Abstract
Background
Insomnia is highly prevalent and cognitive behavioural therapy is the first-line treatment for it. This study aimed to assess the efficacy of remote cognitive behavioural therapy for insomnia, specifically, treatment fully delivered through the internet, mobile phones and telephones for sleep and other health outcomes in adults diagnosed with insomnia or reporting insomnia symptoms. This study also aimed to evaluate the effect of various intervention components as subgroup variables to explain the efficacy of remote cognitive behavioural therapy on health outcomes.
Methods
Randomised controlled trial studies were obtained from five electronic databases. The PEDro scale was used to assess the quality of the studies. A random effect model was used to assess the mean difference, standardised mean difference and standard deviation of the outcome variables. Heterogeneity among the study articles was assessed using I2 and Q tests. Egger regression analysis was used to assess publication bias.
Results
Remote cognitive behavioural therapy for insomnia had significant and positive effects on improving sleep outcomes, depression, anxiety, fatigue and mental health compared with the control conditions. Its effect on physical health was not significant. The effect of the therapy was enhanced when the total length of intervention was shorter than 6 weeks, delivered via the internet and did not include therapist support.
Conclusion
Remote cognitive behavioural therapy for insomnia is effective in improving sleep quality, depression, anxiety, fatigue and mental health in insomnia patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Insomnia is a common type of sleep disorder that is characterised by difficulty falling and remaining asleep, which leads to physical and mental distress during the daytime (Roth, 2007). There is a high prevalence of insomnia across the world. Studies have reported that the overall prevalence of insomnia symptoms among adults in America is over 20% (Dopheide, 2020; Ohayon, 2002) of the total population. A chronic condition of insomnia can lead to heavy burdens on quality of life and the economic condition of an individual, family and society (Daley et al., 2009; Kyle et al., 2010). In addition, insomnia can be a risk factor for other chronic and mental health problems, including cardiovascular diseases, diabetes, anxiety and depression (Guo et al., 2013; Medic et al., 2017).
Given the high prevalence and disease burdens, treatment of insomnia is imperative. Traditional pharmacological treatment for insomnia has risks of providing negative side effects. Further, the long-term effects are limited (Buscemi et al., 2007). In addition to pharmacological treatment, non-pharmacological treatment has been developed and recommended, aiming to provide fewer side effects as an adjunctive method of pharmacological treatment. Cognitive therapy, or cognitive restructuring, helps patients to identify negative understandings and beliefs about sleep and replace them with positive thoughts (Beck & Weishaar, 1989). Behavioural therapy, mainly sleep restriction and stimulus control, for treating insomnia focuses on developing a proper sleep schedule and using the bed only for sleep (Banks & Dinges, 2007; Bootzin et al., 1991). As a part of the non-pharmacological approach, sleep hygiene education involves teaching patients to create a proper bedroom environment and develop daily habits that promote better sleep (Hale & Marshall, 2019; Riemann, 2018). A well-developed cognitive behavioural therapy for insomnia (CBT-I) plan usually contains multiple components, such as a cognitive therapy component, behavioural therapy component, sleep hygiene and other components. The aim of CBT-I is to identify and change the sustaining factors of insomnia, including problematic thoughts, feelings and sleep behaviours.
The traditional way of delivering CBT-I is through face-to-face consultation sessions between therapists and patients; however, limitations still exist for face-to-face delivery. The concept of telemedicine, which refers to the delivery of treatment across a distance, has been developed since last century (Wootton, 2001). Adapting telemedicine concepts, remote CBT-I has been developed to be fully delivered through the internet, telephones and mobile phone applications (Salazar de Pablo et al., 2023). Studies have shown that remote CBT-I has a higher level of cost and clinical effectiveness compared with face-to-face treatments, especially for patients in rural areas because they can receive treatments at home without travelling to medical facilities (Hjelm, 2005; Wootton et al., 2017). In addition, remote CBT-I can be delivered using a minimum level of support from real therapists, which reduces the cost of treatment and is more scalable for patients (Fairburn & Patel, 2017; Karyotaki et al., 2017).
Although CBT-I was recommended as the first-line treatment for insomnia by the American College of Physicians (Qaseem et al., 2016), the actual dissemination of CBT-I remains challenging given the high cost of distribution and lack of professional therapists (Muench et al., 2022). Previously published meta-analysis studies have concluded that CBT-I has a significant effect in treating insomnia (Seyffert et al., 2016; Straten et al., 2018; Trauer et al., 2015; Zachariae et al., 2016; Zweerde et al., 2019a). Recent meta-analysis studies (Gao et al., 2022; Hasan et al., 2022; Simon et al., 2023) have mentioned that remote CBT-I has significant effects on improving sleep in insomnia patients. However, these studies mainly focused on the effect of CBT-I on sleep outcomes. Patients who had insomnia were frequently reported as experiencing depression, anxiety and daytime fatigue problems, including a decreased quality of life, which were also important factors when evaluating the overall health of these patients. Other studies (Alimoradi et al., 2022; Cunningham & Shapiro, 2018; Lee et al., 2023) have concluded that remote CBT-I has positive effects on depression, anxiety and quality of life; however, the effects of the detailed intervention design and various CBT-I components were not well explained.
To address the research gaps, this study aimed to provide a comprehensive overview of the efficacy of remote CBT-I on not only sleep outcomes but also co-existing depression and anxiety symptoms, daytime fatigue and quality of life-related physical and mental health in patients who have been diagnosed with insomnia disorder or are reporting insomnia symptoms. Subgroup analysis was conducted to assess the effect of remote CBT-I characteristics and components on the overall impact of remote CBT-I treatment. The results of this study will contribute to the theoretical understanding of remote CBT-I in treating insomnia and assist the development of proper treatment plans in clinical conditions, which may help to disseminate remote CBT-I.
Methods
The procedure of this study was developed using the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines (Liberati et al., 2009). This study was registered at the international prospective register of systematic reviews (PROSPERO) and the registration ID is CRD42020200091. The research protocol can be found at the following website: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020200091.
Database Search
A whole database search and study selection process was completed by two researchers independently. A third researcher was consulted in cases of disagreement until consensus was reached. Relevant studies were searched for in five electronic databases: PubMed, Scopus, EMBASE, Cochrane Library and PsycINFO. Grey literature was acquired from ProQuest Central: Dissertations and Thesis. A Boolean approach was used to search for the following keywords in titles and abstracts: ‘insomnia’ OR ‘sleep’ AND ‘remote CBT’ OR ‘telehealth’ AND ‘cognitive behavioural therapy’ OR ‘CBT’ AND ‘internet’ OR ‘telephone’ OR ‘mobile phone’ AND ‘randomised controlled trial’ OR ‘randomised controlled trial’ OR ‘RCT’. The search results from the five defined databases were exported into EndNote X9 software, in which duplicates across the databases were removed. The titles and abstracts of the articles were then examined, and articles focusing on remote CBT and insomnia were excluded from the study. The researchers then conducted a further review of the full text of the articles and screened the eligible articles for data analysis in accordance with the designed inclusion and exclusion criteria.
Study Selection
The following inclusion and exclusion criteria were developed according to the population, intervention, control and outcomes (PICO) approach (Leonardo, 2018).
Inclusion Criteria
P: The target population in the studies were over 18 years in age and had been diagnosed with insomnia (regardless of disease severity) according to valid definitions, guidelines or surveys (Association, 2013; Buysse et al., 1989; Insomnia, 1993; Sateia, 2014). Articles that reported the recruitment of subjects using self-reported insomnia symptoms without specific diagnostic criteria were also included.
I: The intervention described in the articles included at least one behavioural component (e.g. sleep restriction, stimulus control) and one cognitive component (e.g. cognitive restructure) and at least four intervention sessions. The number of other components in the intervention plan was not limited. The intervention was remotely delivered via telephone, internet or mobile phone applications.
C: Participants in the control groups received normal care for insomnia, including basic sleep education and pharmacological intervention (Riemann et al., 2017), or were put on a waitlist and received intervention later. Participants in the control groups could also receive face-to-face CBT-I.
O: The primary outcomes in this study were subjective sleep outcomes, including insomnia severity measured by the insomnia severity index (Insomnia, 1993), sleep quality measured by the Pittsburgh sleep quality index (Buysse et al., 1989), total sleep time, sleep efficiency, sleep onset latency, wake after sleep onset and number of awakenings. Secondary outcomes in this study included depression symptoms, anxiety symptoms, fatigue and quality of life-related physical and mental health. Depression symptoms were measured by scores of depression scales (Beck et al., 1996; Eaton et al., 2004; Hamilton, 1986; Yesavage, 1988; Zung, 1965), and anxiety symptoms were measured by anxiety scales (Beck et al., 1988; Bieling et al., 1998; Zigmond & Snaith, 1983). The fatigue outcome was measured by the scores of fatigue scales (Krupp et al., 1989; Smets et al., 1995). The quality of life-related health outcomes were measured by the scores of the physical health and mental health sections in quality of life surveys (SF-12, SF-36 or any other verified quality of life surveys comprising physical health and mental health sections) (Ware et al., 1994). Articles reporting at least one of the primary outcomes were included. For all outcome variables, articles should report the means and standard deviations before and after intervention for the intervention and control groups or mean differences with standard deviations.
