Abstract
Introduction
Colorectal cancer screening continuously decreased its mortality and incidence. In 2010, the Affordable Care Act extended Medicaid eligibility to low-income and childless adults. Some states elected to adopt Medicaid at different times while others chose not to. Past studies on the effects of Medicaid expansion on colorectal cancer screening showed equivocal results based on short-term data following expansion.
Aims
To examine the long-term impact of Medicaid expansion on colorectal cancer screening among its targeted population at its decade mark.
Methods
Behavioral Risk Factor Surveillance System data were extracted for childless adults below 138% federal poverty level in states with different Medicaid expansion statuses from 2012 to 2020. States were stratified into very early expansion states, early expansion states, late expansion states, and non-expansion states. Colorectal cancer screening prevalence was determined for eligible respondents. Difference-in-differences analyses were used to examine the effect of Medicaid expansion on colorectal cancer screening in states with different expansion statuses.
Results
Colorectal cancer screening prevalence in very early, early, late, and non-expansion states all increased during the study period (40.45% vs. 48.14%, 47.52% vs 61.06%, 46.06% vs 58.92%, and 43.44% vs 56.70%). Difference-in-differences analysis showed significantly increased CRC screening prevalence in very early expansion states during 2016 compared to non-expansion states (Crude difference-in-differences + 16.45%, p = 0.02, Adjusted difference-in-differences + 15.9%, p = 0.03). No statistical significance was observed among other years and groups.
Conclusions
Colorectal cancer screening increased between 2012 and 2020 in all states regardless of expansion status. However, Medicaid expansion is not associated with long-term increased colorectal cancer screening prevalence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the second most common cause of cancer death in the United States.1 Routine screening for CRC has been proven to be a cost-effective approach in reducing both its incidence and mortality [1,2,3]. Guidelines from the U.S. Preventive Services Task Force (USPSTF) endorse the use of multiple modalities of endoscopy and fecal testing for CRC screening [3]. Despite so, the prevalence of up-to-date CRC screening is estimated to be around 60% [1]. Patients who are among racial and ethnic minorities, economically disadvantaged, and underinsured showed a disproportionately lower screening prevalence [1].
Medicaid is a federal and state health program that provides health insurance to U.S. patients with low income and limited resources [4, 5]. Historically, Medicaid was only available to selected populations, including children, parents with dependents, pregnant women, persons older than 65 with conditions not covered by Medicare, and those with income well below the federal poverty level (FPL). The “working poor” represents a large population who could not receive adequate insurance coverage from their employer yet also would not qualify for Medicaid’s strict historical enrollment criteria. In 2010, the passage of the Patient Protection and Affordable Care Act (ACA) included several provisions aimed at increasing access to health care for this population [6]. One of its provisions was the expansion of Medicaid eligibility to include all adults earning < 138% of the FPL [7]. The expansion supports low-income adults without dependents to obtain affordable health insurance. As of July 2018, 34 states (including the District of Columbia) opted to expand Medicaid eligibility. Six very early expansion states expanded Medicaid eligibility prior to 2012; however, the majority of participating states expanded Medicaid coverage on January 1, 2014 [8].
The selective and asynchronous adoption of Medicaid expansion has created an opportunity to study the health care outcomes of its targeted populations, those that exhibit risk factors for lower compliance with CRC screening. Prior literature suggested that Medicaid expansion is associated with earlier stage of CRC diagnosis and increased CRC survival [9,10,11]. However, evaluations to date have not consistently demonstrated a positive association with Medicaid expansion and CRC screening [12,13,14,15,16,17,18,19]. State-level and national data utilizing different databases have generated inconsistent results, with a majority of the studies indicating an increased CRC screening and colonoscopy use immediately after Medicaid expansion. A small number of studies, on the other hand, suggested no significant impact from Medicaid expansion on CRC screening. Nonetheless, understanding of the long-term effect of Medicaid expansion on CRC screening is still lacking. As we approach the decade mark of Medicaid expansion under the ACA, we aimed to investigate the long-term impact of Medicaid expansion on CRC screening among its targeted population of low-income childless adults [5, 20]. We aimed to answer the question of how the prevalence of CRC screening changed long-term since Medicaid expansion between states with different expansion timeline in its targeted population. We hypothesized observing higher CRC screening in this population among states that adopted Medicaid expansion earlier.
Materials and Methods
Population Source
We used the Behavioral Risk Factor Surveillance System (BRFSS), a joint initiative of the Centers for Disease Control (CDC) and the U.S states/territories and the world’s longest continuously conducted health survey via phone. The survey is administered annually and provides nationally representative estimates via a complex sampling design that incorporates iterative proportional fitting to account for cellphone respondents. Patient responses are weighted by age, gender, race/ethnicity, level of education, marital status, property ownership, and telephone ownership. Data from the BRFSS were extracted for the years 2012, 2014, 2016, 2018, and 2020. These data represent non-overlapping annual cohorts and reflect respondent-reported health behaviors. The median response rates for the 2012, 2014, 2016, 2018, and 2020 BRFSS surveys were 46%, 47%, 47%, 50%, and 48% respectively.
