Abstract
Background
Motorized Spiral Enteroscopy (MSE) reduces procedure time and increases insertion depth into the small bowel; however, there is scarce evidence on factors affecting MSE efficacy.
Aims
To evaluate diagnostic yield and adverse events of MSE including patients with prior major abdominal surgery.
Methods
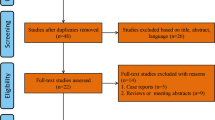
A prospective observational study was conducted on patients undergoing MSE from June 2019 to December 2021. Demographic characteristics, procedure time, depth of maximum insertion (DMI), technical success, diagnostic yield, and adverse events were collected.
Results
Seventy-four anterograde (54.4%) and 62 retrograde (45.6%) enteroscopies were performed in 117 patients (64 males, median age 67 years). Fifty patients (42.7%) had prior major abdominal surgery. Technical success was 91.9% for anterograde and 90.3% for retrograde route. Diagnostic yield was 71.6% and 61.3%, respectively. The median DMI was 415 cm (264–585) for anterograde and 120 cm (37–225) for retrograde enteroscopy. In patients with prior major abdominal surgery, MSE showed significantly longer small bowel insertion time (38 vs 29 min, p = 0.004), with similar diagnostic yield (61 vs 71.4%, p = 0.201) and DMI (315 vs 204 cm, p = 0.226). The overall adverse event rate was 10.3% (SAE 1.5%), with no differences related to prior abdominal surgery (p = 0.598). Patients with prior surgeries directly involving the gastrointestinal tract showed lower DMI (189 vs 374 cm, p = 0.019) with equal exploration time (37.5 vs 38 min, p = 0.642) compared to those with other abdominal surgeries.
Conclusions
MSE is effective and safe in patients with major abdominal surgery, although longer procedure times were observed. A lower depth of insertion was detected in patients with gastrointestinal surgery.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Deep enteroscopy (DE) has become an essential endoscopic technique for the small bowel (SB), especially when dealing with vascular lesions and Crohn’s disease [1]. Due to the technological advances leading to video capsule endoscopy, DE has mainly become a therapeutic procedure with a well-characterized role in diagnostic algorithms of some SB diseases [2].
An optimal enteroscopy procedure is required to be safe, relatively fast, with a high diagnostic and therapeutic yield, and, whether necessary, capable of performing a complete enteroscopy [3]. In daily practice, the time of exploration has a significant impact on hospital costs and limits the number of procedures performed; moreover, speed and high insertion depth are essential when lesions have not been adequately localized by previous exams and may potentially require a complete SB assessment [4].
Recent technological improvements have focused on the direction of insertion depth and ease of use, moving from double-balloon enteroscopy (DBE- Fujifilm, Tokyo, Japan) to single-balloon enteroscopy (SBE—Olympus Medical Systems Corporation, Tokyo, Japan), despite with similar results [5]. More recently, a technical change in the advancement system has led to spiral enteroscopy (SE—Spirus Medical Inc., Stoughton, MA, USA) [6]. The manual rotational movement of a spiral overtube allows the enteroscope to advance through the SB reducing the time of exploration, but without a significantly higher insertion depth compared to SBE [7]. In addition, no significant differences have been observed between SE and DBE in terms of diagnostic and therapeutic yield, procedure time, and safety [8].
The novel PowerSpiral Enteroscope (PSE, Olympus Corporation, Tokyo, JAPAN) has been recently introduced and the first case report was published in 2016 [9]. The activation of a user-controlled motor permits a rotational movement of a spiral overtube mounted on the enteroscope, thus, achieving advances by pleating the SB onto the tube. Several reports have been published since then, showing the potential abilities of Motorized Spiral Enteroscopy (MSE) in exploring the SB [10, 11]. The recently published feasibility trial of MSE in 132 patients described the efficacy and safety of anterograde explorations with this new device, with a high diagnostic yield and a low adverse event rate [12]. Two other clinical studies showed a total SB enteroscopy rate of around 61–70% [13, 14]. These first three studies excluded patients with prior major abdominal surgery due to safety concerns. However, the efficacy of MSE in surgically altered intestinal anatomy was documented [15]. A recent Danish multicenter study, including 20% of patients with surgically altered intestinal anatomy, showed a high diagnostic yield (61.4%) and no major adverse events; moreover, a multicenter European study focused on MSE safety demonstrated comparable SAE rates in the overall study population (2.3%) and patients with prior gastrointestinal surgery (1.9%) [16, 17]. In the present observational study, we aimed at describing the efficacy and safety of MSE in the daily clinical practice of a tertiary referral hospital, including patients with prior major abdominal surgeries.
