Abstract
In Participatory Design (PD), the design of a cooperative digital solution should involve all stakeholders in the co-design. When one stakeholder’s position is weaker due to socio-cultural structures or differences in knowledge or abilities, PD methods should help designers balance the power in the design process at both the macro and micro levels. We present a PD method that addresses the power relations arising during the design process and draws on theories about participation and power in the design and organisation of change processes. We contribute to Computer Supported Cooperative Work (CSCW) by using the PD method to design computer support for cooperation on cognitive rehabilitation between people with Mild Acquired Brain Injuries (MACI) and their healthcare professionals, where strengthening the cooperation is considered an element of patient empowerment. This method is presented as a contribution to the intersection between PD and CSCW. The discussion of power in PD contributes to the discussion of cooperation in CSCW. We found that EquiP supported the creation of choices, and hence the ‘power to’ influence the design. This method can contribute to a power ‘equilibrium’ and a positive-sum power relation in PD sessions involving all stakeholders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
In this paper, we present a method of co-design for cooperation that addresses power imbalances among the cooperating parties in the co-design sessions for technologies that will support their cooperation. The method is theoretically grounded in the fields of Participatory Design (PD) and Computer Supported Cooperative Work (CSCW) and addresses what we define as ‘micro-power’ relations in a co-design for cooperation sessions.
CSCW is relevant in today’s societies in view of the increasing specialisation of professional work, making cooperation between parties necessary in order to offer a complete service or product. Moreover, co-design as the practice of PD aimed at the involvement of users in co-designing technologies that influence them (Schuler and Namioka, 1993; Simonsen and Robertson, 2012) has been applied since the 1970s in a wide range of contexts aiming to include new, previously marginalised user groups. While addressing power imbalances in design stands at the core of PD, power imbalances are present in every cooperative relation. These power imbalances may be influenced by differences in knowledge and abilities, or in established social structures that influence cooperative relations. Power structures exist in any cooperative relationship. They vary from one context to another and over time within the context.
We report on a project in which we applied and tested the method in rehabilitation practice, to design a cooperative tool for people with Mild Acquired Brain Injuries (MACI) and their healthcare professionals during cognitive rehabilitation. Cognitive rehabilitation is a programme offered to people with an Acquired Brain Injury (ABI) who suffer from cognitive impairment. In the case we report, the rehabilitation programme is offered in a rehabilitation hospital where the person with cognitive impairment (from the ABI) is a patient. Our method aimed to strengthen MACI patients’ influence on this cooperative tool’s design process, strengthening their power over their own rehabilitation and promoting a more cooperative relationship between the patients and their healthcare providers.
The paper is structured as follows: We start by presenting the theoretical foundation for the method, give an overview of CSCW research in healthcare, and discuss power in relation to PD. The next section presents the method and provides the rationale for it. After presenting the elements of the method, the paper reports on how the method has been applied and evaluated in practice in cognitive rehabilitation. To evaluate the method, we analysed how decisions were made in the design process and what and who influenced the decisions. Based on the decision-making journey for the final design decisions, we analysed the power relations among the stakeholders in the PD sessions. The last section discusses how the method has contributed to balancing power in the PD process.
2 Theoretical background
In this section, to better position our method, we initially present PD and CSCW as research fields and focus on their interconnections. The most relevant concept in our paper is power. We thus present a review of the discourse on power in PD. As we have applied the method in a healthcare context, we present an overview of the design for cooperation in healthcare. We conclude the section with knowledge about the challenges of people with MACI and how to involve them in PD.
2.1 PD and CSCW and their perspectives
PD is a design approach concerned with the involvement of future users in the co-design of technologies intended for them (Schuler and Namioka, 1993; Simonsen and Robertson, 2012). In this paper, we focus on equalising power relations and democratic practices (Greenbaum and Kensing, 2012). Users should not only ‘have a voice’ in the decision-making regarding technologies designed for them, but should also influence the outcome. They should ‘have a say’ (Bratteteig et al., 2012). This is made possible by adopting different methods and techniques that promote genuine participation. In recent years, PD researchers have expanded their focus to more marginalised user groups, investigating tools and techniques to include these groups in the design process. CSCW is concerned with understanding cooperative work in groups and designing adequate computer support for this cooperation. Schmidt and Bannon (1992, p. 11) state that CSCW is ‘a design oriented research area’. However, they also add that ‘by virtue of its commitment to support cooperative work, CSCW should not be defined in terms of the techniques being applied’ (p.10).
PD has also been used to design technologies that support cooperative work (Bratteteig and Wagner, 2016), and PD techniques have been applied to CSCW to understand current cooperative work practices and to design better computer-based solutions (ibid).
While CSCW can make use of PD design methods and adapt them to contribute to the design of digital solutions for cooperative work, PD can also learn from CSCW about the understanding of cooperative work to improve cooperation among the stakeholders involved during design (Kensing and Blomberg, 1998).
Despite cooperation, there are also other aspects of the work that are relevant to consider, such as power conflicts and control (Kyng, 1991). Power issues do not receive much attention in CSCW. Suchman’s (1993) paper ‘Do categories have politics?’, in which she considers the normative imposition of categories by some actors as acts of power, has brought attention to power issues in CSCW. Similarly, Star and Strauss (1999) discuss the relations between power and invisible work. These examples discuss power issues in the workplace and their influence on cooperation, but they do not specifically discuss how power imbalances and power issues would influence a design process in which all parties to the cooperative relationship are involved.
The work of Bratteteig and Wagner (Bratteteig and Wagner, 2012, 2014, 2016) contributes to conceptualising the details of work practices in terms of ‘power’ within PD and CSCW. They present a decision-making framework to analyse participation in PD and take their analysis further by discussing the issues of sharing power and their influence on decision-making.
PD has also been applied to the design of CSCW artifacts (Karasti, 2001; Kinnula et al., 2017; McPhail et al., 1998) and power issues have also been discussed and conceptualised in CSCW research. Yet no attempt has been made to develop a method that is positioned in the power discussions relevant for PD and which is aimed specifically at the design of digital solutions that support cooperative work. Moreover, there is a lack of research of CSCW that considers cooperative work from an empowerment perspective and as a space in which power issues need to be problematised, negotiated and balanced. It is in this common research space between PD and CSCW that the method presented in this paper has a contribution to make.
2.2 Power
Power is a relevant concept in PD, and this paper adheres to the PD principle of balancing power. We focus on power, participation and decision-making in PD by drawing on theoretical studies of power in PD and selected literature that has shaped the power discourse in the field. At the core of this paper are the power relations present in a co-design session, the movement of the design ideas to a design result, and the influence of decision-making participants in the moment-to-moment design process. We thus focus specifically on the studies of power in PD that theorised the design idea’s lifecycle and discussed the power imbalances present during the design idea’s lifecycle. Furthermore, we emphasise the studies concerned with power imbalances in PD within different participant groups, and not only one group, and the relation with the designer.
The most common understanding of power is ‘power as domination’, which is largely characterised as ‘power over’ (Haugaard, 2012). Power as domination is often defined as the power of getting someone to do something that they would not otherwise do (Dahl, 1957) and is associated with zero-sum power, where the empowerment of one group entails diminishing power for another group. Another common meaning of power is as empowerment, which is frequently theorised as the ‘power to’ (Bratteteig and Wagner, 2012, 2014; Pitkin, 1993). Power as empowerment is referred to as positive-sum power, in which one party does not gain at the expense of the other. Rather, the power of both is expanded. ‘Power to’ denotes capacity, potential, ability or wherewithal (Pitkin, 1993), and the agency and capacity to shape action, which is partly influenced by access to organisational resources or power/knowledge in a Foucauldian sense.
Both ‘power over’ and ‘power to’ occur in a PD project, and often together (Joshi and Bratteteig, 2016). Power in PD is the ability to contribute (power to), but the ability to act often depends on power over resources, as well as the relational aspect of any kind of power (power over). Having the opportunity to contribute and share power with other participants in the design process involves both aspects, which need to be examined. When PD processes aim to have the participants move to achieve common ends, the power games differ from conflict-oriented PD processes (Bratteteig and Wagner, 2014) and are more in line with positive-sum power (Haugaard, 2012) or ‘power with’ (Bratteteig and Wagner, 2014). We also note that power can occur in the form of influence, trust and loyalty, in particular when there are differences between the stakeholders’ power/knowledge (Bratteteig and Wagner, 2012, 2014; Bratteteig et al., 2016). The concept of empowerment is also used in the power discourse in PD. Although it is often used to characterise the level of participation, rather than what the participation is about or how it is achieved (Bratteteig and Wagner, 2012). Although paternalism is discussed as a potential power game in PD, there are also discussions about stakeholders with a lack of knowledge to represent their own interests themselves (Vines et al., 2013, 2014; Dæhlen, 2019; Maartmann-Moe, 2019). Haugaard (2012) notes that ‘power over’ does not imply a difference in interest and that actors can prevail over others in ways that may be beneficial to those who are being prevailed over, called ‘benign paternalism,’ entailing concerted power, which is a positive-sum power. Thaler and Sunstein (2009) suggest the label of ‘libertarian paternalisms’ and the concept of ‘nudge’ to describe a choice architecture has designed for benign paternalism, in which the nudge is used as an incentive for changing behaviour. This will promote health, happiness and well-being when the person nudged may not have a full overview of the choices or their consequences.
Analysing power relations at the level of the PD project (Bratteteig and Wagner, 2012, 2014) is very relevant for defining the course of the project. However, there are also power games played among the actors in situ, when different stakeholders come together in a PD session, a workshop or a focus group. It is relevant to distinguish small, situated, moment-to-moment power exercises during PD sessions from decision-making influence at the project level. Capturing what happens at the detailed level of interaction between people in PD sessions and in cooperative interaction has been described by Spiel et al. (2018) as micro-ethics looking at the ethically charged small in-situ decisions that shape the relationship, as well as the resulting design work. In their special issue discussing the politics of PD, Huybrechts et al., (2020) refer to the politics associated with the interactions in PD sessions as micro-politics, as distinguished from politics on the ‘big issues’ at the macro level. In a cooperative work setting, Luff and Heath (1998) coin the concept of ‘micro-mobility’ to emphasise the relevance of a moment-to-moment, detailed use of medical paper documents.
Inspired by these studies, we will use the term ‘micro-power’ for the moment-to-moment power game in a PD session among different stakeholders as the assumed democratic discussion unfolds. PD researchers in workshops or focus groups need to balance these micro-power relations to achieve the PD principle of a democratic practice in which all are represented in the final design. The micro-power relations are influenced by the macro powers created due to differences in people’s abilities or knowledge, or as a consequence of institutionalism and social constructions. Micro-power is present in every interaction in our lives and changes from one context to another, and even in time within a context. The micro-power relations are at the core of our method. By studying, understanding and equilibrating the micro-power relations, PD can contribute to the macro-power dynamics in societies.
As stated earlier, power imbalances have been discussed by looking at the decision-making process and at which of the actors involved have influenced the decisions made (Bratteteig and Wagner, 2014). To have a balanced outcome, the aim is for all stakeholders and their views to be represented in the final design. Bratteteig and Wagner (2012, 2014, 2016) Bratteteig et al. (2016) draw on Schön (1984) Schön and Wiggins, (1992) who described design as sequences of seeing-moving-seeing, and Schütz (1951) who described how we imagine possible futures in our minds. To discuss what users participate in, they describe design as decision-making concerned with four steps: 1) the creation of possibilities, design ideas or choices; 2) the selection of which design idea to explore; 3) how to form and shape the idea; and 4) evaluation of the idea. In line with Schön (1984), Bratteteig et al. (2016) define a design idea as conceptual expressions of ‘what could be in the future’ that emerge in conversations with the material of the situation and are inspired by engagement with different materials. However, design ideas must be represented for others to appreciate or critically evaluate them. They need to be supported by a representation to ‘survive’ and become part of the final design result. Here, a representation can be a physical or visual representation, such as a sketch or an oral confirmation by another participant. Design ideas represented visually in the situation have a better chance of being included in the final design result.
Bratteteig et al. (2016) distinguish between four stages of a design idea, from initial conception to a concretely formed design result: 1) a statement, 2) an idea, 3) a representation, and 4) a design result. A statement supported by more than one person becomes an idea because a confirmation serves as a representation that enables the idea to be shared and supported by others. A confirmation or physical representation or form has to be recognised as an idea by others. Strong support in the form of a positive evaluation (step 4 above) makes the design process move on, and the design idea will be part of the design result.
Both the four steps of the design process and the four stages of a design idea require ‘power to’. However, the selection and evaluation of ideas also seem to rely on ‘power over’ or domination of other ideas. ‘Power to’ refers to the ability to generate statements, argue for the ideas in a group, and represent the design ideas. The power in a PD session resides in the ability to move a statement to the final design decision. However, the journey of a statement is long, and factors such as the ability to articulate or represent one’s own ideas can diminish the chances of a statement from one person becoming part of the design results. A person who already has a set of design ideas is better prepared to argue and gain support from other stakeholders in the PD session, according to Bratteteig et al. (2016).
A strong factor influencing micro-power relations in PD relates to the organisation of the PD process. PD researchers have presented different ways of facilitating user participation (Bratteteig et al., 2012; Joshi and Bratteteig, 2016). Moreover, different methods and techniques have been described in the literature. Techniques and tools are relevant for supporting democratic practices and contributing to balancing power (Greenbaum and Kensing, 2012).
2.3 Cooperative digital solutions in healthcare
The healthcare sector has benefited from both CSCW research and PD practices in designing digital solutions that promote cooperation. The design of electronic patient records (EPRs) that support the coordination of work between clinicians has been studied extensively in CSCW (Fitzpatrick and Ellingsen, 2013) settings, such as radiology departments (Tellioğlu and Wagner, 2001), surgical intensive care units (Reddy et al., 2006), emergency departments (Bjørn and Hertzum, 2011) and hospital wards (Bossen, 2002; Bardram and Bossen, 2005; Cabitza et al., 2005). Such studies, focused on the work of healthcare professionals, have, in our view, contributed to delivering better care, but have also supported the existing model of care, in which the healthcare professionals have control over the care process, thereby institutionalising the underlying power structures. However, there is an ongoing discourse on a paradigm shift in healthcare – from a paternalistic culture, where the doctor takes care of the patient, to an equal-level partnership, in which both doctor and patient contribute to the care process (Meskó et al., 2017).
