Abstract
Background
Poor sleep is common in inflammatory bowel disease (IBD), predicting increased risk of flares, surgery, and/or hospitalization and reducing quality of life.
Aims
To profile specific sleep disorder symptoms in IBD, informing intervention efforts.
Methods
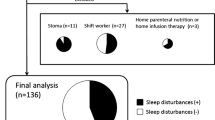
312 adults with Crohn’s disease or ulcerative colitis were recruited from an academic medical center in New Hampshire, USA. Participants completed online surveys about sleep including well-validated measures of sleep quality, insomnia, restless leg syndrome, sleep apnea, and circadian rhythms. Participants also answered questions about IBD-related problems that could interfere with sleep.
Results
69.4% of participants reported experiencing poor sleep and 50% reported clinically significant insomnia. Participants with active IBD symptoms were more likely to have poor sleep and insomnia. Of those with poor sleep, 67.8% met the clinical threshold for insomnia disorder and 31.3% met criteria for two or more sleep disorders. IBD-related sleep disruptions (e.g., nighttime awakenings due to bowel movements) were not significantly related to poor sleep quality, but significantly related to insomnia severity for participants with active Crohn’s disease.
Conclusions
While poor sleep in IBD is reflective of a number of different sleep problems, it is most frequently related to insomnia. IBD symptom severity contributes to insomnia, but insomnia is also distinct from IBD-related sleep disruptions. Future research on the treatment of insomnia disorder in particular in individuals with IBD is warranted.

Similar content being viewed by others
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Ananthakrishnan AN, Long MD, Martin CF, Sandler RS, Kappelman MD. Sleep disturbance and risk of active disease in patients with Crohn’s disease and ulcerative colitis. Clin Gastroenterol Hepatol. 2013;11:965–971.
Ali T, Madhoun MF, Orr WC, Rubin DT. Assessment of the relationship between quality of sleep and disease activity in inflammatory bowel disease patients. Inflam Bowel Dis. 2013;19:2440–2443.
Iskandar HN, Linan EE, Patel A, Moore R, Lasanajak Y, Gyawali CP et al. Self-reported sleep disturbance in Crohn’s disease is not confirmed by objective sleep measures. Sci Rep. 2020;10:1–9.
Sofia MA, Lipowska AM, Zmeter N, Perez E, Kavitt R, Rubin DT. Poor sleep quality in Crohn’s disease is associated with disease activity and risk for hospitalization or surgery. Inflam Bowel Dis. 2020;26:1251–1259.
Graff LA, Vincent N, Walker JR, Clara I, Carr R, Ediger J et al. A population-based study of fatigue and sleep difficulties in inflammatory bowel disease. Inflam Bowel Dis. 2010;17:1882–1889.
Keefer L, Stepanski EJ, Ranjbaran Z, Benson LM, Keshavarzian A. An initial report of sleep disturbance in inactive inflammatory bowel disease. J Clin Sleep Med. 2006;2:409–416.
Uemura R, Fujiwara Y, Iwakura N, Shiba M, Watanabe K, Kamata N et al. Sleep disturbances in Japanese patients with inflammatory bowel disease and their impact on disease flare. SpringerPlus. 2016;5:1792.
Gingold-Belfer R, Peled N, Levy S, Katz N, Niv Y, Fass R et al. Impaired sleep quality in Crohn’s disease depends on disease activity. Dig Dis Sci. 2014;59:146–151. https://doi.org/10.1007/s10620-013-2890-8.
Kappelman MD, Long MD, Martin C, DeWalt DA, Kinneer PM, Chen W et al. Evaluation of the patient-reported outcomes measurement information system in a large cohort of patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2014;12:1315–1323.
Ranjbaran Z, Keefer L, Farhadi A, Stepanski E, Sedghi S, Keshavarzian A. Impact of sleep disturbances in inflammatory bowel disease. J Gastroenterol Hepatol. 2007;22:1748–1753.
Scott AJ, Flowers O, Rowse G. A comparative study of the nature and magnitude of problems sleeping in inflammatory bowel disease (IBD) compared to healthy controls. Psychol Health Med. 2020;20:1–11.
Chrobak AA, Nowakowski J, Zwolińska-Wcisło M, Cibor D, Przybylska-Feluś M, Ochyra K et al. Associations between chronotype, sleep disturbances and seasonality with fatigue and inflammatory bowel disease symptoms. Chronobiol Int. 2018;35:1142–1152.
Becker J, Berger F, Schindlbeck KA, Poddubnyy D, Koch PM, Preiß JC et al. Restless legs syndrome is a relevant comorbidity in patients with inflammatory bowel disease. Int J Colorectal Dis. 2018;33:955–962.
Cohen ER, Melmed GY. Making a case for patient-reported outcomes in clinical inflammatory bowel disease practice. Clin Gastroenterol Hepatol. 2018;16:603–607.
