Abstract
Introduction
The prevalence of frailty among patients with chronic pancreatitis (CP) and its impact on clinical outcomes is unclear. We report the impact of frailty on mortality, readmission rates, and healthcare utilization among patients with chronic pancreatitis in the United States.
Methods
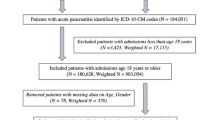
We extracted data on patients hospitalized with a primary or secondary diagnosis of CP from the Nationwide Readmissions Database 2019. We applied a previously validated hospital frailty risk scoring system to classify CP patients into frail and non-frail on index hospitalization and compared the characteristics of frail and non-frail patients. We studied the impact of frailty on mortality, readmission, and healthcare utilization.
Results
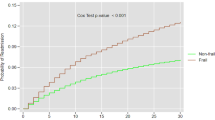
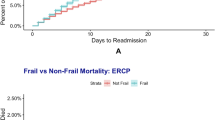
Of 56,072 patients with CP, 40.78% of patients were classified as frail. Frail patients experienced a higher rate of unplanned and preventable hospitalizations. Almost two-thirds of frail patients were younger than 65, and one-third had no or only single comorbidity. On multivariate analysis, frailty was independently associated with two times higher mortality risk (adjusted hazard ratio [aHR], 2.05; 95% CI 1.7–2.5). Frailty was also associated with a higher risk of all-cause readmission with an aHR of 1.07; (95% CI 1.03–1.1). Frail patients experienced a longer length of stay, higher hospitalization costs, and hospitalization charges. Infectious causes were the most common cause of readmission among frail patients compared to acute pancreatitis among non-frail patients.
Conclusions
Frailty is independently associated with higher mortality, readmission rates, and healthcare utilization among patients with chronic pancreatitis in the US.


Similar content being viewed by others
References
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. The Lancet. 2013;381:752–762.
Qian AS, Nguyen NH, Elia J, Ohno-Machado L, Sandborn WJ, Singh S. Frailty is independently associated with mortality and readmission in hospitalized patients with inflammatory bowel diseases. Clinical Gastroenterology and Hepatology. 2021;19:2054–63.e14.
Kim S, Han H, Jung H, Kim K, Hwang D, Kang S. Multidimensional frailty score for the prediction of postoperative mortality risk. JAMA Surgery. 2014;149:633.
Conroy S, Dowsing T. The ability of frailty to predict outcomes in older people attending an acute medical unit. Acute Medicine Journal. 2013;12:74–76.
Haley MN, Wells YD, Holland AE. Relationship between frailty and discharge outcomes in subacute care. Australian Health Review. 2013;38:25–29.
McAdams-DeMarco MA, Law A, Salter ML et al. Frailty and early hospital readmission after kidney transplantation. American Journal of Transplantation. 2013;13:2091–2095.
Murali-Krishnan R, Iqbal J, Rowe R, Parviz Y, Sultan A, Gunn J. Impact of Frailty on Length of Hospital Stay After Percutaneous Coronary Intervention. Heart. 2014;100:A451–A45.
Kahlon S, Pederson J, Majumdar SR, Belga S, Lau D, Fradette M et al. Association between frailty and 30-day outcomes after discharge from hospital. Cmaj. 2015;187:799–804.
Wallis S, Wall J, Biram R, Romero-Ortuno R. Association of the clinical frailty scale with hospital outcomes. QJM: An International Journal of Medicine. 2015;108:943–9.
Juma S, Taabazuing M-M, Montero-Odasso M. Clinical frailty scale in an acute medicine unit: a simple tool that predicts length of stay. Canadian Geriatrics Journal. 2016;19:34.
de la Iglesia D, Vallejo-Senra N, López-López A, Iglesias-Garcia J, Lariño-Noia J, Nieto-García L et al. Pancreatic exocrine insufficiency and cardiovascular risk in patients with chronic pancreatitis: A prospective, longitudinal cohort study. Journal of Gastroenterology and Hepatology. 2019;34:277–283.
