Abstract
Background
Few studies have evaluated the prevention of upper gastrointestinal complications (UGIC; bleeding or perforation) in patients with uncomplicated peptic ulcer (PU). We assessed the effect of proton pump inhibitors (PPI) in a non-randomized setting. To maximize exchangeability of exposed and unexposed groups we restricted the study to patients with a new diagnosis of PU, i.e., a clear indication. To minimize selection bias we mimicked an intention to treat approach by assessing the effect of PPI prescription after PU diagnosis.
Methods
Within a population of subjects aged 40–84 years from The Health Improvement Network database, 1997–2006, we identified 3,850 patients with incident PU. Among them, we confirmed 74 first UGIC episodes during a mean follow-up of 4 years. Exposure was prescription coverage during the month following PU diagnosis. We performed a nested case–control analysis and compared UGIC cases with 400 controls matched for age, sex, year and duration of follow-up. Relative risks (RR) and 95 % confidence intervals (CI) were estimated.
Results
The overall incidence of UGIC was 4.6 cases/1,000 person-years; it was highest during the months after PU diagnosis, increased with age, and it was higher in men and subjects with Helicobacter pylori infection, anemia, and alcohol use at PU diagnosis. The RR for UGIC associated with PPI prescriptions during the month after PU diagnosis was 0.56 (95 % CI 0.31–1.0). The RR for NSAIDs with and without a PPI was 1.72 (0.68–4.45) and 3.27 (0.85–12.67), respectively.
Conclusions
Findings suggest that prescription of PPIs after a PU diagnosis is associated with a reduced risk of UGIC.


Similar content being viewed by others
References
Hernández-Díaz S, García Rodríguez L. Incidence of serious upper gastrointestinal bleeding/perforation in the general population: review of epidemiologic studies. J Clin Epidemiol. 2002;55:157–163.
García Rodríguez L, Cattaruzzi C, Troncon MG, Agostinis L. Risk of hospitalization for upper gastrointestinal tract bleeding associated with ketorolac, other nonsteroidal anti-inflammatory drugs, calcium antagonists, and other antihypertensive drugs. Arch Intern Med. 1998;158:33–39.
Hernández-Díaz S, García-Rodríguez L. Overview of epidemiological studies published in the nineties on the association between non-steroidal anti-inflammatory drugs and upper gastrointestinal bleed/perforation. Arch Intern Med. 2000;160:2093–2099.
Hawkey C, Jeffrey A, Szczepnski L, et al. A comparison of omeprazole and misoprostol for treating and preventing ulcers associated with non-steroidal anti-inflammatory drugs. N Engl J Med. 1998;338:727–734.
Yeomans N, Tulassay Z, Juhasz L, et al. A comparison of omeprazole and ranitidine for treating and preventing ulcers associated with non-steroidal anti-inflammatory drugs. N Engl J Med. 1998;338:719–726.
Silverstein F, Graham D, Senior J, et al. Misoprostol reduces serious gastrointestinal complication in patients with rheumatoid arthritis receiving non-steroidal anti-inflammatory drugs. Ann Intern Med. 1995;123:241–249.
García-Rodríguez L, Hernández-Díaz S. Relative risk of upper gastrointestinal complications among users of acetaminophen and nonsteroidal anti-inflammatory drugs. Epidemiology. 2001;12:570–576.
Jensen D, Cheng S, Kovacs T, et al. A controlled study of ranitidine for the prevention of recurrent hemorrhage from duodenal ulcer. N Engl J Med. 1994;330:382–386.
Lai K, Lam S, Chu K, et al. Lansoprazole for the prevention of recurrences of ulcer complications from long-term low-dose aspirin use. N Engl J Med. 2002;346:2033–2038.
García Rodríguez L, Ruigómez A. Secondary prevention of upper gastrointestinal bleeding associated with maintenance acid-suppressing treatment in patients with peptic ulcer bleed. Epidemiology. 1999;10:228–232.
Walker AM. Observation and inference. An introduction to the methods of epidemiology. Newton Lower Falls: Epidemiology Resources Inc.; 1991.
Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158:915–920.
Hernán M, Brumback B, Robins J. Marginal structural models to estimate the joint effect of non randomized treatments. J Am Stat Assoc. 2001;96:440–448.
Hernán M, Robins J. Instrumental variables for causal inference: an epidemiologist dream? Epidemiology. 2006;17:360–372.
Hernan MA, Hernandez-Diaz S. Beyond the intention-to-treat in comparative effectiveness research. Clin Trials. 2012;9:48–55.
Bourke A, Dattani H, Robinson M. Feasibility study and methodology to create a quality-evaluated database of primary care data. Inform Prim Care. 2004;12:171–177.
NHS Terminology Service. http://www.connectingforhealth.nhs.uk/terminology/readcodes. 2006. Accessed 12 January 2013.
First Databank. MULTILEX for Primary Care. http://www.firstdatabank.co.uk/8/multilex-drug-data-file. 2010. Accessed March 2012.
Margulis AV, Garcia Rodriguez LA, Hernandez-Diaz S. Positive predictive value of computerized medical records for uncomplicated and complicated upper gastrointestinal ulcer. Pharmacoepidemiol Drug Saf. 2009;18:900–909.
Andersen IB, Jorgensen T, Bonnevie O, Gronbaek M, Sorensen TI. Smoking and alcohol intake as risk factors for bleeding and perforated peptic ulcers: a population based cohort study. Epidemiology. 2000;11:434–439.
Lanas A, Remacha B, Esteva F, Sainz R. Risk factors associated with refractory peptic ulcers. Gastroenterology. 1995;109:1124–1133.
Gabriel SE, Jaakkimainen L, Bombardier C. Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs. Ann Intern Med. 1991;115:787–796.
Patrono C, Coller B, Dalen J, et al. Platelet-active drugs: the relationships among dose, effectiveness, and side effects. Chest. 2004;126:234S–264S.
Fitzgerald G, Patrono C. The coxibs, selective inhibitors of cyclooxygenase-2. N Engl J Med. 2001;345:433–442.
Laine L. Review article: the effect of Helicobacter pylori infection on non-steroidal anti-inflammatory drug-induced upper gastrointestinal tract injury. Aliment Pharmacol Ther. 2002;16:34–39.
Hopkins R, Girardi L, Turney E. Relationship between Helicobacter pylori eradication and reduced duodenal and gastric ulcer recurrence: a review. Gastroenterology. 1996;110:1244–1252.
Acknowledgments
The Pharmacoepidemiology Program at the Harvard School of Public Health and CEIFE are partially supported by training and research grants from various pharmaceutical companies, some of which manufacture non-steroidal anti-inflammatory drugs and/or gastroprotective agents. This study was funded by an unrestricted research grant from AstraZeneca R&D Mölndal, Sweden.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
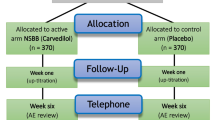
See Fig. 3.
Simplified causal diagram for an observational study with prescription of Z, use of treatment A, and outcome Y. U represents the unmeasured common causes of A and Y. An “intention to treat” analysis of the Z-Y association will be confounded unless prognostic factors L1 are adjusted for. An “as treated” analysis of the A-Y association will be confounded unless all prognostic factors L are adjusted for
Appendix 2
Rights and permissions
About this article
Cite this article
Hernández-Díaz, S., Martín-Merino, E. & García Rodríguez, L.A. Risk of Complications After a Peptic Ulcer Diagnosis: Effectiveness of Proton Pump Inhibitors. Dig Dis Sci 58, 1653–1662 (2013). https://doi.org/10.1007/s10620-013-2561-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-013-2561-9