Abstract
The multiple benefits of family-based treatment (FBT) used in substance use disorder (SUD) treatment include increased treatment engagement, better treatment outcomes, and cost-effectiveness compared to other behavioral health treatment modalities. However, the prevalence and types of FBTs offered among SUD treatment facilities are largely unknown. The present study used data collected during 2009–2010 from 325 treatment centers in the United States to (1) explore the prevalence in the utilization of FBT in SUD treatment, and (2) identify differences between treatment facilities that do and do not offer FBT. Results indicated that the adoption of FBT was negatively associated with the percentage of clients who were unemployed or involved in the criminal justice system at time of intake, and positively related to the number of hours of individual therapy and treatment center emphasis on utilizing the 12 Steps. Additionally, the majority of treatment centers that followed the American Society of Addiction Medicine (ASAM) clinical guidelines offered FBT. Lastly, the percentage of families involvement was negatively associated with centers’ proportion of revenues from Medicaid (i.e., health insurance for those with limited income) and positively associated with treatment center revenues from private insurance. The impact of having FBT in SUD treatment centers is discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2021, over 61 million individuals in the United States aged 12 years and older reported illicit drug use in the past year (Center for Behavioral Health Statistics and Quality, 2023). In the same year, over 100,000 people in the United States died of a drug overdose (Center for Disease Control, 2023). With such high rates of substance use, it is no surprise that substance misuse impacts approximately half of all families living in the United States (Saad, 2019). The detrimental impact of substance use disorders (SUDs) on the family system is well-documented and linked to higher rates of mental and physical health problems (Lander et al., 2013), divorce (Cranford, 2014), abuse and neglect (Brook & McDonald, 2009), and increased risk of partner substance misuse (Cafferky et al., 2018; Hogue et al., 2022; Lander et al., 2013). Complicating matters further, the intergenerational cycle of addiction continues to perpetuate substance misuse and associated problems across multiple generations (Knight et al., 2014). Though the impact of substance use on the family is deleterious, the role of the family as a critical component of treatment and recovery continues to emerge (Ventura & Bagley, 2017).
Research examining family-based treatment (FBT) has demonstrated efficacy for both adolescents (Horigian et al., 2016) and adults (Fals-Stewart et al., 2000; Ruff et al., 2010) substance use. FBT encompasses a wide range of services available to individuals enrolled in SUD treatment as well as their family and loved ones (i.e., family of origin or chosen family) and consists of treatment that focuses on relational dynamics among individuals and their social network. The myriad of ways for family involvement in the treatment process include family counseling, couple counseling, or family support groups. The multitude of identified potential benefits of FBT in SUD treatment include increased treatment engagement, better treatment outcomes (Reiter, 2019; Ventura & Bagley, 2017), and cost effectiveness compared to other behavioral health treatment modalities (Morgan et al., 2013; Morgan & Crane, 2010). Family therapy models have been established as efficacious stand-alone and multicomponent treatment modalities for SUDs (Hogue et al., 2022). While the term ‘family’ represents various constellations including partners, siblings, aunts, uncles, grandparents, children, and other non-biological members, previous evidence-based FBT practices and outcomes largely focused on adolescents (Tambling et al., 2021), at the exclusion of adult relationships. Despite efforts to increase access to FBT in SUD treatment, family therapy remains widely underutilized in treatment.
While a multitude of potential benefits of FBT for families impacted by SUDs has been identified(National Institute on Drug Abuse (NIDA), 2018; Reiter, 2019; Werner et al., 2007), little is known about the consistency of family therapy integration within SUD treatment facilities (Substance Abuse and Mental Health Services Administration (SAMHSA), 2020; Stanton & Shadish, 1997), and the prevalence and types of FBT being offered among SUD treatment facilities are largely unknown. Knowledge of current integration strategies of FBTs into treatment programs for individuals with SUDs is needed in order to determine the ‘lay of the land’, and the characteristics of SUD treatment programs that are offering FBT, allowing for more detailed analysis about how to best infuse FBT into SUD treatment programming and ultimately, to examine treatment outcomes related to the use of FBT. As a step toward this important set of goals, the purpose of the current study was to examine the prevalence of FBT in treatment centers, and to examine client, programmatic, and organizational differences among treatment centers that do and do not utilize FBT.
National Guidelines Include FBT for SUD Treatment
Several national organizations have identified best practices and guidelines for SUD treatment. For example, NIDA identified a comprehensive care model for effective treatment (NIDA, 2018) that focuses on services beyond direct SUD treatment to include medical, legal, educational, and vocational services. Notably, the role of family and family-based services are also identified as important quality indicators of SUD treatment.