Study Population
We chose to limit our study population to childless adults age greater than or equal to 18 but less than 65 (not Medicare eligible) and living in the 50 states and the District of Columbia (hereafter referred to as a state); earning < 138% of FPL (newly eligible for Medicaid under ACA provisions in expansion states); and eligible for colon cancer screening.
This cohort was selected for several reasons. First, Medicaid FPL eligibility criteria for parents of dependent children varied widely pre-ACA, and thus, it is difficult to adjust for the magnitude of eligibility expansion in this cohort. Second, as part of the ACA’s Medicaid expansion, states were required to cover, without cost sharing, all adult preventive services recommended by the USPSTF (grade A or B) and the CDC’s Advisory Committee on Immunization Practices [21]. However, this stipulation only applied to adults who were newly eligible for Medicaid and did not by statute extend to those who were previously enrolled in traditional Medicaid pre-ACA expansion (i.e., parents of dependent children) [21]. Although some states did opt for offering the recommended preventive services without cost-sharing to previously enrolled beneficiaries, this was not uniformly adopted [21].
Outcome Measures and Covariates
The primary outcome of interest was self-reported prevalence of colon cancer screening among childless adult patients living below 138% of the FPL in NES, VEES, EES, and LES in each of the survey years.
Covariates included year, age, race, marital status, education, smoking status, FPL, and state expansion status. FPL was determined by applying Department of Health and Human Services criteria to the estimated household income and calculated household size. Detailed methodology and codes utilized to calculate FPL could be found in the “Appendix.” Cancer screening eligibility was determined by age, gender, and lack of a condition or prior history that would preclude screening. The receipt of appropriate CRC screening is determined to be adults aged 50–64 without prior history of colon cancer, who received a fecal occult blood test within the past year, or sigmoidoscopy within the past 5 years and an FOBT within the past three years, or colonoscopy within the past 10 years. Based on publicly available information regarding Medicaid expansion status and dates of expansion, three state groupings were created: Non-expansion states (NES), Very Early Expansion States (VEES) Early Expansion States (EES), and Late Expansion States (LES). Further details regarding classification of VEES, EES, LES, and NES can be found in the “Appendix.”
Statistical Analyses
Baseline descriptive statistics were derived for each covariate, stratified by state expansion status and compared via the Chi-Square test. CRC screening prevalence was calculated in each survey year between VEES, EES, LES, and NES from 2012 to 2020.
Difference-in-differences (DID) analyses, a quasi-experimental approach comparing the changes in outcomes between the treatment group and control group over the time periods before and after the intervention, were utilized to examine the effect of Medicaid Expansion under the ACA on CRC prevalence. Subsequently, adjusted DID analyses were conducted using multivariable logistic regression. Each multivariate model included state expansion status, year, and an interaction term of state expansion status and year, adjusting for age, sex, race, and marital status. The coefficient of this interaction term represents the DID estimator. Crude DID was also calculated using the multivariable logistic regression without adjusting for covariates.
Two-sided significance levels were set at p < 0.05. Statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). Complex sampling design was accounted for to obtain population-level estimates.
Results
Baseline Demographics
A weighted estimate of 5.4 million (n = 14,725), 6.8 million (n = 16,556), 7.8 million (n = 16,227), 7.6 million (n = 13,972), and 7.6 million (n = 12,275) respondents met the USPSTF recommended CRC screening criteria respectively from the 2012, 2014, 2016, 2018, and 2020 BRFSS surveys. Baseline characteristics of these cohorts stratified into states with different expansion statuses are listed in Table 1.
Difference-in-Differences Analysis
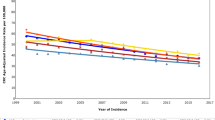
Overall, the CRC screening prevalence were 40.45%, 47.52%, 46.06%, and 43.44% for VEES, EES, LES, and NES prior to expansion and increased to 48.14%, 61.06%, 58.92%, and 56.70% a decade later after expansion. DID analysis did not show significant difference in changes in screening prevalence immediately after expansion in 2014. In 2016, following the late expansion, there were significant increases in the proportion of respondents in VEES undergoing CRC screening (Crude difference-in-differences 16.45%, p = 0.02, Adjusted difference-in-differences + 15.9%, p = 0.03) compared to respondents in NES (Fig. 1, Table 2). Such difference was not found between other expanding states and NES. Furthermore, in year 2018 and 2020, we did not find any statistically significance in crude and adjusted change in CRC screening prevalence in expansion states (VEES, EES, and LES) compared to NES.
