Abstract
Background
This study aimed to determine the rate, timing, and predictors of diabetes and exocrine pancreatic insufficiency after pancreatectomy in order to inform preoperative patient counseling and risk management strategies.
Methods
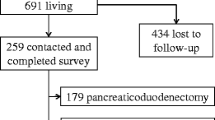
Using prescription claims as a surrogate for disease prevalence, IBM Watson Health MarketScan was queried for claims patterns pre- and post-pancreatectomy. Multivariable models explored associations between clinical characteristics and medication use within 2 years of surgery.
Results
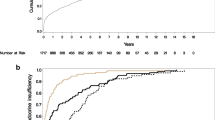
In total, 18.96% of 2,848 pancreaticoduodenectomy (PD) patients and 18.95% of 1,858 distal pancreatectomy (DP) patients had preoperative diabetic medication prescription claims. Fewer (6.6% and 3.88%, respectively) had pancreatic enzyme replacement therapy (PERT) claims. Diabetic medication claims increased to 28.69% after PD and 38.59% after DP [adjusted relative risk (aRR) = 1.36 (95% CI 1.27, 1.46)]. Other associated factors included age > 45, medical comorbidity, and obesity. The incidence of new diabetic medication claims among medication naïve patients was 13.78% for PD and 24.7% for DP (p < 0.001) with a median 4.7 and 4.9 months post-operatively. The prevalence of PERT claims was 55.97% after PD and 17.06% after DP [aRR = 0.32 (0.29, 0.36)]. The incidence of postoperative PERT claims 53.98% (PD) and 14.84% (DP) (p < 0.0001). The median time to new PERT claim was 3.0 (PD) and 3.2 (DP) months, respectively. Claims for both diabetic medications and PERT rose sharply after surgery and plateaued within 6 months.
Conclusions
This study defines prevalence, timing, and predictors for post-pancreatectomy insufficiency to inform preoperative counseling, risk modification strategies, and interventions related to quality of life.



Similar content being viewed by others
References
Rosales-Velderrain A, Bowers SP, Goldberg RF, et al. National trends in resection of the distal pancreas. World J Gastroenterol. 2012;18(32):4342-4349. https://doi.org/10.3748/wjg.v18.i32.4342
Shaw K, Thomas AS, Rosario V, et al. Long term quality of life amongst pancreatectomy patients with diabetes mellitus. Pancreatology. Published online January 22, 2021. https://doi.org/10.1016/j.pan.2021.01.012
Stoop TF, Ateeb Z, Ghorbani P, et al. Impact of Endocrine and Exocrine Insufficiency on Quality of Life After Total Pancreatectomy. Ann Surg Oncol. 2020;27(2):587-596. https://doi.org/10.1245/s10434-019-07853-3
Huang JJ, Yeo CJ, Sohn TA, et al. Quality of life and outcomes after pancreaticoduodenectomy. Ann Surg. 2000;231(6):890-898. https://doi.org/10.1097/00000658-200006000-00014
Roberts KJ, Blanco G, Webber J, et al. How severe is diabetes after total pancreatectomy? A case-matched analysis. HPB (Oxford). 2014;16(9):814-821. https://doi.org/10.1111/hpb.12203
Elliott IA, Epelboym I, Winner M, Allendorf JD, Haigh PI. Population-Level Incidence and Predictors of Surgically Induced Diabetes and Exocrine Insufficiency after Partial Pancreatic Resection. Perm J. 2017;21:16-095. https://doi.org/10.7812/TPP/16-095
Maeda H, Hanazaki K. Pancreatogenic diabetes after pancreatic resection. Pancreatology. 2011;11(2):268-276. https://doi.org/10.1159/000328785
Woodmansey C, McGovern AP, McCullough KA, et al. Incidence, Demographics, and Clinical Characteristics of Diabetes of the Exocrine Pancreas (Type 3c): A Retrospective Cohort Study. Diabetes Care. 2017;40(11):1486-1493. https://doi.org/10.2337/dc17-0542
Tseng DSJ, Molenaar IQ, Besselink MG, van Eijck CH, Borel Rinkes IH, van Santvoort HC. Pancreatic Exocrine Insufficiency in Patients With Pancreatic or Periampullary Cancer: A Systematic Review. Pancreas. 2016;45(3):325-330. https://doi.org/10.1097/MPA.0000000000000473
Mayeux SE, Kwon W, Rosario VL, et al. Long-term health after pancreatic surgery: the view from 9.5 years. HPB (Oxford). Published online September 25, 2020.https://doi.org/10.1016/j.hpb.2020.08.017
Kusakabe J, Anderson B, Liu J, et al. Long-Term Endocrine and Exocrine Insufficiency After Pancreatectomy. J Gastrointest Surg. 2019;23(8):1604-1613. https://doi.org/10.1007/s11605-018-04084-x