In addition to NIDA, the American Society of Addiction Medicine (ASAM) criteria are a widely-used set of standards applied to the placement, treatment, and continued care for SUDs across four broad levels of care. ASAM offers guidelines for each level of care that focus on the care setting, services typically offered, and utilization of the ASAM needs assessments to optimize treatment for each client (Kampman & Jarvis, 2015). Additionally, the recently released 2020 ASAM National Practice Guidelines for the Treatment of Opioid Use takes into consideration the role of family members in treatment and recovery support (Kampman & Jarvis, 2015; Wong et al., 2020). However, while adhering to ASAM guidelines is highly recommended, it is not a requirement of treatment centers.
In recent years, family therapy and treatment approaches that integrate families into the care of the individual have become the gold standard of treatment, and have received increased funding for their implementation and research to assess their efficacy (SAMHSA, 2020). Despite both the NIDA and ASAM models highlighting the importance of including FBTs in SUD treatment, there continues to be a dearth of research in clearly understanding the prevalence and utilization of evidence-based FBT in SUD treatment. The current study aims to address this gap in the literature.
Predictors of Evidence-Based Treatment in SUD Treatment
Past research documented the predictive utility of client characteristics, program services, and organizational characteristics on the adoption and implementation of other evidence-based treatment for SUD treatment (Aletraris et al., 2015a, Aletraris et al., 2017a; Aletraris et al., 2014; Aletraris et al., 2017b; Aletraris & Roman, 2015; Edmond et al., 2015; Paino et al., 2015, 2016). Specifically, the use of evidence-based practices (EBPs) was significantly affected by caseload characteristics, such as a center’s caseload of privately- and Medicaid-insured patients, and other organizational characteristics, such as profit status (e.g. non-profit, for-profit) and levels of care (e.g. inpatient, outpatient) (Aletraris et al., 2015a). Findings also indicated the importance of leadership and staff expertise in sustaining implementation of EBPs over time (Aletraris et al., 2016; Aletraris et al., 2015b).
Inter-organizational relationships through pressure from accreditation bodies and other healthcare organizations are also important predictors of EBP adoption (Edmond et al., 2015; Knudsen & Roman, 2015, 2016), as are other organizational characteristics, including state Medicaid reimbursement and other health policies (Ducharme & Abraham, 2008). For example, a significant negative association was found between referrals from the criminal justice system and treatment center adoption of various EBPs (Edmond et al., 2015). Policies within in the criminal justice system may not always align with the goals of adopting specific EBPs, particularly the use of medications. Similarly, funding mechanisms for criminal-justice affiliated clients could result in limited reimbursement for specific services, which could affect the number and types of services covered and offered by treatment centers serving them. Nevertheless, none of these studies specifically examined the implementation of evidence-based FBTs in SUD treatment, which focus on a relational-systemic orientation compared to an individual orientation traditionally used in treatment centers.
There are numerous empirically-validated FBT modalities used to treat individuals with SUD and their families, such as solution-focused therapy (Berg & Miller, 1992); brief strategic family therapy (BSFT), multisystemic therapy (MST) (Cunningham & Henggeler, 1999); and structural and strategic family therapy (SAMHSA, 2020; Stanton, 1981; Stanton & Todd, 1982; Szapocznik, 2003; Szapocznik & Williams, 2000), all of which highlight the importance of treating the family system rather than just the individual.
BSFT is an FBT that has long been applied to adolescent substance use (Szapocznik et al., 1988; Szapocznik et al., 2003). It focuses on changing interactional patterns among families that may promote or maintain substance use among adolescents (Szapocznik et al., 2013). MST was developed specifically for adolescents involved with the criminal justice system and are using substances, and emphasizes behavior change through therapeutic intervention with the family and community (Henggeler et al., 2009). MST has demonstrated efficacy in reducing adolescent substance use (Henggeler et al., 1999). However, to date, limited examination exists on the use of FBT as a modality explicitly used within SUD treatment centers. As a result, there are no known standard guidelines for the utilization of FBT among SUD treatment centers, despite prior research evidencing multiple evidenced-based FBT models as listed above.
Resource Dependence and Innovation Compatibility
Resource dependence and innovation compatibility are concepts that are applied to examine factors influencing organizational decision-making regarding implementing organizational practices that involve the family (Pfeffer & Salancik, 2003; Rogers, 2003). The proposed study provides an opportunity to examine the relative explanatory power of each of these influences on the use of FBT in SUD treatment. Resource dependence is defined as the extent to which there are external environmental expectations and pressures on the organization that provide incentives for adoption and supports the examination of external factors as predictors of FBT implementation. Innovation compatibility is the extent to which the innovation is compatible with the existing practices, philosophy, and culture of the organization, and thereby provides rationale for the examination of internal factors in the present study.