Bewtra M, Brensinger CM, Tomov VT, Hoang TB, Sokach CE, Siegel CA et al. An optimized patient-reported ulcerative colitis disease activity measure derived from the Mayo score and the simple clinical colitis activity index. Inflam Bowel Dis. 2014;20:1070–1078.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psych Res. 1989;28:193–213.
Heslop P, Smith GD, Metcalfe C, Macleod J, Hart C. Sleep duration and mortality: the effect of short or long sleep duration on cardiovascular and all-cause mortality in working men and women. Sleep Med. 2002;3:305–314.
Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A et al. A prospective study of sleep duration and coronary heart disease in women. Arch Int Med. 2003;163:205–209. https://doi.org/10.1001/archinte.163.2.205.
Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E. Sleep loss: a novel risk factor for insulin resistance and Type 2 diabetes. J Appl Physiol. 2005;99:2008–2019. https://doi.org/10.1152/japplphysiol.00660.2005.
Allen RP, Burchell BJ, MacDonald B, Hening WA, Earley CJ. Validation of the self-completed Cambridge-Hopkins questionnaire (CH-RLSq) for ascertainment of restless legs syndrome (RLS) in a population survey. Sleep Med. 2009;10:1097–1100.
Allen RP, Picchietti DL, Garcia-Borreguero D, Ondo WG, Walters AS, Winkelman JW et al. Restless legs syndrome/Willis–Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria–history, rationale, description, and significance. Sleep Med. 2014;15:860–873.
Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. https://doi.org/10.1016/S1389-9457(00)00065-4.
Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–608.
Horne JA, Östberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;25:958–968.
Kantermann T, Sung H, Burgess HJ. Comparing the morningness-eveningness questionnaire and munich chronotype questionnaire to the dim light melatonin onset. J Biol Rhyt. 2015;30:449–453.
Chakradeo PS, Keshavarzian A, Singh S, Dera AE, Esteban JPG, Lee AA et al. Chronotype, social jet lag, sleep debt and food timing in inflammatory bowel disease. Sleep Med. 2018;52:188–195.
Taillard J, Philip P, Chastang J-F, Bioulac B. Validation of Horne and Ostberg morningness-eveningness questionnaire in a middle-aged population of French workers. J Biol Rhyt. 2004;19:76–86.
Paine S-J, Gander PH, Travier N. The epidemiology of morningness/eveningness: influence of age, gender, ethnicity, and socioeconomic factors in adults (30–49 years). J Biol Rhyt. 2006;21:68–76.
Ong JC, Huang JS, Kuo TF, Manber R. Characteristics of insomniacs with self-reported morning and evening chronotypes. J Clin Sleep Med. 2007;3:289–294.
Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S et al. Stop questionnairea tool to screen patients for obstructive sleep apnea. Anesthesiol J Am Soc Anesthesiol. 2008;108:812–821.
Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6:65–70.
Kim H-Y. Statistical notes for clinical researchers: assessing normal distribution (2) using skewness and kurtosis. Restor Dent Endod. 2013;38:52.
Sochal M, Małecka-Panas E, Gabryelska A, Talar-Wojnarowska R, Szmyd B, Krzywdzińska M et al. Determinants of sleep quality in inflammatory bowel diseases. J Clin Med. 2020;9:2921.
Singareddy R, Vgontzas AN, Fernandez-Mendoza J, Liao D, Calhoun S, Shaffer ML et al. Risk factors for incident chronic insomnia: a general population prospective study. Sleep Med. 2012;13:346–353.
Mai E, Buysse DJ. Insomnia: prevalence, impact, pathogenesis, differential diagnosis, and evaluation. Sleep Med Clin. 2008;3:167–174.
Scott AJ, Flowers O, Rowse G. Do specific types of sleep disturbances represent risk factors for poorer health‐related quality of life in inflammatory bowel disease? A longitudinal cohort study. Br J Health Psychol. 2020:e12457.
Ballou S, Alhassan E, Hon E, Lembo C, Rangan V, Singh P et al. Sleep disturbances are commonly reported among patients presenting to a gastroenterology clinic. Dig Dis Sci. 2018;63:2983–2991. https://doi.org/10.1007/s10620-018-5237-7.
Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Comorbidity of chronic insomnia with medical problems. Sleep. 2007;30:213–218.
Burish MJ, Chen Z, Yoo SH. Emerging relevance of circadian rhythms in headaches and neuropathic pain. Acta Physiol. 2019;225:e13161.
Hagenauer MH, Crodelle JA, Piltz SH, Toporikova N, Ferguson P, Booth V. The modulation of pain by circadian and sleep-dependent processes: a review of the experimental evidence. Women Math Biol. 2017; 1–21.
Kivelä L, Papadopoulos MR, Antypa N. Chronotype and psychiatric disorders. Curr Sleep Med Rep. 2018;4:94–103.
Koo BB. Restless leg syndrome across the globe: epidemiology of the restless legs syndrome/Willis-Ekbom disease. Sleep Med Clin. 2015;10:189–205.
