Abstract
Background
The histopathologic diagnosis of celiac disease (CD) may be challenging when the duodenal biopsies mucosal injury is limited. Intraepithelial T-lymphocytes (IELs) can be useful to characterize the degree of mucosal inflammation. A small fraction of IELs expresses the γδ T-cell receptor (named γδ-IELs), whose density, determined by flow cytometry or frozen section immunohistochemistry (IHC), is a specific marker for CD.
Aim
To establish a new IHC assay for γδ-IELs applicable to formalin-fixed paraffin-embedded (FFPE) duodenal biopsies.
Methods
We analyzed γδ-IELs using IHC in 138 duodenal biopsies using a standard IHC staining protocol with a new monoclonal antibody H-41. IELs were quantitated with digital image analysis.
Results
Compared to those in non-celiac controls (n = 51), γδ-IEL density was significantly increased in newly diagnosed celiac disease patients (n = 22, p < 0.0001). In ROC-curve analysis, the cutoff of 6.5 γδ-IELs/100 enterocytes distinguished optimally active CD patients from non-celiac controls (sensitivity 96%, specificity 95%). γδ-IEL density in CD patients on a gluten-free diet (n = 53) were also higher than in controls (p < 0.0001), but lower than those in newly diagnosed CD (p < 0.0001). The diagnostic value of γδ-IELs outperformed that of CD3 + IELs in both patient groups. γδ-IELs were better than CD3 + IELs distinguishing between celiac disease and conditions histologically mimicking celiac disease (n = 12).
Conclusions
Intraepithelial γδ T-lymphocytes can be stained and quantitated reliably in FFPE duodenal biopsies. The results showed excellent specificity and sensitivity for celiac disease. The new IHC method of detection of γδ-IELs is a promising addition to the routine histopathologic assessment methodology of celiac disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Celiac disease (CD) is an autoimmune disorder in which dietary gluten causes a gradually developing inflammation, villous atrophy, and crypt hyperplasia in the mucosa of the small intestine [1]. Currently, the only therapeutic option is a life-long, strict gluten-free diet (GFD), which is burdensome and limits the normal day-to-day life [1]. Active research is underway to develop drugs, vaccines, and safe dietary products to overcome the burden of this disease [2,3,4].
The histopathologic diagnosis of celiac disease presents no difficulties when biopsies from serologically positive patients show severe villous atrophy and crypt hyperplasia. Diagnostic difficulties may arise, however, when serology and biopsy findings are borderline. In such cases, there is significant interobserver variation between pathologists, and risk for both under- and overdiagnosis [5,6,7,8]. Histological findings may show celiac disease-unrelated inflammation (e.g., due to non-specific duodenitis, Helicobacter infection, or olmesartan use). Histologic diagnosis is often challenging in patients who have avoided gluten without a previous diagnosis of celiac disease.
Diagnostic approaches beyond conventional histopathology and serology have been introduced for the diagnosis of celiac disease [1 and references there in]. Quantitation of intraepithelial T-lymphocytes (IELs), identified by either hematoxylin-eosin (H&E) staining or CD3 immunohistochemistry (CD3-IHC), can be used to characterize celiac disease [7,8,9]. However, CD3 + IEL counts have been shown to overlap between diagnostic entities and cannot be used as the main criterion for celiac disease diagnosis [7, 8]. A small fraction of intraepithelial T-lymphocytes expresses the γδ T-cell receptor (γδ-IELs) [9,10,11]. Their abundance in the villus epithelium is a highly specific marker of celiac disease [10,11,12,13]. γδ-IEL densities respond to a gluten-free diet (GFD) and gluten challenge [3, 10, 12] but may remain slightly elevated despite a strict GFD [11, 12, 14]. Recent guidelines suggest that in doubtful cases, a high γδ-IEL density is an indicator of celiac disease diagnosis or evolving celiac disease [15, 16].
