Abstract
Background
Defining factors associated with severe reflux esophagitis allows for identification of subgroups most at risk for complications of strictures and esophageal malignancy. We hypothesized there might be unique clinical features in patients with reflux esophagitis in a predominantly Hispanic population of a large, safety-net hospital.
Aim
Define clinical and endoscopic features of reflux esophagitis in a predominantly Hispanic population of a large, safety-net hospital.
Methods
This is retrospective comparative study of outpatients and hospitalized patients identified with mild (Los Angeles Grade A/B) and severe (Los Angeles Grade C/D) esophagitis through an endoscopy database review. The electronic medical record was reviewed for demographic and clinical data.
Results
Reflux esophagitis was identified in 382/5925 individuals: 56.5% males and 79.8% Hispanic. Multivariable logistic regression model adjusted for age, gender, race, body mass index (BMI), tobacco and alcohol use, and hospitalization status with severity as the outcome showed an interaction between gender and BMI (p ≤ 0.01). Stratification by gender showed that obese females had decreased odds of severe esophagitis compared to normal BMI females (OR = 0.18, 95% CI = 0.07-0.47; p < 0.01). In males, the odds of esophagitis were higher in inpatient status (OR = 2.84, 95% CI = 1.52 − 5.28; p < 0.01) and as age increased (OR = 1.37, 95% CI = 1.03 − 1.83; p = 0.03).
Conclusions
We identify gender-specific associations with severe esophagitis in a predominantly Hispanic cohort. In females, obese BMI appears to be protective against severe esophagitis compared to normal BMI, while in men inpatient status and increasing age were associated with increased odds of severe esophagitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastroesophageal reflux disease (GERD) afflicts over 20% of American adults, and the burden of disease appears to be increasing worldwide [1]. GERD-related esophagitis can lead to additional complications such as strictures and Barrett’s esophagus, the only known precursor of esophageal adenocarcinoma [2]. Identification of risk factors for severe esophagitis can help identify populations most at risk for these complications and allow for proper allocation of limited endoscopic resources.
Male gender [3, 4], Caucasian ethnicity [3,4,5], and obesity [3, 4, 6, 7] have previously been identified as risk factors for severe esophagitis (Los Angeles classification Grades C, D). However, reports about the role of obesity and its association with GERD and its complications have been contradictory [6, 8,9,10,11]. Further, the applicability of reported risk factors for severe esophagitis in the vulnerable population served by a safety-net hospital or in the burgeoning Hispanic population is unknown. We were therefore interested in exploring risk factors for severe esophagitis in this population. Our aim was to determine clinical and endoscopic features of reflux esophagitis and to identify risk factors for reflux esophagitis in the predominantly Hispanic population of a large, safety-net hospital. Understanding risk factors for severe esophagitis in a potentially vulnerable population provides the opportunity to identify subgroups most at risk for complication of GERD.
Materials and Methods
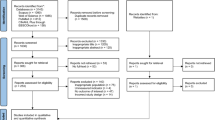
Study Design and Population
A retrospective comparative study was designed to examine the clinical and endoscopic characteristics of mild and severe esophagitis. The study population was comprised of outpatients and inpatients who underwent esophagogastroduodenoscopy (EGD) at the endoscopy suite at Los Angeles County Hospital (LAC) between January 2017 and December 2018 and were identified with esophagitis through an endoscopy database review. In patients who underwent multiple endoscopies during the time period of the study, only the first one was recorded. LAC is a multidisciplinary teaching hospital affiliated with the University of Southern California and is a safety-net hospital for underserved patients. The study was approved by the University of Southern California Institutional Review Board. All authors had access to the study data and reviewed and approved the final manuscript prior to submission.