In addition, the article should involve a randomised controlled trial design, in which participants were randomly assigned to intervention or control groups, having no restrictions in sample size and length of follow-up. There were no restrictions on language and publication date. The full text of the article was available online or through reasonable attempts, such as sending emails directly to the authors to request the full text of the articles.
Exclusion Criteria
The participants in the study were diagnosed with severe psychiatric diseases that exerted cognitive or behavioural impairment, such as schizophrenia, severe depression and severe bipolar disorders. The study design did not use remote CBT-I intervention or did not include any control groups. The study was also excluded if participants in the control group received any form of complementary or non-pharmacological intervention for insomnia other than CBT-I, including light therapy, mindfulness therapy, homeopathy and acupuncture (Riemann et al., 2017). The study did not provide complete data for at least one of the primary outcomes. The articles were literature reviews or study protocols. Duplicated articles, journal articles that were not peer-reviewed and low-quality studies scoring 3 or lower on the physiotherapy evidence database (PEDro) scale (Verhagen et al., 1998) were also excluded.
Quality Assessment
The quality assessment of studies was completed by two researchers independently using the PEDro scale (Verhagen et al., 1998). The PEDro scale evaluates the quality of randomised controlled trials by giving scores ranging from 0 to 10. The marking criteria include random allocation of subjects, concealed allocation of subjects, similar baseline characteristics, blinding to all subjects, blinding to all therapists, blinding to assessors who assessed the key outcomes, enough outcome measures obtained, subjects received intervention or control condition as study designed, presence of between-group comparison analysis and presence of point measures and measures of variability. One point is given if the study completely meets each of the criterion, otherwise no point is given. The quality of studies was categorised into four levels: low quality (≤ 3 points), moderate quality (4–5 points), good quality (6–8 points) and excellent quality (9–10 points) (Cashin & McAuley, 2020).
Data Extraction
The data extraction process was completed by two researchers independently. In cases of disagreement, the third researcher was invited to review and confirm the data. If the article provided results for post-intervention and follow-up, the results for post-intervention and the longest follow-up time were extracted. When the published articles did not provide enough data, reasonable attempts, such as direct email requests to the corresponding authors, were made to acquire the full data sets of the studies.
Characteristics of Included Studies
The following characteristics of included studies were extracted: author, year of publication, location (name of country), sample size, average age of participants, gender (number and percentage of female), type of disease, including comorbidity, diagnosis criteria of insomnia, description of intervention, delivery format, use of manual, duration of treatment, length of longest follow-up, therapist support, percentage of participants that completed the treatment, description of control condition, outcome variable names and PEDro score.
Primary and Secondary Outcomes
The means and standard deviations for the primary and secondary outcomes were extracted from the included studies for the intervention and control groups before and after intervention. The extracted data were exported into an Excel document.
Subgroup Variables
The designs and groupings of the subgroup variables were in accordance with the recommended CBT-I design and characteristics from the published CBT-I guidelines for treating insomnia (Perlis et al., 2005). The characteristics of intervention were collected from each study and manually coded into subgroups. The subgroup variables included overall dropout rate (0 for < 20% and 1 for ≥ 20%), length of intervention (0 for ≤ 6 weeks and 1 for > 6 weeks), length of follow-up (0 for ≤ 3 months and 1 for > 3 months), delivery format (0 for telephone, 1 for internet and 2 for mobile phone applications), presence of therapist support (0 for self-help and 1 for guided), control condition (0 for no treatment, 1 for other treatment and 2 for education and information) and presence of important components, including sleep hygiene, relapse prevention, relaxation training, sleep education and homework (0 for not present and 1 for present).
Statistical Analysis
The software used for data analysis in this study was STATA 17.0. The significance level was set as 0.05 (two-sided) and a p value of less than 0.05 was considered to be statistically significant. A separate meta-analysis using a random effects model, which provided a statistical parameter of the variations among the studies (DerSimonian & Kacker, 2007), was performed for each of the primary and secondary outcomes. The meta-analysis was conducted separately for the post-intervention and follow-up results. Given that all of the outcome variables in this study were continuous variables, pooled mean differences (MD) that had 95% confidence intervals (CIs) were used in the results presentation. Forest plots were plotted to give a straightforward overview of the results. A standardised mean difference (SMD) that had a CI of 95% was used to measure the effect size of the variables. The SMD was calculated by dividing the mean difference by the pooled standard deviation (Hedges & Olkin, 2014). A SMD between 0.2 and 0.5 indicated a small effect size, between 0.5 and 0.8 a medium effect size and greater than 0.8 a large effect size (Ferguson, 2009).
Heterogeneity of the studies was assessed using I2 values (Higgins et al., 2003) and Q tests (Huedo-Medina et al., 2006). The I2 value ranged from 0 to 100%. An I2 value larger than 50% for a certain variable indicated that there was a high heterogeneity and a subgroup analysis was required to examine the possible causes. A greater Q test value also indicated a higher level of heterogeneity. Sensitivity analysis was conducted by removing one study at a time from the meta-analysis to examine the stability of the pooled results and the potential source of the heterogeneity.
Egger’s regression analysis (Lin & Chu, 2018) was used to investigate the potential publication bias among the studies for each of the primary and secondary outcomes. The results are presented as Egger’s t values that have 95% CIs and p values. A p value greater than 0.05 indicated that the publication bias was not statistically significant. Funnel plots were presented to assist in the evaluation of publication bias.
Results
Literature Search and Study Selection
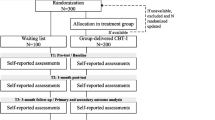
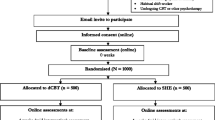
During the database search, 1849 relevant studies were identified from the five defined databases and 152 items of grey literature from other sources. The earliest record available for title and abstract examination was published in 1993 (Morin et al., 1993). A total of 546 duplicates were removed and the remaining 1455 studies underwent title and abstract examination. After the screening of titles and abstracts, 1204 articles that did not focus on remote CBT-I or insomnia were excluded from this study. The total number of articles eligible for full-text assessment was 251. Another 209 studies were excluded during full-text assessment and the final number of studies eligible for data analysis was 42. The PRISMA flow chart of the literature search and screening is presented in Fig. 1.
Characteristics of Included Studies
A total of 10,496 participants were included in the 42 studies (Abdelaziz et al., 2022; Ahorsu et al., 2020; Arnedt et al., 2013, 2021; Blom et al., 2015; Brenes et al., 2012; Chan et al., 2023; Chapoutot et al., 2021; Cheng et al., 2019; Espie et al., 2012; Freeman et al., 2015, 2017; Gieselmann & Pietrowsky, 2019; Glozier et al., 2019; Godzik et al., 2021; Hagatun et al., 2019; Ho et al., 2014; Horsch et al., 2017; Hürlimann et al., 2023; Jernelöv et al., 2012; Kaldo et al., 2015; Kalmbach et al., 2020; Lancee et al., 2016; Lokman et al., 2017; Lorenz et al., 2019; McCurry et al., 2016, 2021; Morris et al., 2016; Oswald et al., 2022; Rajabi Majd et al., 2020; Ritterband et al., 2009, 2017; Siebmanns et al., 2021; Straten et al., 2014; Thorndike et al., 2013; Vedaa et al., 2020; Vincent & Lewycky, 2009; Yeung et al., 2022; Zachariae et al., 2018; Zhang et al., 2023; Zweerde et al., 2019b, 2020). The average age ranged from 25 to 72 years old. Among the participants, 8558 were female (81.5%). All of the participants in the included studies had insomnia and some of them had been diagnosed with other diseases, including epilepsy, depression, anxiety, cancer, kidney disease and cardiovascular disease. Participants in intervention groups all received remote CBT-I interventions delivered via telephone, internet or mobile phone applications. A total of 16 studies used study manuals. The total length of intervention ranged from 12 days to three months. The content of the interventions was delivered by trained therapists in 21 studies, and self-help content were provided in the other 21 studies. There was an overall high rate of completion for the interventions: the lowest compliance rate was 48% in one of the studies (Cheng et al., 2019). The control group design was divided into three categories: participants did not receive any CBT-I treatment, participants received information or education about sleep and insomnia, or participants received intervention content through face-to-face delivery. All of the 42 studies reported at least one of the primary outcomes. Among the 42 included studies, five were moderate quality, 21 were high quality and 16 were excellent quality. Details of study characteristics are displayed in Table 1.
Effect of Remote CBT-I on Sleep Outcomes
The results of the meta-analysis of the primary and secondary outcomes are presented in Tables 2 and 3. The forest plots for the meta-analysis are presented in Figs. 2 and 3.
