Abstract
Background
The coronavirus 2019 (COVID-19) pandemic required an immediate and large-scale transition to telemedicine. Telemedicine includes phone visits and video visits. Studies suggest that hepatocellular cancer (HCC) screening rates fell at the beginning of the COVID-19 pandemic. If left unaddressed, HCC morbidity/mortality may increase following the pandemic due to inadequate screening.
Aims
To assess the impact of phone-only visits on HCC screening rates in patients with cirrhosis.
Methods
Utilizing ICD-10 codes, 2 cohorts of patients with cirrhosis were identified. The pre-pandemic cohort had index visit between 1/1/2019 and 6/30/2019 (n = 290). The pandemic cohort (n = 112) was evaluated between 4/7/2020 and 6/7/2020. Each cohort was followed for 6 months from their index visit to determine HCC screening rate. Demographics and socioeconomic data from the American Community Survey database were compiled and compared between the cohorts.
Results
HCC screening rates in the pre-pandemic and pandemic cohorts were 72.4% and 69.6%, respectively, p = 0.67. No differences in HCC screening rates were observed between the two cohorts when stratified by demographic and socioeconomic factors.
Conclusions
Use of phone-only visits was associated with adherence to HCC screening similar to that seen with in-person visits. The lack of influence on screening rates by racial/socioeconomic factors suggest telephone-only visits do not exacerbate healthcare disparities. In times of public health of crisis, telephone-only visits may provide the necessary access to hepatology care to ensure HCC screening regimens remain in-place for at-risk patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The social distancing and stay at home orders instituted to slow the spread of coronavirus 2019 (COVID-19) abruptly shifted the landscape of delivering care to patients with cirrhosis. Though previously not in widespread use, telemedicine became an essential component of healthcare delivery, and its use increased by 4000% [1]. While this technology helped maintain access to care remotely, certain aspects of care in cirrhosis require in-person visits including hepatocellular carcinoma (HCC) and variceal screening/surveillance.
Professional society guidelines recommend semiannual surveillance in high-risk individuals using abdominal ultrasound (US) with or without alpha-fetoprotein (AFP). A multinational study demonstrated a decline of 26.7% of new HCC cases reported, and delays in diagnosis near 50% during the pandemic compared to pre-pandemic times [2]. In a study from the United Kingdom comparing the modes of presentation of HCC in pre-pandemic and pandemic cohorts, the pandemic cohort demonstrated an increased number of patients presenting with symptomatic disease and a decrease in the number of HCC cases found through surveillance [3]. Another study demonstrated a significant decrease in the number of abdominal US examinations performed at a site in the USA at the onset of pandemic-associated travel restrictions [4].
This disruption of guideline-based cancer screening resulting in decreases and delays in identifying new cancers and subsequent delivery of treatment has been a topic of alarm and focus during the pandemic. In the absence of effective interventions, concerns have been raised that cancer morbidity/mortality rates may rise in the years following the pandemic [5].
Telemedicine platforms have been proposed as a way to maintain access to hepatology care and allow providers to stress the need to remain vigilant to HCC screening regimens. However, concerns have been raised that telemedicine does not mitigate disparities in vulnerable populations [6]. Factors such as access to high-speed internet/mobile devices and digital literacy represent barriers. In one study, Black race and age ≥ 60 were associated with a higher rate of telephone-only visits compared to video visits [1]. This is particularly relevant given the average age in the HCC population.
The primary aim of this study was to assess if linkage to hepatology care through telephone-only visits would prevent the decrease in HCC screening rates observed in the aforementioned studies at the onset of the pandemic as compared to a pre-pandemic cohort. The secondary aim was to assess if social determinants of health influenced the rate of HCC surveillance in either cohort.
Methods
Study Populations
The study was approved by our Institutional Review Board. The study population included adult patients ≥ 18 years of age with cirrhosis receiving care at a tertiary medical center outpatient Hepatology clinic between 1/2019 and 6/2020. Patients with cirrhosis were identified using the following problem list ICD-10 diagnoses: B19.10, B19.2, E83.110, K70.3, K70.31, K70.30, K71.7, K74, K74.3, K74.4, K74.5, K74.6, K74.60, K74.69, K76, and K78.81. From the resulting list of patients, charts in the electronic medical record (EMR) were independently vetted by study personnel (JU, SR, SS) to confirm the diagnosis of cirrhosis. Two cohorts (based on time period) were identified for comparison; the pandemic cohort and the pre-pandemic cohort. The pandemic cohort (n = 112) consisted of encounters between 4/7/2020 and 6/7/2020 that were conducted via telephone visit only. The pandemic cohort date ranges correspond to the time period with the highest volume of telemedicine services at our institution following statewide stay at home orders in response to the SARS-CoV-2 outbreak [7].
The pre-pandemic cohort (n = 290) included encounters between 1/1/2019 and 6/30/2019. The pre-pandemic cohort represented "standard of care" (“SOC”) prior to implementation of telemedicine (100% of visits in-person). This date range was specifically chosen to ensure pertinent outcomes measured were appropriately linked (temporally) to the appropriate cohort.