Technology is seen as an enabler of this paradigm shift (Palumbo, 2017). Different digital healthcare solutions have emerged in the pursuit of patient involvement as a partner in the care process. Piras and Zanutto (2010) talked about shared artifacts with patients in 2010. Fitzpatrick and Ellingsen (2013) discuss patient-care professionals’ cooperative digital solutions when they review healthcare at home or care in new development contexts. Some of this work is more at the stage of design exploration through design workshops and conceptual prototypes, such as in Christensen and Grönvall (2011) for home care of older adults, and Bagalkot and Sokoler (2011) for stroke rehabilitation. Cooperative digital solutions have mostly been studied for patients with chronic conditions and their healthcare professionals (Sokoler et al., 2007; Consolvo et al., 2008; Larsen and Bardram, 2008; Mamykina et al., 2008; Balaam et al., 2011).
While the research to design cooperative digital solutions to be used by patients and their healthcare professionals has been ongoing for more than a decade, there has been less focus on the methods and techniques used to design these solutions. Taking a PD approach in the design process has been deemed adequate in previous research, because it would allow both patients and healthcare professionals to participate in the design process. PD practices and concern about political issues have promoted the increasing involvement of patients in hospitals and ill people in general at home, in their communities, and many digital solutions that comply with people’s needs have been developed. Andersen (2010) introduces the ‘participant patient’ concept, referring to the patient’s dual enactment of participation in PD projects in healthcare and bringing attention to the patient’s contribution not only in the design, but also in the negotiation of cooperative processes.
We deem the application of PD practices to the design of cooperative digital solutions between patients and healthcare professionals to be relevant. This is due not only to the principle of the democratic practice of PD, but also the equalising power relations principle on which we focus, particularly in the method described in this paper.
PD in the context of healthcare normally involves patients and healthcare professionals separately in the design. When they are involved together, healthcare professionals, or the network of people supporting the person, have mostly taken on the role of consultant or supporter of the patient during the PD sessions. This is particularly common for people with cognitive impairments or differences in cognitive abilities (O'Connor et al., 2006; Plaisant et al., 2006; Dawe, 2007; Wu et al., 2010; Balaam et al., 2011; Lindsay et al., 2012a; Muriana and Hornung, 2017). In other cases, healthcare professionals have taken on the role of patients’ proxies in PD (Colonius et al., 2010; Galliers et al., 2012; Borges et al., 2013). In these cases, the patients’ contributions have been less significant, and their voices less heard, and they have not co-designed as equals with healthcare professionals (Joshi and Bratteteig, 2016). Consideration of how to involve patients and healthcare professionals in co-designing for cooperative digital solutions and how to empower patients in the co-design process in healthcare can therefore inspire better future solutions in the health and well-being context. This is relevant to creating an opportunity for patients to become significant actors in their own care and empowerment.
2.4 MACI people and their involvement in PD
Cognition is defined as an individual’s capacity to acquire and use information to adapt to environmental demands (Toglia, 2003). Cognitive impairment can be the consequence of an acquired brain injury (ABI) or may be associated with cognitive decline, due to normal aging, or with a more serious decline as dementia. In this paper, we focus on people with ABI stemming from a traumatic brain injury (e.g. an accident), or a non-traumatic brain injury (e.g. stroke), affecting cognitive, physical, emotional, social or independent functioning (Turner-Stokes, 2008). Cognitive impairment often persists after ABI and can significantly affect an individual’s abilities to perform everyday tasks, fill former roles, and maintain personal-social relationships (Prigatano, 1999; Toglia, 2005; Krogstad, 2011; Nilsson et al., 2011). However, the consequences vary from mild to severe.
We have developed and applied EquiP for designing together with MACI people and their care providers. MACI people are ‘a subgroup of patients with mild cognitive impairment(s) (MCI) who are expected to reach a stable cognitive level over time. These people have acquired MCI from a head injury or mild stroke’ (Eghdam et al., 2012, p.1). In our study, we involved adult MACI people who have a chance of a stable state after an acquired brain injury (ABI) and can restore functions or cope with their current situation through rehabilitation.
MACI people can have symptoms such as reduced capacity, memory problems, attention and concentration problems, reduced speed of activity, reduced multitasking capacity, problems with starting or initiating something, difficulty in making mental changes from one topic to another, a tendency to think specifically, problems with using language and communicating, and difficulties in processing information (Haskins et al., 2012). The number of MACI people is increasing, due to a higher number of people surviving a stroke or accident.
Involving MACI people in PD workshops requires special consideration. In PD, extensive research has been conducted in user groups with more severe cognitive impairments. For example, dementia (Hendriks et al., 2013), aphasia (McGrenere et al., 2002), amnesia (Wu et al., 2004), children with autism spectrum (Herstad and Holone, 2012), and older adults (Joshi and Bratteteig, 2016; Bråthen et al., 2019), and less focus has been given to MACI patients (Çarçani and Holone, 2019), despite the challenges they face in everyday life.
Due to similarities in symptoms, involving MACI patients in PD presents similar challenges to older adults or people with dementia, amnesia or aphasia. These user groups struggle with abstract thinking (Galliers et al., 2012; Kane et al., 2012; Muriana and Hornung, 2017; Dæhlen and Joshi, 2019) and the ability to envision future solutions (Massimi et al., 2007; Lindsay et al., 2012a, b; Mayer and Zach, 2013; Branco et al., 2016; Maartmann-Moe, 2019). Including structure and review in PD sessions is considered useful for these user groups (Wu et al., 2004; Massimi et al., 2007; Frennert et al., 2012; Lindsay et al., 2012a; Muriana and Hornung, 2017). Support through prompts or visual cues has also been described as enhancing active participation and facilitating the envisioning of future solutions (Galliers et al., 2012; Hendriks et al., 2013; Mayer and Zach, 2013; Orso et al., 2015; Muriana and Hornung, 2017). Other researchers have emphasised the relevance of building on personal experience (Frennert et al., 2012; Galliers et al., 2012; Lindsay et al., 2012b; Hendriks et al., 2013; Orso et al., 2015; Talamo et al., 2017). Involving people with cognitive impairment in PD sessions also requires consideration of the fidelity of the prototype designed and the tools involved. In most cases, paper prototypes and tools have been used, and in fewer cases, researchers have involved this category of users in medium-level (Wu et al., 2005) or high-level prototyping. However, there has recently been an increased interest in involving people with cognition challenges in co-development and exploration with tangible solutions (Herstad and Holone, 2012).
3 EquiP: designing cooperative solutions
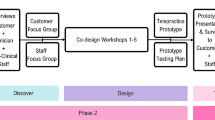
Drawing on the literature previously presented, we have developed Equilibria Power (EquiP), a PD method to use in the collaborative design of cooperative digital solutions. The method aims to contribute to an equilibrium (‘Equilibria’) of ‘power’ imbalances among the stakeholders, as argued above, by equilibrating the chances of generating design ideas and influencing design decisions. This equilibrium can be achieved by alternating the situated discussion during co-design among different stakeholders. Instead of imposing rules, we use a nudge approach to contribute to maintaining a normal flow of conversation without limiting options. Moreover, the method is presented as a set of principles that should be considered in the three phases of the method. It is necessary to tailor the method to the project in hand. Figure 1 presents a summary of the principles relevant to each step of the method, and each of the steps is presented in detail in Sub-Sections 3.1, 3.2, and 3.3.
EquiP builds on the lifecycle of a design idea from Bratteteig et al. (2016). The theoretical basis for the method consists of splitting the lifecycle of design ideas towards design decisions into three parts distributed in each phase of the method:
-
Generation of design statements and their initial representation by the designer/researcher, who takes the perspective of each end-user group who are to use the digital tool for cooperation. The statements aim to remind users of the crucial cooperation moments that can spark discussion.
-
PD sessions with parallel horizontal groups (people that belong to the same user group) to move statements to design ideas.
-
PD sessions with vertical groups (compounded by people who belong to different user groups who will use the digital solution for their cooperation) to bring design ideas to the representation of the final design outcomes.
The horizontal and vertical group labels were inspired by the structure of what is called the search conference method (Thoresen, 1993; Emery and Purser, 1996). This is a method to create change in organisations through democratic dialogue (Gustavsen, 1985). The idea is to bring together groups of employees who do not normally sit together, to establish a shared goal and more flexible channels of communication.
Bratteteig et al. (2016) also found that the ability to create representation influenced the power dynamics in the co-design sessions. Facilitating users with the representation of ideas can thus contribute to flattening power imbalances.
The method targets the design of technologies that support cooperation between users with differences in power, driven by differences in knowledge or abilities, or due to the existing social structure to which they belong. All user groups in the cooperation can represent themselves in cooperative work and co-design. As stated above, the method targets the design of technologies that support cooperative work, as defined in CSCW, where people are interdependent at work. Cases where a user group cannot represent themselves in the cooperative workspace and, consequently, in the co-design process, lie beyond the method’s scope.
In the following sections, we list recommendations for applying the method by describing the main principles to consider in each phase. The Start phase can only be completed when the next two phases’ aim and how-to have been understood. We therefore recommend reading all the steps and returning to the Start phase.
3.1 Start: Building insight and generating statement representations
Aim
To understand existing cooperative practices and power tensions in the specific context of enquiry. Use the understanding to generate, for each participant group, cue design statements that will contribute to the discussion of future solutions to enhance the cooperation for each stakeholder group. Define design statement representation options that are adapted to the representation abilities of the most vulnerable group involved in the cooperative relationship. Plan the Move and Land phases by a) considering the aim and how-to of each step as described below, b) considering the representation options, and c) co-creating how the representations can change in the two subsequent phases of the method towards the aimed outcome of the method. Finally, create representations and all the tools necessary for each of the subsequent phases of the method.
How
The PD researcher or designer managing a PD project should initially create in-depth knowledge of the current cooperative processes that will be influenced by the design of the new technology. Hence, a) map the main stakeholders that will be influenced by the design; b) investigate the power dynamics between stakeholders by considering structural power, differences in knowledge, and differences in abilities to generate ideas and represent them; c) investigate the cooperation process; d) map the key points for cooperation in the process for each group involved in the cooperation; and e) define possible representation options adapted to the abilities of the weakest group. Then the PD researcher or designer, in cooperation with domain experts, should generate statements for each cooperative user group, based on the steps of the cooperation process mapped in d) above. Finally, based on the knowledge mapped in b) and e), co-create representations for the Move and Land phases based on their aim and how-to.
Techniques
To map stakeholders, their cooperative activities and power dynamics, we recommend using ethnographic methods, which have been found to contribute to better technology design (Blomberg and Karasti, 2012). The knowledge gained through ethnographic methods should be used as a resource to generate statements and representations for the Move and Land phase of the method. Hence, ethnographic investigations not only aim at ‘understanding’ the current cooperation, but also provide material that can be explored (by the design team) in search of design openings in the later phases. Future opportunities can be found in existing practices. Starting from existing practices will provide a ‘creative resistance’ that challenges participants to envision possible futures that are different from, but still an extension of, existing practices.
The PD researcher or designer should plan the two subsequent phases in close collaboration with experts who deeply understand the current domain practices. We call these people ‘domain experts’, as persons with an overview of the process and an overall understanding of the needs of different stakeholders. The knowledge that the PD researcher or designer acquires during the ethnographic study supplements the domain expert’s knowledge by adjoining a) critical thinking of the cooperation process; b) pledging to a democratic process and balance of power; and c) making invisible/tacit knowledge visible/expressed. In the current cooperation process, both types of expertise should be used to generate statements and representations that will bring different parts of the existing cooperative process to the participants’ attention, enabling discussion and reconceptualization of the cooperation.
Considerations
PD researchers or designers should be aware of the risk associated with generating statements and their influence on the outcome. To mitigate the risk, we suggest using metonymic sentences. Gibbs (1999) states that ‘a metonymic sentence can serve as a script header which, when stated, will recall in people’s minds what the script was about’, as a nudge to enable people to envision future solutions. The metonymic structure of a sentence can help to draw attention to and highlight different events, places, times and people. It aims to guarantee that the researchers’ ideas are not influencing the outcome, but enabling participants’ awareness in the cooperation process.
Representation, as stated above, should be adapted to the abilities of the weakest group in the cooperation. In our method, we use the term EquiP representations. We define EquiP representations as ‘a tangible probing of statements which, based on knowledge of the representation abilities (limitations) of each stakeholder in the cooperation, will be ideated and designed by the PD researcher(s) or designer(s) in collaboration with domain experts, to match the abilities of the group that has the most limited representation abilities’. This ensures that groups with higher representation abilities do not dominate the design space. EquiP representations should be ideated to a) contribute to the generation of design ideas; b) be transformed to support the creation of new ideas; c) be easily transferred from Move to Land; d) be further transformed during the Land phase; and e) be represented in the outcome of the method in its new, transformed shape. Such consideration of the transformation of representations is relevant to maintain the power equilibrium of the representation abilities by allowing the weakest group in representations to take their ideas and design decisions to design outcomes.
3.2 Move: Horizontal groups and the ‘move’ to design ideas
Aim
Move the statements represented as EquiP representations to design ideas for each cooperating stakeholder group by enabling the generation and selection of design ideas that the group endorses as in the Land phase. Refine the initial representation of the design ideas by adapting, changing and adding the EquiP representations as part of selecting and evaluating choices (Bratteteig et al., 2016).
How
Organise parallel PD sessions where representatives of each stakeholder group generate design ideas relevant to the group. Based on the search conference terminology (Emery and Purser, 1996), we use the term horizontal groups. A horizontal group will be created for each stakeholder group relevant to the cooperation. In each PD session, participants should be involved in generating design ideas and corresponding representations. To do so, the PD researcher or designer should facilitate activities that use the statement as a starting point to a) enhance future envisioning by facilitating the ideation process; and b) move the abstract thinking into representations by providing instructions on options for how to change the EquiP representations to visualise the new design ideas. While the individual process of seeing-moving-seeing in Schön and Wiggins (1992) is relevant, the PD researcher or designer should plan activities that enable collective seeing-moving-seeing of design ideas and their representations. Hence, the PD researcher or designer should facilitate activities that encourage group discussion and selection of design ideas and co-design of representations.
