Abstract
In this study, we examine to what extent availability of a crisis center in a behavioral health district is related to changes in emergency hold petitions and outcomes of those holds as submitted by police officers. Using data from between 2010 and 2020 and a series of interrupted time series analysis, we analyze 22,619 police petitions for involuntary commitment and their outcomes related to crisis center availability. Results show inconsistent and varied effects between availability of a crisis center and emergency hold petitions. Similar results are observed for the emergency hold evaluation process outcome and associated final disposition outcome. The implementation of crisis centers in the study site may not have achieved the immediate goals of reducing the use of the emergency hold petitions nor relevant outcomes. The results vary in direction and magnitude indicating there is more research to be done to understand if, and how, crisis center availability and use are associated with changes in the involuntary emergency hold system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Police hold a unique position as boundary spanners intersecting public safety and public health. The quintessential ‘node’ where this intersection is readily observable are those involving serious mental health. Over the last two decades, concerted efforts have been made to improve mental health responses by improving officer awareness (Comartin et al., 2019; Hacker & Horan, 2019; Soares & Pinto da Costa, 2019; Wise et al., 2019), decision-making by way of crisis intervention training and mental health first aid (Comartin et al., 2019; Dalton et al., 2018; Kane et al., 2018; Watson et al., 2010, 2017), and modifying the interaction through some co-responding model (i.e., where an officer is co-deployed with a behavioral health expert, or where a behavioral health expert is deployed prior to an officer). Research shows mixed results (Borschmann et al., 2010; Kane et al., 2018; Shapiro et al., 2015; Taheri, 2016; Teller et al., 2006), though largely results show improvements can be made in officer awareness, decision-making, and diversion when such interventions are targeted, leveraging a holistic response (Carson & Wellman, 2018; Chester et al., 2016; Enang et al., 2019; Ullman, 2022; Wood, 2020). Embedded within this holistic response is the importance of examining and documenting the influence of public health interventions (Pepler & Barber, 2021; van Dijk et al., 2017; van Dijk et al., 2019; White, 2021; Wood, 2020), which in concert with training and co-responding models could further complement improving police responses to serious mental health issues.
In 2018, Makin and colleagues examined the emergency hold (EH) petition process (involuntary civil commitment) in the state of Idaho. Results of this research revealed the use of the EH petition on the part of police officers were among the lowest of the qualified petitioners with 49% of petitions evaluated as congruent (p. 12). Interpretation of this result engaged research suggesting the outcome may be a result of population differences introducing bias when interpreting variability across petitioners, a training effect, wherein the diffusion of crisis intervention team training and messaging inadvertently conveyed a “when in doubt call” effect increasing petitions and decreasing rates of congruence, and lastly, the authors explored research suggesting expanding the officer “toolkit”, through non-legal means, suggesting the availability of community resources could improve the use of emergency hold petitions on the part of police officers.
In 2014, the Idaho legislature funded crisis centers as a community health intervention. Each of the seven behavioral health districts in Idaho employs a version of a crisis center. Six districts use standard crisis centers to supply substance use disorder and mental health services. These six centers are augmented by a Rural Crisis Center Network with three locations in more remote communities. Idaho staggered the implementation of these crisis centers, with the first center launching in December of 2014 and the final one in November 2019. Building from the work of Makin and colleagues (2018), this research examines if, and to what extent, the availability of a crisis center within a behavioral health district is associated with measurable changes in police officer emergency hold petitions, rates of congruence with court-ordered examiners, and petition outcomes, including the rate of dismissal and individuals committed. In what follows, we turn our attention to an overview of the literature associated with the intersection of public health and public safety, the emergency hold petitions or involuntary civil commitment process, responses implemented in the public safety sector, and the state of research on crisis centers as a community health intervention.
Literature Review
At the center of interest in the literature on the intersection of serious mental illness (SMI) and policing is the awareness of increased interactions between the two groups (SMI individuals and police). Bittner’s seminal work on mental health policing (1967) conceptualizes “skid-row” as a strange primordial place full of problematic people and relegates their containment to the police. The mythos of skid-row catches and contains all of the disorder of society and shifts the policing model from law enforcement to “peace keeping.” The author found that police are reluctant to make referrals or intervene with SMI crisis calls unless the individual shows considerable evidence of SMI (Bittner, 1967). Another article conceptualizes the increase of police interactions with SMI individuals around deinstitutionalization, a reduction of mental health care, and more rigorous legal standards for involuntary commitment to psychiatric hospitals (Boyd & Kerr, 2016). Police as “streetcorner psychiatrists” have less options to help SMI individuals, and people with SMI have more options for staying out of treatment and help. The research finds that whether officers choose to refer, commit, or arrest individuals with SMI largely comes down to officer discretion and available options (Teplin & Pruett, 1992).
Involuntary Commitment and Relevant Legislation
The modern precedent for involuntary commitment to a psychiatric hospital comes from the Lanterman-Petris-Short Act (LPSA) of 1967. Written as a California state law by State Assemblyman Frank Lanterman with help from State Senators Nicholas Petris and Alan Short, the idea of the legislation spread to other states in America, and other states wrote and enacted similar legislation (Stone, 1975, pg. 60). The criteria for involuntary commitment in the LPSA are simple:
1) Danger to self—this criterion most often involves threats of self-harm or suicide,
2) Danger to others—this criterion most often involves threats or attempts to harm others,
3) Gravely disabled—this criterion most often involves inability to take care of oneself through eating enough food or maintaining proper housing (Warren, 1977).
A police officer or mental health clinician can recommend someone meeting any of these criteria for initial 5150 hold, which means the individual showing signs of SMI can be held for up to 72 h. During this hold, mental health professionals will further examine the individual. If a mental health professional finds the person needs additional treatment, or will be unwilling to receive voluntary treatment, a second hold (5250) can be filed for the SMI individual to be held for up to 14 days (California Office of Patients’ Rights, 2018).
