Abstract
Background and Aims
Endoscopic therapies for Barrett’s esophagus (BE) associated dysplasia, particularly radiofrequency ablation (RFA), are popular alternatives to surgery. The effect of such therapies on dysplastic stem/progenitor cells (SPC) is unknown. Recent studies suggest that AKT phosphorylation of β-Catenin occurs in SPCs and may be a marker of activated SPCs. We evaluate the effect of RFA in restoring AKT-mediated β-Catenin signaling in regenerative epithelium.
Methods
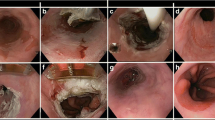
Biopsies were taken from squamous, non-dysplastic BE, dysplastic BE and esophageal adenocarcinoma (EAC). Also, post-RFA, biopsies of endoscopically normal appearing neosquamous epithelium were taken at 3, 6, and 12 months after successful RFA. Immunohistochemistry and Western blot analysis was performed for Pβ-Catenin552 (Akt-mediated phosphorylation of β-Catenin), Ki-67 and p53.
Results
There was no difference in Pβ-Catenin552 in squamous, GERD, small bowel and non-dysplastic BE. There was a fivefold increase in Pβ-Catenin552 in dysplasia and EAC compared to non-dysplastic BE (P < 0.05). Also, there was a persistent threefold increase in Pβ-Catenin552 in neosquamous epithelium 3 months after RFA compared to native squamous epithelium (P < 0.05) that correlated with increased Ki-67. Six months after RFA, Pβ-Catenin552 and Ki-67 are similar to native squamous epithelium.
Conclusions
Enhanced AKT-mediated β-Catenin activation is seen in BE-associated carcinogenesis. Three months after RFA, squamous epithelial growth from SPC populations exhibited increased levels of Pβ-Catenin552. This epithelial response becomes quiescent at 6 months after RFA. These data suggest that elevated Pβ-Catenin552 after RFA denotes a repair response in the neosquamous epithelium 3 months post-RFA.





Similar content being viewed by others
Abbreviations
- BE:
-
Barrett’s esophagus
- EAC:
-
Esophageal adenocarcinoma
- GERD:
-
Gastroesophageal reflux disease
- SPC:
-
Stem/progenitor cell
- RFA:
-
Radiofrequency ablation
- HGD:
-
High grade dysplasia
References
Camilleri M, Dubois D, Coulie B, et al. Prevalence and socioeconomic impact of upper gastrointestinal disorders in the United States: results of the US upper gastrointestinal study. Clin Gastroenterol Hepatol. 2005;3:543–552.
Morales CP, Souza RF, Spechler SJ. Hallmarks of cancer progression in Barrett’s oesophagus. Lancet. 2002;360:1587–1589.
Lagergren J, Bergstron R, Lingdgren A, et al. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. New Engl J Med. 1999;340:825–831.
Shaheen NJ, Crosby NA, Bozymski EM, et al. Is there publication bias in the reporting of cancer risk in Barrett’s esophagus? Gastroenterology. 2000;119:587–589.
Pohl H, Welch HG. The role of overdiagnosis and reclassification in the marked increase of esophageal adenocarcinoma incidence. J Natl Cancer Inst. 2009;97:142–146.
Rastogi A, Puli S, El-Serag H, et al. Incidence of esophageal adenocarcinoma in patients with Barrett’s esophagus and high-grade dysplasia, a meta-analysis. Gastrointest Endosc. 2008;67:394–398.
Birkmeyer JD, Sierwers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. New Engl J Med. 2002;346:1128–1137.
Sharma P, Wani S, Rastogi A. Endoscopic therapy for high-grade dysplasia in Barrett’s esophagus: ablate, resect, or both? Gastrointest Endosc. 2007;66:469–474.
Williams V, Watson T, Herbella F, et al. Esophagectomy for high grade dysplasia is safe, curative, and results in good alimentary outcome. Gastrointest Surg. 2007;11:1589–1597.
Shaheen NJ, Sharma P, Overholt BF, et al. Radiofrequency ablation in Barrett’s esophagus with dysplasia. N Engl J Med. 2009;360:2277–2288.
Ganz R, Overholt B, Sharma V, et al. Circumferential ablation of Barrett’s esophagus that contains high-grade dysplasia: a US multicenter registry. Gastrointest Endosc. 2008;68:35–40.
Sharma V, Kim H, Das A, et al. A prospective pilot trial of ablation of Barrett’s esophagus with low-grade dysplasia using stepwise circumferential and focal ablation (halo system). Endoscopy. 2008;40:388–392.
Gondrie J, Pour R, Sondermeijer C, et al. Effective treatment of early Barrett’s neoplasia with stepwise circumferential and focal ablation using the halo system. Endoscopy. 2008;40:370–379.
Pouw R, Gondrie J, Sondermeijer C. Eradication of Barrett esophagus with early neoplasia by radiofrequency ablation, with or without endoscopic resection. J Gastrointest Surg. 2008;12:1627–1636.
Goss KH, Groden J. Biology of the adenomatous polyposis coli tumor suppressor. J Clin Oncol. 2000;18:1967–1979.
Clevers H. Wnt/beta-catenin signaling in development and disease. Cell. 2006;127:469–480.