Techniques
The techniques chosen for this phase should initially account for individual engagement with the statement and the EquiP representations. Furthermore, each participant should be encouraged to share individual ideas by giving the same space to everyone to articulate and represent their ideas. Then the group should be challenged to select a limited number of design ideas and representations as a group. This will allow for discussion ideas with one another, changing the EquiP representations, and building a set of design ideas that have emerged from the group and are jointly supported.
Tools
There are two main requirements in this part of the method. First, tools should be adapted to the EquiP representations and to how the representations will be transformed during the move of statements to design ideas. Second, tools should be adapted to the abilities of people with cognitive impairments and should be the same across all the horizontal groups, to promote the sense of equality.
Considerations
In these sessions, group thinking can prevail (Geuens et al., 2018), and people’s individual ideas can be suppressed. The PD researcher, designer and domain experts involved in planning the session structure and tasks should be the facilitators for each parallel session. The planning of the activities should guarantee that each participant has the space and the chance to have a say. The structure of the session should contribute to the equilibration of powers. The involvement of the facilitator(s) during the sessions is solely to explain the activities and support the group to stay focused on the aim of the activity.
3.3 Land: Vertical groups and implementing design ideas in a prototype
Aim
Move design ideas towards the design results (Bratteteig et al., 2016).
How
Participants belonging to the same horizontal group and working together in the Move phase should be distributed in new groups, compounded by representatives from each stakeholder group involved in cooperation. In line with the search conference terminology, these are called vertical groups. The number of participants from each stakeholder group in the vertical groups should be balanced to enable democratic discussion (Emery and Purser, 1996). Participants in a vertical group should bring with them the latest EquiP representations of the design ideas selected as the most relevant by a specific horizontal group. The facilitator(s) should support the smooth transition of the representations from one physical space to another. Participants will be instructed by the facilitator(s) to present the vertical group with their design ideas and the respective EquiP representations. Finally, the group will be instructed to discuss each of the design ideas and to ideate how these ideas can be integrated into the cooperation process. Based on the desired design result, the participants will be introduced to a representation of the design result that they can use as a starting point to promote their design ideas, transform the EquiP representations, and visualise the agreed design outcome.
Techniques
Some of the techniques recommended as useful in this phase are co-construction of rapid prototyping, mock-up, storyboard or scenario design. The technique chosen should be influenced by and influence the EquiP representations’ journey from statements to design outcomes. The PD researcher should adopt the techniques chosen to achieve the final outcome of the PD process. However, a) giving space to each participant’s group to share design ideas and representations; b) requesting participants to collectively reflect on how to accommodate all the design ideas in the session’s outcome; and c) adapting the EquiP representations to ideas for the outcome either as it is, or in a transformed way, helps to equalise the powers and make each group’s ideas and representations part of the design outcome. If there are conflicting ideas, participants should articulate their position and negotiate a common solution through a democratic dialogue.
Tools
Similar to the previous step, the tools provided should be adapted to the abilities of the weaker group and involve options to refine the representation of the design ideas, so they can be implemented in the outcome.
Considerations
In this phase, no constraints should be introduced regarding how the stakeholders should interact or who should have the right to decide. The method’s structure should contribute to the equilibration of powers. The role of the facilitator(s) is to explain the tasks and guarantee that the participants do not deviate from the aim of the activity.
4 Research methods
In this section, we present the research setting in which the method was applied, the data collection process, and how we analysed the data to evaluate the application of the method. The EquiP method framework is theoretically grounded. Customisation for the healthcare context, particularly for MACI people, is grounded in the knowledge from conducting PD with MACI people, as presented in Chapter 2. The role of the researcher\designer in the application of the method is that of a facilitator who does not have a say in decision-making. The researcher\designer considers all stakeholders involved in co-design as equally relevant to the design space and cooperation.
4.1 Research setting
We applied the EquiP method in the context of cognitive rehabilitation at Sunnaas Rehabilitation Hospital in Norway.
Cognitive rehabilitation can be defined as ‘a process whereby people with brain injuries work together with professional staff and others to remediate or alleviate cognitive deficits arising from a neurological insult’ (Wilson, 2002, p.22). Cognitive rehabilitation is usually offered to patients who have cognitive challenges after an ABI. Cognitive rehabilitation aims to help these people improve their functioning or to support them in coping with the new situation. Sunnaas Rehabilitation Hospital is Norway’s largest specialist hospital in the field of physical medicine and rehabilitation. It provides multidisciplinary rehabilitation for people with complex functional impairments following illness or injury (Sunnaas, 2017). Among other things, it offers cognitive rehabilitation to people with mild to moderate cognitive impairments due to ABI (Becker et al., 2014). The hospital has established Norway’s first permanent unit for cognitive rehabilitation for ABI – offering individual and group-based rehabilitation services – called Kognitiv Rehabiliteringsenhet Sunnaas Sykehus in Norwegian (hereafter referred to as KReSS), or the Cognitive Rehabilitation Unit in English.
The process of cognitive rehabilitation at KReSS is as follows: The patient receives an evaluation of the condition at an outpatient clinic. If the patient is admitted to the programme, they have to wait for an appointment at the hospital. During the waiting time, the patient can attend two introductory meetings held at the outpatient clinic, in which they learn about the cognitive rehabilitation programme and are introduced to defining rehabilitation goals. This introduction is given by a nurse who has been working at KReSS for a long time and is always up-to-date on possible changes in the process. When the time comes, the patient is hospitalised for five weeks. During this period, the patient is supported by a multidisciplinary team comprising different healthcare professionals, such as a medical doctor, a nurse, a physiotherapist, an occupational therapist, a social worker, a speech and language therapist, and a psychologist. Together with the multidisciplinary team, the patient defines a set of rehabilitation goals, which are articulated towards functioning in everyday life (WHO, 2017). Patients and team members seek to divide the goals into sub-goals that can be achieved within a shorter timeframe. After setting goals and sub-goals for rehabilitation, the patient and the team together discuss and define a set of interventions for each sub-goal that the patient will undergo during rehabilitation. The information about goals, sub-goals and interventions is recorded in a health record document called the goal plan. All activities in which the patient participates at the hospital are related to a specific intervention, or set of interventions, aimed at helping the patient achieve rehabilitation sub-goals and goals. The involvement of the patient in the process and increased awareness of their rehabilitation process are deemed relevant to the rehabilitation outcome (Wilson et al., 2009).
Despite the common goal of improving the patients’ condition or helping them cope with their new selves, the cooperation and coordination between patient and staff are not always smooth. Usually, the patient cannot define clear rehabilitation goals, and the staff dig into personal stories to understand the patient’s needs in everyday life. In other cases, the patient does not understand what is going on with the rehabilitation activities. Hence, new ways to involve patients in their rehabilitation are needed.
As part of an internationally funded project, a cooperative digital tool that supports cooperation between the patient and the multidisciplinary team (the team that supports the patient during rehabilitation at the hospital) in setting rehabilitation goals and keeping track of the rehabilitation process while the patient is at Sunnaas, and continuing after they go home, will be developed. Currently, cooperation is facilitated through paper artifacts that serve as coordination mechanisms between a patient and their multidisciplinary team. On designing this new cooperative digital solution, there is a need to negotiate how much of the workload the patient can and is willing to take on in the cooperative space. Moreover, this will require the staff to negotiate their way of working. The relationship among actors is not conflictual, but the discussion of the processes and how to share the cooperative space places them on two different sides. With the help of technology they should seek to negotiate how to achieve the goals of a patient who is more involved and aware of their own rehabilitation, thereby promoting a positive outcome for the rehabilitation.
Building on Sunnaas’ philosophy of patient participation and empowerment, the project’s leading committee, comprising Sunnaas ‘domain experts’ and two PD researchers (authors of the paper), decided to take a PD approach to designing this new solution. This required the involvement of patients from KReSS, as well as the medical staff from this unit, to co-design the solution and negotiate the cooperative process for how they would use the digital solution.
In a PD process with healthcare professionals, patients are in a ‘weaker’ position, due to differences in knowledge and abilities. A patient does not have the same knowledge as healthcare professionals when it comes to rehabilitation, and their cognitive challenges create barriers to relationships with others. Moreover, this is related to the social structure within healthcare, where the patient is in a weaker position than the healthcare professional, mostly attributable to differences in power/knowledge. On designing a cooperative digital solution, applying our method between cognitive rehabilitation patients and the multidisciplinary team to empower patients can help to balance power in the PD process and contribute to giving the weaker group a stronger voice in the design process.
4.2 Data collection and analysis
Data collection and analysis were related to applying the method in practice. We applied the method in a series of two workshops within the project described above. Each of the workshops had a different aim, but the framework of the workshops, techniques and tools used was the same in both cases. In the first workshop, the aim was to design a digital tool that could improve coordination for setting goals in rehabilitation (the Defining Rehabilitation Goals workshop). In the second workshop, the aim was to design a digital tool that could be used to track the continuation of rehabilitation after the goals were set (the Facilitating Rehabilitation workshop).
The two workshops were audio-recorded. We took pictures that would help with the triangulation of the data analysis. Moreover, we received information from the hospital regarding the patients’ diagnoses and specific cognitive impairments. Finally, during the vertical group sessions we kept notes about whether the healthcare professional with whom the patient was working was their direct therapist, or just one of the team members not directly involved with that specific patient. Moreover, after each of the workshops, the two facilitators had a reflection-on-action (Schön, 1984) session. The reflections on the impressions from the workshop were audio-recorded.
Each of the patients and team members received a consent form describing the project and the aim of the specific workshop, with a brief description of the activities, and how the data would be stored and analysed later. All participants signed the consent form. Moreover, we deliberately did not save patients’ names or personal information. Digital content collected during the workshops was saved on the safe network on the hospital’s premises. The workshop materials that did not have any patient-related information were stored in a locked drawer. An ‘ethics of care’ (Gilligan, 1993) approach was adopted throughout the project (Table 1).
The aim of the analysis of the workshop recordings, pictures, EquiP cards and storyboards was to evaluate whether the method had fulfilled its aim. We thus initially drafted some assumptions about how the method might have contributed:
-
1.
In the Move phase, statements move to design ideas.
-
2.
In the Land phase, the EquiP cards support the ‘weaker’ group in discussing their design ideas.
-
3.
The method supports the balancing of power in decision-making in the Land phase.
-
4.
The method is adequate for the design of cooperative digital solutions.
We analysed the data sources mentioned above by taking a qualitative interpretative approach (Willis et al., 2007) to test whether the assumptions were true when the method was applied in the research setting described above. We conducted the analysis in four parts by using the assumptions as analysis questions. We analysed four recording transcripts from the horizontal group sessions (two from one patient in each workshop and two from one healthcare professional in each workshop). Moreover, we analysed five of the seven recorded transcripts from the vertical group sessions because the recording device compromised the quality of two of the recordings, so we could not transcribe them.
In the first part, we reflected on and analysed how the statements in cue cards moved into design ideas in the horizontal groups’ PD sessions. This was based on discourse analysis (Wooffitt, 2005) of the audio recordings from the horizontal groups’ PD sessions. As stated previously, the method aims to increase the opportunity of people with cognitive impairments to ‘have their say’ in PD sessions and to influence the micro-power relations emerging from moment-to-moment in the session. Discourse analysis is a suitable method to capture the moment-to-moment snippets of conversation and to analyse and interpret them within a specific context.
We were interested in the EquiP cards that were selected from each horizontal group as their design ideas. We thus initially traced the discussion journey for each of the cards that had made it into design ideas and analysed how each of the participants had contributed to the conversation and discussion of the cards. Pieces of conversation referring to the same card in different parts of the recordings were put together to facilitate interpretation. Moreover, snippets of discourse related to other cards that did not move to design ideas were considered, but not analysed thoroughly. Hence, we interpreted the interactions among the participants through their discourse for each of the design ideas. An open coding process was employed to extract recurring themes from the discourse analysis regarding different movement paths of the EquiP cards as they transitioned from statements to design ideas. The codes that emerged were grouped into categories presented in depth in Sub-Section 6.1.
In the second part of the analysis, the aim was to determine how the ‘weaker’ group – the patients – had made use of the cards, while discussing the positioning of the cards in the storyboard. Again, we applied discourse analysis to the discussion of each of the cards in each vertical group session and then applied an open coding process to extract recurring themes on how the patients used the cards.
In the third part of the analysis, the aim was to determine how decision-making regarding implementation of the cue cards in the storyboard took place. We conducted a discourse analysis (Wooffitt, 2005) of the audio recordings of the vertical group sessions. We analysed the snippets of discourse in which a specific card was discussed and then positioned on the storyboard. The analysis consisted of three parts: who did the card belong to, how much did each of the stakeholders discuss a specific card (speech bubble consisting of the number of sentences used to discuss a card), and which argument was more influential when deciding where the card would be positioned on the storyboard. From the analysis, we thus had the card owner, the speech bubbles of each stakeholder, and the design decision for the card represented, based on which arguments from the speech bubbles influenced the final decision. We then applied an open coding process to define a set of categories for the types of decision making. In Table 2 below, we call 1.1 the vertical group session in the Defining Rehabilitation Goals workshop, and 2.1 to 2.4 the four vertical group sessions in the Facilitating Rehabilitation workshop.
The fourth part was to create vignettes based on the storyboard and workshop recordings and to apply reflective analysis (Osmond and Darlington, 2005) to reflect on whether the storyboards presented a version of a digital solution involving cooperation between parties and new forms of division of labour. From the ethnography, we have a deep knowledge of the current processes, so it was easy to recognise in which storyboard there was a reflection of changes due to a new hypothetical digital solution.
Based on the analysis, we then discuss how the EquiP method contributed to the balancing of power among participants and influenced their ability to influence the design of this new cooperative digital solution.
5 Method EquiP in practice
The first author was directly involved in planning the workshops and facilitating them. We therefore write about the application of the method in the workshops in a personal way. As all authors have experience with PD and the reflective practitioner approach (Schön, 1984), we found that the personal perspective aided reflections on and analysis of how the method was applied and its impact on the micro-power relations. In Sections 6.1, 6.2, and 6.3, we use the auto-ethnographic storytelling first person ‘I’ to report on the workshops. In Section 6.4, where we present the analysis results, we return to the analytical ‘we’.