Data Collection
The electronic medical record was reviewed for demographic and clinical data. Demographic data collected included age, sex, and ethnicity/race. Tobacco and alcohol use were also recorded based on chart review. Clinical data included body mass index (BMI), hospitalization status, listed medications, comorbidities, and indications for endoscopy. BMI was calculated from data extracted from the chart at the time of endoscopy. BMI was calculated by dividing weight (kg) by height squared (m2) at the time of endoscopy and was categorized as underweight (< 18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (≥ 30 kg/m2). Endoscopy reports were reviewed for the presence of hiatal hernia, strictures, or Barrett’s esophagus. Esophagitis severity was defined according to the Los Angeles (LA) classification as A, B, C, or D and was dichotomized into two populations a priori. Those with Los Angeles Grade A/B were classified as mild esophagitis and those with Grade C/D as severe esophagitis [4]. Endoscopic images were reviewed to confirm the LA classification and for the presence of stricture or hiatal hernia or Barrett’s esophagus. We excluded non-erosive disease and Barrett’s esophagus, focusing only on erosive esophagitis as a complication of GERD.
Statistical Analysis
The median and interquartile ranges (IQR) were reported for continuous variables that were not normally distributed, and the frequency counts and percentages were reported for the categorical variables. A Wilcoxon test was performed to assess whether continuous variables differed by severity, and a Chi-square test or Fisher’s exact test was performed to assess whether the categorical variables differed by severity. Similar methods were used to assess indication for endoscopy, endoscopy findings, and medication. Subgroup analyses were also performed to observe the differences in baseline characteristics by severity groups for inpatients, outpatients, males, and females. A multivariable logistic regression was performed on severity outcome adjusting for age, gender, race, BMI, tobacco use, alcohol use, and hospitalization status. Due to the interaction of BMI and gender, analyses were stratified by gender. The odds ratio, 95% confidence interval, and p values were reported. Age was reported as 10-year increments. Significance tests were two-tailed, with α = 0.05. All analyses were performed using SAS software v. 9.4 (SAS Institute Inc.).
Results
Baseline Characteristics of Patients
Reflux esophagitis was identified in 382 individuals out of 5925 upper endoscopies (6.4%) at our institution; 56.5% were males and 43.5% female (Table 1). The median age was 55.6 years. Most patients (79.8%) were Hispanic, followed by 8.4% Caucasian, 5.8% African American, and 6.0% other (Korean, Chinese, and Filipino). There were 64.7% of esophagitis cases identified during outpatient endoscopy, and 35.3% were identified during inpatient endoscopy.
There were 59% (n = 225) of esophagitis cases that were mild and 41% (n = 157) of cases that were severe. The median ages of those with mild and severe esophagitis were 56 and 58 years old, respectively (p = 0.05). Patients with mild esophagitis were 52% male and 48% female, while those with severe esophagitis were 63.1% male and 36.9% female (p = 0.03). Hospitalization status significantly differed between severity groups (p < 0.01). There was a higher percentage of outpatients in the mild group (74.2% vs. 25.8%) and a similar distribution of outpatients and inpatients in the severe group (52% vs. 49%). There were no significant differences in tobacco and alcohol use in mild vs severe esophagitis.
The majority of individuals in our cohort were either obese or overweight (n = 269, 70.4%). BMI categories differed between the severity groups (p < 0.01). There was a higher distribution of underweight and normal weight patients in the severe group compared to the mild group (7.7% vs. 2.7% and 32.1% vs. 19.6%, respectively), and a higher percentage of obese patients in the mild group compared to the severe group (41.8% vs. 22.4%).
Comorbidities and Indications for Endoscopy
A number of listed comorbidities were captured during the time period of the study (Table 2). Comorbidities were not mutually exclusive, and a patient may have reported multiple comorbidities. The primary comorbidities in all patients undergoing endoscopy were GERD (n = 127), followed by diabetes (n = 112), and cirrhosis (n = 74). The most frequent comorbidity in patients with mild esophagitis was diabetes (32.0%), and the most frequent comorbidity in severe esophagitis was GERD (38.2%). Cirrhosis was more frequently a recorded comorbidity in mild versus severe esophagitis (23.1% vs. 14.0%, p = 0.03). All other comorbidities were not statistically different between mild and severe esophagitis.
