Abstract
Background and Aims
Pancreatic enzyme replacement therapy (PERT) is most commonly used to treat exocrine insufficiency related to pancreatic diseases, but can be used for non-pancreatic digestive conditions (NPDC). We aimed to determine the prevalence of PERT use and describe prescription patterns in individuals with NPDC.
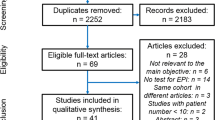
Methods
A nationally representative claims database of 48.6 million enrollees was used to identify individuals who received PERT prescription(s) in the absence of any pancreas-related diagnosis. Data on demographics, enrolment, comorbidities, exocrine function testing, treatment and potential indications for PERT were retrieved, and compared with individuals who received PERT for primary diagnosis of chronic pancreatitis (CP).
Results
A total of 29,234 individuals (64.1% female, mean age 52.4 ± 16.5 years) received PERT for NPDC. The overall estimated US population prevalence rate for PERT use for NDPC was 60.2/100,000 persons. Rates increased significantly with age and were higher in women in all age groups except 1–20 years old. When compared with CP, individuals with NPDC receiving PERT were more likely to be older (52.4 vs. 50.1 years), female (64.1% vs. 51.0%), have lower prevalence of alcoholism (3.6% vs. 25.0%), tobacco abuse (8.4% vs. 30.1%), and received PERT for shorter mean duration (5.3 vs. 8.2 months) (all p < 0.001). Median dose of PERT in individuals with NPDC was 2880 lipase units/day.
Conclusions
Although proportionally low, a sizable population receives PERT for NPDC. PERT for NPDC is usually prescribed at a low dose and for shorter duration, suggesting it is used mostly as a trial for or until resolution of symptoms.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from IQVIA Legacy PharMetrics. Restrictions apply to the availability of these data, which were used under license for this study. Data are available from the corresponding author with permission of IQVIA.
Abbreviations
- AP:
-
Acute pancreatitis
- CI:
-
Confidence interval
- CP:
-
Chronic pancreatitis
- EPI:
-
Exocrine pancreatic insufficiency
- ICD:
-
International classification of diseases
- IQR:
-
Inter-quartile range
- NPDC:
-
Non-pancreatic digestive conditions
- PERT:
-
Pancreatic enzyme replacement therapy
- SD:
-
Standard deviation
References
Struyvenberg MR, Martin CR, Freedman SD. Practical guide to exocrine pancreatic insufficiency - Breaking the myths. BMC Med. 2017;15:29.
Greer JB, Greer P, Sandhu BS et al. Nutrition and Inflammatory Biomarkers in Chronic Pancreatitis Patients. Nutr Clin Pract. 2019;34:387–399.
Joker-Jensen H, Mathiasen AS, Kohler M, Rasmussen HH, Drewes AM, Olesen SS. Micronutrient deficits in patients with chronic pancreatitis: prevalence, risk factors and pitfalls. Eur J Gastroenterol Hepatol. 2020;32:1328–1334.
O’Brien SJ, Omer E. Chronic Pancreatitis and Nutrition Therapy. Nutr Clin Pract. 2019;34:S13–S26.
Singh VK, Schwarzenberg SJ. Pancreatic insufficiency in Cystic Fibrosis. J Cyst Fibros. 2017;16:S70–S78.
Gilliland TM, Villafane-Ferriol N, Shah KP, et al. Nutritional and Metabolic Derangements in Pancreatic Cancer and Pancreatic Resection. Nutrients. 2017;9(3).
Hallac A, Aleassa EM, Rogers M, Falk GA, Morris-Stiff G. Exocrine pancreatic insufficiency in distal pancreatectomy: incidence and risk factors. HPB (Oxford). 2020;22:275–281.
Hollemans RA, Hallensleben NDL, Mager DJ et al. Pancreatic exocrine insufficiency following acute pancreatitis: Systematic review and study level meta-analysis. Pancreatology. 2018;18:253–262.
Singh VK, Haupt ME, Geller DE, Hall JA, Quintana Diez PM. Less common etiologies of exocrine pancreatic insufficiency. World J Gastroenterol. 2017;23:7059–7076.
Nousia-Arvanitakis S, Fotoulaki M, Tendzidou K, Vassilaki C, Agguridaki C, Karamouzis M. Subclinical exocrine pancreatic dysfunction resulting from decreased cholecystokinin secretion in the presence of intestinal villous atrophy. J Pediatr Gastroenterol Nutr. 2006;43:307–312.
DiMagno EP, Go WL, Summerskill WH. Impaired cholecystokinin-pancreozymin secretion, intraluminal dilution, and maldigestion of fat in sprue. Gastroenterology. 1972;63:25–32.