Scholten L, Stoop TF, Del Chiaro M, et al. Systematic review of functional outcome and quality of life after total pancreatectomy. Br J Surg. 2019;106(13):1735-1746. https://doi.org/10.1002/bjs.11296
Scholten L, Latenstein AEJ, van Eijck C, et al. Outcome and long-term quality of life after total pancreatectomy (PANORAMA): a nationwide cohort study. Surgery. 2019;166(6):1017-1026. https://doi.org/10.1016/j.surg.2019.07.025
Okano K, Murakami Y, Nakagawa N, et al. Remnant pancreatic parenchymal volume predicts postoperative pancreatic exocrine insufficiency after pancreatectomy. Surgery. 2016;159(3):885-892. https://doi.org/10.1016/j.surg.2015.08.046
Shah KP, Baugh KA, Brubaker LS, et al. Long-Term Assessment of Pancreatic Function After Pancreatectomy for Cystic Neoplasms. J Surg Res. 2020;247:547-555. https://doi.org/10.1016/j.jss.2019.09.045
Oh HM, Yoon YS, Han HS, Kim JH, Cho JY, Hwang DW. Risk factors for pancreatogenic diabetes after pancreaticoduodenectomy. Korean J Hepatobiliary Pancreat Surg. 2012;16(4):167-171. https://doi.org/10.14701/kjhbps.2012.16.4.167
Traverso LW, Kozarek RA. Pancreatoduodenectomy for chronic pancreatitis: anatomic selection criteria and subsequent long-term outcome analysis. Ann Surg. 1997;226(4):429–435; discussion 435–438.https://doi.org/10.1097/00000658-199710000-00004
Sakorafas GH, Sarr MG, Rowland CM, Farnell MB. Postobstructive chronic pancreatitis: results with distal resection. Arch Surg. 2001;136(6):643-648. https://doi.org/10.1001/archsurg.136.6.643
Falconi M, Mantovani W, Crippa S, Mascetta G, Salvia R, Pederzoli P. Pancreatic insufficiency after different resections for benign tumours. Br J Surg. 2008;95(1):85-91. https://doi.org/10.1002/bjs.5652
Halloran CM, Cox TF, Chauhan S, et al. Partial pancreatic resection for pancreatic malignancy is associated with sustained pancreatic exocrine failure and reduced quality of life: a prospective study. Pancreatology. 2011;11(6):535-545. https://doi.org/10.1159/000333308
Phillips ME. Pancreatic exocrine insufficiency following pancreatic resection. Pancreatology. 2015;15(5):449-455. https://doi.org/10.1016/j.pan.2015.06.003
Sikkens ECM, Cahen DL, de Wit J, Looman CWN, van Eijck C, Bruno MJ. A prospective assessment of the natural course of the exocrine pancreatic function in patients with a pancreatic head tumor. J Clin Gastroenterol. 2014;48(5):e43-46. https://doi.org/10.1097/MCG.0b013e31829f56e7
Schnelldorfer T, Lewin DN, Adams DB. Operative management of chronic pancreatitis: longterm results in 372 patients. J Am Coll Surg. 2007;204(5):1039–1045; discussion 1045–1047. https://doi.org/10.1016/j.jamcollsurg.2006.12.045
Belyaev O, Herzog T, Chromik AM, Meurer K, Uhl W. Early and late postoperative changes in the quality of life after pancreatic surgery. Langenbecks Arch Surg. 2013;398(4):547-555. https://doi.org/10.1007/s00423-013-1076-3
Matsumoto J, Traverso LW. Exocrine function following the whipple operation as assessed by stool elastase. J Gastrointest Surg. 2006;10(9):1225-1229. https://doi.org/10.1016/j.gassur.2006.08.001
Beger HG, Poch B, Mayer B, Siech M. New Onset of Diabetes and Pancreatic Exocrine Insufficiency After Pancreaticoduodenectomy for Benign and Malignant Tumors: A Systematic Review and Meta-analysis of Long-term Results. Ann Surg. 2018;267(2):259-270. https://doi.org/10.1097/SLA.0000000000002422
Hutchins RR, Hart RS, Pacifico M, Bradley NJ, Williamson RCN. Long-term results of distal pancreatectomy for chronic pancreatitis in 90 patients. Ann Surg. 2002;236(5):612-618. https://doi.org/10.1097/00000658-200211000-00011
Schoenberg MH, Schlosser W, Rück W, Beger HG. Distal pancreatectomy in chronic pancreatitis. Dig Surg. 1999;16(2):130-136. https://doi.org/10.1159/000018705
Shoup M, Brennan MF, McWhite K, Leung DHY, Klimstra D, Conlon KC. The value of splenic preservation with distal pancreatectomy. Arch Surg. 2002;137(2):164-168. https://doi.org/10.1001/archsurg.137.2.164
King J, Kazanjian K, Matsumoto J, et al. Distal pancreatectomy: incidence of postoperative diabetes. J Gastrointest Surg. 2008;12(9):1548-1553. https://doi.org/10.1007/s11605-008-0560-5
Lillemoe KD, Kaushal S, Cameron JL, Sohn TA, Pitt HA, Yeo CJ. Distal pancreatectomy: indications and outcomes in 235 patients. Ann Surg. 1999;229(5):693–698; discussion 698–700. https://doi.org/10.1097/00000658-199905000-00012