Various indications for endoscopy were also recorded during the time period of the study. Indications for endoscopy were not mutually exclusive, and a patient may have reported multiple indications. The primary indications for endoscopy in all patients were gastrointestinal bleeding (n = 98), followed by surveillance for history of esophagitis (n = 80), iron-deficiency anemia (n = 68), dysphagia/odynophagia (n = 58), reflux/regurgitation (n = 53), and abdominal pain (n = 45) (Table 3). Nausea/vomiting (n = 25), abnormal imaging (n = 21), and other (n = 19) were remaining indications. In those with mild esophagitis, the most frequent indication for endoscopy was a surveillance endoscopy for a prior history of esophagitis (25.3%). In those with severe esophagitis, gastrointestinal bleeding (35%) was the most frequent indication. Gastrointestinal bleed (35% vs. 19.1%, p < 0.01), dysphagia (22.9% vs. 9.8%, p < 0.01), and nausea/vomiting (10.2% vs. 4%, p = 0.02) were more frequent indications for endoscopy in severe versus mild esophagitis. There was a higher rate of surveillance endoscopy in mild esophagitis patients compared to severe esophagitis patients (25.3% vs. 14.7%, p = 0.01). The remainder of indications for endoscopy was similar between mild and severe esophagitis.
Endoscopic Findings
The most common endoscopic finding overall was hiatal hernia (n = 191, 50%) (Table 4). First time and repeat endoscopies accounted for nearly 70% and 30% of procedures, respectively. Hiatal hernia (58.6% vs. 44%, p < 0.01) and esophageal strictures (11.5% vs. 4%, p = 0.01) were more frequent in severe than mild esophagitis. Endoscopy findings were not mutually exclusive, and a patient may have reported multiple findings.
Medication Use
Proton-pump inhibitor use was similar per review of the electronic medical record between mild (44.9%, n = 101) and severe esophagitis (48.4%, n = 76) (Table 5). Other medications that were recorded included H2 antagonists, aspirin, clopidogrel, NSAIDs, and corticosteroids. Patients may have been on multiple medications. Clopidogrel was reported in eight patients with mild esophagitis, and there was no clopidogrel use in cases of severe esophagitis (p = 0.02). Other medication use between groups was similar.
Hospitalization Status and Esophagitis Severity
The diagnosis of esophagitis in our endoscopy database reflected a heterogeneous population of inpatients and outpatients, which recent reports suggest may have distinct disease pathogenesis [10]. We therefore evaluated characteristics of outpatients and inpatients separately.
Among 247 patients diagnosed with esophagitis as outpatients, 51.4% were male and 67.6% had mild esophagitis, while 32.4% had severe esophagitis (Table 6). Obese BMI was reported in 41.3% of outpatients with esophagitis. BMI categories differed between outpatients with mild and severe esophagitis (p < 0.01). Outpatients with severe esophagitis had a higher percentage of patients with underweight, normal weight, and overweight BMI compared to those with mild esophagitis, while those with mild esophagitis had a higher percentage of patients with obese BMI.
Among 135 cases of inpatient esophagitis, 65.9% were male and 43.0% had mild esophagitis and 57.0% had severe esophagitis (Table 7). There were no significant differences in baseline characteristics between mild and severe esophagitis groups.
Gender and Severity of Esophagitis
We were then interested in examining baseline characteristics in our population by gender and by severity of esophagitis (Table 8). In males, the median age in severe patients was higher than in mild patients (p = 0.03). Females with mild esophagitis had a higher median age than males with mild esophagitis (p = 0.03). There was no difference in the median ages of females and males with severe esophagitis.
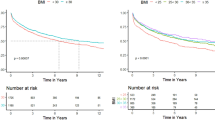
BMI differed in females with mild versus severe esophagitis (p < 0.01). More than half the female patients with mild esophagitis had an obese BMI (55.6%), while 17.5% of females with severe esophagitis had an obese BMI. There was no statistical difference between BMI and severity groups within males.