Street-Level Policing SMI Tactics
Street Triage
An interesting policing model in the UK that is being investigated is called “street triage.” The goal of street triage is lowering s136 detentions. A psychiatric nurse attends potential s136 calls with a police officer to supply immediate care, or to refer to other pathways of care when necessary. Oftentimes, psychiatric nurses are stationed at the police station, where they can screen calls and attend s136 calls with police (Dyer et al., 2015; Rodgers et al., 2019). In one study, the street triage model in a single constabulary involved the following: a dedicated officer and psychiatric nurse who would attend s136 calls, a dedicated unmarked vehicle for the team, and designated uniforms—a standard police uniform and a lanyard and arm band designating the nurse. During the trial time for this study, s136 detentions dropped by 39% (Heslin et al., 2016). Because street triage cuts down on the amount of s136 detentions, it cuts down the money associated with them as well. One study found that over an eighteen-month period, the police force made 558 s136 detentions, while a street triage team for the same department made only 13 detentions. The cost difference of this is quite significant, amounting to £993,240 for the police force compared to just £23,140 for the street triage team (Dyer et al., 2015).
Dyer et al. (2015) comment on a few challenges to street triage, noting “self-presenters,” repeat referrals, and tension between agencies. Self-presenters are people who present willingly to police for help but are taken to the hospital during times when the street triage team is unavailable. Some officers were noted for bypassing the street triage team altogether, opting for a quicker route of dealing with the problem. A similar problem are the repeat referrals. Although street triage helps people overcome their problems related to mental health crisis or substance misuse, it doesn’t incentivize them to make lasting change (Comartin et al., 2019). Finally, the tension between agencies has to do with disagreement about what needed to be done. An existing model before street triage (crisis teams) was seen as the paragon of providing mental health crisis assistance for the police, but the crisis teams were phased out. Street triage and the model that not everyone needs to be detained is not a model that all cooperating agencies (police, medical and mental health professional, social services) agree with (Dyer et al., 2015).
Crisis Intervention Teams and Co-Responding Units
The idea for co-response is that mental health professionals either offer assistance over the phone or are dispatched to the call with officers to help on location; this is similar to the street triage model in the UK (Dyer et al., 2015). Co-response is believed to increase cooperation between police agencies and mental health providers and increases police knowledge of mental illness as a byproduct rather than overt training. Similar to the CIT model, the idea is to have a specially trained officer and mental health professional on a shift to ease up call volume for other officers on the shift (Lamanna et al., 2018). While plenty of research has been done on the CIT model, the co-responding model is lacking in the amount of literature available (Boscarato et al., 2014; Shapiro et al., 2015). A meta-analysis on the co-responding units model found that while mental health providers felt safer answering mental health calls with officers, law enforcement officers did not feel that the co-response was necessary. The co-responding model has been found to lower arrest rates for SMI individuals, and lower time spent on calls, but it is not the perception of some officers in co-responding units (Boyd & Kerr, 2016; Shapiro et al., 2015). More research has been called for on co-responding units (Forchuk et al., 2010).
One study on co-responding units determined that men and women in mental health crisis used the crisis response option almost evenly in their sample (50% and 48% respectively). Of diagnoses uncovered from the data, psychotic disorders ranged among the highest (42.9%), and nearly a third of the sample were repeat consumers of the program (29.9%). Co-responding units were more likely to escort people on their calls to a psychiatric hospital than police-only units, but police-only units were more likely to initiate involuntary holds from their calls (Lamanna et al., 2018). Another unit found that co-responding units both increases the hospitalization and involuntary commitment of SMI individuals, as well as decreases use of force incidents. It increases referral to community resources and helps people find help within their own social network (Blais et al., 2020).
Crisis Centers
Central to the police intervention models for people with SMI are crisis centers. A policy analysis of Vancouver Police Department’s response to mental health service calls found that the police were more interested in increased police presence in the area of the mental health calls rather than community resources for SMI individuals. The justification for this is so that those visiting and living in the area would feel safer. This model and justification came at the ignoring of multiple community services available for individuals with SMI (Boyd & Kerr, 2016). Rather than focusing on a paradigm of competition between the police and a transient population of individuals with SMI, the public health literature shifts to a focus community resources and recovery as the priority. The principle of this model is to relieve care from psychiatric and specialist care, and shift focus to primary care. However, recovery is not a standard measure for care, and so mental health consumers may experience disparate outcomes, resulting in a variety of outcomes on a community level (Battersby & Morrow, 2012). A collaborative community level of recovery, coupled with a chronic illness model of care, has been a public health exhortation for over fifteen years (Jacobson & Greenley, 2001; Lester & Gask, 2006).
An alternate point of contact for individuals with SMI apart is through calling a crisis hotline (Ingram et al., 2007). The crisis hotline can alert crisis services, which can then respond to the mental health crisis, and then take the individual with SMI to the physical location—the crisis center (Steadman et al., 2001). A systematic review found no standard measure of what a “frequent” caller is, and mixed results of how studies of crisis hotlines define. Some were as low as eight times a month, but some thresholds were as high as twenty times a month. Analysis of covariates of frequent callers find suicidality and self-harm were commonly found with frequent callers, as well as anxiety and panic disorders. Other covariates included loneliness, physical illness or disability, and having seen a psychiatrist in the last month (Mishara et al., 2022). Further hotline studies have found an increase of calls to crisis hotlines in the wake of the COVID-19 pandemic and restrictive government lockdowns. The pandemic has influenced mental health, and the rise in crisis hotline volume shows this (Arendt et al., 2020). Three out of four callers to a hotline were found with newly onset anxiety or insomnia from fear of exposure to COVID-19. The hotline was able to refer 86% of callers who needed help to telehealth options for mental health counseling (Abdullah et al., 2021).
The availability of care through crisis centers is on the rise. A study of crisis centers from 2001 to 2007 found an increase in the number of centers, and the amount of people receiving services from them. A total of crisis centers between 2001 and 2007 rose from 748 to 1067, and the service reach increased from 1,223,408 to 2,738,408 encounters. The same study found that by 2007, 77% of these crisis centers offered mental health services, 51% offered substance abuse treatment, but only 20% offered 24-h crisis intervention services (Wells et al., 2010). While crisis centers are a common and expanding mode of service for helping people in crisis, there is a lack of literature on them. One study referred to them as the “black box” of the service sector (Edmond et al., 2020). This may be from the small and community nature of these centers, or that taboo nature of the services they provide. Crisis centers specialize in a service for those who need it—the most common of these centers are mental health crisis (most commonly suicide or self-harm), substance abuse problems, or victims of rape or sexual violence (Forchuk et al., 2010; Steadman et al., 2001).
