Abstract
Background and Aims
To facilitate access for interventional EUS, flexible (nitinol) 19-G needles have been introduced to permit needle puncture even when the echoendoscope is in an angulated position, such as in the second part of the duodenum. The aims of the study were to evaluate the performance of a flexible 19-G needle during interventional EUS procedures and compare outcomes when the echoendoscope was in the straight versus angulated position.
Methods
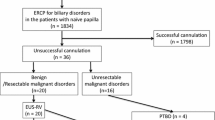
A retrospective review was undertaken of 162 consecutive patients that underwent a variety of interventional EUS procedures with a flexible 19-G needle across five centers. Patients were subdivided into categories (straight or angulated) depending on the echoendoscope position used for obtaining access to the area of interest (Fig. 1).

Flexible 19-G needle design. a The needle is able to exit the sheath despite the rotated position. b The needle beveled needle tip
Results
In the entire cohort, needle-specific technical success was achieved in 93.2 %, procedural success in 85.2 %, and overall clinical success in 76.5 % of cases at a mean follow-up of 3.1 months. Needle-specific technical success was similar between the straight and angulated cohorts (94.0 vs. 91.2 %, p = 0.74). Procedural success (86.7 vs. 77.2 %, p = 0.05), and rate of clinical success was similar between the cohorts (83.3 vs. 86.4 %, p = 0.79), respectively. Overall adverse events were noted in 14.2 % of patients with no difference between the straight and angulated cohorts (p = 0.48).
Conclusions
This study demonstrates equivalent technical success, clinical success and safety of using a flexible 19-G needle in straight and angulated endoscope positions for interventional EUS. Therefore, a flexible needle may be considered where an angulated echoendoscope position is encountered.
Similar content being viewed by others
References
Varadarajulu S, Bang JY, Sutton BS, et al. Equal efficacy of endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage in a randomized trial. Gastroenterology. 2013;145:583–590.
Ishiwatari H, Hayashi T, Yoshida M, et al. EUS-guided celiac plexus neurolysis by using highly viscous phenol-glycerol as a neurolytic agent (with video). Gastrointest Endosc. 2015;81:479–483.
Doi S, Yasuda I, Kawakami H, et al. Endoscopic ultrasound guided celiac ganglia neurolysis vs. celiac plexus neurolysis: a randomized multicenter trial. Endoscopy 2013;45:362–369.
LeBlanc JK, Al-Haddad M, McHenry L, et al. A prospective, randomized study of EUS-guided celiac plexus neurolysis for pancreatic cancer: one injection or two? Gastrointest Endosc. 2011;74:1300–1307.
Musumba C, Tutticci N, Nanda K, et al. Endosonography-guided drainage of malignant fluid collections using lumen-apposing, fully covered self-expanding metal stents. Endoscopy. 2014;46:690–692.
Kahaleh M, Artifon E, Perez-Miranda M, et al. Endoscopic ultrasonography guided drainage: Summary of consortium meeting, May 21, 2012, San Diego, California. World J Gastroenterol. 2015;21:726–741.
Khashab MA, Dewitt J. EUS-guided biliary drainage: is it ready for prime time? Yes! Gastrointest Endosc. 2013;78:102–105.
Choi JH, Lee SS. Endoscopic ultrasonography-guided gallbladder drainage for acute cholecystitis: from evidence to practice. Dig Endosc. 2015;27:1–7.
Itoi T, Sofuni A, Tsuchiya T, et al. Initial evaluation of a new plastic pancreatic duct stent for endoscopic ultrasonography-guided placement. Endoscopy. 2015;47:462–465.
Holt B, Varadarajulu S. Endoscopic ultrasound-guided pelvic abscess drainage (with video). J Hepatobiliary Pancreat Sci. 2015;22:12–15.
Khashab MA, Valeshabad AK, Afghani E, et al. A comparative evaluation of EUS-guided biliary drainage and percutaneous drainage in patients with distal malignant biliary obstruction and failed ERCP. Dig Dis Sci. 2015;60:557–565.