Discussion
The selective adoption of the ACA’s Medicaid expansion to adults living at < 138% of the FPL provides an opportunity to elucidate the impact of access to health insurance on a vulnerable segment of the population. While it continues to influence health care [22], economics [23], and civic matters [24], our understanding of the policy’s direct impact on CRC screening has remained elusive. As we approach the decade mark since the passage of ACA, we examined the long-term effect of ACA on CRC screening. We limited our analysis to those who were newly eligible to Medicaid after the passage of ACA: low income, childless, adults earning < 138% of the FPL. Our results highlighted two key findings. First, we found significantly higher screening prevalence among all states in this population regardless of expansion status since the passage of ACA. Second, a higher increase in CRC screening prevalence was observed in 2016 among VEES compared to NES. However, different from our hypothesis of continuously observing similar effects long-term, such effects from Medicaid expansion were no longer present in the years to follow.
Regardless of the adoption of Medicaid expansion, we found that all states have showed a significantly higher prevalence of CRC screening since the passage of ACA. With the rapid acceptance of colonoscopy since early 2000s, CRC screening prevalence has been steadily increasing while CRC mortality continues to decline [1, 25]. A national CRC screening prevalence of 68% was reported in recent data. Our results matched the national trend of increasing utilization of CRC screening. However, the childless low-income population we included in this study showed consistently lower than expected screening prevalence throughout the study period. Known risk factors such as higher rate of being without insurance, insured by Medicaid, and at lower-income brackets that are innate to the chosen study population likely have contributed the observed inequalities [1, 26, 27]. Our cohort are also more likely to belong to groups of lower education levels and racial minorities, who may suffer from the lack of access to a consistent provider for screening. Past studies also suggested that, up to 24% of Medicaid-eligible population among early Medicaid-expanding states were yet to enroll into Medicaid, which could also contribute to the low CRC screening prevalence observed in our study population, particularly those in VEES [28, 29]. Several proposed explanations included perceived unaffordability of health care by those with suboptimal health conditions, barriers to enrollment into Medicaid, and job changes contributing to loss of Medicaid coverage [29]. While the CRC screening prevalence corroborated the national trend of improved preventative health behaviors, significant inequalities still exist within the population targeted by ACA a decade after its passage.
After observing a more rapid increase in CRC screening prevalence in VEES in 2016, we did not find a similar statistical significance from our difference-in-differences analysis in the 4 years following. Prior literature on ACA’s effect on CRC screening vary in their designs and study period and showed miscellaneous results. While a significant number of past studies suggested increased CRC screening among states with earlier Medicaid expansion times, others suggested no significant changes [10, 16, 17, 30,31,32,33,34,35,36,37]. Most of these studies utilized data within 2 years immediately after Medicaid expansion with rare ones seeing beyond short-term effects. Among those, Fedewa et al. studied the utilization of cancer screening among adults with income below 138% FPL up to 2016. Similar to our results, they found significantly increased prevalence of CRC screening in 2016 among states that expanded Medicaid before 2014 [36]. Hendryx et al. studied the rate of colonoscopies performed among individuals with income < $20,000 and found a significant 1.12 odds ratio of colonoscopy use in year 2016 compared to 2012 [37]. To our knowledge, we added to existing literature as the first analysis studying the long-term impact of Medicaid expansion on CRC screening. Compared to prior studies, the population of our study was more stringent as we included only childless adults < 138% of FPL with the hope to precisely isolate a subpopulation that would likely receive the greatest benefit from Medicaid expansion. Our results corroborated a similar increase in CRC screening among VEES during relatively early years after Medicaid expansion [36, 37]. At the same time, our analysis helped clarify that such difference in screening prevalence associated with Medicaid expansion did not persist in the long run.
While different from our initial hypothesis of observing long-term increase of CRC screening in states that adopted Medicaid expansion earlier, our findings can be interpreted from various angles. One possible explanation of our observed trends is that although Medicaid expansion significantly improved CRC screening prevalence in its targeted population during early years, an overall increase in public awareness in cancer screening likely diluted the effect from Medicaid expansion. Although multiple studies have demonstrated a larger increase in health insurance coverage in states that adopted Medicaid expansion, insurance coverage does not always translate to an increase in preventative health behaviors. Conversely, national data suggested that being covered by Medicaid as primary insurance is linked to a CRC screening prevalence of around 53% [1]. A variety of patient-level factors not captured by our database could also have contributed. For example, the lack of recommendation from physician, recommendation of only colonoscopy as the method of screening, lack of awareness of the need to be screened, fear and unwantedness, expense, and inability to take time off work were patient-reported factors that have been shown to reduce screening prevalence [38]. A high level of awareness and knowledge of CRC screening does not always translate to high participation rates in screening [39]. Another possible explanation is that ACA provided federal subsidies to purchase health insurance for individuals earning between 100 and 138% of FPL. These federal subsidies may have mitigated the lack of expansion for this cohort [40]. However, a sensitivity analysis with individuals within incomes below 100% FPL did not show significance, making such hypothesis less likely (“Appendix”).