Martínez-Moneo E, Stigliano S, Hedström A, Kaczka A, Malvik M, Waldthaler A et al. Deficiency of fat-soluble vitamins in chronic pancreatitis: A systematic review and meta-analysis. Pancreatology. 2016;16:988–994.
Olesen SS, Frandsen LK, Poulsen JL, Vestergaard P, Rasmussen HH, Drewes AM. The prevalence of underweight is increased in chronic pancreatitis outpatients and associates with reduced life quality. Nutrition. 2017;43:1–7.
Stigliano S, Waldthaler A, Martinez-Moneo E, Lionetto L, Robinson S, Malvik M, et al. (2018) Vitamins D and K as factors associated with osteopathy in chronic pancreatitis: a prospective multicentre study (P-BONE study). Clinical and Translational Gastroenterology. 9
Tignor AS, Wu BU, Whitlock TL, Lopez R, Repas K, Banks PA et al. High prevalence of low-trauma fracture in chronic pancreatitis. Official journal of the American College of Gastroenterology ACG. 2010;105:2680–6.
Vujasinovic M, Hedström A, Maisonneuve P, Valente R, von Horn H, Löhr J-M et al. Zinc deficiency in patients with chronic pancreatitis. World Journal of Gastroenterology. 2019;25:600.
Zhu X, Liu D, Wei Q, Lin H, Zhi M, Chen Y et al. New-onset diabetes mellitus after chronic pancreatitis diagnosis: a systematic review and meta-analysis. Pancreas. 2019;48:868–875.
Peery AF, Crockett SD, Barritt AS, Dellon ES, Eluri S, Gangarosa LM et al. Burden of gastrointestinal, liver, and pancreatic diseases in the United States. Gastroenterology. 2015;149:1731–41. e3.
McNabb-Baltar J, Chang MS, Suleiman SL, Banks PA, de Silva DPS. A time trend analysis of CT and MRI scan imaging in acute pancreatitis patients presenting to US emergency departments. The American Journal of Emergency Medicine. 2018;36:1709–1710.
Yadav D, Timmons L, Benson JT, Dierkhising RA, Chari ST. Incidence, prevalence, and survival of chronic pancreatitis: a population-based study. Official Journal of the American College of Gastroenterology ACG. 2011;106:2192–9.
Shah R, Haydek C, Mulki R, Qayed E. Incidence and predictors of 30-day readmissions in patients hospitalized with chronic pancreatitis: A nationwide analysis. Pancreatology. 2018;18:386–393.
Garg SK, Sarvepalli S, Campbell JP, Anugwom C, Singh D, Wadhwa V et al. Incidence and predictors of 30-day readmission among patients hospitalized for chronic pancreatitis. Pancreas. 2018;47:1008–1014.
2014 Introduction to the NRD. Healthcare Cost and Utilization Project (HCUP). December 2016. Agency for Healthcare Research and Quality, Rockville, MD. [Available from: www.hcup-us.ahrq.gov/db/nation/nrd/NRD_Introduction_2014.jsp.
Overview. N. Healthcare Cost and Utilization Project (HCUP) (2021). Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/nrdoverview.jsp
Gilbert T, Neuburger J, Kraindler J et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. The Lancet. 2018;391:1775–1782.
HCUP NIS Description of Data Elements. Healthcare Cost and Utilization Project (HCUP). September 2008. Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/db/vars/aprdrg/nisnote.jsp
McCormick PJ, Lin HM, Deiner SG, Levin MA. Validation of the all patient refined diagnosis related group (APR-DRG) risk of mortality and severity of illness modifiers as a measure of perioperative risk. Journal of Medical Systems. 2018;42:1–6.
Elgwairi E, Yang S, Nugent K. Association of the all-patient refined diagnosis-related groups severity of illness and risk of mortality classification with outcomes. Southern Medical Journal. 2021;114:668–674.
Agency for Healthcare Research and Quality Prevention Quality Indicators Technical Specifications Updates Version v2021 (ICD 10-CM/PCS). Agency for Healthcare Research and Quality, Rockville, MD2018 ( https://qualityindicators.ahrq.gov/Modules/Log_Coding_Updates_PQI_v2021.aspx Published 20201. Accessed December 2nd, 2021)
Stata F. How can I check for collinearity in survey regression. UCLA: Academic Technology Services, Statistical Consulting Group from http://www.ats.ucla.edu/stat/stata/faq/svycollin.htm (Accessed October 5, 2010). 2010.