So far, the assessment of γδ-IELs has been performed mainly by flow cytometry (reviewed in 12, which is usually not available in daily histopathologic practice. Alternatively, immunohistochemistry of frozen or PAXgene-fixed tissue sections has been used with success [9,10,11, 17,18,19]. The only γδ antibody compatible with immunohistochemical detection has been the clone g3.20, which was recently withdrawn from the market. Prompted by this fact, Jungbluth et al. [20] tested several γδ T-lymphocyte antibodies and showed that the monoclonal antibody clone H-41 is a good choice to replace clone g3.20 in IHC of lymphomas. H-41 was shown to react with both the δ1 or δ2 chains of the T-cell receptor [20], making it potentially useful also for celiac disease research and diagnostics. We tested the utility of the monoclonal antibody H-41 in IHC of duodenal FFPE biopsies to detect γδ-IELs in newly diagnosed celiac disease patients, patients on a long-term GFD and non-celiac disease controls.
Materials and Methods
Patients
The study material was collected at “Casa Sollievo della Sofferenza” Hospital, San Giovanni Rotondo (Foggia, Italy), and half of the non-celiac control group at Central Finland Hospital (Jyväskylä, Finland). The material consisted of duodenal biopsies from 138 patients divided into four groups: First, 22 newly diagnosed untreated celiac disease patients were included. Second, we included 53 long-term treated celiac disease patients (GFD for at least 2 years). Forty-six of the GFD patients belonged to a randomized clinical trial of a dietary wheat product (ClinicalTrials.gov Identifier NCT03137862). Third, 12 patients had histologic diagnoses of well-known mimics of celiac disease as defined by signs of mucosal atrophy and/or intraepithelial lymphocytosis (see Tables 1 and 3). Fourth, 51 non-celiac disease control patients underwent clinically indicated upper gastrointestinal endoscopy due to unexplained abdominal symptoms, dyspepsia, or symptoms of gastroesophageal reflux without suspicion of celiac disease. In non-celiac control patients, celiac disease was excluded by negative celiac-specific serology and duodenal biopsy histopathological examination.
Biopsy Processing and Histopathology Analysis
Duodenal biopsy samples were taken during upper gastrointestinal endoscopy and fixed in neutral buffered formalin and embedded in paraffin blocks using a standard FFPE protocol. Tissue Sections (3–4 µm thick) were stained for H&E. Eighty-seven well-oriented samples were classified using morphometric measurements of villous height (VH) and crypt depth (CrD) ratios [21], which were further converted to the Marsh–Oberhuber grading system using the conversion table by Adelmann et al. [22]. The measurements were made by two scientists having large experience on quantitative histomoprhopmetry of celiac disease (co-authors A.P and J.T. of this study).
Immunohistochemistry
The FFPE biopsy tissue samples were sent to Jilab Inc., Tampere, Finland for immunohistochemical analysis. IHC for CD3-IELs was performed with a rabbit monoclonal anti-CD3 antibody (clone SP7, product RM-9107, Thermo Scientific, Waltham MA, dilution 1:300, incubation 1 h at room temperature). For γδ-IELs, a monoclonal antibody H-41 was used (product sc-100289, Santa-Cruz Biotechnology, Dallas TX, at dilution 1 µg/ml, incubation 1 h at room temperature). A standard IHC staining protocol using high-pH, high-temperature antigen retrieval (Tris-EDTA buffer, pH 9.0, 121C for 2 min), and a peroxidase-polymer-based detection kit (HistoFine Simple-Stain Nichirei Biosciences, Tokyo, Japan) was employed. Diaminobenzidine (DAB-2V, Nichirei) was used as chromogen (using reaction intensification with 0.5% copper sulphate) and hematoxylin for counterstaining. The staining procedure was carried out using an automated staining platform (LabVision Autostainer, ThermoFisher, Waltham, MA). An FFPE section of a known positive control (human tonsil) was included on every slide.