Mosli MH, Bukhari LM, Khoja AA, Ashour NA, Aljahdali HR, Khoja OA et al. Inflammatory bowel disease and restless leg syndrome. Neurosci (Riyadh, S Arab). 2020;25:301–307.
Strange C, Richard CL, Shan S, Phillips BA, Kanotra S, Drummond MB et al. A population-based estimate of the health care burden of obstructive sleep apnea using a STOP-BAG questionnaire in South Carolina. J Clin Sleep Med. 2020
Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Basta M et al. Insomnia with short sleep duration and mortality: the Penn State cohort. Sleep. 2010;33:1159–1164.
Vgontzas AN, Fernandez-Mendoza J, Liao D, Bixler EO. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep Med Rev. 2013;17:241–254.
Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165:125–133.
Jacobs GD, Pace-Schott EF, Stickgold R, Otto MW. Cognitive behavior therapy and pharmacotherapy for insomnia: a randomized controlled trial and direct comparison. Arch Intern Med. 2004;164:1888–1896.
Smith MT, Perlis ML, Park A, Smith MS, Pennington J, Giles DE et al. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. Am J Psych. 2002;159:5–11.
Morin CM. Cognitive behavioral therapy for chronic insomnia: state of the science versus current clinical practices. Ann Intern Med. 2015;163:236–237.
Espie CA, Kyle SD, Williams C, Ong JC, Douglas NJ, Hames P et al. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. 2012;35:769–781.
Ritterband LM, Thorndike FP, Ingersoll KS, Lord HR, Gonder-Frederick L, Frederick C et al. Effect of a web-based cognitive behavior therapy for insomnia intervention with 1-year follow-up: a randomized clinical trial. JAMA Psych. 2017;74:68–75.
Salwen-Deremer JK, Siegel CA, Smith MT. Cognitive behavioral therapy for Insomnia: a promising treatment for insomnia, pain, and depression in patients with IBD. Crohn’s Colitis 360. 2020;2:otaa052.
Taylor DJ, Pruiksma KE. Cognitive and behavioural therapy for insomnia (CBT-I) in psychiatric populations: a systematic review. Int Rev Psych. 2014;26:205–213.
Zeng L-N, Zong Q-Q, Yang Y, Zhang L, Xiang Y-F, Ng CH et al. Gender difference in the prevalence of Insomnia: a meta-analysis of observational studies. Front Psych. 2020;11.
Johnson DA, Jackson CL, Williams NJ, Alcántara C. Are sleep patterns influenced by race/ethnicity–a marker of relative advantage or disadvantage? Evidence to date. Nat Sci Sleep. 2019;11:79.
Williet N, Sandborn WJ, Peyrin-Biroulet L. Patient-reported outcomes as primary end points in clinical trials of inflammatory bowel disease. Clin Gastroenterol Hepatol. 2014;12:1246–1256.
Zeitz J, Ak M, Müller-Mottet S, Scharl S, Biedermann L, Fournier N et al. Pain in IBD patients: very frequent and frequently insufficiently taken into account. PLoS ONE. 2016;11:e0156666.
Edwards RR, Almeida DM, Klick B, Haythornthwaite JA, Smith MT. Duration of sleep contributes to next-day pain report in the general population. PAIN. 2008;137:202–207.
Finan PH, Goodin BR, Smith MT. The association of sleep and pain: an update and a path forward. J Pain. 2013;14:1539–1552.
Afolalu EF, Ramlee F, Tang NK. Effects of sleep changes on pain-related health outcomes in the general population: a systematic review of longitudinal studies with exploratory meta-analysis. Sleep Med Rev. 2018;39:82–97.
Taylor DJ, Wilkerson AK, Pruiksma KE, Williams JM, Ruggero CJ, Hale W et al. Reliability of the structured clinical interview for DSM-5 sleep disorders module. J Clin Sleep Med. 2018;14:459–464.
Funding
This work was supported by internal funding from the Departments of Psychiatry and Medicine (section of Gastroenterology and Hepatology) at Dartmouth-Hitchcock/Geisel School of Medicine at Dartmouth.
Author information
Authors and Affiliations
Contributions
JSD designed the study with critical input from MTS and CAS, JSD, HGH, and CAS collected the data and JSD and CS analyzed the data. JSD developed the initial draft of the paper, and all authors critically revised the manuscript for important intellectual content. All authors approved the final version of this manuscript, including the authorship list. JSD is the Guarantor of the article.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Dartmouth-Hitchcock Institutional Review Board and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Individuals in this study agreed to a consent document prior to their participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Salwen-Deremer, J.K., Smith, M.T., Haskell, H.G. et al. Poor Sleep in Inflammatory Bowel Disease Is Reflective of Distinct Sleep Disorders. Dig Dis Sci 67, 3096–3107 (2022). https://doi.org/10.1007/s10620-021-07176-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-021-07176-y