Methods
Study Protocol
This prospective single-center observational study was conducted on all consecutive patients undergoing MSE at the Hospital Clinic of Barcelona from June 2019 to December 2021. During the study period, all patients with indication of enteroscopy were addressed to MSE, except those presenting the following contraindications: (1) known esophageal, gastric, or SB varices; (2) complicated eosinophilic esophagitis; (3) pregnancy; (4) the presence of implantable devices in the intestinal tract; (5) more than one known foregut strictures; (6) severe co-morbidities; and (7) inability to tolerate general anesthesia or deep sedation.
This study was conducted in accordance with the declaration of Helsinki Ethical Principles and Good Clinical Practices. The study protocol was approved by the local Ethical Committee of Hospital Clínic of Barcelona and patients signed informed consent.
The primary endpoint was to assess diagnostic yield and adverse events of MSE. Secondary endpoints were to evaluate (1) technical success, (2) therapeutic yield, (3) procedure times, and (4) learning curve.
MSE Device
The novel PSE (Olympus Corporation, Tokyo, JAPAN) consists of a 168-cm reusable enteroscope with a diameter of 11.3 mm and includes a 3.2 mm instrument channel and an integrated water-jet channel. A rotating spiral overtube is directly mounted and secured on the distal part of the enteroscope, at 16 cm from the tip, and driven by an incorporated motor. An Exera III Endoscopy System (Olympus Corporation, Tokyo, JAPAN) and a dedicated Power Spiral control unit are needed. The device is controlled by pedals which regulate the force and direction (backward and forward) of the advancement. The rotating spiral overtube pleats the SB onto the tube, thus, permitting the advancement of the tip, as previously reported [10]. An external visual force gage shows the force applied to the SB and, in case of too high resistance, the system automatically stops the rotation to avoid traumas.
MSE Technique
All procedures were performed by two endoscopists (BG-S, AG) with previous experience in SBE (more than 150 procedures a year). All patients had to avoid solid food for 8 h and clear fluids for 2 h before enteroscopy.
Patient monitoring during enteroscopy consisted of electrocardiography (ECG), oscillometric blood pressure measurement, pulse oximetry, bispectral index (BIS) monitor, respirometer, and capnography in case of general anesthesia, whereas ECG, blood pressure measurement, and pulse oximetry in case of deep propofol sedation. Anterograde procedures (A-MSE) were performed under general anesthesia and orotracheal intubation. On the same day of the procedure, an upper endoscopy was performed to exclude potential lesions which would preclude the insertion of the enteroscope. An endoscopic dilation with a Savary-Gilliard hollow-centered bougie of 18 mm in diameter was performed in the first procedures of the learning curve, according to the manufacturer’s recommendations, to enable the insertion of the enteroscope. In the following procedures, the esophageal dilation was limited to cases of narrowing. Retrograde procedures (R-MSE) were performed under deep sedation with previous bowel preparation (2 L Polyethylene Glycol) according to local protocols for colonoscopy.
The enteroscopy route was decided according to the findings in previous exams: localization of lesions according to Magnetic Resonance Imaging and Computerized Tomography scan reports or intestinal transit times of capsule endoscopy. All procedures were performed in the left lateral position. External abdominal compressions, as well as changes in the patient’s position, were routinely used in all patients to facilitate the enteroscope progression. All enteroscopies were performed with carbon dioxide insufflation. Fluoroscopy was not required for any enteroscopy.