The proposed study considers a variety of inter-organizational relationships relevant to resource dependence, such as type of referral sources, state accreditation bodies, and payer mix that may influence adoption and implementation. In addition to resource dependence, Rogers’ diffusion of innovations theory (Pfeffer, 1997) argues that adoption of a practice partly depends on compatibility between its characteristics and features of the organization (Knudsen & Roman, 2004). Specifically, a treatment practice is more likely to be adopted (a) if it is compatible with an organization’s prior and ongoing practices, (b) if it fits the particular treatment needs of its client base, and (c) if these practices affirm organizational norms. Thus, various inter-organizational elements should be examined regarding influencing organizational decision-making for the implementation of FBTs among SUD treatment.
Current Study
In order to contextualize the current study, it is important to consider substance use and treatment patterns during the timeframe of the study’s data collection. In 2010 in the United States, there were over 22 million individuals who reported illicit substance use. The rate of substance use continued to slightly increase from 2008 from 8 to 8.7% in 2009, and finally to 8.9% of the population in 2010 (Substance Abuse and Mental Health Services Administration, 2011). In the same year, there were only approximately 1.8 million individuals admitted to substance use treatment in the United States and Puerto Rico; with the top five substances used being alcohol (41%), opioids (23%), marijuana (18%), cocaine (8%), and methamphetamine/amphetamines (6%). Additionally, a majority (68%) of the individuals entering treatment in 2010 were males (Blacklow et al., 2012). During this time frame, family therapy models were being recognized for their effectiveness and efficacy among substance use populations, including BSFT (Briones et al., 2008; Robbins et al., 2008), MST (Henggeler et al., 2009), Behavioral Couples Therapy (BCT) (Ruff et al., 2010; Lam et al., 2009), Multidimensional Family Therapy (MDFT) (Morgan & Crane, 2010; Henderson et al., 2010) and Community Reinforcement and Family Training (CRAFT) (Dutcher et al., 2009).
While client characteristics, program services, and organizational characteristics have been linked to the implementation of EBPs among SUD treatment (Aletraris et al., 2015a; Aletraris et al., 2016; Aletraris, Shelton et al., 2015b), little is known about the prevalence and utilization specifically of FBTs among SUD treatment centers across the United States.
Because family-based services are an understudied asset to treatment, the goal of the present study was to identify patterns of the utilization of FBTs services in SUD treatment facilities. As such, the present study used survey data from treatment centers to:
-
1.
Explore the prevalence in the utilization of FBTs in SUD treatment, including adoption of two specific evidence-based FBTs (BSFT and MST);
-
2.
Identify relationships between client characteristics, program services offered, and organizational characteristics among treatment facilities that do and do not offer FBT.
Method
Data Source
The current study used data from the National Treatment Center Study (NTCS) (Edmond et al., 2015). The purpose of the NTCS was to examine evidence-based patient care and management practices in representative national samples of privately-funded non-profit and for-profit treatment centers. The study was conducted in eight waves of onsite data collection from a combination panel/longitudinal study design of treatment organizations. The current study used 2009–2010 data, which were the most recent available data that included questions on FBT.
Participants & Procedures
Data were collected via in-depth in-person interviews with the administrators and clinical directors at their treatment programs, and the current analysis is limited to those who completed the question on family therapy utilization (n = 325). Treatment programs were selected via a two-stage random sampling design (Knudsen et al., 2007) and were required to offer alcohol and drug treatment at a level of intensity equivalent to at least ASAM Level 1 outpatient services (see Aletraris and Roman (2015) for more methodological details).
Measures
A codebook for the present analyses was developed to identify the following variables: client characteristics, program services offered, organizational characteristics, and FBT (see Table 1).
Family-Based Treatment
FBT was measured by variables assessing therapeutic modalities that are focused on the family or family sub-systems (e.g. couples). Two questions were used as the primary variables of interest: (1) if programming was available to families of clients enrolled in treatment on a dichotomous scale of yes/no, and (2) the approximate percentage of patients’ families involved in FBT. A question on family counseling explored whether (1) it was available through a formal agreement or contract with another organization, (2) the center referred patients elsewhere for the service, or (3) whether the service was not available. Additional questions further examined FBT, including the extent to which the treatment center emphasized family therapy (0 = no extent, 5 = a very great extent), and whether the center adopted two specific evidence-based FBTs; BSFT (1 = yes, 2 = no), and MST (1 = yes, 0 = no).
Client Characteristics
Information about clients enrolled at the treatment centers was included to contextualize the data for the current study. Demographic information included: total number of treatment admissions over the past fiscal year, gender, race/ethnicity, employment status, ages of the center’s caseload, percentage of patients involved in the criminal justice system, and percent center caseload using different substances.
Program Services Offered
Clinical services examined the use of cognitive behavioral therapy (CBT), motivational incentives/contingency management (MI/CM), and motivational interviewing (MI) (1 = yes, 0 = no). Clinical services also included 12-step meetings being held at the treatment center, and housing, childcare, and transportation services offered (1 = yes, 0 = no).