5.1 Start
I researched the cognitive rehabilitation process at the hospital for three years before applying the EquiP method as subsequently described. This involved five months of observations of the process by participating in meetings between the patients and various healthcare professionals. Moreover, I conducted a document analysis of the main documents involved in the cooperation process. Data analysis helped me map the main stakeholders: a) MACI patients, and b) their multidisciplinary team that worked together with MACI patients during the five weeks of rehabilitation at the hospital. I decided to consider the multidisciplinary team as one group. Each of the different members of the multidisciplinary team has almost the same role in relation to the management of the rehabilitation goals, despite the specific activities each of them conducts with a patient. I learned about the abilities of MACI people. I mapped the events, places and actors and created different customer journey maps that identified the main activities in the process and possible improvement points.
To plan for the Move and Land phase, I worked with a domain expert with in-depth knowledge of the cognitive rehabilitation process and MACI patients. We had three meetings for each workshop, to discuss how to apply the method. When reflecting on the representations’ options and the structure of the Move and Land phases, I applied the theoretical knowledge of the cognitive limitation of MACI patients presented in Section 2.4. For MACI people, structure and review are relevant to increase opportunities to contribute to the discussion and decision-making, and they can manipulate and interact easily with paper-based and tangible, concrete prototypes.
The first meeting was a brainstorming session on the customer journeys, to align our views on key points of cooperation we wanted to address in the workshop. As the rehabilitation process involves many activities distributed over time, we decided to have two workshops focusing on two parts: Defining Rehabilitation Goals and Facilitating Rehabilitation.
The second meeting was to generate statements for the two groups (MACI and healthcare professionals). We would use the cues during the workshop to engage the participants in critical thinking and to express needs regarding their cooperation and how that could be improved with the help of technology to support the main goal: patient empowerment in owning their rehabilitation process. During my observations, I noted, ‘the patient had not been in contact with KReSS in the last six months’. This refers to six months after the patient had left hospital and had to continue rehabilitation before returning to hospital for a follow-up week. In another situation, the patient said, ‘I have gone for a walk, but I haven’t worked with the goals’. Meanwhile, the domain experts reiterated how relevant it was for the patient to continue working toward rehabilitation goals and interventions at home. Therefore, a statement regarding the management of rehabilitation at home was necessary. We thus started with a set of keywords for writing such a statement. For example, ‘communication home’, ‘goal plan for home’, and ‘tracking activities home’. We also discussed that the statement should be written as a wishful thought, starting with ‘I want’ or ‘I would like’ as possible future scenarios for the rehabilitation process, with the help of a cooperative digital goal plan that supports patient empowerment. Writing this using the individual ‘I’ was meant to help the participants create a closer connection with the statements and, at the same time, foster a sense of responsibility representing one’s own opinion.
I drafted the first version of the statements. We then had around eight rounds of email exchanges to rephrase the sentences. The main rule was to be general and simple because, in this way, patients would be able to understand better. Referring to the period between discharge and the follow-up week, we arrived at this set of statements: ‘I want to have the opportunity to choose goals and sub-goals that I can continue working on at home; I want to have the possibility to continue rehabilitation at home and to have an overview of my achievements; I want the digital tool to remind me of what I have done at KReSS, and to suggest tips for how I can continue rehabilitation at home.’ As the events happening in rehabilitation are cooperative, they require both the patients and the healthcare professionals to be in charge. For example, we also prepared a set of Home cards for the healthcare professionals: ‘I would like to have the possibility to agree with the patient on a set of goals that the patient will work on in the next six months; I would like the opportunity to review how the patient has worked with the goals during the time at home when they come for follow up; I would like to have the possibility to prepare plans for the patients for when they go home.’ These cards are similar to the patient cards for the same element of cognitive rehabilitation, but they tackle the event from the healthcare professionals’ perspective.
The third meeting was about reflecting on EquiP representations and defining the activities of the Move and Land phase, based on the abilities of the MACI people.
We built on MACI people’s ability to work better with paper prototypes and decided to design the EquiP representations for co-design with MACI people and their healthcare professionals as paper play cards that carry a written statement and are then referred to as EquiP cards. In further detail, we considered that the text should be large enough to read. The statements should have numbers, so they are easy to reference. The size of the representation should be easy to keep at hand and move, to help patients become familiar with the cards and give them the opportunity for an easy overview as required. Each participant being a patient or a healthcare practitoner should be able to uniquely identify their set of EquiP cards. I thus designed the cards as shown in Figure 2. Together with the domain expert, we decided to use different colours to distinguish the cards for each patient and to use the same colour scheme for the healthcare professionals’ card sets. I added the hospital’s logo to bring this closer to the research context. I cut all the cards by hand, which also contributed to participants experiencing this as work in progress, rather than a perfect statement that could not be changed.
Figure 2a shows card number 15 – the ‘Home card’. We also show examples of the Kin card (I want it (the digital tool) to help me define goals together with KReSS and my kin) and the Change card (I want the opportunity to change my goals, sub-goals and interventions together with my therapist), which were also triggered from the observations.
We also discussed and planned the final prototype of the workshop. The main requirement was to gain the participants’ ideas on how to implement the wishful statements in the process, similar to a future workshop, where the implementation phase is focused on how the tool will be used. The outcome would thus be a scenario or story describing how patients and healthcare professionals could see their design ideas implemented together, and how far they would be able to negotiate and agree. To adapt to the EquiP cards, we needed a paper-based prototype in which the patients could include the cards. Based on my previous experience with MACI patients and the PD literature on people with cognitive impairment, writing a story can be overwhelming. The domain expert was completely against this. Instead, I proposed the idea of a storyboard. To co-create the storyboard, participants would be supplemented with visual animations of possible moments during rehabilitation, portraying either patients or healthcare professionals and using a digital tool in different environments. The domain expert found the idea very interesting. She suggested adding some text to the animation that could facilitate interpretation and avoid confusion. Moreover, the domain expert suggested dividing the storyboard into smaller parts whereby a set of related activities can come together to ‘facilitate the envisioning of the story’, she said. The storyboard template was adapted to the shape of the EquiP cards, and vice versa. We created the EquiP cards to be easily integrated into the storyboard boxes.
5.2 Move
At each of the workshops, two PD sessions, as shown in Figure 3, were conducted in parallel with the two horizontal groups: patients and healthcare professionals. The session framework for both groups was the same.
The domain expert and I facilitated each of the sessions. She sat with the patients, and I sat with the healthcare professionals. We asked the participants in each group to choose a random set of cards positioned on the table. We had initially explained to the participants that the session aimed to discuss design needs for the digital goal plan. To facilitate the participants’ understanding, however, we repeated this slowly and carefully in each horizontal group. As the cards were individual for each group, it was more reasonable to address their meaning within the group. We asked participants to open the cards, start reading them, and select the cards that referred to the activities in the rehabilitation process that they would like to be improved with the help of a digital goal plan. They could also add more activities/needs/wishes to some additional empty cards, or change the current cards by altering the text. If they wanted to make changes to cards, many pens and pencils were already on the table. Some of the participants understood more easily that the statements were just a set of suggestions from the facilitators and were by no means final decisions. One of the Facilitating Rehabilitation workshop participants asked the facilitator, ‘so, these are your thoughts?’. She explained carefully again that the cards were suggestions.
Meanwhile, some patients and healthcare professionals raised questions such as ‘what is this about’, or comments such as ‘I don’t understand this’ or ‘these seem very similar.’ However, both facilitators were involved in writing the statements and had adequate knowledge to address all the questions. Moreover, participants also supported each other in their understanding of the cards. Referring to the Home card, one of the participants said: ‘these are things that we want to have in a digital tool that we can also use from home.’ The facilitator said ‘yes’, and then another participant added, ‘oh, now I understand’.
After all the participants had gone through all the cards, we asked them to select and extract the five most relevant cards. The number of five selected cards was chosen randomly, aiming to make participants reflect on the most relevant ideas and make some choices at this stage, based on what they individually considered relevant ideas. They were asked to mark the five cards with a random sign. This would help us, as facilitators, later understand and interpret which cards (symbolising design ideas) during the discussion in group (the following activity of the workshop session) were selected individually and turned into a design decision and which were dropped. Selecting the cards was, again, an individual process. We observed that participants engaged with the cards, taking them in their hands and positioning them back on the table until they came up with a final selection.
We then asked participants to show the cards chosen to the others in the group and to explain why they thought the specific situation described in the card was important and ‘what the card meant for them’. The presentation of the cards created opportunities for discussion. While one participant presented their cards, another would say, ‘I have the same’ and engage in the discussion. Moreover, after revealing and discussing their cards with the group, we asked participants to agree as a group on a set of five final cards that they all found to be relevant functionalities to include in the digital goal plan.
In this part, the conversation became dynamic. The facilitator asked whether any of the participants was willing to start showing their cards. In the patient group, the facilitator added: ‘do you X want to start?’. While presenting her cards, the patient said, I have this ‘home one’ before starting the argument about what functionality at home would be relevant for her. The word home triggered her interest in the card. She explained that she would like ‘a way to communicate with the therapists once I’m back home’. Another participant intervened and said that he also had that card. He said he wanted ‘to continue things started at Sunnaas after returning home’. Another patient added that he would like ‘to have a colour structure of activities when at home’. This created a more dynamic discussion whereby, if someone had similar cards to the one presented, they would say so and possibly add to the explanation provided by the person presenting the card. In this case, the numbering of the cards was very useful, as participants would say the card number, and the others could easily look at their set and create an association with the card. As facilitators, we were careful to ask everyone whether they had any cards in their set that had not been discussed.
After sharing the cards and ideas, the next step was selecting the design ideas as a group. However, this process had already started with the individual presentation of the cards. One of the patients said, ‘so we all have the home card, what else?’. Then the Home card was taken from everyone and put in the middle of the table.
In the selection phase, we observed two different approaches to popular cards. For example, the Change card was selected individually by all participants and agreed upon as relevant. However, it was not discussed extensively on presenting individual cards or in the final design idea selection. Instead, for the Home card, each participant shared their individual interpretations when they presented individual choices, and this was also discussed again extensively in the selection of design ideas as a group. Thus, the Home card changed from a simple general statement in the EquiP card into a more detailed wish list of functionalities for the digital solution.
Regarding the change in representations, the patients only rewrote the statements in a few cases. Instead, the healthcare professionals were keener to rewrite the statements, as shown in Figure 2d.
Once the popular cards had been selected, some participants put forward cards they had chosen, but which were not popular. Hence, even the not-so-popular ideas were discussed in the group.
5.3 Land
At the start of the Land phase, we asked patients to find one healthcare professional (matching the cards’ colour as an element to generate random pairs) and sit together in pairs. Participants had to bring along the five cards chosen in the horizontal sessions. The pairs that were created represented the vertical group. The setting of the positions is shown in Figure 4. As facilitators we ensured that each participant had their own set of the horizontal session cards chosen for the next session. While participants enjoyed the coffee and snacks, we distributed the necessary materials in each planned position.
Once the vertical groups had been created, the first task was to show/present and explain the cards to each other. We only had two vertical group sessions in the Defining Rehabilitation Goals workshop, so the other facilitator and I sat with each group. We had five groups in the Facilitating Rehabilitation workshop, so sitting with them was impossible. We provided written material with the steps of the activities, displayed them on a big screen in the workshop room, and went to each group to explain the tasks verbally.
After presenting to each other the design ideas generated in the horizontal group and represented as EquiP cards, the second task was to rank the cards chronologically, based on the time when each of the events that the cards represented took place during the rehabilitation process. The aim was to make it easier for the vertical groups to envision how the design ideas represented by the EquiP cards would be embedded in the rehabilitation process. For example, design ideas related to managing the situation at home would be grouped together. However, there was a period at home before coming to the hospital and another period after. So distinguishing the chronology of events could help envision the dynamics of cooperation. The Home card described above was included in the activities performed with the digital tool at home after discharge. In addition to chronological grouping, we asked for a more event-oriented discussion of how design ideas could be grouped. For example, we asked participants to think about their design ideas concerning how a patient and healthcare professionals could cooperate in an individual session. The ranking of cards was intended to enable groups to get to know each other’s cards and to think of these ideas in a more concrete and structured way related to the rehabilitation process.
After ranking the ten cards, the third task was to create a storyboard of how each of the situations captured in each of the cards could be applied in practice at the hospital. We gave each group a storyboard template. In addition to the initial EquiP cards, participants were given some animated pictures using a digital tool from possible situations during rehabilitation at hospital, at home, or at an outpatient clinic. The animated pictures were general depictions, and the participants were free to assign meaning to the pictures, while not having to start drawing from scratch. Some of the pictures had captions that facilitated their interpretation. Some animated pictures of the Home cards are shown in Figure 5.
To facilitate the creation of the storyboard for the patients and reduce the barrier to their involvement in the process, we divided the storyboard into three parts: activities the patients do alone, activities that the patient and team members do together, and activities that the team member does on their own or with other colleagues.
The only prerequisite for the outcome (the storyboard) was that all cards had to be represented in the story, and if the aim of the cards was changed, that was also to be represented in the story. Referring again to the Home card, the vertical group had to discuss and in the storyboard show the process for how the tool could be used at home. One group interpreted this as ‘when the patient is at home, she could look at some content regarding rehabilitation therapies (Figure 5, left) and also log rehabilitation activities that she is doing daily and view some statistics of progress during the period at home’ (Figure 5, middle).
The participants in each vertical group managed to integrate the ten design ideas (in some cases ideas were merged as they were considered too similar) into the storyboard. The integration was not difficult for them, as the design ideas related to the same common rehabilitation process. Moreover, some cooperative structures were already in place, so they needed to negotiate how the tool could enhance the current cooperation and what to change in the cooperation. Most of the discussion focused on the possible changes, thus making it realistic to discuss and integrate each design idea.
6 Evaluation of the method
In this section, we present the findings from the evaluation of the method based on the assumptions presented in Section 4.2.
6.1 Moving EquiP cards to design ideas
The question we answer in this subsection is how the statements on EquiP cards moved into what Bratteteig et al. (2016) define as design ideas in the Move phase of the method.