Exploration was stopped in case of identification of a significant lesion according to pre-detected findings or in case of excessive resistance that impeded the advancement of the endoscope. During the procedure, polypectomy, electrocoagulation with Argon Plasma, and biopsy sampling were performed whether required. Tattooing with India ink was performed to mark the site of a detected lesion or, in the absence of findings, at the deepest point of insertion.
MSE Efficacy and Safety Definition
-
Diagnostic yield was defined as the percentage of explorations with lesions compatible with the indication for the exam.
-
Technical success was defined as the percentage of explorations with the enteroscope advancing beyond the angle of Treitz (anterograde procedures) or proximally to the ileocecal valve (retrograde procedures).
-
Therapeutic yield was defined as the percentage of procedures with interventional treatments except for biopsy.
-
Interventional yield was defined as the percentage of procedures with at least one treatment or biopsy.
-
All adverse events were registered from the beginning of the procedure up to 14 days.
Performance Measures Definition
-
Depth of maximum insertion (DMI) was defined as the maximal distance accomplished from the angle of Treitz or the ileocecal valve; it was estimated with a previously published method, an assistant endoscopist counted the number of complete folds (valvulae conniventes) during withdrawal and then a conversion formula was applied (cm = number of folds × 0.9) [18, 19].
-
Total procedure time (TPT) was calculated from the beginning to the end of the endoscopic procedure.
-
Small bowel insertion time (SBIT) was calculated from the angle of Treitz or the ileocecal valve to the DMI.
Statistical Analysis
A per-patient analysis was conducted for demographic data, whilst a per-procedure description was adopted for performance measures and adverse events. All qualitative variables were expressed as frequency and percentages. Quantitative variables were presented as median and interquartile range (IQR). Univariate analyses were performed with the Chi-squared test (o Fisher’s exact test, whether appropriate) and Mann–Whitney U-test (for two-group comparison) or Kruskal–Wallis test (for three-group comparison); variables with p ≤ 0.1 were subsequently analyzed with binary multivariate analysis. p values < 0.05 were considered statistically significant. Statistical analysis was performed using SPSS Statistical Software, version 25 (IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp).
Results
Study Population and Indication for SB Exploration
One hundred-seventeen patients were analyzed, corresponding to 136 enteroscopy procedures (Table 1). Most patients were males (54.7%) with a median age of 67 years (IQR 58–74). Fifty patients (42.7%) had at least one previous major abdominal surgery: the most common surgeries were small bowel resection (n = 11), appendicectomy (n = 11), Cesarean section (n = 9), and cholecystectomy (n = 8). Full details are provided in Table 2. Overall technical success and diagnostic yield were 91.2% (124/136) and 66.9% (91/136), respectively. Therapeutic yield was 41.2% (56/136), including 46 treatments with Argon Plasma Coagulation (APC), 6 polypectomies, 3 combined treatments (APC and metallic clip placement), and 1 endoscopic balloon dilation of an ileal stricture. In 30.1% of procedures (41/136), at least one biopsy was taken. Interventional yield was 67.6% (92/136). The main clinical indications for SB exploration, pre-enteroscopy procedures, details on findings, and final enteroscopy diagnoses are fully described in Supplementary Material.
Efficacy of MSE Related to Prior Abdominal Surgery
Enteroscopy procedures in patients with prior major abdominal surgery (43.4%, n = 59) showed no significant differences in terms of technical success (89.9 vs 92.2%, p = 0.629), diagnostic yield (61 vs 71.4%, p = 0.201), and DMI (315 vs 204 cm, p = 0.226), whilst significant longer procedures times were observed: TPT (68 vs 55 min, p = 0.001) and SBIT (38 vs 29 min, p = 0.004). Interventional yield (62.7 vs 71.4%, p = 0.282) and therapeutic yield (44.1% vs 38.9%, p = 0.359) did not differ significantly.
A subpopulation analysis separating patients with gastrointestinal surgeries (n = 16) and other abdominal surgeries (n = 43) showed that patients with prior gastrointestinal surgery presented a lower DMI (189 vs 374 cm, p = 0.019), with equal SBIT (37.5 vs 38 min, p = 0.642) and diagnostic yield (56.3 vs 62.8%, p = 0.647). Complete comparison data are presented in Table 3.