Organizational Characteristics
Organizational characteristics were measured as binary (yes/no) variables for the following: use of ASAM clinical criteria to guide treatment, a center’s profit status, e, and accreditation status,, as well as the percentage of revenues from Medicaid and from private insurance.
Analytic Plan
Data were downloaded and analyzed using SPSS v27 (IBM Corp, 2020). Data cleaning and screening analyses were conducted. Log transformation and listwise deletion were used to address skewed and missing data. The following data analysis plan was developed per aim: 1). Frequencies were used to examine the prevalence and trends of FBT in treatment centers that offered FBT versus those that did not offer FBT, 2). Independent samples t-tests and chi-squared analyses were used to examine group differences between family-based service utilization and outcomes of clinical characteristics, program services, and organizational characteristics.
Results
Descriptive Statistics
The average number of annual treatment admissions for the 325 centers was M = 864.90 (SD = 1,879.79). African American clients represented a mean percentage of M = 16.06 (SD = 20.26) of a center’s caseload, while the mean percentage of clients that identified as Hispanic/Latino was M = 10.48 (SD = 15.11). The mean percentage of clients was M = 67.64 (SD = 47.94) for the 19 to 49 age range, and was M = 9.32 (SD = 18.30) for clients under 19 years old. Clinical directors reported that the substances being used among their center’s caseload were alcohol (M = 65.43, SD = 23.77), marijuana (M = 43.42, SD = 27.23), and opioids (M = 29.08, SD = 22.91).
Aim # 1 Prevalence and Utilization of FBT
Frequencies and percentages were examined to establish the prevalence in the utilization of FBT. Table 2 highlights the frequencies of FBT across studies. Most treatment centers (74.5%; n = 242) reported offering FBT. On average, 38.29% of clients’ families were involved in the family treatment program (n = 242; SD = 30.12). In total, 70.8% (n = 230) of treatment centers reported emphasizing family counseling at a three or higher on a scale of zero to five (M = 3.19 L SD = 1.63). In terms of family counseling, the majority (67.4%, n = 219) of treatment centers provided family counseling onsite while some (23.5%, n = 76) reported informal referrals for family counseling. Lastly, in terms of adoption of evidence-based FBTs among all treatment centers, 10.2% (n = 33) of treatment centers reported offering BSFT, and 13.5% (n = 244) reported offering MST. Of the centers that reported offering FBT (75%), only a small percentage reported offering BSFT (11%) and MST (14%).
Aim # 2 Client, Program, and Organizational Characteristics in Relation to FBT
To examine the second aim, FBT utilization was examined in relation to client characteristics, program services offered, and organizational characteristics. Table 3 provides a detailed description of program and client characteristics by FBT vs. non-FBT.
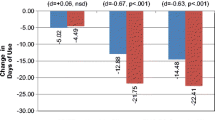
Client Characteristics
Client characteristics included examining both client demographics and special populations. An independent samples t-test indicated a significant negative relationship between the provision of FBT and a center’s percentage of patients who were unemployed at time of intake (t127.18 = 2.08, p = .04). Treatment centers providing FBT had a lower mean percentage of unemployed patients (M = 33.23) compared to centers that did not offer FBT (M = 41.44). Likewise, there was a significant relationship between use of FBT and the percentage of a center’s caseload that was involved in the criminal justice system (t128.86 = 3.47, p = .001). Treatment centers providing FBT had a lower mean percentage of patients involved with the criminal justice system (M = 41.42) compared to centers not providing FBT (M = 55.85). Pearson correlation analyses (not shown) indicated that the percentage of families who participated in FBT was also significantly negatively related to the percentage of a center’s caseload of individuals who were unemployed (r = − .27, p = .002) and the percentage who were involved in the criminal justice system (r = − .25, p = .00). Lastly, there was a significant positive relationship between offering FBT and a center’s caseload that used prescription opiates (r = .13, p = .04). No significant findings were found for other substances in a center’s caseload.
Program Services
Program Services refers to other clinical services offered at the sites including individual therapy practices, 12-step meetings, and case management services. An independent samples t-test indicated a significant relationship between the average hours per week patients spend in individual therapy and FBT (t323 = -3.37, p = .001); specifically, centers providing FBT had a slightly higher mean of weekly hours in individual therapy (M = 1.66) compared to those not providing FBT (M = 0.93). A Pearson correlation (not shown) indicated a significant positive relationship between individual counseling hours and the percentage of families that participate in treatment (r = .16, p = .01). The majority of treatment centers (60.6%; n = 197) reported offering 12-step meetings at the center. Treatment centers that offered 12-step meetings at the center were more likely to offer FBT (χ (1) = 9.71, p = .00). Interestingly, most participants reported their treatment center was based on the 12-step model, with 80% (n = 260) of respondents reporting between three and five on a scale from zero (no extent) to five (great extent). The relationship between the extent of the use of 12-steps and family therapy was also significant (χ (5) = 16.21, p = .01). There was no significant relationship between offering EBPs such as CBT or MI in relation to offering FBT. However, there was a significant negative relationship between using MI/CM and offering FBT χ (2) = 8.76, p = .01.