A total of 34 studies reported the insomnia severity index as an outcome measurement. We found that there was an overall significant reduction in insomnia severity for participants in the remote CBT-I intervention groups compared with the control groups, given that there was a larger reduction in the average insomnia severity index scores than in the control groups (MD = − 3.92, 95% CI − 4.57 to − 3.26, p < 0.001, I2 = 96.65) and a large effect size (SMD = − 1.45, 95% CI − 2.13 to − 0.78, p < 0.001, I2 = 99.54). Given the high level of heterogeneity, subgroup analysis was conducted for the insomnia severity index. The results are presented in Table 3. According to the subgroup analysis, the subgroup variables that provided the greatest effect in reducing insomnia severity was form of delivery. CBT-I delivered through the internet (MD = − 4.19, 95% CI − 5.04 to − 3.34, p < 0.001, I2 = 97.40) more effectively reduced insomnia severity index scores than telephone-delivered CBT-I (MD = − 3.58, 95% CI − 4.38 to − 2.79, p < 0.001, I2 = 80.86) and CBT-I delivered through mobile phone applications (MD = − 2.92, 95% CI − 4.62 to − 1.22, p < 0.001, I2 = 82.17). In addition, remote CBT-I significantly reduced insomnia severity index scores compared with no treatment (MD = − 4.62, 95% CI − 5.53 to − 3.71, p < 0.001, I2 = 95.89) and education only conditions (MD = − 3.87, 95% CI − 4.66 to − 3.08, p < 0.001, I2 = 91.20) but showed similar effects in reducing insomnia severity compared with other deliveries of CBT-I intervention (MD = − 0.53, 95% CI − 1.63 to − 0.58, p > 0.05, I2 = 0.00).
The Pittsburgh sleep quality index was reported by 14 studies. There was an overall significant improvement in sleep quality, measured by the reduction of Pittsburgh sleep quality index scores in the remote CBT-I intervention groups compared with the control groups (MD = − 2.68, 95% CI − 3.10 to − 2.25, p < 0.001, I2 = 86.18), which had a large effect size (SMD = − 1.46, 95% CI − 2.24 to − 0.68, p < 0.01, I2 = 98.11). Subgroup analysis was conducted for the Pittsburgh sleep quality index. The results are presented in Table 3. The subgroup analysis showed that the Pittsburgh sleep quality index scores were greatly affected by the forms of CBT-I delivery. CBT-I delivered via telephone (MD = − 1.60, 95% CI − 1.77 to − 1.43, p > 0.05, I2 = 0.00) had a smaller effect on reducing Pittsburgh sleep quality index scores than therapy delivered through the internet (MD = − 2.79, 95% CI − 3.26 to − 2.32, p < 0.001, I2 = 52.29) and mobile applications (MD = − 3.09, 95% CI − 3.66 to − 2.52, p < 0.001, I2 = 0.00). The level of sleep quality index scores was not significantly affected by other subgroup variables.
For sleep outcomes from sleep diaries, there was a significant increase in total sleep time in the remote CBT-I intervention groups compared with the control groups (MD = 13.35, 95% CI 7.65–19.05, p < 0.001, I2 = 95.42), which had a medium effect size (SMD = 0.69, 95% CI 0.10–1.28, p < 0.01, I2 = 98.73). The results of the subgroup analysis on total sleep time are presented in Table 4. A more significant improvement in total sleep time could be found in studies that had a lower dropout rate (MD = 15.91, 95% CI 7.95–23.86, p < 0.001, I2 = 84.78) than studies that had a dropout rate greater than 20% (MD = 8.74, 95% CI − 2.10 to 15.37, p < 0.05, I2 = 97.19). Moreover, greater improvement in total sleep time was observed when intervention was shorter than six weeks (MD = 20.19, 95% CI 11.23–29.14, p < 0.001, I2 = 95.50) compared with interventions longer than six weeks (MD = 7.90, 95% CI 2.54–13.27, p < 0.01, I2 = 76.81). Greater improvement in total sleep time was also observed in studies that had a shorter follow-up period (MD = 18.62, 95% CI 10.26–26.98, p < 0.001, I2 = 96.71) compared with studies that had a longer follow-up (MD = 7.71, 95% CI 1.74–13.67, p < 0.05, I2 = 55.99). Other effective subgroup characteristics for total sleep time included internet delivery and presence of relaxation training.
Sleep efficiency was improved in remote CBT-I intervention groups compared with control groups (MD = 6.40, 95% CI 4.67–8.13, p < 0.001, I2 = 97.24), which had a large effect size (SMD = 1.26, 95% CI 0.57–1.96, p < 0.01, I2 = 98.98). Subgroup analysis was conducted on sleep efficiency. The results are displayed in Table 4. There was a more significant increase in sleep efficiency in studies that had a shorter follow-up (MD = 7.52, 95% CI 5.41–9.63, p < 0.001, I2 = 95.18) than studies that had a longer follow-up (MD = 4.47, 95% CI 1.69–7.25, p < 0.001, I2 = 96.15). Telephone-delivered CBT-I showed a limited effect in improving sleep efficiency (MD = 1.96, 95% CI − 1.73 to 5.65, p > 0.05, I2 = 58.57) compared with internet-delivered (MD = 6.97, 95% CI 4.97–8.96, p < 0.001, I2 = 97.56) and mobile application-delivered CBT-I (MD = 6.35, 95% CI 3.17–9.54, p < 0.001, I2 = 39.55). Remote CBT-I had a greater effect on sleep efficiency when the intervention was shorter than 6 weeks, delivered by internet, had no treatment in the control group and provided a relaxation training component.
The meta-analysis found that remote CBT-I effectively shortened the sleep onset latency time compared with the control conditions (MD = − 11.78, 95% CI − 15.74 to − 7.82, p < 0.001, I2 = 96.37), which had a large effect size (SMD = − 0.95, 95% CI − 1.38 to − 0.51, p < 0.001, I2 = 97.39). The subgroup analysis results for sleep onset latency are presented in Table 5. The subgroup variable that provided the greatest effect on sleep onset latency was relaxation training. Studies that included relaxation training (MD = − 15.15, 95% CI − 22.13 to − 8.16, p < 0.01, I2 = 97.01) showed a greater improvement in sleep onset latency than studies that did not include relaxation training (MD = − 9.26, 95% CI − 13.03 to − 5.49, p < 0.001, I2 = 87.88). Other effective subgroups included intervention length shorter than six weeks, internet delivery, no treatment in control group and sleep hygiene.
Likewise, remote CBT-I had a significant effect on improving wake after sleep onset. The average wake time after sleep onset was significantly shortened in intervention groups compared with control groups (MD = − 16.25, 95% CI − 22.39 to − 10.11, p < 0.001, I2 = 98.71), which had a large effect size (SMD = − 1.96, 95% CI − 3.52 to − 0.40, p < 0.001, I2 = 99.75). Given the high level of heterogeneity, subgroup analysis was performed on wake after sleep onset. The results can be found in Table 5. Therapist support and sleep hygiene were the two subgroup variables that had the greatest effect on shortening wake time after sleep onset. Wake time after sleep onset was more effectively shortened in studies that used self-help interventions (MD = − 18.97, 95% CI − 26.66 to − 11.28, p < 0.001, I2 = 98.77) than in studies providing therapist-guided interventions (MD = − 9.20, 95% CI − 20.68 to − 6.00, p < 0.001, I2 = 49.23). Studies that included a sleep hygiene component (MD = − 17.05, 95% CI − 23.65 to − 10.45, p < 0.001, I2 = 94.36) had a greater effect on wake after sleep onset than studies that did not (MD = − 7.40, 95% CI − 18.34 to 3.55, p > 0.05, I2 = 0.00). Other effective subgroup characteristics included a follow-up shorter than three months, internet delivered, no treatment in control group and relaxation training.
The number of awakenings was also significantly improved in remote CBT-I intervention groups compared with control groups (MD = − 0.41, 95% CI − 0.64 to − 0.17, p < 0.01, I2 = 61.33), which had a medium effect size (SMD = − 0.37, 95% CI − 0.64 to − 0.10, p < 0.01, I2 = 76.98).
Similar meta-analysis results for all sleep outcomes were found when comparing pre-intervention with post-intervention and follow-up. All of the Q test results were consistent with the I2 results in all analyses, indicating the same levels of heterogeneity in all sleep outcomes and subgroup variables. In all subgroup analysis, the p values between groups were smaller than 0.001, which suggested that there was a significant difference between groups for each of the subgroup variables.