Efficacy of MSE Related to the Route of Exploration
Seventy-four procedures (54.4%) were anterograde and 62 retrograde (45.6%). Sixteen patients (13.7%) underwent a combined approach (A-MSE and R-MSE). In 13 A-MSE (17.6%) esophageal dilation was performed (12 with bougie and 1 with a Controlled Radial Expansion balloon).
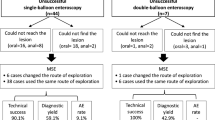
Diagnostic yield was 71.6% (53/74) for A-MSE and 61.3% (38/62) for R-MSE. In 31 (22.8%) procedures, the suspected lesion was not found (in 3 A-MSE and 11 R-MSE the DMI was limited by high intestinal fixation). Technical success was 91.9% (68/74) for A-MSE and 90.3% (56/62) for R-MSE. Data are shown in Table 4.
In 6.8% (5/74) of anterograde procedures, repeated automated motor stops occurred during the passage through the esophagus because of high resistance, thereby impeding the progression of the enteroscope to the stomach. In 1 anterograde procedure, the enteroscope could not pass the angle of Treitz due to high resistance on the spiral overtube at an angulated duodenal flexure. As per the retrograde procedures, in 5 patients, the ileocecal valve could not be intubated, whilst in 1 patient with multiple surgeries of the SB due to complicated appendicitis, the left colon could not be passed due to high bowel fixation. The median TPT was 60 min (IQR 51–89 min) for A-MSE, with a median time from mouth to the angle of Treitz of 4 min (IQR 3–6 min) and a median SBIT of 32 min (IQR 25–50 min). Regarding R-MSE, the TPT was 56 min (IQR 45–71 min) with a median time from anus to the ileocecal valve of 10 min (IQR 7–15 min) and a median SBIT of 31 min (IQR 21–48 min).
Median DMI was 415 cm (IQR 264–585 cm) for A-MSE and 120 cm (IQR 37–225 cm) for R-MSE. In 18 patients (15.4%), a complete SB exploration was performed: 10 of them were total anterograde enteroscopies and 6 were combined explorations (oral + anal route). In the other 2 anterograde procedures, the enteroscope reached the terminal ileum without passing the ileocecal valve: the site was tattooed and a posterior ileo-colonoscopy confirmed the localization in the terminal ileum.
Multiple binary logistic regression was performed, and SBIT was identified as a predictive factor associated with diagnostic yield (p = 0.008). Details are presented in Table 5.
Safety
The total number of procedure-related adverse events (AEs) was 14 (10.3%). No differences were detected in relation with major prior abdominal surgery (11.9 vs 9.1%, p = 0.282). In 7 patients, mild self-limiting abdominal pain was observed. In 5 anterograde procedures, during withdrawal phase, the enteroscope could not be pulled back from the stomach as the control unit safety system stopped the rotation due to high pressure on the spiral overtube at the height of the esophagus; this caused a prolongation of procedures and the need for multiple maneuvers of neck hyperextension, to avoid the marked angulation of the esophagus, multiples forward and backward advancements to change the enteroscope position, and, in a few cases, a gentle pressure to extract the enteroscope; however, no clinical sequelae were observed. Two (2.1%) serious adverse events (SAE) were observed. One patient, with history of mitral insufficiency and atrial fibrillation treated with acenocoumarol, underwent an anterograde enteroscopy which detected a 20 mm pediculated polyp; epinephrine injection and hot snare polypectomy were performed, followed by the placement of hemostatic clip collocation at polypectomy site; no immediate complications were observed. At 48 h, after the reintroduction of anticoagulation, the patient presented a few episodes of melena and was admitted to the hospital; the bleeding was self-limited and the patient was observed during 48 h with no further intervention required. In another patient undergoing anterograde enteroscopy, arytenoid edema was detected at withdrawal, requiring prolonged intubation of 24 h; the patient was a heavy smoker with oropharyngeal secretions that needed multiple maneuvers of aspiration during the procedure.