Organizational Characteristics
Organizational characteristics examined accreditation, profit status, and Medicaid and private insurance status. In total, 86.2% (n = 280) of participants reported using ASAM criteria to individualize client care among treatment centers. 60% of treatment centers were accredited by either the Joint Commission, Commission on Accreditation of Rehabilitation Facilities (CARF), or Council on Accreditation (COA). The majority of the centers, 65% (n = 212) reported operating as a non-profit, while 34% (n = 111) operated as for-profit centers. For annual revenues, on average, 15% of center revenues came from Medicaid, while 30% came from private/commercial insurance.
Chi-square analysis indicated there was a significant relationship between using ASAM criteria for treatment and offering FBT (χ (6) = 8.60, p = .00) in that centers using ASAM criteria were more likely to offer FBT compared to those not offering FBT. In total, of the centers that followed ASAM criteria, 89.3% (n = 216) offered FBT. Finally, correlation analyses indicated significant relationships between annual revenue source, specifically from Medicaid (r = − .20, p = .002) and private/commercial insurance (r = .27, p < .001), and centers offering FBT as well as revenue source and the percentage of families involved in treatment. Lower revenues from Medicaid were negatively related to the provision of FBT (and percentage of families involved in treatment), while higher revenues from private insurance were positively associated with provision of FBT and percentage of families involved in treatment.
Discussion
The present study sought to examine the prevalence of FBT in community-based substance use treatment facilities and to explore group differences in client characteristics, program services, and organizational characteristics based on FBT utilization at these treatment centers. In doing so, the current findings addressed a critical gap in the literature by explicitly examining the intersection of SUD treatment and FBT services. Several findings emerged from the analysis that can be used to inform future clinical, scholarly, and policy initiatives for further integrating SUD treatment and relational-systemic therapy.
During the timeframe the data were collected, there was clear evidence for the necessity to include family in treatment, though there was also recognition of the challenges to engage family members (Santisteban et al., 2005). In terms of the two FBTs examined in the current study (BSFT and MST), research indicated that BSFT demonstrated positive outcomes related to family alliance (Robbins et al., 2008). Interestingly, the model was adapted to reflect challenges faced when engaging and retaining family members of adolescents in treatment (Briones et al. 2008). MST had been examined among juvenile offenders and demonstrated reduction in substance use among adolescents (Brown et al., 1999; Henggeler et al., 2002). Notably, BSFT was developed to be delivered in treatment and community settings (Robbins et al., 2000) ), while MST was developed to be implemented primarily in the community (e.g. home, school) (Henggeler et al., 1999).
Summary of Key Results and Implications of the Findings
Key findings highlighted the relationship between client characteristics, program services, and organizational characteristics in relation to offering and utilizing FBT. Interestingly, while most treatment centers reported offering FBT (75%), only a small percentage reported offering specific evidence-based FBTs; just 11% used BSFT and 14% used MST. Treatment centers reported that approximately 38% of families participated in treatment in some form. Thus, it is evident that FBT was being offered and family members were participating to some extent; what remains unknown is what type of FBT is being offered, whether it is evidence-based, in what capacity, and by whom. Because family therapy has demonstrated efficacy for SUD treatment (Hogue et al., 2022; Ventura & Bagley, 2017), understanding the implementation elements of FBT may provide foundational knowledge that can support standardizing FBT practice among SUD treatment centers. Additionally, evidence-based practices among SUD treatment are considered the ‘gold standard of care,’(Hogue et al., 2022; McGovern & Carroll, 2003; NIDA, 2018; SAMHSA, 2020), thus it is important to have knowledge of what evidence-based FBTs are being implemented in treatment and examine how those relate to recovery outcomes.
Client Characteristics
The present study indicated that the implementation of FBT as well as the percentage of families involved in treatment were related to centers’ lower percentages of clients who were unemployed or involved in the criminal justice system. This finding highlights the potential for organizational components to promote or limit the access to FBT at the individual level. For example, consideration could be given to structural influences among treatment centers that may limit the ability to involve families. Historically, getting family members of those with SUDs involved in treatment has been difficult (McCollum & Trepper, 2014; Saatcioglu et al., 2006), and perhaps treatment centers with a higher proportion of justice-involved or unemployed clients have particular challenges in getting clients’ families involved in treatment. Treatment centers may also lack the capacity and resources to connect with the criminal justice system in a way that supports the recruitment and retention of family members.
At the individual level, those are who employed often have the economic stability (McCaul et al., 2001) (e.g., transportation, resources) that facilitates remaining in treatment. Likewise, because substance use often negatively impacts obtaining and maintaining employment (Henkel, 2011), it is possible that clients demonstrating the ability to keep a job may increase motivation for family members to participate in treatment.
