Abstract
Background
Sleep disruption is common in inflammatory bowel diseases (IBD). However, studies demonstrating a similar prevalence in irritable bowel syndrome suggest that nighttime disruption due to diarrhea and abdominal pain may be key drivers of poor sleep quality. Whether inflammation is associated with poor sleep independently has not been examined previously.
Methods
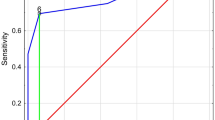
This single-center study included subjects with IBD recruited to an ongoing prospective registry who completed a questionnaire assessing sleep quality and mood. Inflammatory marker levels [C-reactive protein (CRP), erythrocyte sedimentation rate] and clinical disease activity including nighttime disruption on the day of enrollment were obtained from the medical record. Logistic regression models were used to identify predictors of sleep quality.
Results
The study included 131 subjects (72 women) with a median age of IBD diagnosis of 25 years. Twenty-three subjects (19 %) had a high C-reactive protein level (≥8 mg/dL). Poor sleep was more common in those with high CRP levels than with normal values (70 vs. 39 %, p = 0.009). This association remained significant on multivariate analysis [Odds ratio (OR) 4.12, 95 % confidence interval (CI) 1.38–12.29]. Adjusting for the presence of nighttime disruption did not significant alter this association (OR 3.16, 95 % CI 1.01–9.90). High CRP correlated with poor sleep even in patients not experiencing nocturnal symptoms (n = 101, OR 4.89, 95 % CI 1.24–19.36).
Conclusion
High CRP is associated with poor sleep quality in IBD independent of the presence of nighttime disruptions, suggesting that a relationship exists between circulating inflammatory markers and sleep.
Similar content being viewed by others
References
Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361:2066–2078.
Bernstein CN, Loftus EV Jr, Ng SC, et al. Hospitalisations and surgery in Crohn’s disease. Gut. 2012;61:622–629.
Ghosh S, Mitchell R. Impact of inflammatory bowel disease on quality of life: results of the European Federation of Crohn’s and Ulcerative Colitis Associations (EFCCA) patient survey. J Crohns Colitis. 2007;1:10–20.
Ananthakrishnan AN, Weber LR, Knox JF, et al. Permanent work disability in Crohn’s disease. Am J Gastroenterol. 2008;103:154–161.
Jostins L, Ripke S, Weersma RK, et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature. 2012;491:119–124.
Cosnes J, Gower-Rousseau C, Seksik P, et al. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011;140:1785–1794.
Danese S, Fiocchi C. Etiopathogenesis of inflammatory bowel diseases. World J Gastroenterol. 2006;12:4807–4812.
Ananthakrishnan AN. Environmental risk factors for inflammatory bowel diseases: a review. Dig Dis Sci. 2015;60:290–298.
Ananthakrishnan AN, Khalili H, Pan A, et al. Association between depressive symptoms and incidence of Crohn’s disease and ulcerative colitis: results from the Nurses’ Health Study. Clin Gastroenterol Hepatol. 2013;11:57–62.
Ananthakrishnan AN, Long MD, Martin CF, et al. Sleep disturbance and risk of active disease in patients with Crohn’s disease and ulcerative colitis. Clin Gastroenterol Hepatol. 2013;11:965–971.
Bernstein CN, Singh S, Graff LA, et al. A prospective population-based study of triggers of symptomatic flares in IBD. Am J Gastroenterol. 2010;105:1994–2002.
Bitton A, Dobkin PL, Edwardes MD, et al. Predicting relapse in Crohn’s disease: a biopsychosocial model. Gut. 2008;57:1386–1392.
Graff LA, Vincent N, Walker JR, et al. A population-based study of fatigue and sleep difficulties in inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:1882–1889.
Singh S, Graff LA, Bernstein CN. Do NSAIDs, antibiotics, infections, or stress trigger flares in IBD? Am J Gastroenterol. 2009;104:1298–1313. (quiz 1314).
Abad VC, Sarinas PS, Guilleminault C. Sleep and rheumatologic disorders. Sleep Med Rev. 2008;12:211–228.
Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–209.
Brass SD, Duquette P, Proulx-Therrien J, et al. Sleep disorders in patients with multiple sclerosis. Sleep Med Rev. 2010;14:121–129.
Cappuccio FP, Cooper D, D’Elia L, et al. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32:1484–1492.
Cappuccio FP, D’Elia L, Strazzullo P, et al. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–592.
Chandrasekhara PK, Jayachandran NV, Rajasekhar L, et al. The prevalence and associations of sleep disturbances in patients with systemic lupus erythematosus. Mod Rheumatol. 2009;19:407–415.
Keefer L, Stepanski EJ, Ranjbaran Z, et al. An initial report of sleep disturbance in inactive inflammatory bowel disease. J Clin Sleep Med. 2006;2:409–416.
Ranjbaran Z, Keefer L, Farhadi A, et al. Impact of sleep disturbances in inflammatory bowel disease. J Gastroenterol Hepatol. 2007;22:1748–1753.