The impact of COVID-19 pandemic should also be accounted for when our results are being interpreted. Job security was highly impacted within low-wage service workers when COVID-19 recession peaked in 2020 [41]. The recent literature suggested an additional 5 million people covered nationally within 6 months after the economic shutdown that took place in March 2020 [42, 43]. Factors such as reduced work hours likely qualified more people for Medicaid; the maintenance of effort requirement passed by Congress in 2020 during the period of pandemic likely helped increase the overall proportion of Medicaid enrollees; the American Rescue Plan subsidized COBRA and exchange programs also likely helped improve access to care [42,43,44]. Such efforts provide layers of confounding that impact the access to care and cancer screening in our study population of interest, possibly correlating with the steep rise in CRC screening prevalence observed in many states in 2020 compared to 2018. With additional data capturing COVID-19 becoming available soon, we will be able to further elucidate its effect on preventative health.
Limitations
Ultimately, the findings of this work must be interpreted within the context of its limitations. First, the BRFSS survey is not administered to persons institutionalized or without telephone access. Although it is possible that some of these individuals would be eligible for Medicaid, these persons likely represent a minority of qualifying persons, and thus, their absence is unlikely to largely impact the results [45]. Second, BRFSS data are self-reported and, thus, subject to both recall and social desirability bias [45]. Lastly, it is possible that differences in trends between state cohorts reflect widening regional differences in patient-perceived benefits of preventive care rather than the effects of policy implementation. In addition to these general limitations inherent to all BRFSS analyses, there are several limitations specific to this work. Income data used in our FPL calculations were coded in ranges instead of precise numbers. However, this methodology has been previously utilized and accepted [5, 45, 46]. The 2012 BRFSS did not discern the number of household adults for cellphone respondents (a crucial component of the FPL calculation), and thus, cellphone respondents were not included in our 2012 BRFSS calculations. Greater detail regarding our decisions concerning these limitations can be found in the “Appendix.” Although the aforementioned limitations may hinder the precision of our estimates, it is unlikely that the reported trends and differences in trends are significantly misconstrued.
Conclusion
A decade after the passage of ACA, we provided one of the first analyses of the long-term effect of Medicaid expansion on CRC screening prevalence among childless adults below 138% FPL, a targeted population by the policy. While it was encouraging to find increased CRC screening prevalence among all states regardless of expansion status, no long-term effect of Medicaid Expansion was observed on CRC screening prevalence in this selected population. Additional studies are warranted to further elucidate the exact reasons underlying such observed trend.
Abbreviations
- ACA:
-
Affordable Care Act
- BRFSS:
-
Behavioral Risk Factor Surveillance System
- CRC:
-
Colorectal cancer
- NES:
-
Non-expansion states
- EES:
-
Early expansion states
- LES:
-
Late expansion states
- VEES:
-
Very early expansion states
- USPSTF:
-
United States Preventive Services Task Force
References
Siegel RL, Miller KD, Goding Sauer A et al. Colorectal cancer statistics, 2020. CA: A Cancer Journal for Clinicians. 2020;70:145–164.
Montminy EM, Karlitz JJ, Landreneau SW. Progress of colorectal cancer screening in United States: past achievements and future challenges. Prev Med. 2019;120:78–84. https://doi.org/10.1016/j.ypmed.2018.12.004.
Davidson KW, Barry MJ, Mangione CM et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. Jama. 2021;325:1965–1977.
Program History. Accessed November 20, 2017. https://www.medicaid.gov/about-us/program-history/index.html
Sabik LM, Tarazi WW, Hochhalter S, Dahman B, Bradley CJ. Medicaid expansions and cervical cancer screening for low-income women. Health Services Research. 2017. https://doi.org/10.1111/1475-6773.12732.
Patient Protection and Affordable Care Act, §18001–18121, 2010.
Medicaid expansion & what it means for you. Accessed November 20, 2017. https://www.healthcare.gov/medicaid-chip/medicaid-expansion-and-you/
Status of State Action on the Medicaid Expansion Decision. Accessed November 20, 2017. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
Lissenden B, Yao NA. Affordable care act changes to medicare led to increased diagnoses of early-stage colorectal cancer among seniors. Health Affairs. 2017;36:101–36107. https://doi.org/10.1377/hlthaff.2016.0607.
Gan T, Sinner HF, Walling SC et al. Impact of the affordable care act on colorectal cancer screening, incidence, and survival in Kentucky. J Am Coll Surg. 2019;228:342–353. https://doi.org/10.1016/j.jamcollsurg.2018.12.035.
Jemal A, Lin CC, Davidoff AJ, Han X. Changes in insurance coverage and stage at diagnosis among nonelderly patients with cancer after the Affordable Care Act. J Clin Oncol. 2017;35:3906–3915. https://doi.org/10.1200/JCO.2017.73.7817.
Mehta SJ, Polsky D, Zhu J et al. ACA-mandated elimination of cost sharing for preventive screening has had limited early impact. Am J Manag Care. 2015;21:511.
Cooper GS, Kou TD, Schluchter MD, Dor A, Koroukian SM. Changes in receipt of cancer screening in medicare beneficiaries following the Affordable Care Act. J Natl Cancer Inst. 2016;108:374. https://doi.org/10.1093/jnci/djv374.
Hong Y-R, Jo A, Mainous AG, III. Up-to-date on preventive care services under Affordable Care Act: a trend analysis from MEPS 2007–2014. Med Care. 2017;55.