Race/ethnicity was similar across esophagitis severity in males and females, with most patients being Hispanic. Men reported more current/former alcohol and tobacco use than females in mild (p < 0.01) and severe (p < 0.01) esophagitis. However, there was no difference in tobacco or alcohol exposure within either gender in mild versus severe esophagitis. Esophagitis severity differed by hospital status for both females (p = 0.01) and males (p < 0.01). For both genders, there was a higher percentage of outpatient hospitalization among mild esophagitis patients compared to severe patients (females: 78.7% vs. 60.3%, males: 70.1% vs. 45.5%).
Multivariable Logistic Regression Model
We then performed a multivariable logistic regression model adjusting for several variables including age, gender, race, BMI, tobacco use, alcohol use, and hospitalization status with severity as the outcome. There was an interaction between gender and BMI (p = 0.01); therefore, we stratified the multivariable logistic regression by gender (Table 9). In females, there was a decrease in odds of severe esophagitis (OR = 0.18, 95% CI = 0.07 − 0.47, p < 0.01) if the patient had an obese BMI compared to having a normal BMI, after adjusting for all the variables. In males, the odds of severity in inpatients were 2.84 times the odds among outpatients (OR = 2.84, 95% CI = 1.52 − 5.28, p < 0.01). The odds of severe esophagitis were 1.37 (95% CI = 1.03 − 1.83, p = 0.03) times higher for every 10-year increase in age in males after adjusting for the covariates.
Discussion
To our knowledge, this is one of a few cohort studies examining risks for esophagitis severity in a predominantly Hispanic population of a large safety-net hospital that included similar numbers of males and females. Previous studies examining complications of gastroesophageal reflux disease have been skewed toward males and/or did not have significant Hispanic representation [5, 10]. Multivariable logistic regression stratified by gender identified gender-specific risks in this unique population. Females with obese BMI had decreased odds of severe esophagitis compared to normal BMI females after adjusting for all other variables. Inpatient status and increasing age were associated with increased odds of severe esophagitis in males only.
Our results are consistent with multiple epidemiologic studies that reported erosive esophagitis was more predominant in males [12]. This difference has been hypothesized to be due to the more truncal distribution of body fat in men compared to the visceral distribution in women. We did not evaluate distribution of body fat in this study. Epidemiologic studies also suggest that severity of erosive esophagitis is related to the reproductive hormone status in women and may be increased in the postmenopausal state [12]. We did not record menstrual status in this study. However, we did look at age in mild vs severe esophagitis. In our study, there was a not a significant difference in the age of women with severe vs mild esophagitis. Future studies and analysis will address menopausal state and use of hormone replacement therapy. Interestingly, in our cohort, age was associated with an increased odds ratio of severe esophagitis in males only (Table 7).
Our work adds to the complexity of the existing literature regarding the role of obesity in the pathogenesis of esophagitis. For example, overweight and obesity as defined by BMI have been reported as risk factors for GERD symptoms and esophageal erosions in a cross-sectional study consisting of surveys followed by endoscopy [6]. A more recent study looked at the effect of ethnicity and gender on the association between erosive esophagitis and obesity [8]. This case control study of outpatients that were 43% Hispanics showed overweight and obese subjects were more likely to have erosive esophagitis than individuals with normal BMI. The effect of BMI on erosive esophagitis did not appear to vary by race/ethnicity or gender. As noted by the authors, however, the risk of erosive esophagitis with a BMI of 35–39.9 kg/m2 was lower than those with a BMI of 30–34.9 kg/m2. Further, although an increased OR of erosive esophagitis with obesity was reported in both males and females, the severity of esophagitis (i.e., mild vs. severe) was not considered in this study [8]. A meta-analysis of twenty-one studies demonstrated a strong association with increasing BMI and erosive esophagitis in males, but not females [9], while the converse was found in a case–control study [11]. Finally, a retrospective study in a Chinese population demonstrated a positive association between obesity and erosive esophagitis [13].