Effect of Remote CBT-I on Depression and Anxiety Symptoms
The scores of depression scales were measured in 22 studies, and a total of 5914 participants were included in these studies. The meta-analysis showed that remote CBT-I intervention significantly improved the depressive symptoms, given that the average score of depression scales in the intervention groups was significantly lower than in the control groups (MD = − 2.13, 95% CI − 2.95 to − 1.32, p < 0.001, I2 = 88.06), which had a medium effect size (SMD = − 0.48, 95% CI − 0.68 to − 0.28, p < 0.001, I2 = 90.63) immediately after intervention. Given the high level of heterogeneity, subgroup analysis was performed on depression. The results are presented in Table 6. The subgroup variable that provided the greatest effect on depression was the form of delivery. Depression scale scores were more significantly reduced when the intervention was delivered through internet (MD = − 2.37, 95% CI − 3.49 to − 1.26, p < 0.001, I2 = 83.00) and mobile phone applications (MD = − 2.31, 95% CI − 4.23 to − 0.38, p < 0.05, I2 = 93.55). However, telephone-delivered interventions (MD = − 1.14, 95% CI − 2.82 to 0.54, p > 0.05, I2 = 85.34) did not provide a significant effect on depression scale scores. Depression was also improved when the studies had a longer intervention period, longer follow-up, provided self-help materials, had no treatment in the control group and included sleep hygiene and relaxation training components.
Anxiety scales were measured in 17 studies, which used 5,008 participants. Similarly to depression, remote CBT-I showed a greater effect on anxiety than control conditions because the average scores for anxiety scales in intervention groups were more effectively reduced than the scores in the control groups (MD = − 1.51, 95% CI − 2.01 to − 1.02, p < 0.001, I2 = 93.11), which had a medium effect size (SMD = − 0.74, 95% CI − 1.16 to − 0.33, p < 0.001, I2 = 97.35) at post-intervention. Subgroup analysis was conducted on anxiety and the results can be found in Table 6. Studies that provided a relaxation training component (MD = − 1.59, 95% CI − 2.08 to − 1.09, p < 0.001, I2 = 91.19) had the greatest effect on anxiety scale scores compared with studies that did not (MD = − 1.21, 95% CI − 3.16 to − 0.74, p > 0.05, I2 = 88.65). Anxiety was also improved when the remote CBT-I intervention had the following characteristics: an intervention period longer than six weeks, a follow-up longer than three months, self-help and a relaxation training component.
Similar meta-analysis results were found at the post-intervention and follow-up timepoints. The Q test results were consistent with the I2 results, showing the same levels of heterogeneity. The p between groups were all smaller than 0.001, suggesting that the difference between groups for each of the subgroup variables was significant (Table 7).
Effect of Remote CBT-I on Fatigue
A total of 10 studies reported fatigue as an outcome measurement. The total number of participants in these studies was 2775. We found that the level of fatigue measured by fatigue scales was significantly reduced in remote CBT-I intervention groups compared with the control groups (MD = − 1.77, 95% CI − 2.68 to − 0.87, p < 0.01, I2 = 86.89), and there was a medium effect size (SMD = − 0.62, 95% CI − 1.15 to − 0.09, p < 0.05, I2 = 96.55). The Q test result were consistent with the I2 result, indicating a significantly high level of heterogeneity.
Effect of Remote CBT-I on Quality of Life-Related Physical and Mental Health
The scores of quality of life-related physical health were reported in nine studies, and the total number of participants was 2602. The meta-analysis showed that the score difference between remote CBT-I intervention groups and control groups was not significant (MD = − 0.51, 95% CI − 2.88 to 1.86, p > 0.05, I2 = 96.20), and the effect size was small (SMD = − 0.26, 95% CI − 1.19 to 0.66, p > 0.05, I2 = 98.72).
The scores of quality of life-related mental health were reported in nine studies, and the total number of participants was 2285. Unlike the physical health scores, a greater improvement in mental health scores was observed in remote CBT-I intervention groups than the control groups (MD = 4.27, 95% CI 1.71–6.84, p < 0.01, I2 = 92.24), which had a large effect size (SMD = 0.81, 95% CI 0.10–1.51, p < 0.05, I2 = 96.80). In addition, the Q test results for physical health and mental health were consistent with the I2 results, representing the same level of heterogeneity.
Publication Bias
Egger’s regression test was conducted to assess the publication bias of all outcomes. The results are summarised in Table 2. No significant publication bias was found for all of the research outcomes, including the insomnia severity index (t = 0.45, 95% CI − 1.12 to 1.75, p > 0.05), the Pittsburgh sleep quality index (t = − 1.24, 95% CI − 2.20 to 0.61, p > 0.05), total sleep time (t = 1.44, 95% CI − 0.28 to 1.57, p > 0.05), sleep efficiency (t = − 0.56, 95% CI − 1.23 to 2.14, p > 0.05), sleep onset latency (t = − 0.20, 95% CI − 2.43 to 2.00, p > 0.05), wakening after sleep onset (t = 1.38, 95% CI − 0.74 to 3.49, p > 0.05), number of awakenings (t = 0.49, 95% CI − 2.39 to 3.69, p > 0.05), depression (t = − 0.98, 95% CI − 2.22 to 0.80, p > 0.05), anxiety (t = − 0.64, 95% CI − 1.83 to 0.99, p > 0.05), fatigue (t = 1.60, 95% CI − 0.55 to 3.00, p > 0.05), physical health (t = 0.76, 95% CI − 2.24 to 4.36, p > 0.05) and mental health (t = − 0.64, 95% CI − 4.15 to 2.38, p > 0.05). The funnel plots are provided in Supplementary Figs. 1 and 2. Visual inspection of the funnel plots found a symmetric distribution of mean difference for all outcome variables except the Pittsburgh sleep quality index. In addition, results from the sensitivity analysis suggested that removing any single study did not change the overall publication bias results. Therefore, no significant publication bias was found for all outcome variables.
Discussion
This meta-analysis included 42 randomised controlled trial studies that included a total of 10,496 participants. The results from this meta-analysis showed that remote CBT-I intervention was effective in improving sleep outcomes (insomnia severity index, Pittsburgh sleep quality index, total sleep time, sleep efficiency, sleep onset latency, wakening after sleep onset and number of awakenings), depression symptoms, anxiety symptoms, fatigue and quality of life-related mental health. Remote CBT-I intervention did not have significant effects on quality of life-related physical health.
Effect of Remote CBT-I Approach on Sleep Outcomes
Remote CBT-I was significantly effective in improving overall sleep quality and reducing insomnia severity, which is consistent with prior studies (Seyffert et al., 2016; Zachariae et al., 2016). One of the major goals of CBT-I interventions is to limit sleep opportunities during the day to increase the pressure for sleep at normal sleep times, leading to an improved homeostatic regulation of sleep (Koffel et al., 2015; Smith et al., 2002). The establishment of a regulated sleep cycle through a CBT-I approach has produced positive effects on not only overall sleep quality and the reduction of insomnia severity but also the improvement in total sleep time, sleep efficiency, sleep onset latency, wake after sleep onset and number of awakenings.
The subgroup analysis identified sleep hygiene and relaxation training as effective components, and the results were consistent with prior studies (Chung et al., 2018; Garcia et al., 2018; Hayes-Skelton & Lee, 2020; Pardo Cebrián & Calero, 2019). Sleep hygiene education teaches insomnia patients the right behaviours that promote sleep, such as keeping a quiet sleep environment and maintaining regular sleep schedules, while discouraging unhelpful behaviours, such as alcohol and tobacco intake (Morin & Insomnia, 2007). This is effective in improving sleep quality because it helps to develop habits that are advantageous for sleep (Morin & Insomnia, 2007). Relaxation training is also effective in improving sleep because it provides relaxation strategies for physical and mental conditions (Sateia & Insomnia, 2016; Zung, 1965). A more relaxed condition can decrease arousal at night and make it easier to fall asleep and therefore prolong the sleep duration (Buysse, 2013). Relapse prevention appeared to have limited effect, which was possibly because of other effects, given that the level of heterogeneity was still very high. Despite the limited effect, relapse prevention consolidates the acquired skills (Larimer et al., 1999); thus, researchers should be cautious when considering the exclusion of relapse prevention. In addition, sleep education had limited effects because it did not provide any practical skills. Finally, the effect of homework was not significant because in many of the studies, homework was given as recording sleep and filling in sleep diaries, which do not provide a direct effect on sleep improvement. However, we need to mention that completely discouraging homework is not recommended because the completion of homework is important in measuring participant adherence and data collection (Laloyaux et al., 2013).
In addition, sleep outcomes were more significantly improved in studies that had a shorter length of intervention, which differed from the findings of prior studies (Zachariae et al., 2016), in which greater effects were observed in longer interventions. A possible explanation for the difference is that patients might be less focused in longer interventions because they might forget to access the intervention sessions or just have a quick glance at the self-help materials after weeks of treatment. In addition, the dropout rate was closely related to the length of intervention. A longer intervention period usually leads to a higher dropout rate, which also affects the final effect of treatment.
We also found that the improvement in sleep outcomes was more significant in studies that had a shorter follow-up period. As described in prior studies (Jernelöv et al., 2022; Zweerde et al., 2019c), although the effect of CBT-I could last for over 12 months, the overall effect generally decreases over time, which means that the long-term effect of CBT-I is smaller than the short-term effect. The reason for this could be that the patients in intervention groups no longer adhere to the advantageous sleep behaviours developed during the intervention, leading to the increase of insomnia symptoms (Zweerde et al., 2019c).