Ranjbaran Z, Keefer L, Stepanski E, et al. The relevance of sleep abnormalities to chronic inflammatory conditions. Inflamm Res. 2007;56:51–57.
Abedelmalek S, Souissi N, Chtourou H, et al. Effects of partial sleep deprivation on proinflammatory cytokines, growth hormone, and steroid hormone concentrations during repeated brief sprint interval exercise. Chronobiol Int. 2013;30:502–509.
Ali T, Madhoun MF, Orr WC, et al. Assessment of the relationship between quality of sleep and disease activity in inflammatory bowel disease patients. Inflamm Bowel Dis. 2013;19:2440–2443.
Axelsson J, Rehman JU, Akerstedt T, et al. Effects of sustained sleep restriction on mitogen-stimulated cytokines, chemokines and T helper 1/T helper 2 balance in humans. PLoS One. 2013;8:e82291.
Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007;3:519–528.
Fragiadaki K, Tektonidou MG, Konsta M, et al. Sleep disturbances and interleukin 6 receptor inhibition in rheumatoid arthritis. J Rheumatol. 2012;39:60–62.
Rohleder N, Aringer M, Boentert M. Role of interleukin-6 in stress, sleep, and fatigue. Ann N Y Acad Sci. 2012;1261:88–96.
Buysse DJ, Yu L, Moul DE, et al. Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep. 2010;33:781–792.
Yu L, Buysse DJ, Germain A, et al. Development of short forms from the PROMIS sleep disturbance and Sleep-Related Impairment item banks. Behav Sleep Med. 2012;10:6–24.
Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005;19:5–36.
Patel SR, Zhu X, Storfer-Isser A, et al. Sleep duration and biomarkers of inflammation. Sleep. 2009;32:200–204.
Shoham S, Davenne D, Cady AB, et al. Recombinant tumor necrosis factor and interleukin 1 enhance slow-wave sleep. Am J Physiol. 1987;253:R142–R149.
Ananthakrishnan AN, Khalili H, Konijeti GG, et al. Sleep duration affects risk for ulcerative colitis: a prospective cohort study. Clin Gastroenterol Hepatol. 2014;12:1879–1886.
Parekh PJ, Oldfield Iv EC, Challapallisri V, et al. Sleep disorders and inflammatory disease activity: chicken or the egg? Am J Gastroenterol. 2014. doi:10.1038/ajg.2014.247.
Simpson N, Dinges DF. Sleep and inflammation. Nutr Rev. 2007;65:S244–S252.
Swanson GR, Burgess HJ, Keshavarzian A. Sleep disturbances and inflammatory bowel disease: a potential trigger for disease flare? Expert Rev Clin Immunol. 2011;7:29–36.
Tang Y, Preuss F, Turek FW, et al. Sleep deprivation worsens inflammation and delays recovery in a mouse model of colitis. Sleep Med. 2009;10:597–603.
Swanson G, Forsyth CB, Tang Y, et al. Role of intestinal circadian genes in alcohol-induced gut leakiness. Alcohol Clin Exp Res. 2012;35:1305–1314.
Ruperto N, Lovell DJ, Li T, et al. Abatacept improves health-related quality of life, pain, sleep quality, and daily participation in subjects with juvenile idiopathic arthritis. Arthritis Care Res (Hoboken). 2010;62:1542–1551.
Ali T, Choe J, Awab A, et al. Sleep, immunity and inflammation in gastrointestinal disorders. World J Gastroenterol. 2013;19:9231–9239.
Tobaldini E, Cogliati C, Fiorelli EM, et al. One night on-call: sleep deprivation affects cardiac autonomic control and inflammation in physicians. Eur J Intern Med. 2013;24:664–670.
Trammell RA, Verhulst S, Toth LA. Effects of sleep fragmentation on sleep and markers of inflammation in mice. Comp Med. 2014;64:13–24.
Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–19.
Graff LA, Walker JR, Bernstein CN. Depression and anxiety in inflammatory bowel disease: a review of comorbidity and management. Inflamm Bowel Dis. 2009;15:1105–1118.
Sutton EL. Psychiatric disorders and sleep issues. Med Clin North Am. 2014;98:1123–1143.
Acknowledgments
We acknowledge the valuable contributions of the participants and the research staff of our registry. This work was presented as a poster at the American College of Gastroenterology Annual Meeting 2014, Philadelphia, PA. This work is supported by the National Institutes of Health (NIH) (P30 DK043351) to the Center for Study of Inflammatory Bowel Diseases. Ananthakrishnan is supported in part by a grant from the National Institutes of Health (K23 DK097142).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendix: Assessment of Sleep and Mood Using the NIH PROMIS Questions
Appendix: Assessment of Sleep and Mood Using the NIH PROMIS Questions
Sleep Habits

Mood


Rights and permissions
About this article
Cite this article
Wilson, R.G., Stevens, B.W., Guo, A.Y. et al. High C-Reactive Protein Is Associated with Poor Sleep Quality Independent of Nocturnal Symptoms in Patients with Inflammatory Bowel Disease. Dig Dis Sci 60, 2136–2143 (2015). https://doi.org/10.1007/s10620-015-3580-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3580-5