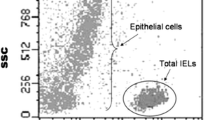
IEL Quantitation
Slides were scanned as high-resolution whole-slide images at a resolution of 0.16 µm per pixel (SlideStrider scanner, Jilab Inc., Tampere, Finland). Areas showing the strongest labeling at low magnification were chosen for CD3+ IEL and γδ IEL cell counting (hotspot sampling). IELs in three to six villi, containing at least 300 enterocytes, were counted automatically using our proprietary Auto-IEL software, which is a modification of our previously described IHC staining cell counting software [23]. In cases presenting with severe villous atrophy, IELs were counted from the flat surface epithelium of the mucosa. The CD3+- and γδ-IEL counts were adjusted per 100 enterocytes, denoted as “IEL density.” Measurements were independent of villous and crypt length data and clinical information.
Statistics
Descriptive statistics, group comparisons, and receiver-operator curve (ROC) analysis were performed using GraphPad Prism software (version 7.03, GraphPad Software San Diego, CA).
Results
The monoclonal antibody H-41 yielded a strong and crisp immunohistochemical staining reaction in duodenal FFPE mucosal tissues with standard high-pH antigen retrieval and a wide range of primary antibody concentrations. Nonspecific background staining was minimal (Fig. 1). With the optimized staining procedure for FFPE, γδ-IELs were visualized similarly to that described previously for frozen and Paxgene-fixed Sections [11, 20]. A high correlation was found between the densities of γδIELs stained with mAb H-41 and the currently unavailable mAb g3.20 in PAXgene-fixed serial sections published in our previous study (r = 0.85, n = 30, data not shown, ref 17).
Examples of immunohistochemistry of TCR γδ intraepithelial lymphocytes on formalin-fixed paraffin-embedded duodenal sections using monoclonal antibody H-41. Panel A represents non-celiac control, panel B represents a celiac patient on a gluten-free diet, and Panel C represents active celiac disease. Hematoxylin counterstain. Magnification × 200
Overall, IHC data from 138 patients were included in this study (Table 1). Digital image analysis using AutoIEL allowed highly reproducible enumeration of IELs, with interobserver correlation coefficient r = 0.9 between two readers. There was a modest positive correlation between CD3 + IEL and γδ-IEL densities in the entire biopsy material (r = 0.52, p < 0.001, data not shown).
In the analysis of the three patient subgroups (non-celiac, GFD celiac, and active CD patients), CD3 + and γδ IEL densities showed significant differences. In the non-celiac controls (n = 51), the median density of CD3 + IELs was 18 per 100 enterocytes (range 6–39), whereas the median density for γδ IELs was 2 (range 0–9, Fig. 2). Thus, of the CD3 + intraepithelial T-lymphocytes, on average 9% expressed the γδ T-cell receptor (range 0–47). Among celiac patients under a GFD (n = 53), the median CD3 + IEL density was 30/100 enterocytes (range 12–55), and that for γδ IELs was 12/100 (range 1–32), both being significantly higher than in non-celiac patients (p < 0.0001 for both). Altogether 38% of the intraepithelial CD3 + T-lymphocytes expressed the γδ receptor in this group (range 5–63). The IEL densities were highest in patients with newly diagnosed active celiac disease (n = 22), for whom the median density of CD3 + IELs was 59/100 (range 28–88), and 33/100 for TCR γδs (range 4–58) (significance for difference vs. non-celiac controls, p < 0.0001 for both, Fig. 2). On average, 41% of the intraepithelial CD3 + T-lymphocytes expressed γδ receptor in this group (range 12–133). The difference was also highly significant between CD patients on GFD and those with active disease (p < 0.0001).
Distribution of duodenal CD3 + and TCR γδ + intraepithelial lymphocyte densities in non-celiac controls, celiac mimics, celiac disease patients on a GFD, and celiac disease patients with active celiac disease. Median and 95% confidence intervals are shown with horizontal lines. Dashed horizontal lines show the diagnostic cutoffs (6.5 and 25, respectively)
Using receiver-operator curve (ROC) analysis, we defined an optimal cutoff value of 6.5/100 for γδ IEL density was able to distinguish between active celiac disease patients and disease controls (area under curve 0.9973, Fig. 3). Using this cutoff, and the commonly used 25/100 for CD3 + IELs, we defined their diagnostic value for celiac disease. As shown in Table 2, γδ IEL density outperforms CD3 in diagnostic classification. The sensitivity and specificity of γδ-IELs for active CD were 95% and 96%, respectively. Using the same cutoff, the sensitivity and specificity between controls and CD patients on GFD were 83% and 96%, respectively (Table 2). It should be noted that the cutoffs defined with the current biopsy material should be validated with independent biopsy materials to establish the true diagnostic value of γδ IEL counts defined by IHC on FFPE biopsies.
