disease activity index: a simplified approach to the diagnosis of pouchitis. Dis Colon Rectum 2003;46:748–753.
Sherrill GC, Esckilsen S, Hudson J et al. Relationship between stages of ileal pouch-anal anastomosis, timing of restoration of fecal continuity, and pouchitis. Dig Dis Sci 2022;11:5220–5226.
Sandborn WJ, Tremaine WJ, Batts KP et al. Pouchitis after ileal pouch-anal anastomosis: a pouchitis disease activity index. Mayo Clin Proc 1994;69:409–415.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–174.
Novello M, Shen B, Stocchi L. Pouchitis as an indication for ileal pouch surgical revision. Inflamm Bowel Dis 2019;25:e25.
Ben-Bassat O, Tyler AD, Xu W et al. Ileal pouch symptoms do not correlate with inflammation of the pouch. Clin Gastroenterol Hepatol 2014;12:831-837.e832.
Barnes EL, Herfarth HH, Kappelman MD et al. Incidence, risk factors, and outcomes of pouchitis and pouch-related complications in patients with ulcerative colitis. Clin Gastroenterol Hepatol 2021;19:1583–1591.
Barnes EL, Kappelman MD, Zhang X et al. Patients with pouchitis demonstrate a significant cost burden in the first two years after ileal pouch-anal anastomosis. Clin Gastroenterol Hepatol 2022;20:2908–2910.
Barnes EL, Allin KH, Iversen AT et al. Increasing incidence of pouchitis between 1996 and 2018: a population-based danish cohort study. Clin Gastroenterol Hepatol 2023;1:192–199.
Shen B, Kochhar GS, Rubin DT et al. Treatment of pouchitis, crohn’s disease, cuffitis, and other inflammatory disorders of the pouch: consensus guidelines from the international ileal pouch consortium. The Lancet Gastroenterol Hepatol 2022;7:69–95.
Batista D, Raffals L. Role of intestinal bacteria in the pathogenesis of pouchitis. Inflamm Bowel Dis 2014;20:1481–1486.
Kohyama A, Ogawa H, Funayama Y et al. Bacterial population moves toward a colon-like community in the pouch after total proctocolectomy. Surgery 2009;145:435–447.
Nicholls RJ, Belliveau P, Neill M et al. Restorative proctocolectomy with ileal reservoir: a pathophysiological assessment. Gut 1981;22:462–468.
Santavirta J, Mattila J, Kokki M, Matikainen M. Mucosal morphology and faecal bacteriology after ileoanal anastomosis. Int J Colorectal Dis 1991;6:38–41.
Maharshak N, Cohen NA, Reshef L et al. Alterations of enteric microbiota in patients with a normal ileal pouch are predictive of pouchitis. J Crohns Colitis 2017;11:314–320.
Reshef L, Kovacs A, Ofer A et al. Pouch inflammation is associated with a decrease in specific bacterial taxa. Gastroenterology 2015;149:718–727.
Barnes EL, Kochar B, Herfarth HH et al. Creation of a case-finding definition for identifying patients with acute pouchitis in administrative claims data. Clin Gastroenterol Hepatol 2021;19:842–844.
Funding
This research was supported by the National Institutes of Health [K23DK127157-01 (ELB)].
Author information
Authors and Affiliations
Contributions
SE: study design, data collection, interpretation of the data, drafting the manuscript, revising the manuscript. BK, KNW, HHH: study design, data collection, interpretation of the data, revising the manuscript. ELB: study design, data collection, data analysis, interpretation of the data, drafting the manuscript, revising the manuscript.
Corresponding author
Ethics declarations
Competing Interest
Scott Esckilsen has no relevant disclosures. Bharati Kochar has served as a consultant for Pfizer. Kimberly N. Weaver has served as a consultant for AbbVie and BMS. Hans H. Herfarth has served as a consultant for Alivio, AMAG, Boehringer, BMS, ExeGi Pharma, Finch, Fresenius Kabi, Gilead, Janssen, Lycera, Merck, Otsuka, Pfizer, PureTech, Seres and research support from Allakos, Artizan Biosciences, Novo Nordisk and Pfizer. Edward L. Barnes has served as a consultant for AbbVie, Bristol-Meyers Squibb, Eli Lilly, and Target RWE.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Esckilsen, S., Kochar, B., Weaver, K.N. et al. Very Early Pouchitis Is Associated with an Increased Likelihood of Chronic Inflammatory Conditions of the Pouch. Dig Dis Sci 68, 3139–3147 (2023). https://doi.org/10.1007/s10620-023-07947-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-07947-9