Discussion
The present study aimed at investigating the diagnostic yield and efficacy of MSE in the daily practice of a tertiary referral hospital, focusing on patients with prior major abdominal surgery. The study population represents a consecutive cohort of patients who underwent MSE according to findings of previous diagnostic exams.
The study population included a high percentage of procedures (43.4%) realized in patients with prior major abdominal surgery, which has been an exclusion criterion in the first published studies [12,13,14]. No significant differences were observed related to technical success (89.9 vs 92.2%, p = 0.629), with results comparable to previous studies [12,13,14, 16, 17]; diagnostic yield did not show significant differences related to abdominal surgery (61% vs 71.4%, p = 0.201) and was superior to the minimum requirements of European guidelines (\(\ge\) 50%) [3]. Both interventional (62.7 vs 71.4, p = 0282) and therapeutic yield (44.1 vs 38.9%, p = 0.359) were similar in both groups with equal adverse events rate (9.1 vs 9.1%, p = 0.598). However, MSE in patients with abdominal surgery showed significantly longer procedure time (TPT 68 min vs 55 min, p = 0.001), especially affecting the insertion phase (SBIT 38 min vs 29 min, p = 0.004). This can be explained by post-operative intestinal adhesions causing small bowel rigidity and hampering the advancement of the enteroscope. Moreover, intestinal surgeries represent the most relevant factor affecting the exploration, as the analysis of this subpopulation of patients showed similar exploration time (37.5 vs 38 min), but lower DMI (189 vs 374 cm) compared to patients with other abdominal surgeries; it demonstrates that surgeries directly involving the gastrointestinal tract make the exploration more demanding and, consequently, more time is needed to explore a shorter length of the small bowel.
Overall cohort adverse event rate was 10.3%, with 26.5% of patients in class III according to ASA (American Society of Anesthesiology) classification. These results are in line with the study by Beyna et al., showing a procedure-related AE rate of 14.4% [12]; in the study by Ramchandani et al., minor AEs accounted for 24.5%, whereas no major adverse events were observed [14]. Interestingly, the adverse event rate was not related to prior abdominal surgery (11.9 vs 9.1%, p = 0.598). Therefore, MSE might be considered technically feasible and safe in patients with previous abdominal surgery.
As regards the route of explorations, in anterograde procedures, MSE showed a high diagnostic yield (71.6%); these findings are in line with the previously published MSE feasibility trial showing a diagnostic yield of 74.2% [12], and superior to results previously described for DBE (64.4%) and SBE (53.9%) [20]. In recent studies, the technical success of this technique was described to be between 93 and 100% [12,13,14], which is similar to present results where the angle of Treitz was traversed in 91.9% of anterograde procedures. A-MSE technical success was not achieved in 6 cases due to difficulty in esophageal intubation or in passing the angle of Treitz in one patient with fixed duodenum; in this case, a posterior diagnosis of jejunal lymphoma was performed using SBE.
Regarding insertion depth, the present study showed a DMI of 415 cm for A-MSE with a median SBIT of 32 min (IQR 25–50 min), in line with previous MSE studies. In contrast, a recent meta-analysis by Baniya et al. that evaluated performance measures of balloon enteroscopy showed a mean DMI for anterograde balloon enteroscopy between 200 and 265 cm, with only two studies showing a DMI of 310 and 346 cm and a mean time to DMI of 45–46 min [21]. These data point out a clear advantage of MSE over balloon enteroscopy in this setting. Moreover, in the MSE feasibility trial, 10% of total anterograde enteroscopies was achieved and, in a recent trial specifically designed to evaluate total enteroscopies, the rate of total anterograde explorations was 16.6% [13]. In the present cohort of patients, complete visualization of the SB was achieved in 18 patients (15.4%), of these 12 were total anterograde explorations (10.3%) reaching the terminal ileum or cecum. This lower result may be explained by the inclusion of a different patient population.
Data on the efficacy of R-MSE are scarce. This study included 62 R-MSE, performed according to previous diagnostic exams; only 4 cases were performed to complete a negative partial anterograde exploration, finally detecting the suspected lesion. In R-MSE, diagnostic yield accounted for 61.3%, which is superior to results published for DBE (37–43%) and SBE (53.7%), although lower than the anterograde route [22, 23]. Technical success for retrograde procedures was 90.3%. In the two published studies where R-MSE was performed to complete negative anterograde explorations, technical success resulted in 100% [13, 14]. However, the previous series presented only a few cases of retrograde explorations and excluded patients with major abdominal surgeries.
