Abstract
Purpose
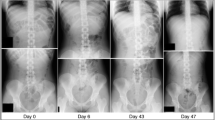
Stool burden on abdominal radiographs is not reflective of constipation, perhaps because of variable fecal shadowing or limited inter-rater agreement. These limitations are hypothetically mitigated by computed tomography (CT). This research aimed (i) to evaluate whether bowel movement frequency, stool form, or a diagnosis of functional constipation correlate or associate with stool burden identified on CT, and (ii) to investigate whether physicians use CT in their assessment of a patients’ bowel function.
Methods
Patients attending for non-emergent abdominal CT imaging were invited to participate by completing a bowel questionnaire. Stool burden identified on imaging was determined and inter-rater reliability was evaluated in a subgroup of patients (n = 20). Descriptive and comparative analyses were performed. An online questionnaire evaluated the use of abdominal imaging in assessing patients’ bowel function in a cross-section of ordering physicians.
Results
The patient response rate was 19% (96/516). No clinically useful associations between fecal burden and stool form, bowel motion frequency, gastrointestinal symptoms or a diagnosis of constipation was identified. The physician response rate was 35% (33/94). Opportunistic use of data was more common than deliberate use. However, an abdominal radiograph or CT scan had been requested by 42% and 18% of physicians respectively to assess patient’s chronic bowel habit. Approximately 30% of physicians believed evidence supported this practice.
Conclusions
Physicians may use abdominal CT in their assessment of patients’ chronic bowel habits. However, objective assessment does not support this practice. Colonic stool burden does not correlate with patient-reported symptoms or a criteria-based diagnosis of constipation.




Similar content being viewed by others
Abbreviations
- CT:
-
Computed tomography
- CSI:
-
Cross-sectional imaging
References
Longstreth, G.F., et al., Functional bowel disorders. Gastroenterology, 2006. 130(5): p. 1480-91.
Lacy, B.E., et al., Bowel Disorders. Gastroenterology, 2016. 150(6): p. 1393-1407.e5.
Dimidi, E., et al., Perceptions of Constipation Among the General Public and People With Constipation Differ Strikingly From Those of General and Specialist Doctors and the Rome IV Criteria. Am J Gastroenterol, 2019. 114(7): p. 1116-1129.
Bellini, M., et al., Different perception of chronic constipation between patients and gastroenterologists. Neurogastroenterol Motil, 2018: p. e13336.
Bharucha, A.E., J.H. Pemberton, and G.R. Locke, 3rd, American Gastroenterological Association technical review on constipation. Gastroenterology, 2013. 144(1): p. 218-38.
Bewley, A., M.J. Clancy, and J.R. Hall, The erroneous use by an accident and emergency department of plain abdominal radiographs in the diagnosis of constipation. Arch Emerg Med, 1989. 6(4): p. 257-8.
Kearney, R., et al., Emergency Provider Use of Plain Radiographs in the Evaluation of Pediatric Constipation. Pediatr Emerg Care, 2019. 35(9): p. 624-629.
Driver, B.E., et al., Utility of plain abdominal radiography in adult ED patients with suspected constipation. Am J Emerg Med, 2019: p. 158377.
de Lorijn, F., et al., The Leech method for diagnosing constipation: intra- and interobserver variability and accuracy. Pediatr Radiol, 2006. 36(1): p. 43-9.
Freedman, S.B., et al., Pediatric Abdominal Radiograph Use, Constipation, and Significant Misdiagnoses. The Journal of Pediatrics, 2014. 164(1): p. 83-88.e2.
Reuchlin-Vroklage, L.M., et al., Diagnostic value of abdominal radiography in constipated children: A systematic review. Archives of Pediatrics & Adolescent Medicine, 2005. 159(7): p. 671-678.
Benninga, M.A., et al., Defaecation disorders in children, colonic transit time versus the Barr-score. Eur J Pediatr, 1995. 154(4): p. 277-84.
Benninga, M.A., M.M. Tabbers, and R.R. van Rijn, How to use a plain abdominal radiograph in children with functional defecation disorders. Archives of disease in childhood - Education & practice edition, 2016. 101(4): p. 187.
Bosch, M., et al., Systematic assessment of constipation on plain abdominal radiographs in children. Pediatric Radiology, 2006. 36(3): p. 224-226.
Cowlam, S., et al., Blinded comparison of faecal loading on plain radiography versus radio-opaque marker transit studies in the assessment of constipation. Clinical Radiology, 2008. 63(12): p. 1326-1331.
Harari, D. and K.L. Minaker, Megacolon in patients with chronic spinal cord injury. Spinal Cord, 2000. 38(6): p. 331.
De Looze, D., et al., Constipation and other chronic gastrointestinal problems in spinal cord injury patients. Spinal Cord, 1998. 36(1): p. 63.
Clark, K., et al., A pragmatic comparative study of palliative care clinician's reports of the degree of shadowing visible on plain abdominal radiographs. Support Care Cancer, 2018. 26(11): p. 3749-3754.
Berger, M.Y., et al., Value of Abdominal Radiography, Colonic Transit Time, and Rectal Ultrasound Scanning in the Diagnosis of Idiopathic Constipation in Children: A Systematic Review. The Journal of Pediatrics, 2012. 161(1): p. 44-50.e2.
Clark, K. and D.C. Currow, Plain Abdominal Radiographs to Diagnose Constipation Patients with Advanced Progressive Illness? Journal of Pain and Symptom Management, 2011. 41(4): p. e2-e3.
Pensabene, L., et al., Lack of utility of abdominal x-rays in the evaluation of children with constipation: comparison of different scoring methods. J Pediatr Gastroenterol Nutr, 2010. 51(2): p. 155-9.
van den Bosch, M., et al., Systematic assessment of constipation on plain abdominal radiographs in children. Pediatr Radiol, 2006. 36(3): p. 224-6.