Additionally, the type of substance was related to FBT in that there was a significant relationship between the percentage of a center’s caseload using prescription opiates and use of FBT, as well as the percentage of families who were involved in treatment. While more research is needed to better understand the relationship between SUD treatment and the utilization of FBT, it is possible that centers treating opioid use disorder (OUD) may also be the same sites that use the ASAM guidelines, which highlight the importance of family involvement in treatment for OUD (Kampman & Jarvis, 2015; Wong et al., 2020). Further, additional recent scholarship has highlighted the importance of the role of family in treatment for opioids (Kaur et al., 2019).
Program Services
The results of the present study also highlight the relationship between treatment centers that implement NIDA’s comprehensive care model (NIDA, 2018) with FBT. Specifically, quality indicators of care including the number of hours in individual therapy and community-based 12-step meetings were linked to the implementation of FBT. A few things should be considered when interpreting this finding. First, SUD treatment still largely focuses on individual recovery (Daley, 2013) and other indicators of care (e.g., family functioning, family involvement) are not as prioritized. For the present study, it is possible that clients seeking SUD treatment are required to participate in individual therapy and then referred to FBT. Because NIDA’s comprehensive care model emphasizes the need for multiple quality indicators of care (NIDA, 2018), efforts should be made to expand treatment services beyond individual therapy to include FBT as a more permanent fixture of treatment.
Second, treatment centers that align with the comprehensive care model and prioritize the integration of multiple services may be more likely to offer FBT. As such, clients may be more likely to seek out treatment centers that offer a myriad of services, such as 12-step meetings and FBT. Research indicates that integrated care models yield the best recovery outcomes (Burnam & Watkins, 2006; Ducharme et al., 2006; Henderson et al., 2017). Interestingly, recent literature underscores the systemic and complementary nature of 12-step programs and FBT (Smith et al., 2019). Future research should continue to examine individual preference for SUD treatment services as well as the relationships between quality indicators of care and FBT. Noteworthy is that offering MI/CM was negatively related to rates of FBT among treatment centers. Because MI/CM have long demonstrated efficacy for SUD treatment (ATTCN, 2018), it is possible that it is offered as a stand-alone treatment modality. Interestingly, use of FBT was not associated with other evidence-based behavioral treatment practices, including CBT or MI. More research is needed to better understand program services that predict the implementation of FBT and how FBTs are used in conjunction with other EBPs.
Organizational Characteristics
Lastly, organizational characteristics that were related to the implementation of FBT included following ASAM criteria and annual revenue source. In addition to the centers’ provision of FBT, the percentage of family involved also decreased as centers’ proportion of Medicaid revenues increased, while family involvement increased as centers’ proportion of private insurance revenues increased. Because Medicaid is intended for individuals and families with low socioeconomic status (SES) (HealthCare.gov, 2022), this finding may represent a lack of resources for those with low SES status seeking treatment. Expectations to attend treatment and have family attend treatment may be more unrealistic for those who use Medicaid and must prioritize getting other needs met. Thus, treatment centers must remain cognizant of ways to increase infrastructure conducive to all individuals and families, including those utilizing Medicaid, in an effort to increase equitable access to treatment and services.
Finally, results indicated that the majority of treatment centers that used ASAM guidelines offered FBT. ASAM clinical guidelines for treating opioid use (Kampman & Jarvis, 2015) and alcohol withdrawal management (Wong et al., 2020) highlight the role of including family members in treatment in various ways, including the utilization of family therapy as part of the psychosocial treatment component of a comprehensive treatment plan. Thus, the connection between utilizing both ASAM guidelines and FBT may be linked to the explicit connections ASAM has made in including family involvement when treating SUD. It is important for family therapists working in SUD treatment centers to become familiar with ASAM guidelines in order to stay updated on best practices and utilize a myriad of resources geared at treating those impacted by substance use and co-occurring disorders. Future work is needed to more thoroughly parse out this relationship and to determine how to better integrate relational-systemic therapies in SUD treatment guidelines more explicitly, including both ASAM and NIDA models.
Other elements that must be considered and may impact current findings are the attitude and culture of the treatment center and family system. In alignment with innovation compatibility, FBT may be more likely to be implemented if it is compatible with ongoing practices (e.g., revenue/ASAM guidelines), fits the needs of the clients, and affirms the norms of the treatment center (e.g. attitudes towards FBTs). Indeed, revenue source and ASAM criteria may impact the implementation of FBTs among SUD treatment centers. However, representation of family therapists and attitudes towards FBTs among treatment center leadership and staff may also be influential. Likewise, family members’ willingness to participate in treatment likely plays an integral role in the implementation of FBTs. Engaging family members in SUD treatment continues to be challenging (Tambling et al., 2021) and should be considered in the implementation efforts of treatment centers.