Reya T, Clevers H. Wnt signalling in stem cells and cancer. Nature. 2005;434:843–850.
Tetsu O, McCormick F. Beta-catenin regulates expression of cyclin d1 in colon carcinoma cells. Nature. 1999;398:422–426.
Morin P, Sparks A, Korinek V, et al. Activation of beta-catenin-tcf signaling in colon cancer by mutations in beta-catenin or apc. Science. 1997;275:1787–1790.
Koppert LB, van der Velden AWVD, van de Wetering M, et al. Frequent loss of the axin1 locus but absence of axin1 mutations in adenocarcinomas of the gastro-oesophageal junction with nuclear beta-catenin expression. Brit J Cancer. 2004;90:892–899.
Fang D, Hawke D, Zheng Y, et al. Phosphorylation of beta-catenin by akt promotes beta-catenin transcriptional activity. J Biol Chem. 2007;282:11221–11229.
Lee G, Goretsky T, Managlia E, et al. Phosphoinositide 3-kinase signaling mediates beta-catenin activation in intestinal epithelial stem and progenitor cells in colitis. Gastroenterology. 2010;139:869–881.
Brown JB, Lee G, Managlia E, et al. Mesalamine inhibits epithelial beta-catenin activation in chronic ulcerative colitis. Gastroenterology. 2010;138:595–605.
Clement G, Braunschweig R, Pasquier N, et al. Alterations of the wnt signalling pathway during the neoplastic progression of Barrett’s esophagus. Oncogenomics. 2006;25:3084–3092.
Veeramachaneni N, Kubokura H, Lin L, et al. Down-regulation of beta catenin inhibits the growth of esophageal carcinoma cells. J Thorac Cardiovasc Surg. 2004;127:92–98.
Bian Y, Osterheld M, Bosman F, et al. Nuclear accumulation of beta-catenin is a common and early event during neoplastic progression of Barrett’s esophagus. Am J Clin Pathol. 2000;114:589–590.
Gonzalez M, Artimez M, Rodrigo L, et al. Mutation analysis of the p53, apc, and p16 genes in the Barrett’s oesophagus, dysplasia, and adenocarcinoma. J Clin Pathol. 1997;50:212–217.
Odze R, Lauwers G. Histopathology of Barrett’s esophagus after ablation and endoscopic mucosal resection therapy. Endoscopy. 2008;40:1008–1015.
Kalabis J, Oyama K, Okawa T, et al. A subpopulation of mouse esophageal basal cells has properties of stem cells with the capacity for self-renewal and lineage specification. J Clin Investig. 2008;118:3860–3869.
Flejou J. Barrett’s oesophagus: from metaplasia to dysplasia and cancer. Gut. 2005;54:i6–i12.
Sansom O, Reed K, Hayes A, et al. Loss of Apc in vivo immediately perturbs Wnt signaling, differentiation, and migration. Genes Dev. 2004;18:1385–1390.
Barker N, Ridgeway R, van Es J, et al. Crypt stem cells as the cells-of-origin of intestinal cancer. Nature. 2009;457:608–611.
Yuan TL, Cantley LC. Pi3k pathway alterations in cancer: variations on a theme. Oncogene. 2008;27:5497–5510.
El Sagatys C, Garrett C, Boulware D, et al. Activation of the serine/threonine protein kinase akt during the progression of Barrett neoplasia. Hum Pathol. 2007;38:1526–1531.
Beales I, Ogunwobi O, Cameron E, et al. Activation of Akt is increased in the dysplasia-carcinoma sequence in Barrett’s oesophagus and contributes to increased proliferation and inhibition of apoptosis: a histopathological and function study. BMC Cancer. 2007;7.
Jaiswal K, Tello V, Lopez-Guzman C, et al. Bile salt exposure causes phophatidyl-inositol-3-kinase mediated proliferation in a Barrett’s adenocarcinoma cell line. Surgery. 2004;136:160–168.
Marsh V, Winton D, Williams G, et al. Epithelial pten is dispensable for intestinal hemostasis but suppresses adenoma development and progression after apc mutation. Nat Genet. 2008;40:1436–1444.
Pouw RE, Gondrie JJ, Rygiel AM, et al. Properties of the neosquamous epithelium after radiofrequency ablation of Barrett’s esophagus containing neoplasia. Am J Gastroenterol. 2009;104:1366–1373.
Bovolenta P, Esteve P, Ruiz J, et al. Beyond Wnt inhibition. New functions of secreted frizzled-related proteins in development and disease. J Cell Sci. 2008;121:737–746.
Zhang H, Spechler S, Souza R, et al. Esophageal aenocarcinoma arising in Barrett esophagus. Cancer Lett. 2009;275:170–177.
Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;1000:57–70.
Acknowledgments
T. A. Barrett was supported by NIH, R01DK-54778 and R01DK-47073.
Conflict of interest
No conflicts of interest exist for any of the authors of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krishnan, K., Komanduri, S., Cluley, J. et al. Radiofrequency Ablation for Dysplasia in Barrett’s Esophagus Restores β-Catenin Activation Within Esophageal Progenitor Cells. Dig Dis Sci 57, 294–302 (2012). https://doi.org/10.1007/s10620-011-1899-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-011-1899-0