From the analysis, we found that four types of ‘moves’ were enabled:
6.1.1 Grounded move
In this category, we included the cards selected by most participants during the individual evaluation in the horizontal group sessions and then discussed extensively within the group. When presenting the cards to each other, the participants discussed these cards and shared individual interpretations and ideas related to them. We considered the involvement of everyone in shaping such statements into a design idea as a grounded move.
Example
The Home card and the dynamic of the conversation, as presented above, show a typical case of a grounded move. Participants started sharing experiences from when they came home after rehabilitation, and further articulated their needs. They presented examples of possible follow-up strategies at home.
6.1.2 Unanimous move
In this category, we included the statements selected during the individual evaluation by virtually all participants. When presenting the cards to each other, the participants detected these common cards and did not discuss them or their interpretation, as in the grounded move. Instead, they unanimously accepted the statement and its shared interpretation. The card was selected by calling out the common card number. The person initiating the discussion would talk about the card’s interpretation, and the others would agree and add to the interpretation.
Example
During the observation period, the MACI patients said they would like to be able to change goals and sub-goals if necessary. The same applied to the healthcare professionals who, at staff meetings, had a continuous discussion of how to achieve a more flexible process that could adapt to changes in patients’ condition during rehabilitation. We thus created the Change card. During the horizontal group session, everyone chose this card. The interpretation was the same as the card statement, and all the participants agreed. In this case, participants’ agreement passed through without much analysis and discussion, and the card’s ‘evaluation’ was based on its popularity among participants.
6.1.3 Modified and joint move
In this category, we included the cards modified to adapt to different viewpoints and then selected as design ideas based on the discussion in the horizontal group session. The other types of cases concerned how participants discussed how to merge two cards that were related to each other. In these cases, this was mainly discussed by one or two participants, and others agreed.
Example
During the observations, we found that next-of-kin (either a family member or a close friend) were always involved in the process. During the observations, the first author met kin in different parts of the patient journey, such as: at the patient’s first meeting with the doctor and nurse; during phone calls with the nurse or social worker; or at the goal planning meeting, when the rehabilitation plan for the patient was adopted. We learned that kin involvement was considered support for the patient to undergo rehabilitation, or support for the patient to better explain their condition. Kin also plays a role in rehabilitation because these family members’ lives have also changed, and they have to find new ways of coping. We therefore created the cards: ‘I want my family, friends or kin to be involved in the digital tool; I want the digital tool to help to define goals in collaboration with my family and KReSS.’ These cards were used in the Defining Rehabilitation Goals workshop. On discussing the card statements, one (of two) participant stated, ‘we have number two the same’. The numbers helped them to look at similarities and differences, and to steer the conversation. As card number 2 both participants chose ‘I want the digital tool to help me in defining my goals’. While the previous participant was talking about card 2, the other participant added that card 14, regarding the involvement of kin in the process, could be connected with card 2. The participant added that it ‘would be better if the patient themselves could give access to the kin, based on a list’, emphasising how relevant it would be for the patient to have control. The other participant added, ‘I hadn’t thought about that, but is a good point’. This card was discussed further because the participants had different viewpoints. One of them argued about the relevance of the family being involved in the process because their life had changed as well, so they should be part of the goal planning and have their space in the ‘app’. The other participant agreed, but thought that this varied, so it would be more beneficial if the patient had the flexibility to decide which kin would be involved and to what extent. This discussion occurred when the participants presented the cards to each other. They moved on to discuss other cards.
During the selection of the five cards we observed how the participants did not give up on their ideas. Instead, they sought to combine them. In the recording, we can hear, ‘oh … this can fit with this’, referring to two different cards. For example, card 2 was combined with card 5, where the patients could decide on their goals, but the family and KReSS therapists would have the opportunity to be involved in the process and make changes to the digital tool. From the discourse analysis in the vertical group sessions, we found that the participants had not changed their interpretation of the design ideas. However, their interpretations had been expanded and merged with what was discussed in the group. A statement about ‘kin’ involvement in the process thus became a design idea. The representation of the card did not change in this case.
6.1.4 An influenced move
In this category we included the cards selected as design ideas with the agreement of the entire group, but which were not among the popular cards selected by the majority. In these cases, one participant presented the card and their interpretation to the others. The other participants agreed on the card and the interpretation, and added something to the discussion. The incidence of influenced move was rare and occurred when the participants had four design ideas, and then added an extra one to get the number of five requested in the workshop.
Example
Overview card – I want to have an overview of my test results.
This card was selected by one participant. When she started presenting her chosen deck of cards, she mentioned the test results card and said, ‘I would like to have the possibility to see all my test results. When I am at home, I can check if I can get the same score’. Another participant added, ‘oh … that is true, I would like that too. We can have more control over the tests’. The other participants also expressed concern by adding, ‘yeah … that’s a good thing … I had that card, too’.
We observed that all participants, on both the patient and healthcare professional sides, engaged in the discussion in groups, and agreed and concluded on the design ideas as a group.
The cards and the discussion about them captured participants ‘imagining of what could be in the future’ on a conceptual and solution-oriented level for the digital tool. The workshop structure facilitated making design choices. When the patients in the Defining Rehabilitation Goals workshop had chosen the card that represented ‘to have the possibility to pick up goals from a suggested list’ instead of ‘writing the goal on my own’, they made a design choice.
When it came to representing ideas on EquiP cards, we evaluated the facilitators’ role in explaining this form of representation to the participants as essential. Both groups had additional questions to ask the facilitators regarding cards and soon embraced the card function. In the recordings, we found that, early in the workshop, participants began engaging with the cards. Having key aspects of the cooperation process written down and discussing them with the other participants and the facilitator at the workshop contributed to the evaluation of the design ideas. This was because on asking for an interpretation of the cards, new interpretations could arise and, in this way, also new choices. While the participants were engaging with the material of the situation, the EquiP cards, and discussing them, new suggestions arose.
We observed that agreement on common ideas in horizontal group sessions presented more challenges for healthcare professionals. This is because, in some respects, they represent different interests relating to their specific professions.
The participants commented that the statements’ representation was a good choice as it allowed them to move the cards around, show them to others, or change them easily. Despite the engaging discussion about the cards, the patients did not make changes to the cards by writing or drawing on them. In contrast to the patients, the healthcare professionals implemented changes to the statements by writing over or on the back of the cards.
We concluded that the horizontal group sessions represent the generation of design ideas based on the definition of design ideas from Bratteteig et al. (2016).
6.2 MACI people using EquiP cards
In this part of the evaluation, we questioned how using the EquiP cards to represent design ideas helped people with cognitive impairment in the discussion in vertical group sessions. We evaluated how people with cognitive impairment specifically used the EquiP cards while creating storyboards. We found that the cards contributed in three ways to the power level in the co-design sessions by aiding people with cognitive impairment in the discussion and decision-making for the storyboards. As we did not experiment with other settings, we could not gauge the degree of patient involvement in a discussion without using cards. Thus, we present what we found during our workshops.
6.2.1 Cards as patients’ voices
In two vertical group sessions, facilitators observed during the workshop and confirmed through audio recordings that the healthcare professional was leading the session. At the beginning of the workshop, the healthcare professional started reading through all the cards, including the patients’ cue cards. They started conversing or thinking aloud about the cards, while the patients listened carefully. This was almost a situation of appropriation of the patients’ cue cards. However, there was a difference between the two vertical sessions.
In one of them, the patients did not contribute actively and agreed with the healthcare professional’s choices. Meanwhile, the patients focused on some form of representation of design ideas, which the patients did not further articulate, but were integrated into the design result by the healthcare professional. Conversation snippets, such as healthcare professional (H): ‘this card goes in the week and this in time home’ and Patient (P): ‘yeah, yeah, I agree’, were repeated.
Instead, in the other case, the patients had some ideas and opinions about the cards and sought to voice them. One example concerned the Home card. The patient said she ‘would like to have the possibility to look at the goals and get feedback from the multidisciplinary team’. The patient’s argument was the same as that used in the horizontal group session. However, we noticed that in this session, the patient argued with a weaker voice. The healthcare professional heard what the patient was saying and then presented her arguments and finalised the decision on her own by convincing the patient.
Another statement from the patient mentioned above was, ‘It wasn’t me that chose this card’. This was used to distance the design ideas and enable the healthcare professional to influence them. In one case, the patient was still articulating something, and the healthcare professional said, ‘should we not continue further’. The same situation arose when another patient tried to explain something and was further interrupted by the healthcare professional saying, ‘well, we are into something here; we continue here’.
In the situations described above, by analysing the prototypes and recordings we found that the healthcare professional even made the final decision for the patients’ cards, but how the final decision came into place varied in the two examples. In one, there is no speech bubble from the patient, and in the other, there is a small speech bubble which is then ‘influenced’ by the healthcare professional during the decision-making.
Yet despite the final decision to implement the required functionality discussed in practice, the patient’s voice was not lost. The cards are the patient’s voice represented in the outcome. The patient’s voice would have been lost if the cards had been missing in the examples presented above. Instead, their ideas were represented in the storyboards derived from the vertical groups of which these two patients were part, even though they in some way trusted the healthcare professionals to make the final design decisions.
As stated above, we also collected information about the patients’ diagnoses and cognitive challenges. By triangulating the data described above with the patient’s cognitive challenges, we found that in one case, due to attention problems, the patient had shifted attention by leaving the healthcare professional to take charge of the decision-making. In another case, the patient had cognitive challenges related to her ability to take the initiative. Even when articulating her ideas, the patient was not able to take the initiative to make a final decision, and the healthcare professional took charge of making a decision. Hence, in the storyboard, the cards were the only patient voice.
6.2.2 Cards as patients’ discussion partners
In this category, we included cases in which the patient or healthcare professional used the cards as an initiator of their argumentation for the cards’ meaning and how it should be implemented in the final prototype, and their argumentation influenced the outcome.
Towards the end of the vertical group session in the Facilitating Rehabilitation workshop, a patient and a healthcare professional were together reflecting on the PD process. They said, Therapist: ‘The cards are meant to help you, to make it easier.’ Patient: ‘Yes, because I can forget … The cards help me to make myself understood/wording when in the situation.’
The same patient, when trying to decide on the card, said ‘I would like to have a digital folder with all my documents’ The healthcare professional suggested that this could be an activity on the storyboard that the patient could do alone, and argued ‘this we can do together. You can share the documents, and we can work on them together’. The discussion continued, and the patient used the card to support the articulation of his ideas for how the process of sharing documents could be implemented. In the case of cards as a partner in our workshop, we found that this was also encouraged by the healthcare professional, who not only let the patient lead the decision-making, but also encouraged the use of the cards as a partner. In this case, the healthcare professional applied a more explorative attitude by asking the patient, ‘what do you think?’.
The patients used the cards as a partner for better self-articulation. In view of an MACI patient’s memory or attention problems, in the absence of the cards the patient might have forgotten what to say or may have been distracted. On the other hand, the card on its own would not represent the patient’s ideas to their fullest. So together they form a more powerful gestalt that can be discussed on equal terms with healthcare professionals.
6.2.3 Cards as patients’ winning arguments
In this category, we included the cases in which the participants used the cards to dominate a discussion and influence decision-making.
An example is the Home card. In this case, one patient told the healthcare professional that the card meant the patient would have the opportunity to make a goal plan that could be continued at home. To strengthen the argument, the patient stated, ‘everyone among the patients found the card regarding the continuation of rehabilitation at home important’. Representing the patient community helped the patient to amplify her voice and decide where the card should be positioned on the storyboard.
Healthcare professionals also considered using cards to be a strength. On one card, the healthcare professionals in the horizontal group session had come up with a design idea: ‘In my therapeutic time I want to have the possibility to log into different tools which I can use during the session. Every therapist can do the same.’ When this was discussed in one of the vertical group sessions, the healthcare professional said: ‘This relates to us … X (mentioned therapist name) has his own tools, I have mine, etc., and we want to have an integrated solution whereby we can link these tools.’
The design ideas discussed extensively in the horizontal group sessions were used as a strong argument to make a point and negotiate fairly with the other party, who could be either the patient or the healthcare professional.
Overall, different patients used cards differently during the vertical group PD sessions. The same card might sometimes be used solely as a voice, and sometimes as a partner or strength. Moreover, we found that the same patient might use different cards in different ways. For example, the Home card was used mostly as a partner and as a strength. According to our discourse analysis, this was because the patients in the horizontal group session discussed the ‘home’ phenomenon exhaustively, so that the patient argumentation level was broader and supplemented with others’ arguments. A grounded move in the patients’ horizontal group session thereby created incentives for patients to use a card as a partner or to win an argument during the vertical group session.
On the other hand, the Change card was not discussed extensively during the horizontal group session. Yet as this was a common card for most participants, they used the ‘design idea supported by all’ as an argument to emphasise the card’s relevance.
Another phenomenon was that when the card was used as the only voice, the participants who held it distanced themselves from it. When the patient stated ‘I didn’t choose this card’, we traced this back to the horizontal group session and found that the patient had not chosen the card. The card was selected as a design idea by association with the majority, so the patient did not have an understanding of and connection with the card.
The types of moves influenced how the cards aided the patients during the vertical group sessions. Greater consideration should be given to how to promote grounded moves when customising the method for other cases. Finally, we found that, in cases where the cards had been used mainly as a partner or strength, more activities were conceptualised as shared and different ways of using the digital tool for cooperation were proposed. This was represented by having more cards positioned in the middle row of the storyboard (Figure 6).
We cannot compare these cases with a similar situation without cards. Furthermore, how the patients use the cards may depend on the patient’s clinical condition, the healthcare professional and the task at hand. However, we found that even in cases where the patient’s only voice was the cards, their ideas were not lost, and they made a more substantial contribution than would have been possible without the cards. When patients used the cards as discussion partners or to win arguments, the contribution was substantial.
6.3 Decision-making in vertical group sessions
The method’s aim was not only to end up with an equal number of design ideas from each stakeholder group implemented in the final storyboard, but also that the storyboard represented the views of people with cognitive impairments and the healthcare professionals. The question raised in this part of the analysis is ‘Who decided on and how were the viewpoints of each group equally represented in the final storyboard?’. We thus analysed how the pairs discussed and made decisions for each card in the storyboards.