The Impact of Crisis Centers
The impact of crisis centers in particular is hard to conceptualize on a community level. It is easy to talk about their need in the terms of mental health crisis and SMI, but it is hard to generalize about their impact. Other measures of lack of availability of mental health and psychiatric care and their impact are worth considering here. A study suggested a general shortage of mental health professionals. An estimate of 18% of counties in America had some unmet need in terms of mental health care, and 77% of counties lacked mental health prescribers (psychiatrists; Thomas et al, 2009). In the same study, this unmet need corresponded with rural areas of America, while met need corresponded with areas of America with higher income (Thomas et al., 2009). One study conceptualized availability of psychiatric care as availability of psychiatric beds, and conceptualized rates of SMI as suicide rates. A decrease of one available psychiatric bed per 100,000 individuals resulted in an estimate of a decrease of 1818 beds nationwide. The estimate of decrease of one psychiatric bed corresponded with 45 suicides per year (Yoon & Bruckner, 2009).
The availability of these crisis centers is critical in helping individuals in crisis. A systematic review of prearrest diversion for individuals in mental health crisis found that those who received help at crisis centers were more likely to be prescribed medication and receive counseling for their mental illness. However, arrest outcomes were inconclusive, as one intervention group showed reduced risk for arrest, while others showed increased risk for arrest. (Schucan Bird & Shemilt, 2019). A review of three crisis centers showed estimates between 450 and 1150 people came through the crisis centers each year, and that 20–70% of those that came through the centers were referrals or direct transports from police officers. While the review did not provide direct outcome measures, the high amount of people coming through the crisis centers, and especially the referrals or direct transports from law enforcement suggest that the police-community collaboration can be a success. The effective principles outlined in the review are central crisis center location, police-friendly procedures (no refusal and quick intake), legal underpinnings to make police referral and access simple, training for mental health professionals and law enforcement (mostly referring to the CIT training here), and referral of SMI individuals to community resources after their crisis center experience (Steadman et al., 2001).
Mental Health and Crisis Centers in Idaho
Idaho is divided into seven regions for public health purposes, and therefore has seven major crisis centers. These are the Northern Idaho Crisis Center (NICC) in Coeur d’Alene; the Pathways Community Crisis Center of Southwest Idaho (PCCCSI) of Boise; The South East Idaho Behavioral Crisis Center (SEIBCC) of Pocatello; the Rural Crisis Center Network (RCCN), which is spread across five counties just south of the panhandle of Idaho, including Latah, Nez Perce, Lewis, Idaho, and Clearwater counties; the Crisis Center of South Central Idaho (CCSCI) of Twin Falls, Idaho; the Western Idaho Community Crisis Center (WIDCCC) of Caldwell, Idaho; and the Behavioral Health Crisis Center of East Idaho (BHCC) of Idaho Falls, Idaho. The data for these crisis centers do not appear consistently collected by the IDHW. Table 1 covers the data put forth in the 2021 State Behavioral Health Planning Council Governor’s Report. The 2021 State Behavioral Health Planning Council Governor’s Report seems to be the available report for any collection of crisis center data from 2020 and 2021 (State of mind, 2021). Other reports from individual crisis centers were encountered, but they were either from a different year, or only for a certain quarter of 2020 or 2021 (2016 annual report, 2016; Quarter Four 2020–2021, 2021; 2nd quarter report, 2021).
Other variables collected by different crisis centers according to the report included total admission and non-episode contacts, percentages of referral sources (i.e. self-referred, hospital, or law enforcement), type of admission (mental health crisis, substance use, or sexual violence), average stays for different types of referrals, average square miles that the crisis center covered, contacts helped via telephone, admission decreases, and admission screening categories (mental health crisis, co-occurring disorders, substance use). According to the 2021 Governor’s Report, the WIDCCC submitted decreased admission rates but not total admission rates, and only the PCCCSI provided cost savings rates. The PCCCSI estimated that their services saved an average of $1000 per mental health call for the police. This estimate was based off the costs to dispatch four officers, one fire truck, and one ambulance, as well as a transport to a hospital (State of mind, 2021).
Idaho seems committed to treatment of SMI through psychiatric hospitals. In May 2021, State Hospital West (SHW) opened in Nampa. This new hospital (SHW) is an adolescent unit, designed to treat patients ages 12–17. This unit replaced the adolescent unit at State Hospital South (SHS) in Blackfoot, which used the new space to free up more beds to treat more individuals with SMI. There are three psychiatric hospitals in Idaho—SHW, SHS, and State Hospital North (SHN), which is in Orofino. State Hospital West is the smallest of the hospitals, is the only adolescent-specific hospital, and has 16 beds, SHN is the next largest with 60 adult beds, and SHS is the largest hospital, with 110 adult beds, and 42 skilled nursing home beds (Jeppeson et al., 2021). Idaho has a hotline called “2-1-1 Idaho Careline” for referring individuals who need crisis care or community resources. Idaho also has the Idaho Suicide Prevention Hotline, which is a state-specific hotline that individuals in crisis can call or text message. (Idaho crisis & suicide hotline, 2022; Sewell, 2020). The Idaho Suicide Prevention Hotline has had approximately 81,000 contacts since 2012 (State of mind, 2021). Notably, Idaho plans to launch a crisis line for behavioral health crisis and suicide prevention in July 2022. This hotline (9-8-8) will help those in crisis find community resources and access to treatment during their crisis and ongoing treatment for mental health problems (Hadley, 2022; State of mind, 2021). For monthly data by region on police and medical holds from 2019 to the current month, please review the mental health public dashboards available through the IDHW Division of Behavioral Health (Mental health dashboards, 2022).
Methods
In partnership with the Idaho Department of Health and Welfare Division of Behavioral Health, data for this study represent emergency hold petitions, as made by police officers between 2010 and 2020. These measures are monthly and were labeled by the Behavioral Health District where the petition originated. There were 22,619 petitions submitted by police officers. Table 2 provides the descriptive statistics associated with petitions made, the percentage of petitions evaluated as not meeting the legal criteria for an involuntary hold, the number of outcomes dismissed, and total number of petitions where the disposition resulted in a commitment. As the purpose of this research is to document to what extent the availability of a crisis center within a behavioral health district is associated with changes in petitions for emergency holds, as made by police officers, the independent variable is the date the crisis center was active. As a layer of obfuscation, we present the year the crisis center was available for each behavioral health district, though the specific month of operational availability is included in each model. Due to the staggered rollout, three of the behavioral health district crisis centers were not implemented until 2019 leaving a limited period of observation suitable for analysis. The Washington State University (WSU) institutional review board approved the protocol used in the study. There are no known conflicts of interest, and all authors certify responsibility for the material contained in the study.
