Abstract
Background/Aims
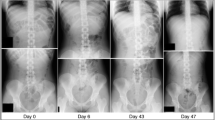
There is currently no gold standard for evaluating stool burden in the colon for patients with gastrointestinal symptoms. We aim to examine the relationship between fecal loading on single view abdominal X-ray imaging and gastrointestinal symptoms such as constipation, diarrhea, bloating, and accidental bowel leakage in adult outpatients.
Methods
This retrospective, cross-sectional study examined patients seen at University of Michigan from 2005 to 2017. Chart review of demographic information, reported gastrointestinal symptoms, past medical history, and abdominal radiographic imaging was performed. Bivariate analysis was performed to assess associations between these characteristics and fecal loading. Factors independently associated with fecal loading were identified using logistic regression. Significance was established at p < 0.05.
Results
In total, 319 patients who had an X-ray were included in the final analysis, with 84.0% demonstrating fecal loading on the initial X-ray and most reporting constipation as a symptom (n = 214, 84.3%, p = 0.0334). In logistic regression, a chief complaint of constipation had higher odds of being associated with fecal loading on X-ray compared to diarrhea (adjusted OR 6.41; CI 1.51–27.24, p = 0.0118). Bloating as a reported symptom was statistically significant with an adjusted OR of 2.56 (CI 1.10–5.96, p = 0.0286).
Conclusions
Constipation (as a chief complaint) and bloating (as a symptom) were associated with fecal loading on X-ray imaging, while accidental bowel leakage and diarrhea were not.

Similar content being viewed by others
References
Saito YA, Schoenfield P, Locke GR 3rd. The epidemiology of irritable bowel syndrome in North America: a systematic review. Am J Gastroenterol. 2002;97:1910–1915.
Belsey J, Greenfield S, Candy D, et al. Systematic review: impact of constipation on quality of life in adults and children. Aliment Pharmacol Ther. 2010;31:938–949.
Camilleri M, Ford AC, Mawe GM, et al. Chronic constipation. Nat Rev Dis Primers. 2017;3:17095. https://doi.org/10.1038/nrdp.2017.95.
Zimmerman J, Hershcovici T. Bowel symptoms in nonerosive gastroesophageal reflux disease: nature, prevalence, and relation to acid reflux. J Clin Gastroenterol. 2008;42:261–265.
Nellesen D, Chawla A, Oh DL, et al. Comorbidities in patients with irritable bowel syndrome with constipation or chronic idiopathic constipation: a review of the literature from the past decade. Postgrad Med. 2013;125:40–50.
Fond G, Loundou A, Hamdani N, et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. 2014;264:651–660.
Rao SS, Seaton K, Miller MJ, et al. Psychological profiles and quality of life differ between patients with dyssynergia and those with slow transit constipation. J Psychosom Res. 2007;63:441–449.
Choi YJ, Seo BS, Lee JH, et al. Treatment of fecal retention is important in the management of overactive bladder in children. Neurourol Urodyn. 2017;36:490–494.
Sampaio C, Sousa AS, Fraga LGA, et al. Constipation and lower urinary tract dysfunction in children and adolescents: a population-based study. Front Pediatr. 2016;4:1–6.
Spence-Jones C, Kamm MA, Henry MM, et al. Bowel dysfunction: a pathogenic factor in uterovaginal prolapse and urinary stress incontinence. Br J Obstet Gynaecol. 1994;101:147–152.
Ng SC, Chen YC, Lin LY, et al. Anorectal dysfunction in women with urinary incontinence or lower urinary tract symptoms. Int J Gynaecol Obstet. 2002;77:139–145.
Kaplan SA, Dmochowski R, Cash BD, et al. Systematic review of the relationship between bladder and bowel function: implications for patient management. Int J Clin Pract. 2013;67:205–216.
Soligo M, Salvatore S, Emmanuel AV, et al. Patterns of constipation in urogynecology: clinical importance and pathophysiologic insights. Am J Obstet Gynecol. 2006;195:50–55.