Although a previous study has reported the association of lower BMI with more severe esophagitis, the population consisted predominantly of White and African American males, with the majority of cases of severe esophagitis made in hospitalized patients [10]. Our patient population was predominantly Hispanic, included similar numbers of males and females, with similar number of cases of severe esophagitis in outpatients and inpatients. Our results showed inpatient hospitalization was associated with an increased OR for severe esophagitis in males only. This finding is consistent with previous reports [10] although it is not clear why inpatient status was not associated with an increased OR of severe esophagitis in females.
There are several limitations to our work. The retrospective nature and its basis on an endoscopy database make the results subject to selection bias. Although “surveillance” was listed as an indication more frequently in mild versus severe esophagitis, there was no difference in antacid use between the two groups. We might be minimizing the number of severe esophagitis cases because of healed esophagitis, and also, PPI use was not recorded in between repeat endoscopies. Medication use was informed by chart review, without pharmacy verification, medicine reconciliation, or telephone interview. Unfortunately, we were not able to find data on compliance and duration of antacid therapy. Antacid medications recorded were a combination of both prescribed and over-the-counter antacids. Medication data may also be inaccurate given that antacids are widely available over the counter and because we did not distinguish whether they were prescribed or taken over the counter and did not follow up on compliance or duration of therapy.
Another limitation is that captured comorbidities were based on documentation available at time of chart review without verification of associated diagnostic studies, potentially leading to inaccuracies and bias. Weight loss as a comorbidity was not specifically captured by this method. Cirrhosis was recorded more frequently in mild esophagitis than in severe esophagitis. However, the etiology of liver disease, including the presence of nonalcoholic fatty liver disease, given its association with metabolic syndromes such as obesity [14], was not recorded.
In addition, all potential indications for the endoscopy may not have been captured by review of the electronic medical record and or endoscopy database, thus further contributing to bias. We also did not quantify alcohol/tobacco consumption, and given the retrospective nature of the study, this information was likely incomplete. We cannot infer causality based on a retrospective single-center study. Although there was no interaction between race/ethnicity and BMI, the majority of population was Hispanic, and conclusions may not be applicable to broader community.
Finally, we recognize that there are several measures of obesity. Prior studies have demonstrated that the pattern of body fat distribution rather than BMI alone may be critical to the pathogenesis of GERD complications [15, 16], presumably through pro-inflammatory effects of metabolically active visceral fat particularly for development of Barrett’s esophagus [17, 18], although mechanisms leading to erosive esophagitis per se remain largely undefined. A recent systematic review and meta-analysis identified an association between central adiposity (measured using visceral adipose tissue, waist–hip ratio and waist circumference) and an increased risk of erosive esophagitis [19]. While BMI may be an imperfect surrogate for central adiposity, it was the only readily available measure for this retrospective study.
In conclusion, this retrospective study aimed to identify unique characteristics of esophagitis in a predominantly Hispanic population of a large safety-net hospital with significant male and female representation. In males, there was an association between severity of esophagitis with age and hospitalization. These results show that previous studies identifying increasing age and inpatient status as risk factors for severe esophagitis are applicable to the predominantly Hispanic males cared for at our safety-net hospital. We also identified an association between severity of esophagitis and BMI in females. Notwithstanding potential limitations of this study, this novel observation merits investigation of the potential mechanisms mediating the observed difference in esophagitis severity in females along the BMI spectrum. Larger studies will also be needed to determine whether this association extends to other ethnicities.
This study was performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study format, consent is not required.
References
El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the Epidemiology of Gastro-Oesophageal Reflux Disease: a Systematic Review. Gut. 2014;63:871–880.
Parasa S, Sharma P. Complications of Gastro-Oesophageal Reflux Disease. Best Pract Res Clin Gastroenterol. 2013;27:433–442.
El-Serag HB, Johanson JF. Risk Factors for the Severity of Erosive Esophagitis in Helicobacter Pylori-Negative Patients with Gastroesophageal Reflux Disease. Scandinavian J Gastroenterol. 2002;37:899–904.