Analytical Plan
Given the purpose of this research is documenting if, and to what extent, the availability of a crisis center is associated with changes in the use of emergency hold petitions by police officers, we employ interrupted time series analysis (ITSA). Developed by Linden (2015), ITSA relies on ordinary least squares (OLS) regression and is available as a downloadable package in Stata. All models were analyzed in version 17 of Stata. Linden (2015) defines the single group and multiple-group interrupted time-series analysis regression series model as follows:
Single Group
As described by Linden (2015) and as summarized by Makin and Bowers (2020), Yt is the emergency hold petition outcome and is measured monthly (t). Xt is the intervention (date the crisis center is available), and XtTt signifies the interaction between the time measurement and the intervention. β0 represents the intercept, or starting point, which is January 2010. β1 assesses represents the slope between the intercept and the availability of the crisis center. β2 indicates the effect of the immediate effects of the implementation, β3 while represents the difference immediately following the intervention. For ease of interpretation, there are three primary variables of interest _t (trend prior to implementation), _x (direct effect of the implementation), and _xt (post intervention trends).
Multi-Group
As described by Linden (2015), and as summarized by Makin et al, (2021), Yt is the outcome variable at each time point, the first four terms (β0 through β3XtTt) represent the comparison group, and the last four terms (β4 through β7ZXtTt) represent the interaction of the treatment group. β0 is the starting point, or intercept, of the outcome variable for the comparison group, whereas β4Z represents the difference in starting points between the comparison group and the treatment group. Tt is the variable for how many time units (in this analysis months) have passed since the initial measurement. Xt is a dummy variable used to indicate the intervention, where any time at or after the time of intervention is 1 and everything before the intervention is 0. XtTt0 is an interaction term between the time measurement and the intervention. Z is a dummy variable to indicate the treatment group (1) and the comparison group (0). The final three terms in the model are the interaction of the treatment group with the regression terms previously described. β5 through β7 indicate the difference between the comparison group and the treatment group outcome variable slopes prior to the intervention, immediately following the implementation of the intervention, and over time post-intervention. All models are adjusted to account for heteroskedasticity issues and seasonality using the Prais transformation command and monthly controls.
Unfortunately, given the staggered nature of the rollout of the crisis centers in Idaho, and as depicted in the descriptive statistics, many of the behavioral health districts are not comparable, nor suitable for synthetic controls. As such, we were unable to employ a multi-group ITSA. Several alternative modeling approaches were tried, though there were concerns over biased estimates. For example, we suppressed the years 2019 and 2020 from the period of analysis to compare BHD C and BHD D (note BHB C deployed a crisis center in 2019). The initial mean level difference and mean baseline slop are significantly different indicating BHB C is not comparable with BHB D. However, this solution did allow for comparison of BHD G and BHD F. For ease of presentation, we present the results of the single group ITSA, and discuss the supplemental analysis in the text.
Results
The availability of a crisis center in a behavioral health district does not show consistent effects on the use of emergency hold petitions. Table 3 depicts the trends in emergency hold petitions made by police in four of the seven behavioral health districts and the immediate and post-intervention trend associated with the availability of the crisis center. Results show there are regional variation in the trends, with two of the four behavioral health districts (A & D) showing an upward trend in petitions prior to availability and two showing decreasing trends (E and G). Marginal significance is associated with the immediate effect of the availability of the crisis center in BHD E, showing a decrease the month of availability (− 2.98, p < 0.10). The post-trend shows mixed results with a decrease in petitions by police in BHD A, an increase in BHD G, and no effect in the remaining districts. The transformed Durbin-Watson statistics corrected issues with autocorrelation showing slight positive autocorrelation for three of the four districts with slight negative autocorrelation for BHD G (Durbin-Watson Statistics should be close to a value of 2).
Recall prior research finds that petitions for emergency hold are more often evaluated by designated examiners as negative (see, Makin et al., 2018). Given crisis centers are believed to act in a diversionary manner, it has been hypothesized the availability of a crisis center would be associated with decreases in the percentage of petitions deemed negative. Table 4 shows the results of the ITSA demonstrating there are no immediate or post-intervention trends associated with the availability of a crisis center. These results are consistent across all of the behavioral health districts.
As shown in Table 5, increasing trends in emergency hold petitions dismissed by a judge were associated with two of the four districts (A and D). The immediate effect of a crisis center shows a substantial decrease in district D (− 2.31, p < 0.05), though was not associated with a post-intervention trend. However, district A did not experience an immediate intervention effect, though shows a decrease in petitions dismissed (− 0.06, p < 0.001).
Lastly, we looked at changes in disposition. Specifically, if the availability of a crisis center is associated with changes in commitment. As shown in Table 6, results are mixed with effects documented across each behavioral health district, though the direction and magnitude of those effects vary. Trends in district A do not show an immediate intervention effect, though the availability of a crisis center in the district is associated with slight decreases in the use of commitment (− 0.04, p < 0.05). District D shows an increasing pre-intervention trend (0.09, p < 0.001), and a decreasing post-intervention trend (*0.011, p < 0.10). District E shows an inverse with a decreasing pre-intervention trend (− 0.04, p < 0.001), and an increasing post-intervention trend (0.04, p < 0.001). Lastly, District G shows a decreasing pre-intervention trend (− 0.08, p < 0.001), an immediate intervention effect (0.91, p < 0.10), and an increasing post-intervention trend (0.08, p < 0.02).
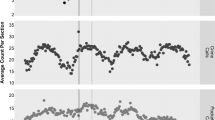
Results of the multiple-group ITSA, comparing Districts G (Control) and F (Intervention) show no effect at the month of the intervention or the post-trend intervention in comparison to the control. However, there is an immediate effect at the month of the intervention, when compared to the control, showing an immediate decrease (− 0.33, p < 0.01). There is no detectable influence of the availability of a crisis center and changes in petitions dismissed, nor committed. These results show the importance of integrating an equivalent control group into the analysis, as the single-group ITSA indicated marginal effects that were statistically significant. The use of commitment was decreasing at equivalent rates for both districts, and flat post the intervention. Figure 1 visualizes the patterns for the respective districts.