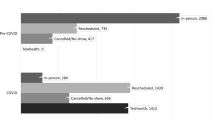
The index visit was defined as the first clinic encounter for a patient occurring within the cohort date range and included visits of new and existing patients to the practice. Individual encounters were then independently vetted through direct review of patient records in the EMR by study personnel. EMR data was followed for a total of 6 months from their index visit in each time cohort to record HCC screening rates. Appropriate HCC screening modality was defined as abdominal ultrasound or contrast-enhanced cross-sectional imaging (MR or CT) based on provider discretion. Figure 1 outlines the process of identifying the two cohorts from the total number of encounters during the respective periods.
Data Collection and Outcomes
Data regarding individual patient-level characteristics, procedure orders, labs, visit metrics, and providers was obtained. In each cohort, patients were followed for 6 months after their index visit to assess for performance of guideline-based HCC screening. Adherence to HCC screening guidelines was evaluated by determining if providers ordered appropriately indicated screening imaging (within 1 month of index visit), and if the imaging study was performed within 6 months of being ordered. The rationale for allowing 6 months for the patient to have the appropriately ordered imaging performed was to allow for flexibility of scheduling both before and during the pandemic.
The American Community Survey (ACS) data was also extracted to further characterize patient-level metrics including urban vs. rural location. Laboratory data was extracted from the EMR then manually reviewed by study personnel. Labs were included if they were obtained within 2 months of the encounter date, and the Model for End-Stage Liver Disease (MELD) and MELD-Na scores were calculated. Labs from ER visits or hospitalizations were excluded as they did not represent the patients’ baseline status. Data regarding etiology of liver disease and evidence of hepatic decompensation (including ascites, hepatic encephalopathy, or variceal hemorrhage) were determined manually by study personnel using progress notes, endoscopy records, and imaging findings. Clinic encounters were characterized as either in-person or telephone visit. Completion of the scheduled imaging for HCC surveillance was the main outcome measure.
Statistical Analysis
We compared HCC screening rates between pandemic and pre-pandemic cohorts using standard descriptive statistics including means, standard deviations, frequencies, and proportions. Unadjusted bivariate comparisons were analyzed using Chi-square, Fisher’s exact, and t-tests, as appropriate. Comparison of HCC screening levels between cohorts were assessed using Chi-square tests. Mixed effects regression, with random intercepts by patient, was performed to examine patient factors associated with HCC screening in pre-pandemic and pandemic cohorts. Statistical tests were two-sided, and α level of 0.05 was used to determine statistical significance. Data processing and statistical analyses were completed using SPSS statistical software, version 3.6.1. (IBM, Armonk, NY).
Results
Study Population
The study population included 402 index visits across both pandemic and pre-pandemic cohorts. The pandemic cohort included encounters conducted via telephone visit only between 4/7/2020 and 6/7/2020 (n = 112). The pre-pandemic cohort included in-person encounters in Hepatology clinic from 1/1/2019 to 6/30/2019 (n = 290).
Demographics
Table 1 details the pertinent characteristics of the cohorts including demographics (mean age, race, and ethnicity), insurance carrier, socioeconomic factors (mean income estimate and location; rural vs. urban), and etiology/severity of liver disease. The two cohorts were similar in age, racial composition, insurance carrier, and mean income. The most common etiology of cirrhosis was non-alcoholic steatohepatitis (NASH) in both cohorts. The severity of liver disease as measured by MELD and proportion of patients with decompensated cirrhosis was similar.
HCC Screening Rates
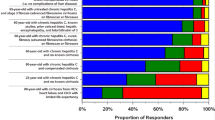
Adherence to HCC screening measured by the ordering of imaging (provider-level) and the completion of the ordered imaging study (patient-level) was not different between cohorts, with HCC screening rate of 72.4% in the pre-pandemic cohort compared to 69.6% in the pandemic cohort (p = 0.67). In the bivariate analysis there were no statistically significant differences observed in HCC screening rates based upon age, race, or location (rural vs. urban). This was true of both pre-pandemic and pandemic cohorts (Table 2).
Discussion
The onset of the COVID-19 pandemic abruptly forced the medical community to adopt the widespread use of telemedicine to maintain delivery of care, with its use increasing by 4000% [1]. In the setting of the COVID-19 pandemic, the main purpose of telemedicine was to mitigate transmission of the SARS-CoV-2 virus, but the application of telemedicine in patients with cirrhosis predates the pandemic. Proposed benefits include overcoming geographical barriers to care, improving efficiency of care with improvement in cost metrics, and improved patient satisfaction/engagement [8, 9].
However, concerns have been raised that socioeconomic factors that represent barriers to accessing Hepatology care are not mitigated by use of telemedicine. In 2021, Wegermann et al. found that Black patients and patients with nonprivate insurance (i.e. Medicaid, Medicare) were more likely to complete a phone-only visit instead of a video visit [6]. Another study suggested Black race and older age were associated with lower digital literacy [1]. Access to electronic devices and/or high-speed Internet to facilitate video visits are affected by geography and socioeconomic status, thus potentially exacerbating existing disparities in access to care for vulnerable populations. These studies highlight the continued need for strategies that link patients to appropriate care through ubiquitous modalities (i.e. the telephone). Though the long-term place of telemedicine in the care of patients with cirrhosis is unclear, what remains certain is the need for in-person visits to complete HCC and variceal screening/surveillance [2–4].