In summary, FBT among SUD treatment is important and the majority of centers reported using some facet of FBT; yet only a small minority utilized specific evidence-based FBTs. Treatment center leaders must continue identifying the need for and impact of family-based interventions among substance use populations. Indeed, there is an opportunity for behavioral health training programs to introduce SUD materials into educational curriculum to keep family therapists engaged in this work (Chou et al., 2023). Likewise, SUD facilities should continue to integrate and prioritize family-based interventions into treatment.
Limitations & Future Research
While the goal of this exploratory study was to contribute to the gaps in literature on FBT utilization among substance use treatment centers was achieved, some limitations must be noted. Due to missing data, we were unable to examine multiple potential predictors of family therapy utilization at once. Relatedly, multiple bivariate tests were conducted, and it is possible that some of the associations observed may be random associations. Future research should consistently operationalize FBT across a large independent sample that would provide the opportunity to examine multiple potential predictors of family therapy utilization concurrently using multivariate analyses. Future research can also build from this study to examine FBT utilization and treatment outcomes specific to the clientele.
The age of the data is a limitation; however, we believe that the information they provide is useful and relevant for two reasons. First, we were unable to find any other treatment data sets that were collected more recently (and available for secondary analyses) that were inclusive of information about FBT. Second, and perhaps more important, we were unable to identify any secular trends since these data were collected that would either significantly increase or decrease the availability of FBT. The use of FBT is not a new concept in SUD treatment, and over the past decade, there have not been major innovations in family therapy with notable impacts on effectiveness that might have accelerated the use of this type of therapy in SUD treatment centers, although it should be noted that other FBTs not examined in this study, such as MST (Henggeler et al., 2009), Behavioral Couples Therapy (BCT) (Ruff et al., 2010), Multidimensional Family Therapy (MDFT) (Morgan & Crane, 2010) may have been adopted within SUD treatment centers during this period. Replicating the study with new data and additional types of FBT would be useful, and the current study serves as a base to compare future surveys on FBT in SUD treatment.
Conclusion
While family-based interventions have been shown to be efficacious in treating SUDs (e.g. Bartle-Haring et al., 2018; Liddle et al., 2018; Vardanian et al., 2020), understanding the prevalence and trends of family-based interventions within the context of community-based substance use treatment facilities has been understudied. The current study addressed this gap by exploring family-based interventions within the context of SUD treatment center data, finding that FBT utilization ranges across sites and that variables, such as centers aligning to ASAM guidelines, centers’ average revenues from private insurance, and centers’ use of other EBPs, such as CM/MI, were significantly associated with centers’ utilization of FBTs. On the other hand, treatment centers were less likely to use FBT with a greater percentage of Medicaid clients, clients who were unemployed, and those referred from the criminal justice system. It is crucial to consider how to expand on this exploratory study and explicitly query the intersection of SUD treatment and FBT, both within the United States substance use treatment facilities and beyond, especially as FBT could increase SUD treatment retention. In doing so, a clearer picture of current treatment strategies and areas for improving treatment integration can be delineated.
Data Availability
The National Treatment Center Study (NTCS) data used for the current study are available to the public via NAHDAP / ICPSR: https://www.icpsr.umich.edu/web/NAHDAP/studies/37621/staff.
References
Aletraris, L., & Roman, P. M. (2015). Provision of onsite HIV services in substance use disorder treatment programs: A longitudinal analysis. Journal of Substance Abuse Treatment, 57, 1–8. https://doi.org/10.1016/j.jsat.2015.04.005.
Aletraris, L., Paino, M., Edmond, M. B., Roman, P. M., & Bride, B. E. (2014). The use of art and music therapy in substance abuse treatment programs. Journal of Addictions Nursing, 25(4), 190. https://doi.org/10.1097/jan.0000000000000048.
Aletraris, L., Edmond, M. B., & Roman, P. M. (2015a). Adoption of injectable naltrexone in US substance use disorder treatment programs. Journal of Studies on Alcohol and Drugs, 76(1), 143–151. https://doi.org/10.1016/j.jsat.2015.04.005.
Aletraris, L., Shelton, J. S., & Roman, P. M. (2015b). Counselor attitudes toward contingency management for substance use disorder: Effectiveness, acceptability, and endorsement of incentives for treatment attendance and abstinence. Journal of Substance Abuse Treatment, 57, 41–48. https://doi.org/10.1016/j.jsat.2015.04.012.
Aletraris, L., Edmond, M. B., Paino, M., Fields, D., & Roman, P. M. (2016). Counselor training and attitudes toward pharmacotherapies for opioid use disorder. Substance Abuse, 37(1), 47–53. https://doi.org/10.1080/08897077.2015.1062457.