For the delivery methods, patients can access the intervention content in the forms of voice, texts, videos, graphs and figures or facial expressions and gestures of the therapists, which can be viewed at any time through internet and mobile application delivery. All of the elements enhance the understanding of the intervention content. However, patients can only make voice contact with the therapists during the telephone sessions, and the opportunity for obtaining extra contact with the therapists after the telephone sessions is limited. Our findings on therapist support differed from prior studies (Zachariae et al., 2016) because self-help designs were more effective than guided ones. Although therapist support may enhance the adherence of participants, self-help materials are more flexible and enable participants to develop their own understanding and practice without being constrained by therapists.
In general, remote CBT-I had similar effects on sleep outcomes to face-to-face treatments. However, the number of studies that have directly compared the difference between remote CBT-I and face-to-face intervention is limited and further studies are required.
Effect of Remote CBT-I Approach on Depression and Anxiety Symptoms
Similar to the findings from prior studies (Carpenter et al., 2018; Hall et al., 2016; Koffel et al., 2015; Lattie et al., 2019), remote CBT-I was effective in reducing depression and anxiety symptoms in patients who had insomnia. Although most of the treatment content in this study targeted sleep behaviours, cognitive components in the interventions still retained the functions of rectifying negative thoughts and beliefs, which could also benefit depression and anxiety conditions (Larzelere & Wiseman, 2002). In addition, prior studies have mentioned that there is a close relationship between insomnia and depression and anxiety symptoms and the relationship is bidirectional (Dopheide, 2020). Treating insomnia is recognised as an important part of treating depression and anxiety. Remote CBT-I provides a significant effect on improving sleep quality and the improvement of sleep quality has a positive influence on daytime symptoms such as depression and pain (Koffel et al., 2015).
There are still differences between the subgroup analysis results for sleep outcomes, depression symptoms and anxiety symptoms. Remote CBT-I showed a greater effect on depression and anxiety symptoms when the length of intervention was longer than 6 weeks. This is reasonable because insomnia is only one of the secondary manifestations of depression (Fang et al., 2019). A longer intervention period allows therapists to develop a closer relationship with patients and the therapists will have a greater chance to provide more specific psychological counselling to target the conditions of every single patients, for insomnia and other factors contributing to their depression and anxiety symptoms (Koffel et al., 2015). Sleep education did not seem to have a great effect on depression and anxiety symptoms because the education content did not include information on depression and anxiety.
Effect of Remote CBT-I Approach on Fatigue
The relationship between sleep and fatigue has been well understood and described in many studies. Studies have claimed that the greatest cause of fatigue is the insufficiency of sleep (Caldwell et al., 2019), which explains the significant effect of remote CBT-I in reducing levels of fatigue. As discussed earlier, remote CBT-I significantly increased sleep quality and reduced insomnia severity, which prolonged the total sleep time at night and reduced the chance of sleep disruption. A regulated sleep cycle enabled the patients to be fully rested in bed and this directly reduced the level of fatigue during the day (Caldwell et al., 2019).
Effect of Remote CBT-I Approach on Quality of Life-Related Physical and Mental Health
Prior studies have mentioned that a chronic condition of insomnia exerts negative effects on mood and cognitive functions (Khan & Aouad, 2017). People in a constant bad mood tend to develop more negative thoughts, which impair overall mental health and quality of life. CBT-I interventions promote better rest and rectify negative thoughts of patients, leading to a positive attitude towards the surroundings and therefore improve mental health (González-Valero et al., 2019). The reason that remote CBT-I did not show a significant effect on physical health is that the CBT-I intervention that participants received focused on insomnia only and the content about other diseases and lifestyles were limited. Moreover, an improvement in physical health usually takes longer to be observed. Therefore, it is reasonable that physical health is not greatly affected by remote CBT-I treatment.
Strength, Limitations and Implications
This study performed a meta-analysis of 42 high-quality randomised controlled trial studies focusing on treating insomnia using remote CBT-I. Subgroup analysis was conducted to identify factors that may explain the effect of remote CBT-I intervention on the improvement of sleep patterns, depression symptoms and anxiety symptoms. This study used a high-quality study design and minimised publication bias.
There are a number of limitations of this study. First, patients who had been clinically diagnosed with insomnia disorder and patients who reported insomnia symptoms or poor sleep quality were included in this study; however, we were not able to perform subgroup analysis on the clinical diagnosis of insomnia and a cut-off for subjective measures. Second, most of the included randomised controlled trials did not provide clear comorbidity information for the participants; thus, we were not able to group comorbidities as subgroup variables and could not identify the effect of remote CBT-I on different comorbidities. During the subgroup analysis process, some groupings of the subgroup variables were presented in a limited number of studies; thus, the evaluation of these subgroup variables might not be possible. Finally, we observed high levels of heterogeneity for some outcomes in the meta-analysis and subgroup analysis, which means that heterogeneity was similar in the analyses for primary outcomes and the subgroup analysis provided a limited explanation of the high levels of heterogeneity. Another limitation was that we did not include an analysis of comorbidities in this study because most of the included randomised controlled trials did not provide clear comorbidity information for the participants; thus, we were not able to group comorbidities as subgroup variables. Therefore, further studies that include more studies are needed to support the findings from this study.
Overall, remote CBT-I intervention is a possible option for treating insomnia. When designing an intervention plan, it is necessary to retain participants in groups and minimise the dropout rate. The recommended intervention plan includes the following characteristics: total intervention period around six weeks, delivered through internet or mobile phone applications, more self-help content and include components such as sleep hygiene and relaxation training while avoiding complex homework that takes a long time to complete. Although the results indicate that relapse prevention and sleep education components provided a smaller influence on the overall intervention effect, this does not mean that these components can be excluded from the intervention design.
Conclusion
In conclusion, remote CBT-I intervention is effective in improving sleep-related outcomes, including insomnia severity as measured by the insomnia severity index, sleep quality as measured by the Pittsburgh sleep quality index, total sleep time, sleep efficiency, sleep onset latency, wake after sleep onset and number of awakenings, in insomnia patients. Remote CBT-I intervention can also improve other health outcomes, including depression, anxiety, fatigue and mental health. Remote CBT-I is more effective when delivered in a shorter period on the internet without therapist support. In addition to the most widely used components, such as sleep restriction, stimulus control and cognitive restructure, other components, such as sleep hygiene, relaxation training and homework, showed positive effects and can be considered to be included in treatment design. More studies that include randomised controlled trials that have different designs are required in further studies to confirm the findings.
References
Abdelaziz, E. M., Elsharkawy, N. B., & Mohamed, S. M. (2022). Efficacy of internet-based cognitive behavioral therapy on sleeping difficulties in menopausal women: A randomized controlled trial. Perspectives in Psychiatric Care, 58(4), 1907–1917.
Ahorsu, D. K., Lin, C. Y., Imani, V., Carlbring, P., Nygårdh, A., Broström, A., et al. (2020). Testing an app-based intervention to improve insomnia in patients with epilepsy: A randomized controlled trial. Epilepsy & Behavior, 112, 107371.
Alimoradi, Z., Jafari, E., Broström, A., Ohayon, M. M., Lin, C.-Y., Griffiths, M. D., et al. (2022). Effects of cognitive behavioral therapy for insomnia (CBT-I) on quality of life: A systematic review and meta-analysis. Sleep Medicine Reviews, 64, 101646.
Arnedt, J. T., Conroy, D. A., Mooney, A., Furgal, A., Sen, A., & Eisenberg, D. (2021). Telemedicine versus face-to-face delivery of cognitive behavioral therapy for insomnia: A randomized controlled noninferiority trial. Sleep. https://doi.org/10.1093/sleep/zsaa136
Arnedt, J. T., Cuddihy, L., Swanson, L. M., Pickett, S., Aikens, J., & Chervin, R. D. (2013). Randomized controlled trial of telephone-delivered cognitive behavioral therapy for chronic insomnia. Sleep, 36(3), 353–362.
Association, A. P. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association.
Banks, S., & Dinges, D. F. (2007). Behavioral and physiological consequences of sleep restriction. Journal of Clinical Sleep Medicine., 3(5), 519–528.
Beck, A. T., Epstein, N., Brown, G., & Steer, R. A. (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56(6), 893–897.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck depression inventory (BDI-II). Pearson.
Beck, A. T., & Weishaar, M. (1989). Cognitive therapy (pp. 21–36). Springer.
Bieling, P. J., Antony, M. M., & Swinson, R. P. (1998). The State-Trait Anxiety Inventory, Trait version: Structure and content re-examined. Behaviour Research and Therapy., 36(7–8), 777–788.
Blom, K., Tarkian Tillgren, H., Wiklund, T., Danlycke, E., Forssén, M., Söderström, A., et al. (2015). Internet-vs. group-delivered cognitive behavior therapy for insomnia: A randomized controlled non-inferiority trial. Behaviour Research and Therapy, 70, 47–55.