We initially looked at the design ideas chosen by each horizontal group. We found that the patients’ and healthcare professionals EquiP cards, brought into vertical group sessions, were complementary (similar or integrative) and did not include contradictory situations. In one of the horizontal group sessions, after finishing the storyboard, a patient said ‘We had common things and cards’. The healthcare professional replied ‘It’s good that we don’t think completely differently, isn’t it’. However, the cards referred to how to shape cooperation based on the perspectives and needs of each group. Even though the ideas on the cards were not contradictory, they required patients and healthcare professionals to negotiate the division of labour in the common cooperative space and how the new coordination mechanism could support this division of labour.
We found three types of decision-making during the vertical group sessions. Figure 7 shows the journey from a) a design idea represented through a card to b) the discussion of the design idea represented in speech bubbles from each participant, and to c) the final decision on how the design idea integrates into the design outcome. The dominant colour in the design decision circle shows who made the final decision. The other colour (in the minority) in the circle represents how far the other group’s idea influenced the final decision. Decision-making is represented as a sum of the speech bubbles on each design card. The speech bubbles represent how far a patient or healthcare professional discussed a specific card in the vertical group.
6.3.1 Common decisions (CD)
Common decisions are situations in which the two participants in the vertical group shaped and decided on how to implement the cards in the storyboard. Usually, one of the participants initiated the decision, but the discourse shows that both presented their arguments and agreed. This type of decision was present on the patients’ cards.
To illustrate this, we present part of the dialogue taking place in group 2.1 regarding the card: ‘I want a digital folder with my documents’:
H: The digital folder comes at first?
P: I think it is all the way, at the beginning. After we have had the assessment, we can receive the weekly plan on the phone ... and maybe daily, after lunch … it can be updated.
H: ah the time edit? (patient calendar).
H: So that folder should be one of the first things that we have here? (referring to the storyboard).
P: Yes, the first time that we come to the hospital.
H: So you think it should be a folder were both the team and the patient can add things?
P: Yeah I thought … Yeah that can maybe be ...
H: Should we maybe paste it here …
P: Yeah, so if I have ... I have a meeting with a nurse, OT and psychologist, and ... then I receive a booked time … First, I accept it ... and when the time comes, we have the meeting.
H: If there is digital, then you would have crossed in the old or you can make changes to the new one.
P: For example, I was in the relaxation session, and I had trouble with balance. I could add something to the tool, and then you could have the overview … and you say: ‘I want to talk to you’, and you can suggest reducing the weight.
H: I would have liked that.
The conversation shows how the patient and the healthcare professional discuss with each other, ask questions and argue for their ideas, and how both shape the decision.
6.3.2 Influenced decisions from either the patient (ID-P) or the healthcare professional (ID-H)
Decisions were taken mainly by one of the participants, a patient or healthcare professional, but the other participant also commented on or contributed some ideas.
A situation considered to be a patient-led decision was recorded in group 2.3 regarding the card ‘I want to have the possibility to choose my goals, sub-goals which I will continue at home’:
P: I meant that ... I want to have … In the six months I am home, I want to be asked: Have you followed goals or not? ... Instead of going six months without talking, we can keep in contact.
H: Maybe we can send like a reminder: How is it going?
P: When we go home, it is the person alone, so that could be nice.
On the other hand, in another situation within the same group, we notice a healthcare professional lead the decision, such as in the conversation snippet below regarding the card ‘I want to have an overview of my test results.’ The patient wanted the overview of test results while at home, while the healthcare professional took her in another direction, stating and deciding that the best use for such a functionality would be during the hospital stay.
P: It seems like we can have this overview at home …
H: I’m not completely sure … I think if you are here during the week and have had a test, you can put that in the app and you can maybe do this weekly. Because when you go out, there are no changes …
6.3.3 One-sided decisions by either the patient (SC-P) or the healthcare professional (SC-H)
In this category, we included the decisions for which one person (patient or healthcare professional) provided the major argumentation and decided where to position the card, by asking the other person for formal confirmation, accompanied mainly by ‘yeah’ by the counterpart with no additional argument.
When they read the card, ‘In a meeting with a therapist: I want to know beforehand what we will talk about. I want to have a summary of the session when we have finished. I want to know how the session relates to my goals’ in group 2.3, the following conversation took place:
H: There are three things here, so maybe it can be positioned here?
P: Yeah, maybe it is there. It was not me that said it was important.
In groups 2.3 and 2.4, there were more cases of patients agreeing without discussion or elaboration. More statements, such as ‘yeah yeah … I don’t know … good luck … you should know’ were recorded.
To answer the question raised in this subsection, we built Table 2. It shows decision-making type for each card. In the table, there are:
-
CD – 15 common decisions
-
ID-P – 7 patient-influenced decisions
-
ID-H – 11 healthcare-professional influenced decisions
-
SC-P – 0 one-side decision from the patient
-
SC-H – 15 one-side decisions from the healthcare professional
To better interpret the results, we triangulated this data with the patient’s condition and the type of card under discussion. The one-sided decisions, mostly in groups 2.4 and 2.3, are on the healthcare professionals’ cards. For some cards, this is understandable because the card referred to the specific needs of the healthcare professionals in the digital solution.
There were high numbers of common decisions and patient-influenced decisions on both patients’ and healthcare professionals’ cards. The common decisions or patient involvement in the decisions show that patients contributed to the workshop regarding things that concerned them, and that power was equilibrated during the design.
The type of decision-making is strongly related to how the patients use the cards in vertical group sessions. The cards as discussion partners are associated with more cases of common decisions or patient-influenced decisions. The same is true for cards as winning arguments.
6.4 Designing a cooperative digital solution
The question we raised in this part of the analysis was how the method contributed to shaping the cooperative processes and designing a cooperative solution to be used among stakeholders.
Below, we present a vignette of the new cooperation process proposed in one of the storyboards from the Defining Rehabilitation Goals workshop. We will call the persona in the vignette Anna.
‘Anna would initially come to the outpatient clinic. Maria, the nurse, would be the first to meet Anna and introduce her to a digital tool she could use for her rehabilitation in cooperation with her multidisciplinary rehabilitation team. The digital tool would have a “getting to know You” functionality whereby Anna would receive different questions about her life with cognitive impairment. Anna would be able to add as much information as she found suitable regarding her everyday life. Anna could also create the opportunity for a next-of-kin login. She relies a lot on her mother, Mia, and will add her to the support group. Mia can log in and help Anna describe her condition to the therapists. Maria can read what Anna and Mia have added, with highlighting of who has added what. This is important for Maria’s job because it describes Anna’s awareness of her symptoms. Once Anna has logged her patient journey, she will be introduced to a page with instruction on how to set rehabilitation goals. She is provided with a list of goals pulled automatically from a pool of previous patients’ goals, based on the functional challenges she has logged. She can select the goals she finds suitable, and she will also have the opportunity to customise these goals according to her needs.”
The vignette shows a new way in which Anna, the patient, and Maria, the healthcare professional, can cooperate using a cooperative digital tool. This is a change from the existing processes described in the research setting.
From our analysis of five out of seven storyboards, a new cooperation practice was envisioned. EquiP can contribute to the design of cooperative computer systems, although this should be customised according to the issue at hand and the project’s development status.
7 Discussion
This section discusses how parts of the method have contributed to enabling different kinds of power, to create a power balance in the vertical sessions. We also discuss the power play for each actor in the PD sessions, with detailed reflections on the facilitator/researcher/designer role. Finally, we discuss how the method is positioned where PD and CSCW meet and their roles in both fields.
‘EquiP’ is a PD method that can be used to balance power in designing for cooperation in cases where the cooperating parties have power disbalances. We argue that facilitating the ‘weaker’ group to generate design ideas within the group and using these ideas in interdisciplinary PD sessions can ensure that positive-sum power is maintained and that people with cognitive challenges ‘have a say’ in the process and influence the outcome. Maartmann-Moe (2019) shows that a mutual learning process with users over time may enable them to develop ‘design-decision competence’. This takes time, however. Our method provides some of the same through the stakeholder-based EquiP representations discussed and selected in the horizontal groups. The method consists of dividing the lifecycle of a design idea (Bratteteig et al., 2016) into three phases and unifying representations of design ideas for all stakeholder groups, by taking the abilities of the weaker stakeholder as a reference. The power relations at the micro level, which emerge during co-design sessions, are the focus. While PD is concerned with balancing power by involving all stakeholders in the design, there has been less discussion of the micro-power relations that influence the democratic dialogue in a moment-to-moment conversation. By aiming to give the weaker group the opportunity to have more power in negotiating design decisions, we contribute to increasing their opportunities to influence the outcome.
In the literature, the relationship between patients and healthcare professionals is considered to be ‘power over’, whereby the medical practitioners decide for the patients (Geuens et al., 2018). This is influenced by the social structure and by the paternalistic relationship between patient and doctor and their differing levels of knowledge. The power balance becomes even more complicated when patients suffer from cognitive impairments, limiting their abilities. As stated above, the power in a PD session resides in the ability to move a statement to the final design decision. However, the journey of a statement is long, and factors such as the ability to articulate or represent one’s own ideas can diminish the chances of a statement from one person becoming part of the design results. According to Bratteteig et al. (2016), a person equipped with design ideas can have stronger arguments and gain peer support. Enabling stakeholders to generate design ideas and standardising the representation in a way that is adapted to the weaker group gives all of the stakeholders equal opportunities to envision future solutions and to represent the ideas in a simple way, thereby equilibrating their opportunities and increasing the weaker user group’s ‘power to’ influence the design outcome.
In the findings, we described different ways in which the patients used the EquiP cards in the co-design workshop with other stakeholders, and in different types of decision-making regarding the storyboard. In the case of cards as the only voice, we found that either healthcare professionals influenced decisions, or they made one-sided decisions. The healthcare professional thus dominated the decision. Power may occur in the form of influence, trust and loyalty, particularly when there are differences between the stakeholders’ power/knowledge (Bratteteig and Wagner, 2012, 2014; Bratteteig et al., 2016). The influence and trust created in the case of cards as the only voice can be discussed as part of the ‘power over’ exerted by the healthcare professional on the patient. However, even in this case of ‘power over’, the power imbalance was redressed by the cards’ existence. This gave the patients the opportunity to be represented in the design outcome through the cards, even when their abilities compromised a dominating position. The patient is influenced by or trusts the healthcare professional who makes the final decision, but the genesis of this decision is still the patient’s cue cards. The patient’s voice, or the voice of all patients that participated in the horizontal group PD, was present in the cards as they discussed, evaluated and selected that specific idea. Hence, the power of the patient and the healthcare professional as a positive sum (Haugaard, 2012) has increased, and they have both contributed to the final outcome. In Figure 7, we present the design decisions as a sum of arguments that influence the final decision, in analogy with power as a positive sum, where the contribution from one stakeholder does not diminish the other.
In other cases, the use of the cards as discussion partners and as winning arguments shows the contribution from the patients’ ‘power to’ and ability to articulate their design ideas, defend them, and further influence the outcome in the form of common decisions or patient-influenced decisions. The patient’s ‘power to’ was supported by the use of cue cards, closing the gap in their ability to envision future solutions compared to healthcare professionals. Moreover, it was supported by discussing the ideas within the group, where patients could freely discuss ideas with others in the same situation and strengthen their arguments by combining them with arguments from others.
The use of the cards as a winning argument in common decisions or patient- or healthcare-professional-influenced decisions helped balance the power in the workshop and create an atmosphere of ‘power with’, where the patient and healthcare professional share the power that grows out of collaboration. We thus conclude that EquiP supported the power balance during the vertical group sessions and contributed to a better understanding of micro-power relations.
Using the cards as partners and winning arguments, the patient has the ‘power to’ discuss equally and influence the outcome from co-designing with their healthcare professionals. However, another ‘group’ is involved and plays an important role in the balance of power. This group is the ‘PD researcher(s) and domain expert(s)’. Even though the cue cards play an important role in creating alternatives for stakeholders, and particularly for patients who need them more, they may also influence the outcome by compromising participants’ ‘power to’. We found that, at an early stage, the patients became aware that the cue cards were only general ideas. The metonymic sentence structure helped in not providing final solutions, but generated some alternatives and served to nudge the further generation of more design ideas. Researchers who might adapt the method in the future should therefore carefully consider the generation of statements and possible representations and, as mentioned in the method, adapt this to the needs of the ‘weakest’ group.
Hence, the researcher is a relevant actor in the method, as the ‘power to’ generate statements falls into her/his hands. However, the statements generated make only some aspects of the current situation explicit and do not suggest ideas to participants that might bias their opinions. The metonymic structure of the sentences in the statements reveals specific moments of the rehabilitation process that serve as trigger words for the patients or healthcare professionals. On analysing the discussion of the EquiP cards in the vertical group by patients or staff, we found that the interpretation the patient gave to the cards was an evolved version of the statement. It had commonalities with the statement, but was more detailed and articulated, and indicated future wishes. This was more common for cards that were discussed extensively within the horizontal groups. Moreover, as facilitators, we made it clear from the start that the statements were ideas that were not completed, and not perfect, and that needed interpretation, change, rejection and approval from the participants.
The involvement of a domain expert familiar with the challenges of the weaker user group and who knows the process well, but is not directly part of it, serves as a control mechanism for generating non-leading statements The ‘power to’ generate statements is thus shared between the designer/researcher and the domain expert.
However, what makes the generation of design ideas possible is the organisation of the horizontal sessions. Individual reflection, prioritisation of ideas, presentation and discussion in the group, and then as a group defining a set of final design ideas, ensures that the voice of the participants is brought forward for discussion in the final outcome in the vertical sessions. Beginning a discussion within the group promotes the unification of power in supporting an idea. The facilitator should ensure that each participant’s voice is heard and that the ideas they support are articulated and discussed to show why they are considered relevant. Through the cards in the first phase and by encouraging the group design ideas to move in the horizontal session, the designer/researcher is thus preparing the weaker group to go to the vertical session with some ‘power to’ discuss and contribute equally to the final design outcome. The designer/researcher concedes the power to the participants after the Start phase and takes on the role of facilitator in the next phases of the method. Although only facilitating the session in the Move and Land phases, the designer/researcher plans the activities of these phases, so they exert power over the choice of techniques and tools. The support from the domain expert in these phases and their deep knowledge of PD should help the designer/researcher organise a process that allows a balance of power. Mutual learning between the designer/researcher and the domain experts involved in the planning is relevant and contributes to aligning objectives for the relevance of patient involvement in the design process.