Histologic classification of CD usually includes the Marsh–Oberhuber classification to describe the degree of mucosal damage. We analyzed the CD3 + IEL and TCR γδ IEL data according to the Marsh–Oberhuber classes. There was a significant trend for higher CD3 + and γδ IEL densities in higher degrees of morphological damage (Marsh–Oberhuber types 3a-3c) (p = 0.001 by ANOVA, Fig. 4).
In routine histopathology, diagnosis of celiac disease may be challenging in patients presenting with non-specific duodenitis, Helicobacter infection, or olmesartan use. Therefore, we analyzed γδ IELs and CD3 + IELs in 12 selected patients, whose duodenal biopsy histology was reported to mimic celiac disease (Table 3). The results are shown in Table 3. Using the cutoff 6.5/100 for γδ-IELs, all cases fell below the cutoff suggesting the absence of celiac disease. In contrast, 7 of 12 could be considered suspicious for celiac disease because of CD3-IEL counts exceeding the commonly used cutoff 25/100. The quantitative IEL counts of CD mimics are compared to the other groups also in Fig. 2. Examples of duodenal mucosal CD3 and TCR γδ IHC stainings in a typical CD and a case of celiac mimic are shown in Fig. 5.
Comparison of CD3 and γδ IHC on serial formalin-fixed paraffin-embedded sections of duodenal biopsies representing active celiac disease (A, B), and drug-related duodenitis (C, D). The lack of intraepithelial TCR-γδ labeling suggests a diagnosis other than celiac disease. Hematoxylin counterstain. Magnification × 200
Discussion
The main finding in our γδ-IEL FFPE biopsy IHC study was excellent specificity and sensitivity for celiac disease, which was also evident in patients on a GFD. In non-celiac controls, the mean γδ-IEL density was only 2/100, and in biopsies mimicking celiac disease histology it was 4/100. Thus, in clinical diagnostics very low γδ-IEL densities are indicative of conditions other than celiac disease even without using digital image analysis. Our results are in line or even better than numerous flow cytometric studies reporting sensitivity varying between 66 and 97% and specificity between 91 and 97% [24, reviewed in 12]. When using IHC of γδ-IELs on frozen sections, slightly lower specificity and sensitivity have been reported in one study [11]. Thus, our IHC on FFPE sections seems to yield similar or better diagnostic results than previously used methods. The advantage of IHC is the possibility to use standard immunohistochemical staining on FFPE biopsy sections, which are readily available in pathology laboratories.
In addition to active celiac disease, we also observed slightly elevated γδ IEL densities in celiac patients who had been on a gluten-free diet for over 2 years. This suggests that even low amounts of inadvertent dietary gluten are sufficient to maintain the presence of γδ IELs. Alternatively, γδ IELs may be present in the villus epithelium as some kind of "memory cells" due to their invasion and abundance before the GFD. Biologically, it is surprising how little is known about the function of γδ-IELs at the molecular level. They are known to possess a regulatory function on gluten‐reactive helper T cells through the release of cytokines and growth factors, but more detailed knowledge of the functional properties remains obscure [25]. Whatever the pathogenetic explanation is, persistence γδ-IELs, also shown in a previous IHC study [19], could be a useful diagnostic feature when diagnosing celiac disease in patients who have been avoiding gluten before diagnostic work-up. In this situation, mucosal damage is usually partial, causing diagnostic uncertainty for villous atrophy. Elevated γδ IEL densities (> 6.5/100) favor the diagnosis of celiac disease irrespective of diet, as indicated by the high specificity and sensitivity. The pathogenetic relevance of higher γδ-IEL densities was evidenced by the significant correlation with Marsh–Oberhuber classification.