Discussion
The goal of this study was to explore the effect of the availability of a crisis center on police officer petitions for emergency holds in Idaho. Results show mixed associations on the availability of crisis centers in a behavioral health district. In terms of the level and slope of the intervention, results are marginal, though there are clear variation across districts with reductions in petitions in one district and an increasing trend in another. Placing these results within the existing body of literature further supports the importance of isolating and examining the contexts and constraints associated with individual decision-making on the part of the officer. As Woods and Beierschmitt (2014) explored in their mixed-method study of officer decision-making, context matters (p. 446). They argue that it is critical to link knowledge systems, including the street level knowledge of officers doing the direct engagement and the knowledge from organizational data systems (p. 446).
As with other situations, officers have an array of options to choose from as they handle situations and make decisions during mental-health related encounters. Early research by Bittner (1967) suggests that police conduct “psychiatric first aid” and act as situational problem solvers with the goal of providing safety and normalcy to a given encounter. To do so, officers engage in a process of communication and interaction. This interaction is inevitably impacted by various contextual factors all complicated by the intersection of law enforcement and mental health/social services in which police operate. Practically, police deal with a range of situations and serve people with a range of needs from day-to-day. The decision police make to transport an individual to a crisis center rather than submitting them for an emergency mental health hold or vice versa could be guided by their desire and discretion to minimize the negative conditions of their work (Lipsky, 2010). For example, Charette et al. (2014) found that police interventions involving individuals with mental illnesses used 87 percent more resources than interventions involving those without, and their analysis included the calculation of time spent in response to both populations. The impact of the daily realities on police work and decision-making, in this case the utilization of crisis centers as a diversionary option instead of emergency services, should further be explored by incorporating the perspective of those conducting the work on the ground.
Another practical explanation in understanding this phenomenon includes the impact of training on police decision-making during encounters involving people with mental illnesses. Although as described in previous sections, the effectiveness of CIT training has been explored, other training and guidance provided to officers must be understood to understand how officer’s make decisions in each situation. This point is noted by Krameddine and Silverstone (2015) who argue that the focus of trainings and evaluations of those trainings needs to be on changing behaviors rather than just attitudes towards people with mental illnesses. Bahora et al. (2008) who distributed surveys to analyze the impact of CIT training on police self-efficacy and social distance also suggest that more research is needed on officer level outcomes. Analyzing the impact of police training on in-field behavior change is difficult for numerous reasons. Notably are the qualitative methodological challenges in terms of gaining access to such population (Nix et al., 2019) and the complexity and inconsistencies across policing-mental health databases (Earley, 2007). Police agencies vary in terms of trainings provided to officers and resources expended on certain concerns. The current study and the findings highlight the need to analyze and evaluate the training (formal) and guidance (informal) officers receive across the state of Idaho regarding the use of emergency holds versus crisis centers. Further, the priorities and approaches to responding to individuals with mental illnesses within each agency exist against a backdrop of several other contextual factors—including the availability of a crisis center.
To conceptualize the extent of contextual influences on police decision-making during encounters with people who have mental illnesses, Morabito (2007) (drawing on Bittner, 1967) suggests that three different contextual layers (referred to as horizons) come into play; scenic, temporal, and manipulative horizons. The scenic horizon incorporates the characteristics of the community, offender and incident shaping an officer’s discretion. In this case, the frequency of repeat contacts and the nature of the relationship that has been established between the police and a specific individual could influence the outcome of the situation. The temporal horizon includes police knowledge that goes beyond the specific incident. For example, this may include officer knowledge of resource availability. Although crisis centers exist as a physical location, officers may be in tune to bed and/or staffing shortages that impede meeting the immediate needs of the individual. The working relationships with involved agencies (police, crisis center staff and emergency services staff) may also factor into decision making at this level.
Lastly, the manipulative horizon involves the immediate incident and officer/community safety concerns. It is possible that police are interacting with a different population that is not suitable for a crisis center. This decision may be influenced by an officer’s concern for community or their own safety during the encounter. If an individual is causing an immediate disruption, the officer’s choice may be reflective of the quickest solution to the problem. Being that a major role of the police is to respond to calls for service and issues that arise within the community, if the situation warrants police attention it may be indicative of more severe situations. The mixed results of the current study indicate that the implementation of crisis centers does not result in consistent decreases in negative petitions for emergency mental health holds across the regions, highlighting the need to explore the impact of contexts. To better understand why, how, and in what way officers decide to utilize diversionary options requires a mixed method approach, informed by our current results. Transitioning to a qualitative approach will provide valuable insight to the inconsistency observed in the present findings.
The overlap between criminal justice, specifically policing, and mental health domains has been extensively noted, demonstrating the need for research that thoroughly explores the complexity of this intersection. The current study contributes to empirical research and practical efforts by further aligning policing and public health discussions aimed at improving the handling, treatment, and processing of people with mental illnesses.
Limitations and Future Research
While our results do not find a direct effect on the availability of crisis centers on police officer petitions for emergency holds, there are limitations that must be considered when interpreting these results. First, these data are monthly measures lacking individual and situational variables that may reveal the conditions under which there may be an effect. That is, the convergence of individual level characteristics and environmental factors or what Wood and Beierschmitt (2014) identify as a transition from “places” to “cases” may reveal situations where the availability of a crisis center contributed to improved officer decision-making. Relatedly, a critical missing data point is the use of the crisis centers, which is a required element to study diversion. It is possible the availability of a crisis center is acting to divert individuals from this formal process, though our inability to track individuals obscures the impact. For the present study, we were unable to track the number of admissions to each crisis center, nor track individual pathways. For example, when analyzed at the individual level, it would be possible to examine how an individual moves within and between the crisis center and emergency hold systems. Research capable of engaging these data sets would enable examinations isolating under what conditions crisis center availability improves individual outcomes—reducing the cycling individuals experience between the public safety and public health systems.
The integration of public health and public safety data sets would allow for a more direct measure of relationships between crisis centers in a community and individual level outcomes. Wood and Watson (2017) introduced the importance of integrated data sets in better isolating and documenting the effects of interventions aimed to improve interactions and outcomes of those impacted by mental illness. Embedded within these data sets is a need to redefine organizational success (Garland, 2012) modifying data collection practices to standardize and collect outcome measures beyond the use of the system to expand to the reliable collection of measures associated with the experience. Krameddine and Silverstone (2015) included data elements specific to police, and while their study focused on improving training efficacy, it demonstrates the importance of data collection across the process to better understand the predictors associated with the decision to petition an individual for an emergency hold and the decision to refer a person to the crisis center. Our inability to engage the crisis center data, nor track individuals as they transition within and between the community health and public safety is a limitation of the present study, and a key area of future research.