In the overall decision-making for the workshop, the patient’s voice was heard and represented in the outcome. The participants’ design ideas create a power gestalt, making participants more able to influence the outcome by having an increased ‘power to’. This ‘power to’ relates to the ability to discuss and stand for their design ideas as representatives of themselves and the entire group. The increase in ‘power to’ by generating ideas in the horizontal group sessions influences the creation of a ‘power with’ situation in the vertical group sessions. This is what PD stands for: the power balance and the ability to share power with others in the design process.
The consideration of power issues among stakeholders in the design process is also relevant for negotiating cooperative work relations. The balance of power in the design served as an incentive for patients to consider common activities they can perform with the healthcare professionals during rehabilitation, and to discuss the division of labour to promote cooperation. We argue that the EquiP method, building on the PD principle of balancing power in design, can be applied to designing digital solutions for cooperative work. The method not only serves as an incentive to discuss the digital solution, but also as a way to negotiate, discuss and reconceptualise the current cooperation. While we agree with Kensing and Blomberg (1998) that PD and CSCW have different perspectives, in this paper we present a case in which the perspectives merge. On one side, PD is applied as the approach to design a cooperative digital solution and re-shape cooperation. On the other side, designing computer support for cooperation is used as a context in which the PD struggles to balance power and democratise design are found crucial in promoting cooperation as empowerment and a positive change in the current social structures. Power issues in organisations are usually hidden under institutional power. This needs to be considered when discussing cooperative work because the socio-cultural and political elements that regulate relationships in cooperative workplaces influence how labour is divided. If the power issues due to differences in knowledge, abilities or social structures are discussed and considered during the design phase, this could contribute to the design of the artifacts that support cooperation and re-thinking of cooperative relations. We consider the case of patients and healthcare professionals as a positive-sum power relation in which strengthening cooperation and redistributing tasks will empower both groups and contribute to delivering better care.
The method we present captures two main issues in both fields – designing for cooperative work in CSCW and balancing power in co-designing and including marginalised user groups in the process in PD. These remain issues of concern for both fields. In CSCW, new domains of cooperative work are being explored, new ways of working together emerge and shift (Schmidt, 2011), and the work is even made visible in new contexts (Bratteteig and Wagner, 2013). In PD, the commitment to democratic practices in design promotes continuously marginalised groups that exist in different social contexts or emerge in new contexts. While the method has been presented in the case of designing a new CSCW digital solution to be used in rehabilitation, it also presents a case for improving the current cooperation and cooperative processes in other contexts.
8 Conclusion
In this paper, we present EquiP, a method that can be used to balance power in the co-design of cooperative digital solutions. The method has been developed on the basis of PD and the organisation of change processes, and we have applied it to an actual project. We presented the theoretical basis for the method, the method itself, and how it was applied in practice in two workshops on the subject of cognitive rehabilitation. Furthermore, we discussed the micro-power relations in vertical group PD sessions, with aiding of equilibration by the EquiP representations and the horizontal group sessions.
We found that the method had contributed to increasing the ‘weaker’ group – in our case, the patients’ ‘power to’ generate and discuss design ideas and then influence the design outcome. While the case we presented is only one way of initiating statements and representing ideas, EquiP has the potential to be customised for contexts where computer systems that are to support cooperation as an element of empowerment are designed. The stakeholders that will use this have differences in terms of power related to socio-cultural structures, knowledge or abilities. In the future, we plan to continue evaluating the method with other forms of EquiP representations and to introduce techniques and tools to motivate people to contribute more to refining the design idea representations.
References
Andersen, Tariq (2010). The participatory patient. In Proceedings of the 11th Biennial Participatory Design Conference (PDC), Sydney, Australia, 29 November - 3 December 2010. New York: ACM. pp. 151–154
Bagalkot, Naveen; and Tomas Sokoler (2011). MyReDiary: Co-designing for collaborative articulation in physical rehabilitation. In ECSCW 2011: Proceedings of the 12th European Conference on Computer Supported Cooperative Work, Aarhus, Denmark, 24–28 September 2011. London: Springer, pp. 121–132.
Balaam, Madeline; Stefan Rennick Egglestone; Geraldine Fitzpatrick; Tom Rodden; Ann-Marie Hughes; Anna Wilkinson; Thomas Nind; Lesley Axelrod; Eric; Harris and Ian Ricketts (2011). Motivating mobility: Designing for lived motivation in stroke rehabilitation. In CHI 2011: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Vancouver, Canada, 7–12 May 2011. New York: ACM, pp. 3073–3082.
Bardram, Jakob E; and Claus Bossen (2005). A web of coordinative artifacts: Collaborative work at a hospital ward. In Proceedings of the 2005 International ACM SIGGROUP Conference on Supporting Group Work, Sanibel Island, Florida, USA 2005. New York: ACM, pp. 168–176.
Becker, Frank; Melanie Kirmess;Sveinung Tornås ; and Marianne Løvstad (2014). A description of cognitive rehabilitation at Sunnaas Rehabilitation Hospital – balancing comprehensive holistic rehabilitation and retraining of specific functional domains. NeuroRehabilitation, vol. 34, no.1, pp. 87–100.
Bjørn, Pernille; and Morten Hertzum (2011). Artefactual multiplicity: A study of emergency-department whiteboards. Computer Supported Cooperative Work (CSCW), vol. 20, no.1–2, pp. 93–121.
Blomberg, Jeanette; and Helena Karasti (2012). Ethnography: Positioning ethnography within participatory design. In Routledge International Handbook of Participatory Design. New York: Routledge, pp. 86–116.
Borges, Luciana Correia Lima de Faria; Lucia Filgueiras; Cristiano Maciel; and Vinicius Pereira (2013). A customized mobile application for a cerebral palsy user. In SIGDOC'13: Proceedings of the 31st ACM International Conference on Design of Communication, Greenville, North Carolina, USA, 30 September 2013- 1 October 2013 . New York: ACM, pp. 7–16.
Bossen, Claus (2002). The parameters of common information spaces: The heterogeneity of cooperative work at a hospital ward. In CSCW 2002: Proceedings of the 2002 ACM Conference on Computer Supported Cooperative Work, New Orleans, Louisiana, USA, 16-20. New York: ACM, pp. 176–185.
Branco, Rita Maldonado; Joana Quental; and Óscar Ribeiro (2016). Playing with personalisation and openness in a codesign project involving people with dementia. In PDC 2016: Proceedings of the 14th Participatory Design Conference Volume 1, Aarhus, Denmark, 15-19. New York: ACM, pp. 61–70.
Bråthen, Heidi; Harald Maartmann-Moe; and Trenton Wade Schulz (2019). The role of physical prototyping in participatory design with older adults. In ACHI 2019: International Conferences on Advances in Computer-Human Interactions, Athens, Greece, 24–28 February 2019. International Academy, Research and Industry Association (IARIA), pp. 141–146.
Bratteteig, Tone; and Ina Wagner (2014). Disentangling Participation: Power and Decision-making in Participatory Design. Cham: Springer.
Bratteteig, Tone; Keld Bødker; Yvonne Dittrich; Preben Holst Mogensen; and Jesper Simonsen (2012). Methods: Organising principles and general guidelines for participatory design projects. In Routledge International Handbook of Participatory Design. New York: Routledge, pp. 137-164.
Bratteteig, Tone; and Ina Wagner (2012). Disentangling power and decision-making in participatory design. In PDC 2012: Proceedings of the 12th Participatory Design Conference: Research Papers – Volume 1, Roskilde, Denmark, 12 - 16 August 2012. New York: ACM, pp. 41–50.
Bratteteig, Tone; and Ina Wagner (2013). Moving Healthcare to the Home: The Work to Make Homecare Work. In: ECSCW 2013: Proceedings of the 13th European Conference on Computer Supported Cooperative Work, 21–25 September 2013, Paphos, Cyprus. London: Springer, pp. 143–162.
Bratteteig, Tone; and Ina Wagner (2016). Unpacking the notion of participation in participatory design. Computer Supported Cooperative Work (CSCW), vol. 25, no.6, pp. 425–475.
Bratteteig, Tone; Ole Kristian Rolstad; and Ina Wagner (2016). The life and death of design ideas. In COOP 2016: Proceedings of the 12th International Conference on the Design of Cooperative Systems, Trento, Italy, 23–27 May 2016. Cham: Springer, pp. 259–275.
Cabitza, Federico; Marcello Sarini; Carla Simone; and Michele Telaro (2005). When once is not enough: The role of redundancy in a hospital ward setting. In GROUP 2005: Proceedings of the 2005 International ACM SIGGROUP Conference on Supporting Group Work, Sanibel Island, Florida USA. New York: ACM, pp. 158–167.
Çarçani, Klaudia; and Harald Holone (2019). Participatory design “Method Story”: The case of patients living with mild acquired cognitive impairments. In ACHI 2019: The Twelfth International Conference on Advances in Computer-Human Interactions, Athens, Greece, 24–28 February 2019. IARIA, pp. 210–217.
Christensen, Lars Rune; and Erik Grönvall (2011). Challenges and opportunities for collaborative technologies for home care work. In ECSCW 2011: Proceedings of the 12th European Conference on Computer Supported Cooperative Work, Aarhus, Denmark, 24–28 September 2011. Springer, pp. 61–80
Colonius, Immo; Sandra Budde; and Roberta Annicchiarico (2010). Participatory design for challenging user groups: A case study. In ECCE '10: Proceedings of the 28th Annual European Conference on Cognitive Ergonomics, Delf, Netherlands, 2010. New York: ACM, pp. 339–340.
Consolvo, Sunny; David W McDonald; Tammy Toscos; Mike Y Chen; Jon Froehlich; Beverly Harrison; Predrag Klasnja; Anthony LaMarca; Louis LeGrand; and Ryan Libby (2008). Activity sensing in the wild: A field trial of ubifit garden. In CHI 2008: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Florence, Italy, 5 -10 April 2008. New York: ACM, pp. 1797–1806.
Dæhlen, Åsmund; and Suhas Govind Joshi (2019). Immersion as a strategy to facilitate participatory design involving people with intellectual disabilities and caretakers as proxies. In ACHI 2019: International Conference on Advances in Computer-Human Interactions, Athens, Greece, 24 - 28 February 2019. International Academy, Research and Industry Association (IARIA), pp. 15–24.
Dæhlen, Åsmund Kristiansen (2019). Facilitating for Capabilities-Empowering People with Intellectual Disabilities Using Proxies to Facilitate Participation. Master Thesis. Department of Informatics, University of Oslo.
Dahl, Robert A (1957). The concept of power. Behavioral Science, vol. 2, pp. 201–215.
Dawe, Melissa (2007). Let me show you what I want: Engaging individuals with cognitive disabilities and their families in design. In CHI‘07: Extended Abstracts on Human Factors in Computing Systems, San Jose, CA, USA, 28 April 2007- 3 May 2007. New York: ACM, pp. 2177–2182.
Eghdam, Aboozar; Jeremiah Scholl; Aniko Bartfai; and Sabine Koch (2012). Information and communication technology to support self-management of patients with mild acquired cognitive impairments: Systematic review. Journal of Medical Internet Research (JMIR), vol. 14, no.6. JMIR Preprints, e159.
Emery, Merrelyn; and Ronald E. Purser (1996). The Search Conference: A Powerful Method for Planning Organizational Change and Community Action. San Francisco: Jossey-Bass Inc Pub.
Fitzpatrick, Geraldine; and Gunnar Ellingsen (2013). A review of 25 years of CSCW research in healthcare: Contributions, challenges and future agendas. In Computer Supported Cooperative Work (CSCW), vol. 22, no.4–6, pp. 609–665.
Frennert, Susanne; Britt Östlund; and Håkan Eftring (2012). Capturing seniors‘ requirements for assistive robots by the use of attention cards. In CHI 2012: Proceedings of the 7th Nordic Conference on Human-Computer Interaction: Making Sense Through Design, Copenhagen, Denmark, 14 - 17 October 2012. New York: ACM, pp. 783–784.
Galliers, Julia; Stephanie Wilson; Abi Roper; Naomi Cocks; Jane Marshall; Sam Muscroft; and Tim Pring (2012). Words are not enough: Empowering people with aphasia in the design process. In PDC 2012: Proceedings of the 12th Participatory Design Conference: Research papers-volume 1, Roskilde, Denmark, 12 - 16 August 2012. New York: ACM, pp. 51–60.
Geuens, Jonas; Geurts Luc; Thijs W Swinnen; René Westhovens; Maarten Van Mechelen; and Vero Vanden Abeele (2018). Turning tables: A structured focus group method to remediate unequal power during participatory design in health care. In PDC 2018: Proceedings of the 15th Participatory Design Conference: Short Papers, Situated Actions, Workshops and Tutorial – Volume 2, Hasselt and Genk, Belgium, 20 - 24 August 2018 . New York: ACM, pp.1–5.
Gibbs, Raymond W (1999). Speaking and thinking with metonymy. Metonymy in Language and Thought, vol. 4, pp. 61–76.
Gilligan, Carol (1993). In a different voice: Psychological theory and women’s development. Cambrige and London: Harvard University Press.
Greenbaum, Joan; and Finn Kensing (2012). Heritage: Having a say. In Routledge International Handbook of Participatory Design. New York: Routledge, pp. 41-56.
Gustavsen, Bjorn (1985). Workplace reform and democratic dialogue. Economic and Industrial Democracy, vol. 6, pp. 461–479.
Haskins, Edmund C; Keith D Cicerone; and Lance E. Trexler (2012). Cognitive Rehabilitation Manual: Translating Evidence-based Recommendations into Practice. Vancouver: ACRM Publishing.
Haugaard, Mark (2012). Rethinking the four dimensions of power: Domination and empowerment. Journal of Political Power, vol. 5, pp. 33–54.
Hendriks, Niels; Frederik Truyen; and Erik Duval (2013). Designing with dementia: Guidelines for participatory design together with persons with dementia. In INTERACT13: Human-Computer Interaction, Vol. 8117, Issue PART 1. Springer. Cham: Springer, pp. 649–666.