Analysis of γδ IELs in conditions histologically mimicking celiac disease provided information with potential differential diagnostic applicability. While CD3 + IELs could not distinguish mimics from a true CD very well, low γδ-IEL densities suggested the diagnosis other than CD in all 12 mimic cases studied. Although many more data sets are needed to establish this finding and the optimal cutoff, it is possible to speculate that H-41 γδ IEL IHC as an aid to the histologic classification of cases presenting with mild enteropathy [13, 26], as well as in patients negative for serum autoantibodies [24, 27].
In conclusion, we encourage researchers and pathology laboratories to test the new IHC method for γδ-IELs on FFPE biopsy materials to assist the diagnosis and classification of celiac disease. This new method may be useful in clinical diagnostics as well as in research, where archived paraffin blocks can now be studied. The utility of the new γδ IEL IHC assay in the diagnostics of pediatric celiac disease remains to be studied.
Change history
25 November 2020
A Correction to this paper has been published: https://doi.org/10.1007/s10620-020-06731-3
References
Lindfors K, Ciacci C, Kurppa K, et al. Coeliac disease (review). Nat Rev Dis Primers. 2019;5:3.
Lähdeaho ML, Scheinin M, Vuotikka P, et al. Safety and efficacy of AMG 714 in adults with coeliac disease exposed to gluten challenge: a phase 2a, randomised, double-blind, placebo-controlled study. Lancet Gastroenterol Hepatol. 2019;4:948–959.
Lähdeaho ML, Kaukinen K, Laurila K, et al. Glutenase ALV003 attenuates gluten-induced mucosal injury in patients with celiac disease. Gastroenterology. 2014;146:1649–1658.
Cellier C, Bouma G, van Gils T, et al. Safety and efficacy of AMG 714 in patients with type 2 refractory coeliac disease: a phase 2a, randomised, double-blind, placebo-controlled, parallel-group study. Lancet Gastroenterol Hepatol. 2019;4:960–970.
Villanacci V, Lorenzi L, Donato F, et al. Histopathological evaluation of duodenal biopsy in the PreventCD project. An observational interobserver agreement study. APMIS. 2018;126:208–214.
Werkstetter KJ, Korponay-Szabo IR, Popp A, et al. Accuracy in diagnosis of celiac disease without biopsies in clinical practice. Gastroenterology. 2017;53:924–935.
Robert ME, Crowe SE, Burgart L, et al. Statement on best practices in the use of pathology as a diagnostic tool for celiac disease: a guide for clinicians and pathologists. Am J Surg Pathol. 2018;42:e44–e58.
Kirmizi A, Kalkan C, Yuksel S, et al. Discriminant value of IEL counts and distribution pattern through the spectrum of gluten sensitivity: a simple diagnostic approach. Virchows Arch. 2018;473:551–558.
Holm K, Mäki M, Savilahti E, et al. Intraepithelial gamma delta T-cell-receptor lymphocytes and genetic susceptibility to celiac disease. Lancet. 1992;339:1500–1503.
Iltanen S, Holm K, Ashorn M, et al. Changing jejunal γδ T cell receptor (TCR)-bearing intraepithelial lymphocyte density in coeliac disease. Clin Exp Immunol. 1999;117:51–55.
Järvinen TT, Kaukinen K, Laurila K, et al. Intraepithelial lymphocytes in celiac disease. Am J Gastroenterol. 2003;98:1332–1337.
Fernández-Bañares F, Carrasco A, Martín A, Esteve M. Systematic review and meta-analysis: accuracy of both gamma delta+ intraepithelial lymphocytes and coeliac lymphogram evaluated by flow cytometry for coeliac disease diagnosis. Nutrients. 2019;11:E1992.
Auricchio R, Mandile R, Del Vecchio MR, et al. Progression of celiac disease in children with antibodies against tissue transglutaminase and normal duodenal architecture. Gastroenterology. 2019;157:413–420.