Conclusion
The last two decades have experienced a concerted effort to improve police interactions and outcomes associated with those experiencing serious mental illness. As boundary spanners, police officers and their organizations become tasked with making critical decisions that directly influence the trajectory of a vulnerable population. Police organizations, by their very nature, focus on short term results because they are both immediate and practical—given their operating constraints. The availability of a crisis centers was believed to impart an expansion to the officer ‘toolkit’ affording officers a diversionary outlet in lieu of a formal legal process. While our results are mixed, they supply a direction for future research moving beyond an “if” analysis to examine “when” the availability of a crisis center influences the interaction and outcome of these contacts. There is an increasing call to reimagine policing within a public health lens (see. Bucerius et al., 2021). Embedded within this public health ideology is a reorientation towards holistic responsivity that is outcome focused on the individual (the case management approach), leverages improvements in local community resourcing, is contextually aware, innovative (looking to improve processes and outcomes) and mindful of equity.
The implementation of crisis centers in Idaho may not have achieved the immediate goals of diversion from the emergency hold system, though this is a crucial step towards investing in communities. This research is a first of many that will explore the direct and indirect effects of crisis center availability on police practice or public safety more broadly. As data collection efforts improve and can be supplemented with primary data collection at the officer level, it will allow for a better understanding around when and how crisis centers are associated with improvement by focusing on individual level outcomes and disrupting the cycling involving those with serious mental health illness who interact with the police.
References
2016 Annual Report. (2016, December 7). Behavioral Health Crisis Center of Idaho Falls. Retrieved June 7, 2022, from https://www.eastidahocrisis.com/storage/app/media/
2nd quarter report. (2021, August 25). Latah Recovery Center. Retrieved June 7, 2022, from https://latahrecoverycenter.files.wordpress.com/2021/09/2021-2nd-quarter-report.pdf
Abdullah, H., Lynch, S., Aftab, S., Shahar, S., Klepacz, L., Cristofano, P., Rahmat, S., Save-Mundra, J., Dornbush, R., Lerman, A., Berger, K., Bartell, A., & Ferrando, S. J. (2021). Characteristics of calls to a COVID-19 mental health hotline in the first wave of the pandemic in New York. Community Mental Health Journal, 57(7), 1252–1254. https://doi.org/10.1007/s10597-021-00868-9
Arendt, F., Markiewitz, A., Mestas, M., & Scherr, S. (2020). COVID-19 pandemic, government responses, and public mental health: Investigating consequences through crisis hotline calls in two countries. Social Science & Medicine, 1982(265), 113532–113532. https://doi.org/10.1016/j.socscimed.2020.113532
Bahora, M., Hanafi, S., Chien, V. H., & Compton, M. T. (2008). Preliminary evidence of effects of crisis intervention team training on self-efficacy and social distance. Administration and Policy in Mental Health and Mental Health Services Research, 35, 159–167.
Battersby, L., & Morrow, M. (2012). Challenges in implementing recovery-based mental health care practices in psychiatric tertiary care. Canadian Journal of Community Mental Health, 33, 103–117.
Bird, S., & Shemilt, I. (2019). The crime, mental health, and economic impacts of prearrest diversion of people with mental health problems: A systematic review. Criminal Behaviour and Mental Health, 29(3), 142–156. https://doi.org/10.1002/cbm.2112
Bittner, E. (1967). The police on skid-row: A Study of peace keeping. American Sociological Review, 32(5), 699–715. https://doi.org/10.2307/2092019
Blais, E., Landry, M., Elazhary, N., Carrier, S., & Savard, A. M. (2020). Assessing the capability of a co-responding police-mental health program to connect emotionally disturbed people with community resources and decrease police use-of-force. Journal of Experimental Criminology, 18(1), 41–65. https://doi.org/10.1007/s11292-020-09434-x
Borschmann, R., Gillard, S., & Turner, K. (2010). Demographic and referral patterns of people detained under section 136 of the Mental Health Act 1983. Medicine, Science and the Law, 50, 15–18.
Boscarato, K., Lee, S., Kroschel, J., Hollander, Y., Brennan, A., & Warran, N. (2014). Consumer experience of formal crisis response services and preferred methods of crisis. International Journal of Mental Health Nursing, 23, 287–295.
Boyd, J., & Kerr, T. (2016). Policing “Vancouver’s mental health crisis”: A critical discourse analysis. Critical Public Health, 26(4), 418–433. https://doi.org/10.1080/09581596.2015.1007923
Bucerius, S. M., Oriola, T. B., & Jones, D. J. (2021). Policing with a public health lens–Moving towards an understanding of crime as a public health issue. The Police Journal: Theory, Practice and Principles. https://doi.org/10.1177/0032258X211009577
California Office of Patients’ Rights. (2018, January 8). Understanding the Lanterman-Petris-Short Act. Disability Rights California. Retrieved May 4, 2022, from https://www.disabilityrightsca.org/publications/Understanding-the-lanterman-petris-short-lps-act
Carson, J. V., & Wellman, A. P. (2018). Problem-oriented policing in suburban low-income housing: A quasi-experiment. Police Quarterly, 21(2), 139–170. https://doi.org/10.1177/1098611117744005
Charette, Y., Crocker, A. G., & Billette, I. (2014). Police encounters involving citizens with mental illness: Use of resources and outcomes. Psychiatric Services, 65(4), 511–516.
Chester, P., Ehrlich, C., Warburton, L., Baker, D., Kendall, E., & Crompton, D. (2016). What is the work of recovery oriented practice? A systematic literature review. International Journal of Mental Health Nursing, 25(4), 270–285. https://doi.org/10.1111/inm.12241
Comartin, E. B., Swanson, L., & Kubiak, S. (2019). Mental health crisis location and police transportation decisions: The impact of crisis intervention team training on crisis center utilization. Journal of Contemporary Criminal Justice, 35(2), 241–260.