Bootzin, R. R., Epstein, D., & Wood, J. M. (1991). Stimulus control instructions. Case studies in insomnia (pp. 19–28). Springer.
Brenes, G. A., Miller, M. E., Williamson, J. D., McCall, W. V., Knudson, M., & Stanley, M. A. (2012). A randomized controlled trial of telephone-delivered cognitive-behavioral therapy for late-life anxiety disorders. American Journal of Geriatric Psychiatry., 20(8), 707–716.
Buscemi, N., Vandermeer, B., Friesen, C., Bialy, L., Tubman, M., Ospina, M., et al. (2007). The efficacy and safety of drug treatments for chronic insomnia in adults: A meta-analysis of RCTs. Journal of General Internal Medicine., 22(9), 1335–1350.
Buysse, D. J. (2013). Insomnia. Jama., 309(7), 706–716.
Buysse, D. J., Reynolds, C. F., 3rd., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213.
Caldwell, J. A., Caldwell, J. L., Thompson, L. A., & Lieberman, H. R. (2019). Fatigue and its management in the workplace. Neuroscience and Biobehavioral Reviews, 96, 272–289.
Carpenter, J. K., Andrews, L. A., Witcraft, S. M., Powers, M. B., Smits, J. A. J., & Hofmann, S. G. (2018). Cognitive behavioral therapy for anxiety and related disorders: A meta-analysis of randomized placebo-controlled trials. Depression and Anxiety, 35(6), 502–514.
Cashin, A. G., & McAuley, J. H. (2020). Clinimetrics: Physiotherapy evidence database (PEDro) scale. Journal of Physiotherapy, 66(1), 59.
Chan, C. S., Wong, C. Y. F., Yu, B. Y. M., Hui, V. K. Y., Ho, F. Y. Y., & Cuijpers, P. (2023). Treating depression with a smartphone-delivered self-help cognitive behavioral therapy for insomnia: A parallel-group randomized controlled trial. Psychological Medicine, 53(5), 1799–1813.
Chapoutot, M., Peter-Derex, L., Schoendorff, B., Faivre, T., Bastuji, H., & Putois, B. (2021). Telehealth-delivered CBT-I programme enhanced by acceptance and commitment therapy for insomnia and hypnotic dependence: A pilot randomized controlled trial. Journal of Sleep Research, 30(1), e13199.
Cheng, P., Luik, A. I., Fellman-Couture, C., Peterson, E., Joseph, C. L. M., Tallent, G., et al. (2019). Efficacy of digital CBT for insomnia to reduce depression across demographic groups: A randomized trial. Psychological Medicine, 49(3), 491–500.
Chung, K. F., Lee, C. T., Yeung, W. F., Chan, M. S., Chung, E. W., & Lin, W. L. (2018). Sleep hygiene education as a treatment of insomnia: A systematic review and meta-analysis. Family Practice, 35(4), 365–375.
Cunningham, J. E. A., & Shapiro, C. M. (2018). Cognitive behavioural therapy for insomnia (CBT-I) to treat depression: A systematic review. Journal of Psychosomatic Research, 106, 1–12.
Daley, M., Morin, C. M., LeBlanc, M., Grégoire, J.-P., & Savard, J. (2009). The economic burden of insomnia: Direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep, 32(1), 55–64.
DerSimonian, R., & Kacker, R. (2007). Random-effects model for meta-analysis of clinical trials: An update. Contemporary Clinical Trials., 28(2), 105–114.
Dopheide, J. A. (2020). Insomnia overview: Epidemiology, pathophysiology, diagnosis and monitoring, and nonpharmacologic therapy. The American Journal of Managed Care, 26(4 Suppl), S76-s84.
Eaton, W. W., Smith, C., Ybarra, M., Muntaner, C., & Tien, A. (2004). Center for Epidemiologic Studies Depression Scale: Review and revision (CESD and CESD-R).
Espie, C. A., Kyle, S. D., Williams, C., Ong, J. C., Douglas, N. J., Hames, P., et al. (2012). A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep, 35(6), 769–781.
Fairburn, C. G., & Patel, V. (2017). The impact of digital technology on psychological treatments and their dissemination. Behaviour Research and Therapy, 88, 19–25.
Fang, H., Tu, S., Sheng, J., & Shao, A. (2019). Depression in sleep disturbance: A review on a bidirectional relationship, mechanisms and treatment. Journal of Cellular and Molecular Medicine, 23(4), 2324–2332.
Ferguson, C. J. (2009). An effect size primer: A guide for clinicians and researchers. Professional Psychology: Research and Practice, 40, 532–538.
Freeman, D., Sheaves, B., Goodwin, G. M., Yu, L. M., Nickless, A., Harrison, P. J., et al. (2017). The effects of improving sleep on mental health (OASIS): A randomised controlled trial with mediation analysis. Lancet Psychiatry, 4(10), 749–758.
Freeman, L. W., White, R., Ratcliff, C. G., Sutton, S., Stewart, M., Palmer, J. L., et al. (2015). A randomized trial comparing live and telemedicine deliveries of an imagery-based behavioral intervention for breast cancer survivors: Reducing symptoms and barriers to care. Psycho-Oncology, 24(8), 910–918.
Gao, Y., Ge, L., Liu, M., Niu, M., Chen, Y., Sun, Y., et al. (2022). Comparative efficacy and acceptability of cognitive behavioral therapy delivery formats for insomnia in adults: A systematic review and network meta-analysis. Sleep Medicine Reviews, 64, 101648.
Garcia, M. C., Kozasa, E. H., Tufik, S., Mello, L. E. A., & Hachul, H. (2018). The effects of mindfulness and relaxation training for insomnia (MRTI) on postmenopausal women: A pilot study. Menopause, 25(9), 992–1003.
Gieselmann, A., & Pietrowsky, R. (2019). The effects of brief chat-based and face-to-face psychotherapy for insomnia: A randomized waiting list controlled trial. Sleep Medicine, 61, 63–72.
Glozier, N., Christensen, H., Griffiths, K. M., Hickie, I. B., Naismith, S. L., Biddle, D., et al. (2019). Adjunctive Internet-delivered cognitive behavioural therapy for insomnia in men with depression: A randomised controlled trial. Australian and New Zealand Journal of Psychiatry, 53(4), 350–360.
Godzik, C., Crawford, S., & Ryan, E. (2021). Feasibility of an online cognitive behavioral therapy program to improve insomnia, mood, and quality of life in bereaved adults ages 55 and older. Geriatric Nursing, 42(1), 99–106.
González-Valero, G., Zurita-Ortega, F., Ubago-Jiménez, J. L., & Puertas-Molero, P. (2019). Use of meditation and cognitive behavioral therapies for the treatment of stress, depression and anxiety in students. A systematic review and meta-analysis. International Journal of Environment Research and Public Health, 16(22), 4394.
Guo, X., Zheng, L., Wang, J., Zhang, X., Zhang, X., Li, J., et al. (2013). Epidemiological evidence for the link between sleep duration and high blood pressure: A systematic review and meta-analysis. Sleep Medicine, 14(4), 324–332.
Hagatun, S., Vedaa, Ø., Nordgreen, T., Smith, O. R. F., Pallesen, S., Havik, O. E., et al. (2019). The short-term efficacy of an unguided internet-based cognitive-behavioral therapy for insomnia: A randomized controlled trial with a six-month nonrandomized follow-up. Behavioral Sleep Medicine, 17(2), 137–155.
Hale, D., & Marshall, K. (2019). Sleep and Sleep Hygiene. Home Healthcare Now, 37(4), 227.
Hall, J., Kellett, S., Berrios, R., Bains, M. K., & Scott, S. (2016). Efficacy of cognitive behavioral therapy for generalized anxiety disorder in older adults: Systematic review, meta-analysis, and meta-regression. The American Journal of Geriatric Psychiatry, 24(11), 1063–1073.
Hamilton, M. (1986). The Hamilton rating scale for depression (pp. 143–152). Springer.
Hasan, F., Tu, Y. K., Yang, C. M., James Gordon, C., Wu, D., Lee, H. C., et al. (2022). Comparative efficacy of digital cognitive behavioral therapy for insomnia: A systematic review and network meta-analysis. Sleep Medicine Reviews, 61, 101567.
Hayes-Skelton, S. A., & Lee, C. S. (2020). Decentering in mindfulness and cognitive restructuring for social anxiety: An experimental study of a potential common mechanism. Behavior Modification, 44(6), 817–840.
Hedges, L. V., & Olkin, I. (2014). Statistical methods for meta-analysis. Academic Press.
Higgins, J. P., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ, 327(7414), 557–560.
Hjelm, N. (2005). Benefits and drawbacks of telemedicine. Journal of Telemedicine and Telecare., 11(2), 60–70.