Calleja S, Vivas S, Santiuste M, Arias L, Hernando M, Nistal E, Casqueiro J, De Morales JGR. Dynamics of non-conventional Intraepithelial lymphocytes—NK, NKT, and γδ T—in celiac disease: relationship with age, diet, and histopathology. Dig Dis Sci. 2011;56:2042–2049. https://doi.org/10.1007/s10620-010-1534-5.
Husby S, Koletzko S, Korponay-Szabó I, et al. European Society for pediatric gastroenterology, hepatology, and nutrition guidelines for the diagnosis of coeliac disease. J Pediatr Gastroenterol. 2020;70:141–156.
Al-Toma A, Volta U, Auricchio R, et al. European Society for the Study of Coeliac Disease (ESsCD) guideline for coeliac disease and other gluten-related disorders. United Eur Gastroenterol J. 2019;7:583–613.
Taavela J, Viiri K, Popp A, et al. Histological, immunohistochemical and mRNA gene expression responses in coeliac disease patients challenged with gluten using PAXgene fixed paraffin-embedded duodenal biopsies. BMC Gastroenterol. 2019;19:189.
Lonardi S, Villanacci V, Lorenzi L, et al. Anti-TCR gamma antibody in celiac disease: the value of count on formalin-fixed paraffin-embedded biopsies. Virchows Arch. 2013;463:409–413.
Zanini B, Marullo M, Villanacci V, et al. Persistent intraepithelial lymphocytosis in celiac patients adhering to gluten-free diet is not abolished despite a gluten contamination elimination diet. Nutrients. 2016;8:525.
Jungbluth A, Frosina D, Fayad M, et al. Immunohistochemical detection of γ/δ T lymphocytes in formalin-fixed paraffin-embedded tissues. Appl Immunohistochem Mol Morphol. 2019;8:581–583.
Taavela J, Koskinen O, Huhtala H, et al. Validation of morphometric analyses of small-intestinal biopsy readouts in celiac disease. PLoS One. 2013;11:8.
Adelman DC, Murray J, Tsung-Teh W, et al. Measuring change in small intestinal histology in patients with celiac disease. Am J Gastroenterol. 2018;113:339–347.
Tuominen VJ, Ruotoistenmäki S, Viitanen A, et al. ImmunoRatio: a publicly available web application for quantitative image analysis of estrogen receptor (ER), progesterone receptor (PR), and Ki-67. Breast Cancer Res. 2010;12:R56.
Fernández-Bañares F, Crespo L, Núñez C, et al. Gamma delta+ intraepithelial lymphocytes and coeliac lymphogram in a diagnostic approach to coeliac disease in patients with seronegative villous atrophy. Aliment Pharmacol Ther. 12/Feb/2020. [Epub ahead of print]
Bhagat G, Naiyer AJ, Shah JG, et al. Small intestinal CD8+TCRγδ+NKG2A+ intraepithelial lymphocytes have attributes of regulatory cells in patients with celiac disease. J Clin Invest. 2008;118:281–293.
Kurppa K, Collin P, Viljamaa M, et al. Diagnosing mild enteropathy celiac disease: a randomized, controlled clinical study. Gastroenterology. 2009;136:816–823.
Salmi T, Collin P, Korponay-Szabo IR, et al. Endomysial antibody-negative coeliac disease: clinical characteristics and intestinal autoantibody deposits. Gut. 2006;55:1746–1753.
Funding
The study was partly supported by the Competitive State Research Financing of the Expert Responsibility Area of Tampere University Hospital, Grants Nos. 9X035 and 9AA053 (AP,MM).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: First name and the surname of all the authors in the author group were corrected.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Popp, A., Taavela, J., Graziano, P. et al. A New Intraepithelial γδ T-Lymphocyte Marker for Celiac Disease Classification in Formalin-Fixed Paraffin-Embedded (FFPE) Duodenal Biopsies. Dig Dis Sci 66, 3352–3358 (2021). https://doi.org/10.1007/s10620-020-06680-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06680-x