Krumholz HM. Post-hospital syndrome–a condition of generalized risk. The New England Journal of Medicine. 2013;368:100.
McIlvennan CK, Eapen ZJ, Allen LA. Hospital readmissions reduction program. Circulation. 2015;131:1796–1803.
Hughes LD, Witham MD. Causes and correlates of 30 day and 180 day readmission following discharge from a medicine for the elderly rehabilitation unit. BMC Geriatrics. 2018;18:1–10.
Khot UN, Johnson MJ, Wiggins NB et al. Long-term time-varying risk of readmission after acute myocardial infarction. Journal of the American Heart Association. 2018;7:e009650.
Kuan LL, Dennison AR, Garcea G. Prevalence and Impact of Sarcopenia in Chronic Pancreatitis: A Review of the Literature. World Journal of Surgery. 2021;45:590–597.
Olesen SS, Büyükuslu A, Køhler M, Rasmussen HH, Drewes AM. Sarcopenia associates with increased hospitalization rates and reduced survival in patients with chronic pancreatitis. Pancreatology. 2019;19:245–251.
Seicean A, Tantău M, Grigorescu M, Mocan T, Seicean R, Pop T. Mortality risk factors in chronic pancreatitis. Journal of Gastrointestinal and Liver Diseases: JGLD. 2006;15:21–26.
Hersh AM, Pennington Z, Hung B, Patel J, Goldsborough E, Schilling A et al. Comparison of frailty metrics and the Charlson Comorbidity Index for predicting adverse outcomes in patients undergoing surgery for spine metastases. Journal of Neurosurgery: Spine. 2021;1:1–9.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2004;59:M255–M263.
Xiao AY, Tan ML, Plana MN, Yadav D, Zamora J, Petrov MS. (2018) The use of international classification of diseases codes to identify patients with pancreatitis: a systematic review and meta-analysis of diagnostic accuracy studies. Clinical and Translational Gastroenterology. 9.
Spanier BM, Schreuder D, Dijkgraaf MG, Bruno MJ. Source validation of pancreatitis-related hospital discharge diagnoses notified to a national registry in the Netherlands. Pancreatology. 2008;8:498–503.
O’malley KJ, Cook KF, Price MD, Wildes KR, Hurdle JF, Ashton CM. Measuring diagnoses: ICD code accuracy. Health Services Research. 2005;40:1620–39.
Author information
Authors and Affiliations
Contributions
VK: Study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript. EB: Interpretation of data, Critical revision of the manuscript for important intellectual content; administrative and material support. DXJ: Interpretation of data, Critical revision of the manuscript for important intellectual content. PB: Critical revision of the manuscript for important intellectual content; study supervision. JM: Study concept and design; drafting of the manuscript; critical revision of the manuscript for important intellectual content; study supervision. All authors approved the final version to be published.
Corresponding author
Ethics declarations
Conflict of interest
Barkoudah, Ebrahim: Dr. Barkoudah reports research support payments from the National Institutes of Health/National Heart, Lung, and Blood Institute, Bristol Myers Squibb and Janssen, payments made to Brigham and Women's Hospital for performing clinical endpoints sponsored by various entities and Advisory Board fees from Bristol Myers Squibb, Janssen, Novartis, Pfizer and Portola, and travel expenses from Alexion. McNabb-Baltar, Julia: Dr McNabb-Baltar reports research support from Healthvibe and Advisory Board fees from Nestle Health. Vivek Kumar, David X Jin, Peter Banks have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kumar, V., Barkoudah, E., Jin, D.X. et al. Hospital Frailty Risk Score (HFRS) Predicts Adverse Outcomes Among Hospitalized Patients with Chronic Pancreatitis. Dig Dis Sci 68, 2890–2898 (2023). https://doi.org/10.1007/s10620-023-07946-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-07946-w