Herstad, Jo; and Harald Holone (2012). What we talk about when we talk about co-creative tangibles. In PDC 2012: Proceedings of the 12th Participatory Design Conference: Exploratory Papers, Workshop Descriptions, Industry Cases – Volume 2, Roskilde, Denmark, 12 - 16 August 2012. New York: ACM, pp.109–112.
Huybrechts, Liesbeth; Maurizio Teli; Mela Zuljevic; and Mela Bettega (2020). Visions that change. Articulating the politics of participatory design. CoDesign, vol. 16, no.1, pp. 3–16.
Joshi, Suhas Govind; and Tone Bratteteig (2016). Designing for prolonged mastery. On involving old people in Participatory Design. In Scandinavian Journal Information Systems (SJIS), vol. 28, no 1, pp. 3–36.
Kane, Shaun K.; Barbara Linam-Church; Kyle Althoff; and Denise McCall (2012). What we talk about: Designing a context-aware communication tool for people with aphasia. In ASSETS '12: Proceedings of the 14th international ACM SIGACCESS conference on Computers and accessibility, October 2012, Boulder, Colorado, USA. New York: ACM, pp. 49–56.
Karasti, Helena (2001). Bridging work practice and system design: Integrating systemic analysis, appreciative intervention and practitioner participation. Computer Supported Cooperative Work (CSCW), vol. 10, pp. 211–246.
Kensing, Finn; and Jeanette Blomberg (1998). Participatory design: Issues and concerns. Computer Supported Cooperative Work (CSCW), vol. 7, pp. 167–185.
Kinnula, Marianne; Molin-Juustila Tonja; Iván Sánchez Milara; Marta Cortes; and Jukka Riekki (2017). What if it switched on the sun? Exploring creativity in a brainstorming session with children through a Vygotskyan perspective. Computer Supported Cooperative Work (CSCW), vol. 26, pp. 423–452.
Krogstad, Jan Magne (2011). Hva er ervervet hjerneskade?. Oslo: Konsis Grafisk AS.
Kyng, Morten (1991). Designing for cooperation: Cooperating in design. Communications of the ACM, vol. 34, no. 12, pp. 65–73.
Larsen, Simon B; and Jakob E Bardram (2008). Competence articulation: Alignment of competences and responsibilities in synchronous telemedical collaboration. In CHI 2008: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Florence, Italy, 5 - 10 April 2008. New York: ACM, pp. 553–562.
Lindsay, Stephen; Katie Brittain; Daniel Jackson; Cassim Ladha; Karim Ladha; and Patrick Olivier (2012a). Empathy, participatory design and people with dementia. In CHI 2012: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Austin, Texas, USA. New York: ACM, pp. 521–530.
Lindsay, Stephen; Daniel Jackson; Guy Schofield; and Patrick Olivier (2012b). Engaging older people using participatory design. In CHI 2012: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Austin, Texas, USA. New York, ACM, pp. 1199–1208.
Luff, Paul; and Christian Heath (1998). Mobility in collaboration. In CSCW '98: Proceedings of the 1998 ACM Conference on Computer Supported Cooperative Work. New York: ACM, pp. 305–314.
Maartmann-Moe, Harald (2019). “These things take time” Unhurried explorations and independent prototypes in participatory design with older adults. Master Thesis. Department of Informatics, University of Oslo.
Mamykina, Lena; Elizabeth Mynatt; Patricia Davidson; and Daniel Greenblatt (2008). MAHI: Investigation of social scaffolding for reflective thinking in diabetes management. In CHI 2008: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Florence, Italy, 5 - 10 April 2008. New York: ACM, pp. 477–486.
Massimi, Michael; Ronald M Baecker; and Michael Wu (2007). Using participatory activities with seniors to critique, build, and evaluate mobile phones. In ASSETS 2007: Proceedings of the 9th international ACM SIGACCESS Conference on Computers and Accessibility, Tempe, Arizona, USA, 15 - 17 October 2007. New York: ACM, pp. 155–162.
Mayer, Julia M.; and Jelena Zach (2013). Lessons learned from participatory design with and for people with dementia. In MobileHCI 2013: Proceedings of the 15th International Conference on Human-Computer Interaction with Mobile Devices and Services, Munich, Germany, 27 - 30 August 2013 . New York: ACM, pp. 540–545.
McGrenere, Joanna; Rhian Davies; Leah Findlater; Peter Graf; Maria Klawe; Karyn Moffatt; Barbara Purves; and Sarah Yang (2002). Insights from the aphasia project: designing technology for and with people who have aphasia. ACM SIGCAPH Computers and the Physically Handicapped, Issue 73–74, June-September 2002. New York: ACM, pp. 112–118.
McPhail, Brenda; Terry Costantino; David Bruckmann; Ross Barclay; and Andrew Clement (1998). CAVEAT exemplar: Participatory design in a non-profit volunteer organisation. Computer Supported Cooperative Work (CSCW), vol. 7, pp. 223–241.
Meskó, Bertalan; Zsófia Drobni; Éva Bényei; Bence Gergely; and Zsuzsanna Győrffy (2017). Digital health is a cultural transformation of traditional healthcare. mHealth, vol. 3, pp. 3–38.
Muriana, Luã Marcelo; and Heiko Hornung (2017). Towards participatory prototyping with older adults with and without cognitive impairment: Challenges and lessons learned. In Bernhaupt et al. (eds): Human-Computer Interaction - INTERACT 2017, Lecture Notes in Computer Science, vol. 10513.. Cham: Springer, pp. 344–363.
O'Connor, Cian; Geraldine Fitzpatrick; Malcolm Buchannan-Dick; and James McKeown (2006). Exploratory prototypes for video: Interpreting PD for a complexly disabled participant. In NordiCHI '06: Proceedings of the 4th Nordic Conference on Human-Computer Interaction: Changing Roles, Oslo, Norway. New York: ACM, pp. 232–241.
Orso, Valeria; Anna Spagnolli; Luciano Gamberini; Francisco Iba; and Maria Elena Fabregat (2015). Involving older adults in designing interactive technology: The case of SeniorChannel. In CHItaly 2015: Proceedings of the 11th Biannual Conference on Italian SIGCHI Chapter, Rome, Italy, 28 - 30 September 2015. New York: ACM, pp. 102–109.
Osmond, Jennifer; and Yvonne Darlington (2005). Reflective analysis: Techniques for facilitating reflection. Australian Social Work, vol. 58, pp. 3–14.
Palumbo, Rocco (2017). The Bright Side and the Dark Side of Patient Empowerment: Co-creation and Co-destruction of Value in the Healthcare Environment. Cham: Springer.
Piras, Enrico Maria; and Alberto Zanutto (2010). Prescriptions, x-rays and grocery lists. Designing a personal health record to support (the invisible work of) health information management in the household. Computer Supported Cooperative Work (CSCW), vol. 19, no.6, pp. 585–613.
Pitkin, Hanna F. (1993). Wittgenstein and Justice: On the Significance of Ludwig Wittgenstein for Social and Political Thought. Oakland: University of California Press.
Plaisant, Catherine; Aaron Clamage; Hilary Browne Hutchinson; Benjamin B Bederson; and Allison Druin (2006). Shared family calendars: Promoting symmetry and accessibility. ACM Transactions on Computer-Human Interaction (TOCHI), vol. 13, no.3, pp. 313–346.
Prigatano, George P. (1999). Principles of Neuropsychological Rehabilitation. Oxford: Oxford University Press.
Reddy, Madhu C; Paul Dourish; and Wanda Pratt (2006). Temporality in medical work: Time also matters. Computer Supported Cooperative Work (CSCW), vol. 15, pp. 29–53.
Schmidt, Kjeld; and Liam Bannon (1992). Taking CSCW seriously. Computer Supported Cooperative Work (CSCW), vol. 1, pp. 7–40.
Schmidt, Kjeld (2011). The concept of ‘work’in CSCW. Computer Supported Cooperative Work (CSCW), vol. 20, pp. 341–401.
Schön, Donald A. (1984). The Reflective Practitioner: How Professionals Think in Action. London: Routledge.
Schön, Donald A; and Glenn Wiggins (1992). Kinds of seeing in designing. Creativity and Innovation Management, vol. 1, pp. 68–74.
Schuler, Douglas; and Aki Namioka (1993). Participatory Design: Principles and Practices. New York: CRC Press.
Schütz, Alfred (1951). Choosing among projects of action. Philosophy and Phenomenological Research, vol. 12, pp. 161–184.
Simonsen, Jesper; and Toni Robertson (2012). Participatory design: An introduction. In Routledge International Handbook of Participatory Design. New York: Routledge, pp. 1-17.
Sokoler, Tomas; Jonas Löwgren; Mette Agger Eriksen; Per Linde; and Stefan Olofsson (2007). Explicit interaction for surgical rehabilitation. In TEI 2007: Proceedings of the 1st International Conference on Tangible and Embedded Interaction, Baton Rouge, Louisiana, 15 - 17 February 2007. New York: ACM, pp. 117–124.
Spiel, Katta; Emelin Brulé; Christopher Frauenberger; Gilles Bailly; and Geraldine Fitzpatrick (2018). Micro-ethics for participatory design with marginalised children. In PDC '18: Proceedings of the Participatory Design Conference, Hasselt and Genk Belgium, Full Papers-Volume 1. New York: ACM, pp. 1-12.
Star, Susan Leigh; and Anselm Strauss (1999). Layers of silence, arenas of voice: The ecology of visible and invisible work. Computer Supported Cooperative Work (CSCW), vol. 8, pp. 9–30.
Suchman, Lucy (1993). Do categories have politics? The language/action perspective reconsidered. In ECSCW’93. In Proceedings of the Third European Conference on Computer Supported Cooperative Work, Milan, Italy, 13–17 September 1993. Dordrecht: Springer, pp. 1–14.
Sunnaas, Sykehus (2017). Sunnaas Rehabilitation Hospital – A Way Forward. https://www.sunnaas.no/Documents/Brosjyrer/Sunnaas_Rehabilitation_Hospital_a_way_forward.pdf Accessed February 2020.
Talamo, Alessandra; Marco Camilli; Loredana Di Lucchio; and Stefano Ventura (2017). Information from the past: How elderly people orchestrate presences, memories and technologies at home. Universal Access in the Information Society, vol. 16, pp. 739–753.
Tellioğlu, Hilda; and Ina Wagner (2001). Work practices surrounding PACS: The politics of space in hospitals. Computer Supported Cooperative Work (CSCW), vol. 10, pp. 163–188.
Thaler, Richard H; and Cass R. Sunstein (2009). Nudge: Improving Decisions about Health, Wealth, and Happiness. Westminister: Penguin Books.
Thoresen, Kari (1993). Principles in practice: two cases of situated of Participatory Design. In Participatory Design: Principles and Practices. New York: CRC Press, pp. 271-287.
Toglia, Joan (2003). Cognitive-perceptual retraining and rehabilitation. In Willard and Spackman’s Occupational Therapy, pp. 607–629.
Toglia, Joan (2005). A dynamic interactional approach to cognitive rehabilitation. Cognition and Occupation Across the Life Span: Models for Intervention in Occupational Therapy, vol. 2, pp. 29–72.
Turner-Stokes, Lynne (2008). Evidence for the effectiveness of multi-disciplinary rehabilitation following acquired brain injury: A synthesis of two systematic approaches. Journal of Rehabilitation Medicine, vol. 40, pp. 691–701.
Vines, John; Roisin McNaney; Rachel Clarke; Stephen Lindsay; John McCarthy; Steve Howard; Mario Romero; and Jayne Wallace (2013). Designing for-and with-vulnerable people. In CHI‘13 Extended Abstracts on Human Factors in Computing Systems, Paris, France, 27 April 2013- 2 May 2013. New York: ACM, pp. 3231–3234.
Vines, John; Róisín McNaney; Stephen Lindsay; Jayne Wallace; and John McCarthy (2014). Special topic: Designing for and with vulnerable people. Interactions, vol. 21, pp. 44–46.
WHO, World Health Organisation (2017). Disability and Rehabilitation. https://www.wcpt.org/node/31113
Willis, Jerry W; Muktha Jost; and Rema Nilakanta (2007). Foundations of Qualitative Research: Interpretive and Critical Approaches. Sage Publications.
Wilson, Barbara A. (2002). Towards a comprehensive model of cognitive rehabilitation. Neuropsychological Rehabilitation, vol. 12, pp. 97-110.
Wilson, Barbara A; Fergus Gracey; Jonathan J Evans; and Andrew Bateman (2009). Neuropsychological Rehabilitation: Theory, Models, Therapy and Outcome. Cambrige: Cambridge University Press.
Wooffitt, Robin (2005). Conversation Analysis and Discourse Analysis: A Comparative and Critical Introduction. Sage Publications.
Wu, Mike; Brian Richards; and Ron Baecker (2004). Participatory design with individuals who have amnesia. In PDC 2004: Proceedings of the Eighth Conference on Participatory Design: Artful Integration: Interweaving Media, Materials and Practices – Volume 1, Toronto, Ontario, Canada, 27 - 31 July 2004. New York: ACM, pp. 214–223.
Wu, Mike; Ron Baecker; and Brian Richards (2005). Participatory design of an orientation aid for amnesics. In CHI 2005: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Portland, Oregon, USA, 2 - 7 April 2005. New York: ACM, pp. 511–520.
Wu, Mike; Ron Baecker; and Brian Richards (2010). Field evaluation of a collaborative memory aid for persons with amnesia and their family members. In ASSETS 2010: Proceedings of the 12th International ACM SIGACCESS Conference on Computers and Accessibility, Orlando, Florida, USA, 25 - 27 October 2010. New York: ACM, pp. 51–58.
Acknowledgements
We are grateful to all of our workshop participants and value their contributions to the insights gained. Finally, thanks are due to the Sunnaas domain experts, who had an essential role in planning and facilitating the workshops.
Funding
Open access funding provided by Ostfold University College The project presented here was, in part, financed by the INTERREG Sverige-Norge project ‘VITAL – för den goda hälsan’ under grant number 20202391.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interests/Competing interests
There are no underlying conflicts or competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Çarçani, K., Bratteteig, T., Holone, H. et al. EquiP: A Method to Co-Design for Cooperation. Comput Supported Coop Work 32, 385–438 (2023). https://doi.org/10.1007/s10606-023-09463-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10606-023-09463-w