Wharam JF, Zhang F, Landon BE, LeCates R, Soumerai S, Ross-Degnan D. Colorectal cancer screening in a nationwide high-deductible health plan before and after the Affordable Care Act. Med Care. 2016;54(5).
Huguet N, Angier H, Rdesinski R et al. Cervical and colorectal cancer screening prevalence before and after Affordable Care Act Medicaid expansion. Prev Med. 2019;124:91–97. https://doi.org/10.1016/j.ypmed.2019.05.003.
Fedewa SA, Goodman M, Flanders WD et al. Elimination of cost-sharing and receipt of screening for colorectal and breast cancer. Cancer. 2015;121:3272–3280.
Fedewa SA, Yabroff KR, Smith RA, Goding Sauer A, Han X, Jemal A. Changes in breast and colorectal cancer screening after medicaid expansion under the Affordable Care Act. Am J Prev Med. 2019;57:3–12. https://doi.org/10.1016/j.amepre.2019.02.015.
Zerhouni YA, Trinh Q-D, Lipsitz S et al. Effect of Medicaid expansion on colorectal cancer screening rates. Dis Colon Rectum. 2019;62:97–103.
Wright BJ, Conlin AK, Allen HL, Tsui J, Carlson MJ, Li HF. What does Medicaid expansion mean for cancer screening and prevention? Results from a randomized trial on the impacts of acquiring Medicaid coverage. Cancer. 2016;122:791–797. https://doi.org/10.1002/cncr.29802.
Gates A, Ranji U, Synder L. Coverage of Preventive Services for Adults in Medicaid. 2014. The Kaiser Commission on Medicaid and the Uninsured. https://www.kff.org/medicaid/issue-brief/coverage-of-preventive-services-for-adults-in-medicaid/
Long SK, Bart L, Karpman M, Shartzer A, Zuckerman S. Sustained gains in coverage, access, and Affordability Under The ACA: A 2017 Update. Health Aff. 2017;36:1656–1662. https://doi.org/10.1377/hlthaff.2017.0798.
Caswell KJ, Waidmann TA. The Affordable Care Act medicaid expansions and personal finance. Med Care Res Rev. 2017. https://doi.org/10.1177/1077558717725164.
Clinton JD, Sances MW. The politics of policy: the initial mass political effects of medicaid expansion in the states. Am Polit Sci Rev. 2017. https://doi.org/10.1017/S0003055417000430.
Zauber AG. The impact of screening on colorectal cancer mortality and incidence: has it really made a difference? Dig Dis Sci. 2015;60:681–691.https://doi.org/10.1007/s10620-015-3600-5.
Jandorf L, Ellison J, Villagra C et al. Understanding the barriers and facilitators of colorectal cancer screening among low income immigrant Hispanics. J Immigr Minority Health. 2010;12:462–469.
Xu MR, Kelly AMB, Kushi LH, Reed ME, Koh HK, Spiegelman D. Impact of the Affordable Care Act on colorectal cancer outcomes: a systematic review. Am J Prev Med. 2020;58:596–603. https://doi.org/10.1016/j.amepre.2019.11.018.
Buettgens M. The Implications of Medicaid Expansion in the Remaining States: 2018 Update. Final Report to The Urban Insti tute tinyurl com/y87ev89u Retrieved August. 2018;3:2018.
Ermer T, Walters SL, Canavan ME et al. Understanding the implications of medicaid expansion for cancer care in the US: a review. JAMA. 2022;8:139–148.
Goold SD, Tipirneni R, Chang T et al. Primary care, health promotion, and disease prevention with Michigan Medicaid expansion. J Gen Internal Med. 2020;35:800–807.
Wharam JF, Zhang F, Landon BE, LeCates R, Soumerai S, Ross-Degnan D. Colorectal cancer screening in a nationwide high-deductible health plan before and after the Affordable Care Act. Med Care. 2016;54(5):466–473.
Cole MB, Galárraga O, Wilson IB, Wright B, Trivedi AN. At federally funded health centers, Medicaid expansion was associated with improved quality of care. Health Aff. 2017;36(1):40–48.
Hong Y-R, Jo A, Mainous AG. Up-to-date on preventive care services under Affordable Care Act. Med Care. 2017;55(8):771–780.
Jensen GA, Salloum RG, Hu J, Ferdows NB, Tarraf W. A slow start: Use of preventive services among seniors following the Affordable Care Act’s enhancement of Medicare benefits in the US. Prev Med. 2015;76:37–42. https://doi.org/10.1016/j.ypmed.2015.03.023.
Cooper GS, Kou TD, Dor A, Koroukian SM, Schluchter MD. Cancer preventive services, socioeconomic status, and the Affordable Care Act. Cancer. 2017;123:1585–1589.
Fedewa SA, Yabroff KR, Smith RA, Sauer AG, Han X, Jemal A. Changes in breast and colorectal cancer screening after Medicaid expansion under the Affordable Care Act. Am J Prev Med. 2019;57:3–12.