Rominger JM, Chey WY, Chang TM. Plasma secretin concentrations and gastric pH in healthy subjects and patients with digestive diseases. Dig Dis Sci. 1981;26:591–597.
Kovacs M, Lakatos PL, Papp M et al. Pancreatic autoantibodies and autoantibodies against goblet cells in pediatric patients with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2012;55:429–435.
Friess H, Bohm J, Muller MW et al. Maldigestion after total gastrectomy is associated with pancreatic insufficiency. Am J Gastroenterol. 1996;91:341–347.
Armbrecht U, Lundell L, Stockbruegger RW. Nutrient malassimilation after total gastrectomy and possible intervention. Digestion. 1987;37:56–60.
Borbely Y, Plebani A, Kroll D, Ghisla S, Nett PC. Exocrine Pancreatic Insufficiency after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2016;12:790–794.
Huddy JR, Macharg FM, Lawn AM, Preston SR. Exocrine pancreatic insufficiency following esophagectomy. Dis Esophagus. 2013;26:594–597.
Evans KE, Leeds JS, Morley S, Sanders DS. Pancreatic insufficiency in adult celiac disease: do patients require long-term enzyme supplementation? Dig Dis Sci. 2010;55:2999–3004.
Leeds JS, Hopper AD, Hurlstone DP et al. Is exocrine pancreatic insufficiency in adult coeliac disease a cause of persisting symptoms? Aliment Pharmacol Ther. 2007;25:265–271.
Armbrecht U, Lundell L, Stockbrugger RW. The benefit of pancreatic enzyme substitution after total gastrectomy. Aliment Pharmacol Ther. 1988;2:493–500.
Bragelmann R, Armbrecht U, Rosemeyer D, Schneider B, Zilly W, Stockbrugger RW. The effect of pancreatic enzyme supplementation in patients with steatorrhoea after total gastrectomy. Eur J Gastroenterol Hepatol. 1999;11:231–237.
Huang W, de la Iglesia-Garcia D, Baston-Rey I et al. Exocrine Pancreatic Insufficiency Following Acute Pancreatitis: Systematic Review and Meta-Analysis. Dig Dis Sci. 2019;64:1985–2005.
Forsmark CE, Tang G, Xu H, Tuft M, Hughes SJ, Yadav D. The use of pancreatic enzyme replacement therapy in patients with a diagnosis of chronic pancreatitis and pancreatic cancer in the US is infrequent and inconsistent. Aliment Pharmacol Ther. 2020;51:958–967.
Gardner TB, Munson JC, Morden NE. The FDA and prescription pancreatic enzyme product cost. Am J Gastroenterol. 2014;109:624–625.
Jensen ET, Martin CF, Kappelman MD, Dellon ES. Prevalence of Eosinophilic Gastritis, Gastroenteritis, and Colitis: Estimates From a National Administrative Database. J Pediatr Gastroenterol Nutr. 2016;62:36–42.
Kappelman MD, Rifas-Shiman SL, Kleinman K et al. The prevalence and geographic distribution of Crohn’s disease and ulcerative colitis in the United States. Clin Gastroenterol Hepatol. 2007;5:1424–1429.
Dilokthornsakul P, Valuck RJ, Nair KV, Corboy JR, Allen RR, Campbell JD. Multiple sclerosis prevalence in the United States commercially insured population. Neurology. 2016;86:1014–1021.
Simon TA, Boers M, Hochberg M et al. Comparative risk of malignancies and infections in patients with rheumatoid arthritis initiating abatacept versus other biologics: a multi-database real-world study. Arthritis Res Ther. 2019;21:228.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619.
Oka P, Parr H, Barberio B, Black CJ, Savarino EV, Ford AC. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5:908–917.
Acknowledgments
We would like to thank Hongzhi Xu, PhD for assistance in data organization and programming.
Funding
Gatorade Foundation (CEF) Research reported in this study was supported by the Gatorade Research Trust (CEF, DY) and the National Cancer Institute (NCI) and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) under award numbers UO1DK108320 (CEF) and UO1DK108306 (DY). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
AEP (Writing: original draft and editing), GT (Data curation, Formal analysis), XW (Data curation, Formal analysis), CEF (Conceptualization, Funding acquisition, Writing: review and editing), DY (Conceptualization, Funding acquisition, Methodology, Supervision, Writing: review and editing). All authors have approved the final version of the article. Dhiraj Yadav is guarantor of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant conflicts of interest to disclose.
Preprint server
The manuscript is not included on any preprint server.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Phillips, A.E., Tang, G., Wang, X. et al. Pancreatic Enzyme Replacement Therapy in Patients with Non-pancreatic Digestive Conditions: A Nationwide Claims Analysis. Dig Dis Sci 68, 1754–1761 (2023). https://doi.org/10.1007/s10620-022-07750-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07750-y