De Bruijn KMJ, van Eijck CHJ. New-onset diabetes after distal pancreatectomy: a systematic review. Ann Surg. 2015;261(5):854-861. https://doi.org/10.1097/SLA.0000000000000819
National Diabetes Statistics Report, 2020 | CDC. Published September 28, 2020. Accessed October 11, 2021. https://www.cdc.gov/diabetes/data/statistics-report/index.html
Das SLM, Singh PP, Phillips ARJ, Murphy R, Windsor JA, Petrov MS. Newly diagnosed diabetes mellitus after acute pancreatitis: a systematic review and meta-analysis. Gut. 2014;63(5):818-831. https://doi.org/10.1136/gutjnl-2013-305062
Ewald N, Kaufmann C, Raspe A, Kloer HU, Bretzel RG, Hardt PD. Prevalence of diabetes mellitus secondary to pancreatic diseases (type 3c). Diabetes Metab Res Rev. 2012;28(4):338-342. https://doi.org/10.1002/dmrr.2260
Ferrara MJ, Lohse C, Kudva YC, et al. Immediate post-resection diabetes mellitus after pancreaticoduodenectomy: incidence and risk factors. HPB (Oxford). 2013;15(3):170-174. https://doi.org/10.1111/j.1477-2574.2012.00520.x
Hirata K, Nakata B, Amano R, Yamazoe S, Kimura K, Hirakawa K. Predictive factors for change of diabetes mellitus status after pancreatectomy in preoperative diabetic and nondiabetic patients. J Gastrointest Surg. 2014;18(9):1597-1603. https://doi.org/10.1007/s11605-014-2521-5
Slezak LA, Andersen DK. Pancreatic resection: effects on glucose metabolism. World J Surg. 2001;25(4):452-460. https://doi.org/10.1007/s002680020337
Seiler CM, Izbicki J, Varga-Szabó L, et al. Randomised clinical trial: a 1-week, double-blind, placebo-controlled study of pancreatin 25 000 Ph. Eur. minimicrospheres (Creon 25000 MMS) for pancreatic exocrine insufficiency after pancreatic surgery, with a 1-year open-label extension. Aliment Pharmacol Ther. 2013;37(7):691–702. https://doi.org/10.1111/apt.12236
Lim PW, Dinh KH, Sullivan M, et al. Thirty-day outcomes underestimate endocrine and exocrine insufficiency after pancreatic resection. HPB (Oxford). 2016;18(4):360-366. https://doi.org/10.1016/j.hpb.2015.11.003
Nakamura H, Murakami Y, Uemura K, et al. Predictive factors for exocrine pancreatic insufficiency after pancreatoduodenectomy with pancreaticogastrostomy. J Gastrointest Surg. 2009;13(7):1321-1327. https://doi.org/10.1007/s11605-009-0896-5
Neophytou H, Wangermez M, Gand E, Carretier M, Danion J, Richer JP. Predictive factors of endocrine and exocrine insufficiency after resection of a benign tumour of the pancreas. Ann Endocrinol (Paris). 2018;79(2):53-61. https://doi.org/10.1016/j.ando.2017.10.003
White MA, Agle SC, Fuhr HM, Mehaffey JH, Waibel BH, Zervos EE. Impact of pancreatic cancer and subsequent resection on glycemic control in diabetic and nondiabetic patients. Am Surg. 2011;77(8):1032-1037.
DiNorcia J, Ahmed L, Lee MK, et al. Better preservation of endocrine function after central versus distal pancreatectomy for mid-gland lesions. Surgery. 2010;148(6):1247–1254; discussion 1254–1256. https://doi.org/10.1016/j.surg.2010.09.003
Geiss LS, Wang J, Cheng YJ, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980-2012. JAMA. 2014;312(12):1218-1226. https://doi.org/10.1001/jama.2014.11494
Wu Y, Ding Y, Tanaka Y, Zhang W. Risk factors contributing to type 2 diabetes and recent advances in the treatment and prevention. Int J Med Sci. 2014;11(11):1185-1200. https://doi.org/10.7150/ijms.10001
Funding
This research is funded by the Columbia University Pancreas Center, Columbia University Medical Center Department of Surgery, and Columbia University Medical Center Department of Obstetrics & Gynecology.
Author information
Authors and Affiliations
Contributions
Each author has made substantial contributions to the conception or design of the work and drafting the work or revising it critically for intellectual content and final approval of the version to be published and agrees to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thomas, A.S., Huang, Y., Kwon, W. et al. Prevalence and Risk Factors for Pancreatic Insufficiency After Partial Pancreatectomy. J Gastrointest Surg 26, 1425–1435 (2022). https://doi.org/10.1007/s11605-022-05302-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05302-3