Hendryx M, Luo J. Increased cancer screening for low-income adults under the Affordable Care Act Medicaid expansion. Med Care. 2018;56:944–949.
Jones RM, Devers KJ, Kuzel AJ, Woolf SH. Patient-reported barriers to colorectal cancer screening: a mixed-methods analysis. Am J Prev Med. 2010;38:508–516. https://doi.org/10.1016/j.amepre.2010.01.021.
Brandt HM, Dolinger HR, Sharpe PA, Hardin JW, Berger FG. Relationship of colorectal cancer awareness and knowledge with colorectal cancer screening. Colorectal Cancer. 2012;1:383–396. https://doi.org/10.2217/crc.12.45.
McMorrow S, Gates JA, Long SK, Kenney GM. Medicaid expansion increased coverage, improved affordability, and reduced psychological distress for low-income parents. Health Aff. 2017;36:808–818. https://doi.org/10.1377/hlthaff.2016.1650.
Bartik AW, Bertrand M, Lin F, Rothstein J, Unrath M. Measuring the labor market at the onset of the COVID-19 crisis. 2020.
Frenier C, Nikpay SS, Golberstein E. COVID-19 has increased medicaid enrollment, but short-term enrollment changes are unrelated to job losses: study examines influence COVID-19 may have had on Medicaid enrollment covering the period of March 1 through June 1, 2020 for 26 states. Health Aff. 2020;39:1822–1831.
Khorrami P, Sommers BD. Changes in US Medicaid enrollment during the COVID-19 pandemic. JAMA Netw Open. 2021;4:e219463–e219463.
Bundorf MK, Gupta S, Kim C. Trends in US health insurance coverage during the COVID-19 pandemic. American Medical Association; 2021:e212487.
Okoro CA, Zhao G, Fox JB, Eke PI, Greenlund KJ, Town M. Surveillance for health care access and health services use, adults aged 18–64 years—behavioral risk factor surveillance system, United States. Morb Mortal Wkl Rep Surveill Summar. 2014;2017:661–742. https://doi.org/10.15585/mmwr.ss6607a1.
Sammon JD, Serrell EC, Karabon P et al. Prostate cancer screening in early medicaid expansion states. J Urol. 2017. https://doi.org/10.1016/j.juro.2017.07.083.
https://aspe.hhs.gov/prior-hhs-poverty-guidelines-and-federal-register-references. Accessed November 1, 2017.
Sabik LM, Tarazi WW, Hochhalter S, Dahman B, Bradley CJ. Medicaid expansions and cervical cancer screening for low-income women. Health Serv Res. 2017;53:2870–2891.
Sammon JD, Serrell EC, Karabon P, et al. Prostate cancer screening in early medicaid expansion states. J Urol. 2017.
Gates A, Ranji U, Synder L. Coverage of Preventive Services for Adults in Medicaid. The Henry J. Kaiser Family Foundation; 2014.
Funding
QDT reports personal fees from Astellas, Bayer, and Janssen, outside the submitted work. QDT reports research funding from the American Cancer Society, the Defense Health Agency, and Pfizer Global Medical Grants. APC reports research funding from the American Cancer Society and Pfizer Global Medical Grants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors of this paper do not have conflicts of interest that would influence the results of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix
Determination of State Medicaid Expansion Cohorts
States were grouped into four categories by expansion status as of March 2022: Non-expansion states (NES), Very Early Expansion States (VEES), Early Expansion States (EES), and Late Expansion States (LES) (Appendix Table 1). A few states adopted Medicaid expansion very recently between year 2019 and 2020 and were classified as NES for the purpose of this study. (Appendix Table 1).
Federal Poverty Level Calculations
Given our interest in the effects of Medicaid expansion on cancer screening behaviors, our analysis includes only respondents newly eligible for Medicaid under the ACA’s expansion provisions, namely childless adults living at < 138% of the Federal Poverty Level (FPL). FPL values are a function of a household’s income and number of occupants and are adjusted and published annually by the U.S. Department of Health and Human Services [47]. Federal poverty levels have been previously calculated from the BRFSS as described in the methodology outlined by Sabik et al. and Sammon et. al. [48, 49].
Household Income Determination
Household income (INCOME2) is reported as a range, and consistent with previous methodology, each respondent was assigned an income corresponding to the middle value of their reported income range. For respondents earning > $75,000, an income of $100,000 was assigned consistent with previously employed methods (Appendix Table 2).
Household Size Determination
For survey years 2014 through 2020, the QSTVER variable identified the route of survey administration (landline or cellphone). The NUMADULT and HHADULT variables reported the number of adults in the household for landline and cellphone respondents, respectively. The CHILDREN variable denotes the number of dependent children living in the household. Respondents were not included if the value for the CHILDREN variable was > 0.