Dalton, J., Thomas, S., Melton, H., Harden, M., & Eastwood, A. (2018). The provision of services in the UK for UK armed forces veterans with PTSD: A rapid evidence synthesis. Health Services and Delivery Research, 6(11), 1–112. https://doi.org/10.3310/hsdr06110
Dyer, W., Steer, M., & Biddle, P. (2015). Mental health street triage. Policing: A Journal of Policy and Practice, 9(4), 377–387. https://doi.org/10.1093/police/pav018
Earley, P. (2007). Crazy: A father’s search through America’s mental health madness. Penguin.
Edmond, T. E., Voth Schrag, R. J., & Bender, A. K. (2020). Opening the black box: Identifying common practice approaches in urban and rural rape crisis centers. Violence against Women, 26(3–4), 312–333. https://doi.org/10.1177/1077801219832903
Enang, I., Murray, J., Dougall, N., Wooff, A., Heyman, I., & Aston, E. (2019). Defining and assessing vulnerability within law enforcement and public health organisations: A scoping review. Health & Justice, 7(1), 2–13. https://doi.org/10.1186/s40352-019-0083-z
Forchuk, C., Jensen, E., Martin, M. L., Csiernik, R., & Atyeo, H. (2010). Psychiatric crisis services in three communities. Canadian Journal of Community Mental Health, 29, 73–86.
Garland, D. (2012). The culture of control: Crime and social order in contemporary society. Chicago: University of Chicago Press.
Hacker, R. L., & Horan, J. J. (2019). Policing people with mental illness: Experimental evaluation of online training to de-escalate mental health crises. Journal of Experimental Criminology, 15(4), 551–567. https://doi.org/10.1007/s11292-019-09380-3
Hadley, E. (2022, May 23). New phone number aims to help Idahoans struggling with mental health crises. KMVT. Retrieved June 7, 2022, from https://www.kmvt.com/2022/05/23/new-phone-number-aims-help-idahoans-struggling-with-mental-health-crises/
Heslin, M., Callaghan, L., Packwood, M., Badu, V., & Byford, S. (2016). Decision analytic model exploring the cost and cost-offset implications of street triage. British Medical Journal Open, 6(2), e009670.
Idaho crisis & suicide hotline. (2022). Idaho Crisis & Suicide Hotline. Retrieved June 7, 2022, from https://idahocrisis.org/Idaho domestic violence help, programs and statistics. (2022). Domesticshelters.org: A service of Theresa's Fund. Retrieved June 8, 2022, from https://www.domesticshelters.org/help/id
Ingram, S., Ringle, J. L., Hallstrom, K., Schill, D. E., Gohr, V. M., & Thompson, R. W. (2007). Coping with crisis across the lifespan: The role of a telephone hotline. Journal of Child and Family Studies, 17(5), 663–674. https://doi.org/10.1007/s10826-007-9180-z
Jacobson, N., & Greenley, D. (2001). What is recovery? A conceptual model and explication. Psychiatric Services, 52, 482–485.
Jeppeson, D., Hettinger, L., Unsworth, M., & Palagi, J. (2021, December). DHW 2021 annual report. Idaho Department of Health & Welfare. Retrieved June 7, 2022, from Safety, support & education. (2022). WCA. Retrieved June 8, 2022, from https://www.wcaboise.org/
Kane, E., & E., & Shokraneh, F. (2018). Effectiveness of current policing-related mental health interventions: A systematic review. Criminal Behaviour and Mental Health, 28(2), 108–119. https://doi.org/10.1002/cbm.2058
Krameddine, Y. I., & Silverstone, P. H. (2015). How to improve interactions between police and the mentally ill. Frontiers in Psychiatry, 5, 186.
Lamanna, D., Shapiro, G. K., Kirst, M., Matheson, F. I., Nakhost, A., & Stergiopoulos, V. (2018). Co-responding police–mental health programmes: Service user experiences and outcomes in a large urban centre. International Journal of Mental Health Nursing, 27(2), 891–900. https://doi.org/10.1111/inm.12384
Lanterman-Petris-Short Act, WIC §5000-5556 (1967). https://www.placer.ca.gov/DocumentCenter/View/34528/Mental-Health-Laws-and-Patients-Rights-in-California-2018-Update-PDF
Lester, H., & Gask, L. (2006). Delivering medical care for patients with serious mental illness or promoting a collaborative model of recovery? British Journal of Psychiatry, 188(5), 401–402. https://doi.org/10.1192/bjp.bp.105.015933
Linden, A. (2015). Conducting interrupted time-series analysis for single-and multiple-group comparisons. The Stata Journal, 15(2), 480–500.
Lipsky, M. (2010). Street-level bureaucracy: Dilemmas of the individual in public service. New York: Russell Sage Foundation.
Makin, D., & Bowers, O. (2020). Netflix as a piracy disruptor? A cross-sectional test of accessibility and affordability on interest in piracy. International Journal of Cyber Criminology, 14(2), 417–432.
Makin, D. A., Bernat, F. P., & Lyons, J. A. (2018). Who decides civil commitments? A statewide analysis of initial hold requests. Victims & Offenders, 13(8), 1171–1192.
Makin, D. A., Meize, M. R., Willits, D. W., Stohr, M. K., Hemmens, C., Lovrich, N. P., & Stanton, D. (2021). The impact of recreational marijuana sales on calls for service: an analysis of neighbouring cities. Policing and Society, 31(7), 848–862.
Mental health public dashboards. (2022, May 19). Idaho Department of Health & Welfare. Retrieved June 7, 2022, from https://publicdocuments.dhw.idaho.gov/WebLink/Browse.aspx?id=2881&dbid=0&repo=PUBLIC-DOCUMENTS
Mishara, B. L., Côté, L., & Dargis, L. (2022). Systematic review of research and interventions with frequent callers to suicide prevention helplines and crisis centers. Crisis: THe Journal of Crisis Intervention and Suicide Prevention. https://doi.org/10.1027/0227-5910/a000838
Morabito, M. S. (2007). Horizons of context: Understanding the police decision to arrest people with mental illness. Psychiatric Services, 58(12), 1582–1587.
Nix, J., Pickett, J. T., Baek, H., & Alpert, G. P. (2019). Police research, officer surveys, and response rates. Policing and Society, 29(5), 530–550.