Results from studies performed during the outset of the pandemic suggest decreased numbers of abdominal US being performed, delays in diagnosis of HCC, declines in new HCC cases reported, decreased number of HCC cases found through surveillance, and increased numbers of patients presenting with symptomatic HCC [2–4]. These studies describe observations pertaining to HCC surveillance and presentations, but did not specifically address what, if any interventions influenced these outcomes. The present study observed similar rates of HCC screening in both the pre-pandemic (in-person visits) and pandemic (telephone-only visits) cohorts of 72.4% and 69.6%, respectively (p = 0.67). This demonstrates that maintained patient-physician communication (in the form of telephone-only clinic visits) were an effective means to ensure adherence to HCC screening even at the outset of the COVID-19 pandemic and avoid the declines observed in the aforementioned studies.
We did not observe statistically significant differences in HCC screening rates in either the pre-pandemic or pandemic cohorts as it related to age, race, income estimate, or location (rural vs. urban). We suspect the essentially universal household or personal presence of telephones across ages, races, incomes, and locations contribute to this finding. While recent evidence suggests a nearly 20-fold increase in cirrhosis age-adjusted mortality between rural and large metropolitan areas, our data suggest that geographic location does not influence HCC screening rates [10]. We speculate that other cirrhosis-related complications requiring access to tertiary centers for complex management may account for this discrepancy.
While optimistic these results suggest a positive influence of telephone-only visits across a diverse population of patients, our study has limitations that must be acknowledged. The derivation of both the pre-pandemic and pandemic cohorts from an outpatient Hepatology practice introduces potential referral bias, thus potentially limiting generalizability to non-tertiary practices screening patients for HCC. The predominantly urban population (~ 77% in both cohorts) also limits generalizability.
The widespread decrease in in-person care and guideline-based HCC screening at the outset of the COVID-19 pandemic raised concerns that without an effective intervention cancer-related morbidity/mortality rates would rise. This study demonstrates that utilization of telephone-only visits results in maintained HCC screening rates in patients with cirrhosis.
Abbreviations
- ACS:
-
American Community Survey
- COVID-19:
-
Coronavirus infection disease 2019
- EMR:
-
Electronic medical record
- HCV:
-
Hepatitis C virus
- HCC:
-
Hepatocellular carcinoma
- MELD:
-
Model for End-Stage Liver Disease
- NASH:
-
Non-alcoholic steatohepatitis
- SOC:
-
Standard of care
- TM:
-
Telemedicine
References
Serper M, Nunes F, Ahmad N et al. Positive early patient and clinician experience with telemedicine in an academic gastroenterology practice during the COVID-19 pandemic. Gastroenterology. 2020;159:1589-1591.e1584.
Gandhi M, Ling WH, Chen CH et al. Impact of COVID-19 on hepatocellular carcinoma management: A multicountry and region study. J Hepatocell Carcinoma. 2021;8:1159–1167.
Geh D, Watson R, Sen G et al. COVID-19 and liver cancer: lost patients and larger tumours. BMJ Open Gastroenterol. 2022;9:19.
Toyoda H, Huang DQ, Le MH et al. Liver care and surveillance: the global impact of the COVID-19 pandemic. Hepatol Commun. 2020;4:1751–1757.
Patt D, Gordan L, Diaz M et al. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for american seniors. JCO Clin Cancer Inform. 2020;4:1059–1071.
Wegermann K, Wilder JM, Parish A et al. Racial and socioeconomic disparities in utilization of telehealth in patients with liver disease during COVID-19. Dig Dis Sci. 2022;67:93–99.
NCDHHS.gov. Governor Cooper Announces Statewide Stay at Home Order Until April 29. Published March 27,2020. Accessed January 2022.
Arrese M. Telemedicine, COVID-19 and liver diseases: revamping remote care initiatives in hepatology. Ann Hepatol. 2020;19:339–340.
Piao C, Terrault NA, Sarkar S. Telemedicine: an evolving field in hepatology. Hepatol Commun. 2019;3:716–721.
Ufere NN, Patzer RE, Kavalieratos D et al. Rural-urban disparities in mortality from cirrhosis in the United States From 1999 to 2019. Am J Gastroenterol. 2022;117:1162–1165.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SR: study design, data review, writing of manuscript. JU: data collection, preparation of tables/figures. SS: data collection, preparation of tables/figures. RB: data extraction, statistical analysis, preparation of tables/figures. AD: study design, data extraction, manuscript editing. MR: study design, manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rudnick, S.R., Ugwuegbu, J., Soufleris, S.J. et al. Telephone-Only Visits Preserved Hepatocellular Cancer Screening Rates in Patients with Cirrhosis Early in the COVID-19 Pandemic. Dig Dis Sci 68, 1791–1796 (2023). https://doi.org/10.1007/s10620-022-07786-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07786-0