Unfortunately, the 2012 survey did not query the number of adults living in the household for respondents who answered the survey via cellphone. After discussing various approaches to account for this absence, we opted to simply omit 2012 cellphone respondents from our analysis. While not ideal, the impact of this exclusion is less pronounced in 2012 where cellphone respondents only account for ~ 28% of the cohort. However, to understand the impact of this exclusion, we performed a Chi-Square test to compare the distribution of respondents within important covariate categories between landline and cellphone respondents in the 2012 survey (Appendix Table 3). Cellphone respondents were more likely to be younger, never married, Black or Hispanic, and current smokers. Additionally, cellphone respondents had lower median incomes and levels of educational attainment and were less likely to have health insurance or access to a personal physician. Rates of all three cancer screenings were also lower among cellphone respondents compared to landline respondents. Finally, the proportion of cellphone respondents was highest in non-expansion states and lowest in early expansion states. The knowledge of these trends allows for more accurate interpretation of figures. For all figures, the depicted 2012 BRFSS percentile estimates are likely, by varying degrees, slightly higher than the true population estimates. Therefore, while the exclusion of the cellphone respondents impacts the validity of the 2012 BRFSS estimates, it is unlikely that this exclusion would significantly alter the observed trends over time.
Appendix Table 1: Groupings of states by participation in ACA Medicaid expansion
Very Early Expansion States (between 3/1/2010–4/14/2011)
-
(1)
Minnesota
-
(2)
Connecticut
-
(3)
District of Columbia
-
(4)
California
-
(5)
Washington
-
(6)
New Jersey
Early Expansion States (between 1/1/2014–8/15/2014)
-
(1)
Arizona
-
(2)
Arkansas
-
(3)
Colorado
-
(4)
Delaware
-
(5)
Hawaii
-
(6)
Illinois
-
(7)
Iowa
-
(8)
Kentucky
-
(9)
Maryland
-
(10)
Massachusetts
-
(11)
Nevada
-
(12)
New Mexico
-
(13)
New York
-
(14)
North Dakota
-
(15)
Ohio
-
(16)
Oregon
-
(17)
Rhode Island
-
(18)
Vermont
-
(19)
West Virginia
-
(20)
Michigan
-
(21)
New Hampshire
Late Expansion States (between 1/1/2015–7/1/2016)
-
(1)
Pennsylvania
-
(2)
Indiana
-
(3)
Alaska
-
(4)
Montana
-
(5)
Louisiana
Non-Expansion (Not expanded before 2017)
-
(1)
Alabama
-
(2)
Florida
-
(3)
Georgia
-
(4)
Idaho (expanded on 1/1/2020)
-
(5)
Kansas
-
(6)
Maine (expanded on 1/10/2019)
-
(7)
Mississippi
-
(8)
Missouri (expanded on 10/1/2020)
-
(9)
Nebraska (expanded on 10/1/2020)
-
(10)
North Carolina
-
(11)
Oklahoma (expanded on 7/1/2020)
-
(12)
South Carolina
-
(13)
South Dakota
-
(14)
Tennessee
-
(15)
Texas
-
(16)
Utah (expanded on 1/1/2020)
-
(17)
Virginia (expanded on 1/1/2019)
-
(18)
Wisconsin
-
(19)
Wyoming [50]
Appendix Table 2: Assigned income values for each self-reported income range category (INCOME2). BRFSS 2012–2020
Income range (INCOME2) | Assigned income |
|---|---|
< $10,000 | $5000 |
$10,000–$15,000 | $12,500 |
$15,000–$20,000 | $17,500 |
$20,000–$25,000 | $22,500 |
$25,000–$35,000 | $30,000 |
$35,000–$50,000 | $42,500 |
$50,000–$75,000 | $62,500 |
> $75,000 | $100,000 |
Appendix Table 3: Baseline demographics of 2012 BRFSS Respondents < 65 years of age and living in the United States stratified by mode of survey administration
Landline respondents (n = 228,520) | Cellphone respondents (n = 88,327) | p value | |
|---|---|---|---|
Age category, (%) | < 0.0001 | ||
18–24 | 10.0 | 24.2 | |
25–29 | 5.3 | 16.6 | |
30–34 | 8.1 | 14.7 | |
35–39 | 9.0 | 10.3 | |
40–44 | 12.2 | 9.8 | |
45–49 | 12.0 | 7.5 | |
50–54 | 15.8 | 7.9 | |
55–59 | 13.7 | 5.2 | |
60–64 | 14.0 | 3.9 | |
Median income, (%) | < 0.0001 | ||
$5,0000 | 5.4 | 10.1 | |
$12,500 | 4.8 | 7.3 | |
$17,500 | 6.3 | 10.6 | |
$22,500 | 7.3 | 11.1 | |
$30,000 | 9.1 | 11.6 | |
$42,500 | 13.2 | 13.8 | |
$62,500 | 16.6 | 14.0 | |
$100,000 | 37.3 | 21.4 | |
Race, (%) | < 0.0001 | ||
White | 67.1 | 56.3 | |
Black | 11.0 | 14.3 | |
Asian | 5.1 | 4.5 | |