Katzka DA, Pandolfino JE, Kahrilas PJ. Phenotypes of Gastroesophageal Reflux Disease: Where Rome, Lyon, and Montreal Meet. Clin Gastroenterol Hepatol. 2020;18(4):767–776.
Spechler SJ, Jain SK, Tendler DA, Parker RA. Racial Differences in the Frequency of Symptoms and Complications of Gastro-Oesophageal Reflux Disease. Aliment Pharmacol Therapeut.. 2002;16:1795–1800.
El-Serag HB, Graham DY, Satia JA, Rabeneck L. Obesity is an Independent Risk Factor for GERD Symptoms and Erosive Esophagitis. Am J Gastroenterol. 2005;100:1243–1250.
Tack J, Pandolfino JE. Pathophysiology of Gastroesophageal Reflux Disease. Gastroenterology. 2018;154:277–288.
Abraham A, Lipka S, Hajar R, et al. Erosive Esophagitis in the Obese: the Effect of Ethnicity and Gender on its Association. Gastroenterol Res Pract. 2016;2016:7897390.
Cai N, Ji GZ, Fan ZN, et al. Association Between Body Mass Index and Erosive Esophagitis: a Meta-Analysis. World J Gastroenterol WJG.. 2012;18:2545–2553.
Nguyen AD, Spechler SJ, Shuler MN, Souza RF, Dunbar KB. Unique Clinical Features of Los Angeles Grade D Esophagitis Suggest that Factors Other Than Gastroesophageal Reflux Contribute to its Pathogenesis. J Clin Gastroenterol. 2019;53:9–14.
Nilsson M, Lundegardh G, Carling L, Ye W, Lagergren J. Body Mass and Reflux Oesophagitis: an Oestrogen-Dependent Association? Scand J Gastroenterol. 2002;37:626–630.
Asanuma K, Iijima K, Shimosegawa T. Gender Difference in Gastro-Esophageal Reflux Diseases. World J Gastroenterol WJG.. 2016;22:1800–1810.
Lee SW, Lien HC, Lee TY, Tung CF, Yeh HZ, Chang CS. Impact of Obesity on a Chinese Population with Erosive Esophagitis and Barrett’s Esophagus. Gut Liver.. 2017;11:377–382.
Younossi Z, Anstee QM, Marietti M, et al. Global Burden of NAFLD and NASH: Trends, Predictions, Risk Factors and Prevention. Nat Rev Gastroenterol Hepatol.. 2018;15:11–20.
Lagergren J. Influence of Obesity on the Risk of Esophageal Disorders. Nat Rev Gastroenterol Hepatol.. 2011;8:340–347.
Nam SY, Choi IJ, Ryu KH, Park BJ, Kim HB, Nam BH. Abdominal Visceral Adipose Tissue Volume is Associated with Increased Risk of Erosive Esophagitis in Men and Women. Gastroenterology. 2010;139:1902–1911.
Francois F, Roper J, Goodman AJ, et al. The Association of Gastric Leptin with Oesophageal Inflammation and Metaplasia. Gut. 2008;57:16–24.
Coussens LM, Werb Z. Inflammation and Cancer. Nature. 2002;420:860–867.
Singh S, Sharma AN, Murad MH, et al. Central Adiposity is Associated with Increased Risk of Esophageal Inflammation, Metaplasia, and Adenocarcinoma: a Systematic Review and Meta-Analysis. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Ass.. 2013;11:1399–1412.
Funding
This study was supported in part by National Institutes of Health DK118065 (AS) and SC CTSI grant #s UL1TR001855 and UL1TR000130.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declared that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Haghighat, S., Park, C., Horwich, B. et al. Gender-Specific Risk Factors for Reflux Esophagitis in a Predominantly Hispanic Population of a Large Safety-Net Hospital. Dig Dis Sci 66, 1940–1948 (2021). https://doi.org/10.1007/s10620-020-06482-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06482-1