Ho, F. Y., Chung, K. F., Yeung, W. F., Ng, T. H., & Cheng, S. K. (2014). Weekly brief phone support in self-help cognitive behavioral therapy for insomnia disorder: Relevance to adherence and efficacy. Behaviour Research and Therapy, 63, 147–156.
Horsch, C. H., Lancee, J., Griffioen-Both, F., Spruit, S., Fitrianie, S., Neerincx, M. A., et al. (2017). Mobile phone-delivered cognitive behavioral therapy for insomnia: A randomized waitlist controlled trial. Journal of Medical Internet Research, 19(4), e70.
Huedo-Medina, T. B., Sánchez-Meca, J., Marín-Martínez, F., & Botella, J. (2006). Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychological Methods, 11(2), 193–206.
Hürlimann, P., Bodenmann, G., Riemann, D., & Weitkamp, K. (2023). Cognitive behavioural therapy to treat stress and insomnia: A randomized wait list-controlled trial of two online courses. Journal of Sleep Research, 32(4), e13874.
Jernelöv, S., Blom, K., Hentati Isacsson, N., Bjurner, P., Rosén, A., Kraepelien, M., et al. (2022). Very long-term outcome of cognitive behavioral therapy for insomnia: One- and ten-year follow-up of a randomized controlled trial. Cognitive Behaviour Therapy, 51(1), 72–88.
Jernelöv, S., Lekander, M., Blom, K., Rydh, S., Ljótsson, B., Axelsson, J., et al. (2012). Efficacy of a behavioral self-help treatment with or without therapist guidance for co-morbid and primary insomnia: A randomized controlled trial. BMC Psychiatry, 12, 5.
Kaldo, V., Jernelöv, S., Blom, K., Ljótsson, B., Brodin, M., Jörgensen, M., et al. (2015). Guided internet cognitive behavioral therapy for insomnia compared to a control treatment: A randomized trial. Behaviour Research and Therapy, 71, 90–100.
Kalmbach, D. A., Cheng, P., O’Brien, L. M., Swanson, L. M., Sangha, R., Sen, S., et al. (2020). A randomized controlled trial of digital cognitive behavioral therapy for insomnia in pregnant women. Sleep Medicine, 72, 82–92.
Karyotaki, E., Riper, H., Twisk, J., Hoogendoorn, A., Kleiboer, A., Mira, A., et al. (2017). Efficacy of self-guided internet-based cognitive behavioral therapy in the treatment of depressive symptoms: A meta-analysis of individual participant data. JAMA Psychiatry, 74(4), 351–359.
Khan, M. S., & Aouad, R. (2017). The effects of insomnia and sleep loss on cardiovascular disease. Sleep Medicine Clinics, 12(2), 167–177.
Koffel, E. A., Koffel, J. B., & Gehrman, P. R. (2015). A meta-analysis of group cognitive behavioral therapy for insomnia. Sleep Medicine Reviews, 19, 6–16.
Krupp, L. B., LaRocca, N. G., Muir-Nash, J., & Steinberg, A. D. (1989). The Fatigue Severity Scale: Application to patients with multiple sclerosis and systemic lupus erythematosus. Archives of Neurology, 46(10), 1121–1123.
Kyle, S. D., Espie, C. A., & Morgan, K. (2010). “… Not just a minor thing, it is something major, which stops you from functioning daily”: Quality of life and daytime functioning in insomnia. Behavioral Sleep Medicine., 8(3), 123–140.
Laloyaux, J., Pellegrini, N., Mourad, H., Bertrand, H., Domken, M.-A., Van der Linden, M., et al. (2013). Performance on a computerized shopping task significantly predicts real world functioning in persons diagnosed with bipolar disorder. Psychiatry Research, 210(2), 465–471.
Lancee, J., van Straten, A., Morina, N., Kaldo, V., & Kamphuis, J. H. (2016). Guided online or face-to-face cognitive behavioral treatment for insomnia: A randomized wait-list controlled trial. Sleep, 39(1), 183–191.
Larimer, M. E., Palmer, R. S., & Marlatt, G. A. (1999). Relapse prevention. An overview of Marlatt’s cognitive-behavioral model. Alcohol Research & Health, 23(2), 151–160.
Larzelere, M. M., & Wiseman, P. (2002). Anxiety, depression, and insomnia. Primary Care, 29(2), 339–360.
Lattie, E. G., Adkins, E. C., Winquist, N., Stiles-Shields, C., Wafford, Q. E., & Graham, A. K. (2019). Digital mental health interventions for depression, anxiety, and enhancement of psychological well-being among college students: Systematic review. Journal of Medical Internet Research, 21(7), e12869.
Lee, S., Oh, J. W., Park, K. M., Lee, S., & Lee, E. (2023). Digital cognitive behavioral therapy for insomnia on depression and anxiety: a systematic review and meta-analysis. NPJ Digital Medicine, 6(1), 52.
Leonardo, R. (2018). PICO: Model for clinical questions. Evidence Based Medicine and Practice, 3(115), 2.
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P., et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Journal of Clinical Epidemiology., 62(10), e1–e34.
Lin, L., & Chu, H. (2018). Quantifying publication bias in meta-analysis. Biometrics, 74(3), 785–794.
Lokman, S., Leone, S. S., Sommers-Spijkerman, M., van der Poel, A., Smit, F., & Boon, B. (2017). Complaint-directed mini-interventions for depressive complaints: A randomized controlled trial of unguided web-based self-help interventions. Journal of Medical Internet Research, 19(1), e4.
Lorenz, N., Heim, E., Roetger, A., Birrer, E., & Maercker, A. (2019). Randomized controlled trial to test the efficacy of an unguided online intervention with automated feedback for the treatment of insomnia. Behavioural and Cognitive Psychotherapy, 47(3), 287–302.
McCurry, S. M., Guthrie, K. A., Morin, C. M., Woods, N. F., Landis, C. A., Ensrud, K. E., et al. (2016). Telephone-based cognitive behavioral therapy for insomnia in perimenopausal and postmenopausal women with vasomotor symptoms A MsFLASH randomized clinical trial. JAMA Internal Medicine, 176(7), 913–920.
McCurry, S. M., Zhu, W., Von Korff, M., Wellman, R., Morin, C. M., Thakral, M., et al. (2021). Effect of telephone cognitive behavioral therapy for insomnia in older adults with osteoarthritis pain: a randomized clinical trial. JAMA Internal Medicine, 181(4), 530–538.
Medic, G., Wille, M., & Hemels, M. E. (2017). Short- and long-term health consequences of sleep disruption. Nature and Science Sleep, 9, 151–161.
Morin, C. M. (1993). Insomnia: Psychological assessment and management. Guilford Press.
Morin, C. M., & Espie, C. A. (2007). Insomnia: A clinical guide to assessment and treatment. Springer Science & Business Media.
Morin, C. M., Kowatch, R. A., Barry, T., & Walton, E. (1993). Cognitive-behavior therapy for late-life insomnia. Journal of Consulting and Clinical Psychology, 61(1), 137–146.
Morris, J., Firkins, A., Millings, A., Mohr, C., Redford, P., & Rowe, A. (2016). Internet-delivered cognitive behavior therapy for anxiety and insomnia in a higher education context. Anxiety Stress and Coping, 29(4), 415–431.
Muench, A., Vargas, I., Grandner, M. A., Ellis, J. G., Posner, D., Bastien, C. H., et al. (2022). We know CBT-I works, now what? Faculty Reviews, 11, 4.
Ohayon, M. M. (2002). Epidemiology of insomnia: What we know and what we still need to learn. Sleep Medicine Reviews, 6(2), 97–111.
Oswald, L. B., Morales-Cruz, J., Eisel, S. L., Del Rio, J., Hoogland, A. I., Ortiz-Rosado, V., et al. (2022). Pilot randomized controlled trial of eHealth cognitive-behavioral therapy for insomnia among Spanish-speaking breast cancer survivors. Journal of Behavioral Medicine, 45(3), 503–508.
Pardo Cebrián, R., & Calero, E. A. (2019). Applying cognitive restructuring in therapy: The clinical reality in Spain. Psychotherapy Research, 29(2), 198–212.
Perlis, M. L., Jungquist, C., Smith, M., & Posner, D. A. (2005). Cognitive behavioral treatment of insomnia: A session-by-session guide (pp. 1–182). Springer.
Qaseem, A., Kansagara, D., Forciea, M. A., Cooke, M., & Denberg, T. D. (2016). Management of chronic insomnia disorder in adults: A clinical practice guideline from the American College of Physicians. Annals of Internal Medicine, 165(2), 125–133.
Rajabi Majd, N., Broström, A., Ulander, M., Lin, C. Y., Griffiths, M. D., Imani, V., et al. (2020). Efficacy of a theory-based cognitive behavioral technique app-based intervention for patients with insomnia: randomized controlled trial. Journal of Medical Internet Research, 22(4), e15841.
Riemann, D. (2018). Sleep hygiene, insomnia and mental health. Journal of Sleep Research, 27(1), 3.