Artifon EL, Aparicio D, Paione JB, et al. Biliary drainage in patients with unresectable, malignant obstruction where ERCP fails: endoscopic ultrasonography-guided choledochoduodenostomy versus percutaneous drainage. J Clin Gastroenterol. 2012;46:768–774.
Romero-Castro R, Ellrichmann M, Ortiz-Moyano C, et al. EUS-guided coil versus cyanoacrylate therapy for the treatment of gastric varices: a multicenter study (with videos). Gastrointest Endosc. 2013;78:711–721.
Storm AC, Kumbhari V, Saxena P, et al. EUS-guided angiotherapy. Gastrointest Endosc. 2014;80:164–165.
Katanuma A, Itoi T, Baron TH, et al. Bench-top testing of suction forces generated through endoscopic ultrasound-guided aspiration needles. J Hepatobiliary Pancreat Sci. 2015;22:379–385.
Varadarajulu S, Bang JY, Hebert-Magee S. Assessment of the technical performance of the flexible 19-gauge EUS-FNA needle. Gastrointest Endosc. 2012;76:336–343.
Ramesh J, Bang JY, Hebert-Magee S, et al. Randomized trial comparing the flexible 19G and 25G needles for endoscopic ultrasound-guided fine needle aspiration of solid pancreatic mass lesions. Pancreas. 2015;44:128–133.
Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71:446–454.
Tyberg A, Karia K, Zerbo S, et al. Endoscopic ultrasonography-guided jejunojejunostomy to facilitate endoscopic retrograde cholangiopancreatography: a minimally invasive option. Gastroenterology. 2015;148:506–507.
Ogura T, Sano T, Onda S, et al. Endoscopic ultrasound-guided biliary drainage for right hepatic bile duct obstruction: novel technical tips. Endoscopy. 2015;47:72–75.
Song TJ, Kim JH, Lee SS, et al. The prospective randomized, controlled trial of endoscopic ultrasound-guided fine-needle aspiration using 22G and 19G aspiration needles for solid pancreatic or peripancreatic masses. Am J Gastroenterol. 2010;105:1739–1745.
Bang JY, Ramesh J, Trevino J, et al. Objective assessment of an algorithmic approach to EUS-guided FNA and interventions. Gastrointest Endosc. 2013;77:739–744.
Chavalitdhamrong D, Draganov PV. Performance characteristics of a new flexible nitinol 19-gauge endoscopic ultrasound-guided fine needle aspiration needle. Gut Liver. 2013;7:756.
Park do H, Jeong SU, Lee BU, et al. Prospective evaluation of a treatment algorithm with enhanced guidewire manipulation protocol for EUS-guided biliary drainage after failed ERCP (with video). Gastrointest Endosc. 2013;78:91–101.
Artifon EL, Marson FP, Gaidhane M, et al. Hepaticogastrostomy or choledochoduodenostomy for distal malignant biliary obstruction after failed ERCP: is there any difference? Gastrointest Endosc. 2015;81:950–959.
Varadarajulu S, Bang JY, Phadnis MA, et al. Endoscopic transmural drainage of peripancreatic fluid collections: outcomes and predictors of treatment success in 211 consecutive patients. J Gastrointest Surg. 2011;15:2080–2088.
Varadarajulu S, Christein JD, Wilcox CM. Frequency of complications during EUS-guided drainage of pancreatic fluid collections in 148 consecutive patients. J Gastroenterol Hepatol. 2011;26:1504–1508.
Author contributions
Vivek Kumbhari and Mouen A. Khashab developed the concept, wrote, and edited the final manuscript. All other authors were involved in data acquisition and editing and final approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jonathan M. Bucaglia is a consultant for Boston Scientific. Payal Saxena is a consultant for Boston Scientific and has received consulting fees from Olympus Australia, Cook Medical, Pentax Medical and research support from Cook Medical. Mouen A. Khashab is a consultant for Boston Scientific and Olympus America and has received research support from Cook Medical. All other authors have no relevant disclosures.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kumbhari, V., Peñas, I., Tieu, A.H. et al. Interventional EUS Using a Flexible 19-Gauge Needle: An International Multicenter Experience in 162 Patients. Dig Dis Sci 61, 3552–3559 (2016). https://doi.org/10.1007/s10620-016-4327-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-016-4327-7