Hispanic | 13.8 | 20.9 | |
Other | 3.0 | 4.0 | |
Marital status, (%) | < 0.0001 | ||
Married | 59.5 | 34.3 | |
Never married | 26.3 | 48.9 | |
Divorced, widowed, separated, other | 14.1 | 16.7 | |
Education, (%) | < 0.0001 | ||
Less than high school | 12.2 | 17.0 | |
High school graduate | 27.6 | 28.5 | |
Some college | 30.9 | 32.0 | |
College graduate | 29.4 | 22.5 | |
Smoker, (%) | < 0.0001 | ||
Current smoker | 17.7 | 24.8 | |
Former smoker | 22.6 | 16.8 | |
Never smoker | 58.1 | 55.9 | |
Refused | 1.6 | 2.4 | |
Insurance coverage, (%) | < 0.0001 | ||
Yes | 82.8 | 70.0 | |
Personal physician, (%) | < 0.0001 | ||
Yes | 82.0 | 62.4 | |
Colon cancer screening, (%) | |||
Yes | 57.6 | 45.0 | < 0.0001 |
State expansion status, (%) | < 0.0001 | ||
Early expansion state | 66.3 | 33.7 | |
Late expansion state | 58.9 | 41.1 | |
Non-expansion state | 52.3 | 47.7 |
Appendix Table 4: Colon cancer screening questions excerpted from BRFSS 2012 to 2020
Question number | Question prompt and answer choices |
|---|---|
17.1 | A blood stool test is a test that may use a special kit at home to determine whether the stool contains blood. Have you ever had this test using a home kit? |
1. Yes | |
2. No | |
7. Don’t Know/Not Sure | |
9. Refused | |
17.2 | How long has it been since you had your last blood stool test using a home kit? |
1. Within the past year (anytime less than 12 months ago) | |
2. Within the past 2 years (1 year but less than 2 years ago) | |
3. Within the past 3 years (2 years but less than 3 years ago) | |
4. Within the past 5 years (3 years but less than 5 years ago) | |
5. 5 or more years ago | |
7. Don’t know/Not Sure | |
9. Refused | |
17.3 | Sigmoidoscopy and colonoscopy are exams in which a tube is inserted in the rectum to view the colon for signs of cancer or other health problems. Have you ever had either of these exams? |
1. Yes | |
2. No | |
7. Don’t Know/Not Sure | |
9. Refused | |
17.4 | For a SIGMOIDOSCOPY, a flexible tube is inserted into the rectum to look for problems. A COLONOSCOPY is similar, but uses a longer tube, and you are usually given medication through a needle in your arm to make you sleepy and told to have someone else drive you home after the test. Was your MOST RECENT exam a sigmoidoscopy or a colonoscopy? |
1. Sigmoidoscopy | |
2. Colonoscopy | |
7. Don’t know/Not Sure | |
9. Refused | |
17.5 | How long has it been since you had your last sigmoidoscopy or colonoscopy? |
1. Within the past year (anytime less than 12 months ago) | |
2. Within the past 2 years (1 year but less than 2 years ago) | |
3. Within the past 3 years (2 years but less than 3 years ago) | |
4. Within the past 5 years (3 years but less than 5 years ago) | |
5. Within the past 10 years (5 years but less than 10 years ago) | |
6. 10 or more years ago | |
7. Don’t know/Not Sure | |
9. Refused |
Appendix Table 5: Sensitivity difference in difference analysis between states with different medicaid expansion times from 2012 to 2020
Crude DD | Adjusted DD | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
2014 v 2012 | 2016 v 2012 | 2018 v 2012 | 2020v2012 | 2014 v 2012 | 2016 v 2012 | 2018 v 2012 | 2020 v 2012 | |||||||||
Up-to-date CRC screening | DD (%) | p value | DD (%) | p value | DD (%) | p value | DD (%) | p value | DD (%) | p value | DD (%) | p value | DD (%) | p value | DD (%) | p value |
VEES | − 10.21 | 0.2727 | 19.48 | 0.0435 | 13.67 | 0.1343 | − 18.60 | 0.2023 | − 9.61 | 0.3242 | 18.15 | 0.0674 | 13.95 | 0.1303 | − 19.23 | 0.2089 |
EES | − 0.66 | 0.9161 | − 8.54 | 0.1668 | − 0.31 | 0.961 | 7.95 | 0.3115 | − 1.87 | 0.7689 | − 8.11 | 0.2012 | 0.89 | 0.8903 | 8.81 | 0.2792 |
LES | 0.16 | 0.9845 | − 6.92 | 0.4558 | 2.31 | 0.8087 | 2.00 | 0.8632 | 3.02 | 0.7141 | − 7.41 | 0.4421 | 1.48 | 0.8777 | − 0.05 | 0.9969 |
NES | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qian, Z., Chen, X., Pucheril, D. et al. Long-Term Impact of Medicaid Expansion on Colorectal Cancer Screening in Its Targeted Population. Dig Dis Sci 68, 1780–1790 (2023). https://doi.org/10.1007/s10620-022-07797-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07797-x