In the retrograde route, DBE showed to achieve a DMI between 92 and 112 cm, although a slightly lower DMI was observed in SBE, accounting for between 68 and 91 cm [17,18,19]. In the present study, the median DMI for R-MSE explorations was 120 cm (37–225 cm). Insertion depth was limited by the strategy of pre-detecting suspected lesions and then selecting the retrograde route only for findings in the medium-distal ileum.
Multivariate analysis showed SBIT as the only independent factor associated with diagnostic yield in this population, remarking the importance of performing a careful and dedicated procedure.
The present data included the first cases performed with the novel enteroscope; however, it was postulated that MSE can be mastered quickly [12]. In the present cohort, the only change adopted after the first procedures was related to the use of esophageal bougienage; in the first three published studies on MSE, a previous dilation was conducted in all patients to facilitate the forward insertion of the endoscope [12,13,14]. In the present series, only 16.2% of A-MSE (12/74 procedures) included esophageal dilation. This practice was adopted in the first 12 cases, according to the experts’ recommendations. As per the following cases, a technical modification was introduced, limiting the use of bougienage to patients with esophageal narrowing detected by previous upper endoscopy or with difficult advancement of the enteroscope at the discretion of the endoscopist, in line with recently published multicenter studies [16, 17]. No adverse events related to this practice were observed.
In conclusion, MSE represents a valid alternative technique for SB exploration. A faster deep insertion length represents the strength of this novel device. Patients with previous abdominal surgery seem to present the inconvenience of longer exploration time, and prior gastrointestinal surgery may significantly reduce the depth of maximum insertion. However, this does not affect diagnostic yield or adverse events, being MSE effective and safe. Larger and multicenter studies are warranted to confirm these results. Further research is necessary to compare MSE with balloon enteroscopy and identify the best target population and predictive factors for diagnostic yield.
References
Schneider M, Höllerich J, Beyna T. Device-assisted enteroscopy: a review of available techniques and upcoming new technologies. World J Gastroenterol. 2019;25:3538–3545.
Pasha SF, Leighton JA, Das A et al. Double-balloon enteroscopy and capsule endoscopy have comparable diagnostic yield in small-bowel disease: a meta-analysis. Clin Gastroenterol Hepatol. 2008;6:671–676.
Spada C, McNamara D, Despott EJ et al. Performance measures for small-bowel endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. United Eur Gastroenterol J. 2019;7:614–641.
Cooley DM, Walker AJ, Gopal DV. From capsule endoscopy to balloon-assisted deep enteroscopy: exploring small-bowel endoscopic imaging. Gastroenterol Hepatol (N Y). 2015;11:143–154.
May A, Färber M, Aschmoneit I et al. Prospective multicenter trial comparing push-and-pull enteroscopy with the single-and double-balloon techniques in patients with small-bowel disorders. Am J Gastroenterol. 2010;105:575–581.
Akerman PA, Agrawal D, Cantero D et al. Spiral enteroscopy with the new DSB overtube: a novel technique for deep peroral small-bowel intubation. Endoscopy. 2008;40:974–978.
Ramkaji B, Subash CS et al. Balloon enteroscopy versus spiral enteroscopy for small-bowel disorders: a systematic review and meta-analysis. Gastrointest Endosc. 2017;86:997–1005.
Messer I, May A, Manner H et al. Prospective, randomized, single-center trial comparing double-balloon enteroscopy and spiral enteroscopy in patients with suspected small-bowel disorders. Gastrointest Endosc. 2013;77:241–249.
Neuhaus H, Beyna T, Schneider M et al. Novel motorized spiral enteroscopy: first clinical case. VideoGIE. 2016;1:32–33.
Mans L, Arvanitakis M, Neuhaus H et al. Motorized spiral enteroscopy for occult bleeding. Dig Dis. 2018;36:325–327.