Riemann, D., Baglioni, C., Bassetti, C., Bjorvatn, B., Dolenc Groselj, L., Ellis, J. G., et al. (2017). European guideline for the diagnosis and treatment of insomnia. Journal of Sleep Research, 26(6), 675–700.
Ritterband, L. M., Thorndike, F. P., Gonder-Frederick, L. A., Magee, J. C., Bailey, E. T., Saylor, D. K., et al. (2009). Efficacy of an Internet-based behavioral intervention for adults with insomnia. Archives of General Psychiatry, 66(7), 692–698.
Ritterband, L. M., Thorndike, F. P., Ingersoll, K. S., Lord, H. R., Gonder-Frederick, L., Frederick, C., et al. (2017). Effect of a web-based cognitive behavior therapy for insomnia intervention with 1-year follow-up: A randomized clinical trial. JAMA Psychiatry, 74(1), 68–75.
Roth, T. (2007). Insomnia: Definition, prevalence, etiology, and consequences. Journal of Clinical Sleep Medicine, 3(5 Suppl), S7-10.
Salazar de Pablo, G., Pascual-Sánchez, A., Panchal, U., Clark, B., & Krebs, G. (2023). Efficacy of remotely-delivered cognitive behavioural therapy for obsessive-compulsive disorder: An updated meta-analysis of randomised controlled trials. Journal of Affective Disorders, 322, 289–299.
Sateia, M. J. (2014). International classification of sleep disorders-third edition: Highlights and modifications. Chest, 146(5), 1387–1394.
Sateia, M. J., & Buysse, D. (2016). Insomnia: Diagnosis and treatment. CRC Press.
Seyffert, M., Lagisetty, P., Landgraf, J., Chopra, V., Pfeiffer, P. N., Conte, M. L., et al. (2016). Internet-delivered cognitive behavioral therapy to treat insomnia: A systematic review and meta-analysis. PLoS One, 11(2), e0149139.
Siebmanns, S., Johansson, P., Ulander, M., Johansson, L., Andersson, G., & Broström, A. (2021). The effect of nurse-led Internet-based cognitive behavioural therapy for insomnia on patients with cardiovascular disease: A randomized controlled trial with 6-month follow-up. Nursing Open, 8(4), 1755–1768.
Simon, L., Steinmetz, L., Feige, B., Benz, F., Spiegelhalder, K., & Baumeister, H. (2023). Comparative efficacy of onsite, digital, and other settings for cognitive behavioral therapy for insomnia: A systematic review and network meta-analysis. Scientific Reports., 13(1), 1929.
Smets, E., Garssen, B., Bonke, B. D., & De Haes, J. (1995). The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. Journal of Psychosomatic Research, 39(3), 315–325.
Smith, M. T., Perlis, M. L., Park, A., Smith, M. S., Pennington, J., Giles, D. E., et al. (2002). Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. American Journal of Psychiatry., 159(1), 5–11.
Thorndike, F. P., Ritterband, L. M., Gonder-Frederick, L. A., Lord, H. R., Ingersoll, K. S., & Morin, C. M. (2013). A randomized controlled trial of an internet intervention for adults with insomnia: Effects on comorbid psychological and fatigue symptoms. Journal of Clinical Psychology, 69(10), 1078–1093.
Trauer, J. M., Qian, M. Y., Doyle, J. S., Rajaratnam, S. M., & Cunnington, D. (2015). Cognitive behavioral therapy for chronic insomnia: A systematic review and meta-analysis. Annals of Internal Medicine, 163(3), 191–204.
van der Zweerde, T., Bisdounis, L., Kyle, S. D., Lancee, J., & van Straten, A. (2019). Cognitive behavioral therapy for insomnia: A meta-analysis of long-term effects in controlled studies. Sleep Medicine Reviews, 48, 101208.
van der Zweerde, T., Bisdounis, L., Kyle, S. D., Lancee, J., & van Straten, A. (2019). Cognitive behavioral therapy for insomnia: A meta-analysis of long-term effects in controlled studies. Sleep Medicine Reviews, 48, 101208.
Van der Zweerde, T., Lancee, J., Slottje, P., Bosmans, J. E., Van Someren, E. J. W., & van Straten, A. (2020). Nurse-guided internet-delivered cognitive behavioral therapy for insomnia in general practice: results from a pragmatic randomized clinical trial. Psychotherapy and Psychosomatics, 89(3), 174–184.
van der Zweerde, T., van Straten, A., Effting, M., Kyle, S. D., & Lancee, J. (2019). Does online insomnia treatment reduce depressive symptoms? A randomized controlled trial in individuals with both insomnia and depressive symptoms. Psychological Medicine, 49(3), 501–509.
van Straten, A., Emmelkamp, J., de Wit, J., Lancee, J., Andersson, G., van Someren, E. J., et al. (2014). Guided Internet-delivered cognitive behavioural treatment for insomnia: A randomized trial. Psychological Medicine, 44(7), 1521–1532.
van Straten, A., van der Zweerde, T., Kleiboer, A., Cuijpers, P., Morin, C. M., & Lancee, J. (2018). Cognitive and behavioral therapies in the treatment of insomnia: A meta-analysis. Sleep Medicine Reviews, 38, 3–16.
Vedaa, Ø., Kallestad, H., Scott, J., Smith, O. R. F., Pallesen, S., Morken, G., et al. (2020). Effects of digital cognitive behavioural therapy for insomnia on insomnia severity: A large-scale randomised controlled trial. Lancet Digit Health., 2(8), e397–e406.
Verhagen, A. P., de Vet, H. C., de Bie, R. A., Kessels, A. G., Boers, M., Bouter, L. M., et al. (1998). The Delphi list: A criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. Journal of Clinical Epidemiology, 51(12), 1235–1241.
Vincent, N., & Lewycky, S. (2009). Logging on for better sleep: RCT of the effectiveness of online treatment for insomnia. Sleep, 32(6), 807–815.
Ware, J. E. (1994). New England Medical Center H, Health I. SF-36 physical and mental health summary scales: a user’s manual. Health Institute, New England Medical Center.
Wootton, R. (2001). Telemedicine. BMJ, 323(7312), 557–560.
Wootton, R., Craig, J., & Patterson, V. (2017). Introduction to telemedicine. CRC Press.
Yesavage, J. A. (1988). Geriatric depression scale. Psychopharmacology Bulletin, 24(4), 709–711.
Yeung, K., Zhu, W., McCurry, S. M., Von Korff, M., Wellman, R., Morin, C. M., et al. (2022). Cost-effectiveness of telephone cognitive behavioral therapy for osteoarthritis-related insomnia. Journal of the American Geriatrics Society, 70(1), 188–199.
Zachariae, R., Amidi, A., Damholdt, M. F., Clausen, C. D. R., Dahlgaard, J., Lord, H., et al. (2018). Internet-delivered cognitive-behavioral therapy for insomnia in breast cancer survivors: A randomized controlled trial. Journal of the National Cancer Institute, 110(8), 880–887.
Zachariae, R., Lyby, M. S., Ritterband, L. M., & O’Toole, M. S. (2016). Efficacy of internet-delivered cognitive-behavioral therapy for insomnia: A systematic review and meta-analysis of randomized controlled trials. Sleep Medicine Reviews, 30, 1–10.
Zhang, C., Liu, Y., Guo, X., Liu, Y., Shen, Y., & Ma, J. (2023). Digital cognitive behavioral therapy for insomnia using a smartphone application in China: A pilot randomized clinical trial. JAMA Network Open, 6(3), e234866.
Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370.
Zung, W. W. (1965). A self-rating depression scale. Archives of General Psychiatry, 12(1), 63–70.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. First author was supported by Australia Postgradaute Scholarship and Griffith University scholarship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dawei Xu, Zhanjiang Li, Unnah Leitner and Jing Sun have completed the Unified Competing Interest form and declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (national and institutional). Informed consent was obtained from all individual subjects participating in the study. Additional informed consent was obtained from any subjects for whom identifying information appears in this paper.
Animal Rights
No animal studies were carried out by the authors for this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10608_2023_10458_MOESM1_ESM.tiff
Supplementary Figure 1. Funnel plots for sleep outcomes. (A) Insomnia Severity Index; (B) Pittsburgh Sleep Quality Index; (C) Total sleep time; (D) Sleep efficiency; (E) Sleep onset latency; (F) Wake after sleep onset. (TIFF 15089 kb)
10608_2023_10458_MOESM2_ESM.tiff
Supplementary Figure 2. Funnel plots for sleep and health outcomes. (A) Number of awakenings; (B) Depression; (C) Anxiety; (D) Fatigue; (E) Physical health; (F) Mental health (TIFF 15089 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, D., Li, Z., Leitner, U. et al. Efficacy of Remote Cognitive Behavioural Therapy for Insomnia in Improving Health Status of Patients with Insomnia Symptoms: A Meta-analysis. Cogn Ther Res 48, 177–211 (2024). https://doi.org/10.1007/s10608-023-10458-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10608-023-10458-6