Leech SC, McHugh K, Sullivan PB. Evaluation of a method of assessing faecal loading on plain abdominal radiographs in children. Pediatr Radiol. 1999;29:255–258.
Barr RG, Levine MD, Wilkinson RH, et al. Chronic and occult stool retention: a clinical tool for its evaluation in school-aged children. Clin Pediatr. 1979;18:674–679.
Blethyn AJ, Verrier Jones K, Newcombe R, et al. Radiological assessment of constipation. Arch Dis Child. 1995;73:532–533.
Pensabene L, Buonomo C, Fishman L, et al. Lack of utility of abdominal X-rays in the evaluation of children with constipation: a comparison of different scoring methods. J Pediatr Gastroenterol Nutr. 2010;51:155–159.
Bongers ME, Voskuijl WP, van Rijn RR, et al. The value of the abdominal radiograph in children with functional gastrointestinal disorders. Eur J Radiol. 2006;59:8–13.
Reuchlin-Vroklage LM, Bierma-Zeinstra S, Benninga MA, et al. Diagnostic value of abdominal radiography in constipated children: a systematic review. Arch Pediatr Adolesc Med. 2005;159:671–678.
Smith RG, Lewis S. The relationship between digital rectal examination and abdominal radiographs in elderly patients. Age Ageing. 1990;19:142–143.
Petroianu A, Alberti LR. Accuracy of the new radiographic sign of fecal loading in the cecum for differential diagnosis of acute appendicitis in comparison with other inflammatory diseases of right abdomen: a prospective study. J Med Life. 2012;5:85–91.
Petroianu A, Alberti LR, Zac RI. Assessment of the persistence of fecal loading in the cecum in presence of acute appendicitis. Int J Surg. 2007;5:11–16.
Khan O, Shankar PR, Parikh AD, et al. Radiographic stool quantification: an equivalence study of 484 symptomatic and asymptomatic subjects. Abdom Radiol. 2018;. https://doi.org/10.1007/s00261-018-1869-5.
Clark K, Lam LT, Talley NJ, et al. Assessing the presence and severity of constipation with plain radiographs in constipated palliative care patients. J Palliat Med. 2016;19:617–621.
Moayyedi P. The epidemiology of obesity and gastrointestinal and other diseases: an overview. Dig Dis Sci. 2008;53:2293–2299.
Camilleri M, Malhi H, Acosta A. Gastrointestinal complications of obesity. Gastroenterology. 2017;152:1656–1670.
Talley N, Quan C, Jones M, et al. Association of upper and lower gastrointestinal tract symptoms with body mass index in an Australian cohort. Neurogastroenterol Motil. 2004;16:413–419.
Talley N, Howell S, Poulton R. Obesity and chronic gastrointestinal tract symptoms in young adults: a birth cohort study. Am J Gastroenterol. 2004;99:1807–1814.
Delgado-Aros S, Locke GR III, Camilleri M, et al. Obesity is associated with increased risk of gastrointestinal symptoms: a population-based study. Am J Gastroenterol. 2004;99:1801–1806.
Eslick GD, Talley NJ. Prevalence and relationship between gastrointestinal symptoms among individuals of different body mass index: a population-based study. Obes Res Clin Pract. 2016;10:143–150.
Reber J, McGauvran A, Froemming A. Abdominal radiograph usage trends in the setting of constipation: a 10-year experience. Abdom Radiol. 2018;43:2231–2238.
Moylan S, Armstrong J, Diaz-Saldano D, et al. Are abdominal X-rays a reliable way to assess for constipation? J Urol. 2010;184:1692–1698.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pleasant, V., Sammarco, A., Keeney-Bonthrone, G. et al. Use of X-ray to Assess Fecal Loading in Patients with Gastrointestinal Symptoms. Dig Dis Sci 64, 3589–3595 (2019). https://doi.org/10.1007/s10620-019-05770-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05770-9