González-Suárez B, Giordano A, Llach J. Are we experiencing a technological revolution? The novel motorized PowerSpiral enteroscope (PSE): a case of total oral enteroscopy. Rev Esp Enferm Dig 2020;112:331.
Beyna T, Arvanitakis M, Schenider M et al. Motorised Spiral enteroscopy? First prospective clinical feasibility study. Gut. 2021;70:261–267.
Beyna T, Arvanitakis M, Schneider M et al. Total motorized spiral enteroscopy: first prospective clinical feasibility trial. Gastrointest Endosc. 2021;93:1362–1370.
Ramchandani M, Rughwani H, Inavolu P et al. Diagnostic yield and therapeutic impact of novel motorized spiral enteroscopy in small-bowel disorders: a single-center real-world experience from a tertiary care hospital (with video). Gastrointest Endosc. 2021;93:616–626.
Achanta CR, Kinhal SV, Imandi V et al. Motorized spiral enteroscope guided biliary intervention for treatment of biliary obstruction in patient with hepaticojejunostomy. Am J Gastroenterol. 2022. https://doi.org/10.14309/ajg.0000000000001822.
Al-Toma A, Beaumont H, Koornstra JJ et al. The performance and safety of motorized spiral enteroscopy, including in patients with surgically altered gastrointestinal anatomy: a multicenter prospective study. Endoscopy. 2022. https://doi.org/10.1055/a-1783-4802.
Beyna T, Moreels T, Arvanitakis M et al. Motorized spiral enteroscopy: results of an international, multicenter, prospective observational clinical study on patients with normal and altered gastrointestinal anatomy. Endoscopy. 2022. https://doi.org/10.1055/a-1831-6215.
Efthymiou M, Desmond PV, Brown G et al. Single-01: a randomized, controlled trial comparing the efficacy and depth of insertion of single- and double-balloon enteroscopy by using a novel method to determine insertion depth. Gastrointest Endosc. 2012;76:972–980.
Ackerman P, Agrawal D, Cantero D et al. Spiral enteroscopy with the new DSB overtube: a novel technique for deep peroral small-bowel intubation. Endoscopy. 2008;40:974–978.
Lenz P, Domagk D. Double- vs. single-balloon vs. spiral enteroscopy. Best Pract Res Clin Gastroenterol. 2012;26:303–313.
Baniya R, Upadhya S, Subedi SC et al. Balloon enteroscopy versus spiral enteroscopy for small-bowel disorders: a systematic review and meta-analysis. Gastrointest Endosc. 2017;86:997–1005.
Teshima CW, Aktas H, Van Buurn HR et al. Retrograde double balloon enteroscopy: comparing performance of solely retrograde versus combined same-day anterograde and retrograde procedure. Scand J Gastroenterol. 2010;46:220–226.
Christian KE, Kapoor K, Goldberg EM. Performance characteristivcs of retrograde signle-balloon endoscopy: a signle center experience. World J Gastrointest Endosc. 2016;8:501–507.
Acknowledgments
None.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. No funding.
Author information
Authors and Affiliations
Contributions
BG-S and AG designed the research study, performed research, analyzed data and wrote the paper. GC, ME, OS, IKA, HC, JM-O collected data. GF-E, AC, ÀG, FB, GM-P, JL and ER contributed to the design of the study and revised the final manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Begoña González-Suárez: speaker fees from Olympus Spain and Norgine Iberia. Antonio Giordano: speaker fees from Olympus Spain. Gloria Fernández-Esparrach: consulting from Medtronic and CDx Diagnostics, speaker fees from Norgine Iberia and Olympus Spain. Àngels Ginès: consulting from Olympus Europe. Francesc Balaguer: endoscopic equipment on loan from Fujifilm, consulting from Sysmex, CPP-FAP speaker fees from Norgine. All other authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Giordano, A., Casanova, G., Escapa, M. et al. Motorized Spiral Enteroscopy Is Effective in Patients with Prior Abdominal Surgery. Dig Dis Sci 68, 1447–1454 (2023). https://doi.org/10.1007/s10620-022-07688-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07688-1