Pepler, E. F., & Barber, C. G. (2021). Mental health and policing: Picking up the pieces in a broken system. Healthcare Management Forum, 34(2), 93–99. https://doi.org/10.1177/0840470420979635
Quarter Four 2020–2021. (2021, December). Southwest District Health. Retrieved June 7, 2022, from https://phd3.idaho.gov/wp-content/uploads/2021/09/WIDCCC-Q4-2020-2021-Report-.pdf
RodgersThomas, M. S., Dalton, J., Harden, M., & Eastwood, A. (2019). Police-related triage interventions for mental health-related incidents: A rapid evidence synthesis. Health Services and Delivery Research, 7(20), 1–164. https://doi.org/10.3310/hsdr07200
Sewell, C. (2020, January 16). Idaho, which has one of the highest suicide rates in the U.S., now has 211 hotlines to help. East Idaho News.Com. Retrieved June 7, 2022, from https://www.eastidahonews.com/2020/01/idaho-which-has-one-of-the-highest-suicide-rates-in-the-u-s-now-has-211-hotline-to-help/
Shapiro, G. K., Cusi, A., & Kirst, M. (2015). Co-responding police-mental health program: A review. Administration and Policy in Mental Health, 42, 606–620. https://doi.org/10.1007/s10488-014-0594-9
Soares, R., & Pinto da Costa, M. (2019). Experiences and perceptions of police officers concerning their interactions with people with serious mental disorders for compulsory treatment. Frontiers in Psychiatry, 10, 187–187. https://doi.org/10.3389/fpsyt.2019.00187
State of mind 2021. (2021, December). Idaho Department of Health & Welfare. Retrieved June 7, 2022, from https://publicdocuments.dhw.idaho.gov/WebLink/DocView.aspx?id=21502&dbid=0&repo=PUBLIC-DOCUMENTS
Steadman, H. J., Stainbrook, K. A., Griffin, P., Draine, J., Dupont, R., & Horey, C. (2001). A specialized crisis response site as a core element of police-based diversion programs. Psychiatric Services, 52, 219–222. https://doi.org/10.1176/appi.ps.52.2.219
Stone, A. (1975). Mental health and the law: A system in transition. Rockville, Maryland: National Institute of Mental Health, Center for Studies of Crime and Delinquency.
Taheri, S. A. (2016). Do crisis intervention teams reduce arrests and improve officer safety? A systematic review and meta- analysis. Criminal Justice Policy Review, 27(1), 76–96. https://doi.org/10.1177/0887403414556289
Teller, J. L. S., Munetz, M. R., Gil, K. G., & Ritter, C. (2006). Crisis intervention team training for police officers responding to mental disturbance calls. Psychiatric Services, 57, 232–237. https://doi.org/10.1176/appi.ps.57.2.232
Teplin, L., & Pruett, N. (1992). Police as streetcorner psychiatrist: Managing the mentally ill. International Journal of Law and Psychiatry, 15, 139–156.
Thomas, K. C., Ellis, A. R., Konrad, T. R., Holzer, C. E., & Morrissey, J. P. (2009). County-level estimates of mental health professional shortage in the United States. Psychiatric Services (washington, D.c.), 60(10), 1323–1328. https://doi.org/10.1176/ps.2009.60.10.1323
Ullman, S. E. (2022). Rape resistance: A critical piece of all women’s empowerment and holistic rape prevention. Journal of Aggression, Maltreatment & Trauma, 31(4), 519–539. https://doi.org/10.1080/10926771.2020.1821851
van Dijk, A., & Crofts, N. (2017). Law enforcement and public health as an emerging field. Policing & Society, 27(3), 261–275. https://doi.org/10.1080/10439463.2016.1219735
van Dijk, A., Herrington, V., Crofts, N., Breunig, R., Burris, S., Sullivan, H., Middleton, J., Sherman, S., & Thomson, N. (2019). Law enforcement and public health: Recognition and enhancement of joined-up solutions. The Lancet (british Edition), 393(10168), 287–294. https://doi.org/10.1016/S0140-6736(18)32839-3
Warren, C. (1977). Involuntary commitment for mental disorder: The application of California’s Lanterman-Petris-Short Act. Law & Society Review, 11(4), 629–649. https://doi.org/10.2307/3053175
Watson, A. C., Compton, M. T., & Draine, J. N. (2017). The crisis intervention team (CIT) model: An evidence-based policing practice? Behavioral Sciences & the Law, 35(5–6), 431–441. https://doi.org/10.1002/bsl.2304
Watson, A. C., Ottati, V. C., Morabito, M. S., Draine, J., Kerr, A. N., & Angell, B. (2010). Outcomes of police contacts with persons with mental illness: The impact of CIT. Administration and Policy in Mental Health and Mental Health Services Research, 37, 302–317.
Wells, R., Morrisey, J. P., Lee, I. H., & Radford, A. (2010). Trends in behavioral health care service provision by community health centers, 1998–2007. Psychiatric Services, 61(8), 759–764. https://doi.org/10.1176/appi.ps.61.8.759
White, C. J. (2021). An inevitable response? A lived experienced perspective on emergency responses to mental health crises. Journal of Psychiatric and Mental Health Nursing, 28(1), 90–93. https://doi.org/10.1111/jpm.12631
Wise, M., Christiansen, L., & Stewart, C. (2019). Examining the effectiveness of mental health education on law enforcement: Knowledge and attitudes. Journal of Police and Criminal Psychology, 36(1), 49–55. https://doi.org/10.1007/s11896-019-09319-4
Wood, J. D. (2020). Private policing and public health: A neglected relationship. Journal of Contemporary Criminal Justice, 36(1), 19–38. https://doi.org/10.1177/1043986219890191
Wood, J. D., & Beierschmitt, L. (2014). Beyond police crisis intervention: Moving “upstream” to manage cases and places of behavioral health vulnerability. International Journal of Lawand Psychiatry, 37(5), 439–447.
Wood, J. D., & Watson, A. C. (2017). Improving police interventions during mental health-related encounters: Past, present and future. Policing and Society, 27(3), 289–299.
Yoon, J., & Bruckner, T. A. (2009). Does deinstitutionalization increase suicide? Health Services Research, 44(4), 1385–1405. https://doi.org/10.1111/j.1475-6773.2009.00986.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no known conflicts of interest, and all authors certify responsibility for the material contained in the study.
Ethical Approval
The Washington State University (WSU) institutional review board approved the protocol used in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Makin, D.A., Carter, P. & Parks, M. Examining Implementation of Crisis Centers on Police Officer Emergency Hold Petitions. Community Ment Health J 59, 1150–1162 (2023). https://doi.org/10.1007/s10597-023-01097-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10597-023-01097-y