Blethyn, A.J., et al., Radiological assessment of constipation. Arch Dis Child, 1995. 73(6): p. 532-3.
Leech, S.C., K. McHugh, and P.B. Sullivan, Evaluation of a method of assessing faecal loading on plain abdominal radiographs in children. Pediatr Radiol, 1999. 29(4): p. 255-8.
Starreveld, J.S., et al., The plain abdominal radiograph in the assessment of constipation. Z Gastroenterol, 1990. 28(7): p. 335-8.
Barr, R.G., et al., Chronic and occult stool retention: a clinical tool for its evaluation in school-aged children. Clin Pediatr (Phila), 1979. 18(11): p. 674, 676, 677–9, passim.
Chen, S.-Y., Z. Feng, and X. Yi, A general introduction to adjustment for multiple comparisons. Journal of thoracic disease, 2017. 9(6): p. 1725-1729.
O'Donnell, L.J., J. Virjee, and K.W. Heaton, Detection of pseudodiarrhoea by simple clinical assessment of intestinal transit rate. Bmj, 1990. 300(6722): p. 439-40.
Librach, S.L., et al., Consensus Recommendations for the Management of Constipation in Patients with Advanced, Progressive Illness. Journal of Pain and Symptom Management, 2010. 40(5): p. 761-773.
Cangemi, D.J., et al., Colonic Stool Burden a Useful Surrogate for Slow Transit Constipation as Determined by a Radiopaque Transit Study. Am J Gastroenterol, 2019. 114(3): p. 519-523.
Burkitt, D.P., A.R. Walker, and N.S. Painter, Effect of dietary fibre on stools and the transit-times, and its role in the causation of disease. Lancet, 1972. 2(7792): p. 1408-12.
Bendezu, R.A., et al., Colonic content: effect of diet, meals, and defecation. Neurogastroenterol Motil, 2017. 29(2).
Lam, C., et al., Colonic response to laxative ingestion as assessed by MRI differs in constipated irritable bowel syndrome compared to functional constipation. Neurogastroenterol Motil, 2016. 28(6): p. 861-70.
Boccia, G., et al., Dyspeptic symptoms in children: the result of a constipation-induced cologastric brake? Clin Gastroenterol Hepatol, 2008. 6(5): p. 556-60.
Jiang, X., et al., Prevalence and risk factors for abdominal bloating and visible distention: a population-based study. Gut, 2008. 57(6): p. 756-63.
Vijayvargiya, P., et al., Novel association of rectal evacuation disorder and rumination syndrome: Diagnosis, comorbidities, and treatment. United European Gastroenterology Journal, 2014. 2(1): p. 38-46.
Park, S.Y., et al., Rectal gas volume: Defining cut-offs for screening for evacuation disorders in patients with constipation. Neurogastroenterol Motil, 2017. 29(7).
Park, S.Y., et al., Rectal Gas Volume Measured by Computerized Tomography Identifies Evacuation Disorders in Patients With Constipation. Clin Gastroenterol Hepatol, 2017. 15(4): p. 543-552.e4.
Altman, D.G. and P. Royston, The cost of dichotomising continuous variables. Bmj, 2006. 332(7549): p. 1080.
Del Priore, G., P. Zandieh, and M.-J. Lee, Treatment of continuous data as categoric variables in obstetrics and gynecology. Obstetrics & Gynecology, 1997. 89(3): p. 351-354.
Naggara, O., et al., Analysis by categorizing or dichotomizing continuous variables is inadvisable: an example from the natural history of unruptured aneurysms. AJNR Am J Neuroradiol, 2011. 32(3): p. 437-40.
Lee, C.I., et al., Diagnostic CT Scans: Assessment of Patient, Physician, and Radiologist Awareness of Radiation Dose and Possible Risks. Radiology, 2004. 231(2): p. 393-398.
Choung, R.S., et al., A low response rate does not necessarily indicate non-response bias in gastroenterology survey research: a population-based study. Journal of Public Health, 2013. 21(1): p. 87-95.
Stastics Canada. Linguistic Characteristics of Canadians. 2011 [cited 2020 January 7th]; Available from: https://www12.statcan.gc.ca/census-recensement/2011/as-sa/98-314-x/98-314-x2011001-eng.cfm.
Ghoshal, U.C., et al., Development, Translation and Validation of Enhanced Asian Rome III Questionnaires for Diagnosis of Functional Bowel Diseases in Major Asian Languages: A Rome Foundation-Asian Neurogastroenterology and Motility Association Working Team Report. Journal of neurogastroenterology and motility, 2015. 21(1): p. 83-92.
Suares, N.C. and A.C. Ford, Prevalence of, and Risk Factors for, Chronic Idiopathic Constipation in the Community: Systematic Review and Meta-analysis. American Journal of Gastroenterology, 2011. 106(9): p. 1582-1591.
Funding
None.
Author information
Authors and Affiliations
Contributions
DF: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualization; Roles/Writing—original draft. DH: Investigation, Formal analysis, Writing—review & editing. RS: Investigation, Writing—review & editing. MA: Investigation, Writing—review & editing. JB: Conceptualization, Methodology, Formal Analysis, Writing—review & editing. FD: Conceptualization, Formal Analysis, Writing—review & editing. DOP: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualization; Roles/Writing—original draft, Supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Ethical approval for this study was granted by the University of British Colombia Research Ethics Board (H14-02754).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ferguson, D., Holmes, R.D., Scott, R. et al. Colonic stool burden on computed tomography does not correlate with bowel habit: a cross-sectional study. Abdom Radiol 46, 506–516 (2021). https://doi.org/10.1007/s00261-020-02689-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02689-y