Aletraris, L., Edmond, M. B., & Roman, P. M. (2017a). Insurance receipt and readiness for opportunities under the affordable care act: A national survey of treatment providers for substance use disorders. Journal of Psychoactive Drugs, 49(2), 141–150. https://doi.org/10.1080/02791072.2017.1306661
Aletraris, L., Roman, P. M., & Pruett, J. (2017b). Integration of care in the implementation of the affordable care act: Changes in treatment services in a national sample of centers treating substance use disorders. Journal of Psychoactive Drugs, 49(2), 132–140. https://doi.org/10.1080/02791072.2017.1299263
ATTCN (2018). Motivational Incentives—A Proven Approach to Treatment. Addiction Technology Transfer Center Network. https://attcnetwork.org/centers/attc-network-coordinating-office/product/motivational-incentives-proven-approach-treatment.
Bartle-Haring, S., Slesnick, N., & Murnan, A. (2018). Benefits to children who participate in Family Therapy with their substance‐using mother. Journal of Marital and Family Therapy, 44(4), 671–686. https://doi.org/10.1111/jmft.12280.
Bea Blacklow, D., Walker, S., & Sinha, L. (2012). Henderson Treatment Episode Data Set (TEDS): 2000–2010 National Admissions to Substance Abuse Treatment Services. Synectics for Management Decisions, Inc. https://www.samhsa.gov/data/2k12/TEDS2010N/TEDS2010NWeb.pdf.
Berg, I. K., & Miller, S. D. (1992). Working with the problem drinker: A solution-focused approach. WW Norton & Company.
Briones, E., Robbins, M., & Szapocznik, J. (2008). Brief strategic family therapy: Engagement and treatment. Alcoholism Treatment Quarterly, 26(1–2), 81–103. https://doi.org/10.1300/j020v26n01_05.
Brook, J., & McDonald, T. (2009). The impact of parental substance abuse on the stability of family reunifications from foster care. Children and Youth Services Review, 31(2), 193–198. https://doi.org/10.1016/j.childyouth.2008.07.010.
Brown, T. L., Henggeler, S. W., Schoenwald, S. K., Brondino, M. J., & Pickrel, S. G. (1999). Multisystemic treatment of substance abusing and dependent juvenile delinquents: Effects on school attendance at posttreatment and 6-month follow-up. Children’s Services: Social Policy Research and Practice, 2(2), 81–93. https://doi.org/10.1207/s15326918cs0202_2.
Burnam, M. A., & Watkins, K. E. (2006). Substance abuse with mental disorders: Specialized public systems and integrated care. Health Affairs, 25(3), 648–658. https://doi.org/10.1377/hlthaff.25.3.648.
Cafferky, B. M., Mendez, M., Anderson, J. R., & Stith, S. M. (2018). Substance use and intimate partner violence: A meta-analytic review. Psychology of Violence, 8(1), 110. https://doi.org/10.1037/vio0000074.supp.
Center for Behavioral Health Statistics and Quality (2023). 2023 National Survey on Drug Use and Health (NSDUH): Prescription drug images for the 2023 questionnaires Substance Abuse and Mental Health Administration.
Center for Disease Control and Prevention, National Center for Injury Prevention and Control (2023). Drug overdose death rates Center for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/deaths/index.html.
Chou, J. L., Patton, R., Zaarur, A., Katafiasz, H., Swint, P., Dang, Y., & Feeney, E. (2023 Aug). Understanding families impacted by opioid use: Outcomes of a therapist training program. Families, Systems & Health : The Journal of Collaborative Family Healthcare, 24, https://doi.org/10.1037/fsh0000818.
Cranford, J. A. (2014). DSM-IV alcohol dependence and martial dissolution: Evidence from the national epidemiologic survey on Alcohol and related conditions. Journal of Studies on Alcohol and Drugs, 75(3), 520–529. https://doi.org/10.15288/jsad.2014.75.520.
Cunningham, P. B., & Henggeler, S. W. (1999). Engaging multiproblem families in treatment: Lessons learned throughout the development of multisystemic therapy. Family Process, 38(3), 265–281. https://doi.org/10.1111/j.1545-5300.1999.00265.x.
Daley, D. C. (2013). Family and social aspects of substance use disorders and treatment. Journal of Food and Drug Analysis, 21(4, Supplement), S73–S76. https://doi.org/10.1016/j.jfda.2013.09.038.
Ducharme, L. J., & Abraham, A. J. (2008). State policy influence on the early diffusion of buprenorphine in community treatment programs. Substance Abuse Treatment Prevention and Policy, 3, 1–10. https://doi.org/10.1186/1747-597x-3-17.
Ducharme, L. J., Knudsen, H. K., & Roman, P. M. (2006). Availability of integrated care for co-occurring substance abuse and psychiatric conditions. Community Mental Health Journal, 42(4), 363–375. https://doi.org/10.1007/s10597-005-9030-7.
Dutcher, L. W., Anderson, R., Moore, M., Luna-Anderson, C., Meyers, R. J., Delaney, H. D., & Smith, J. E. (2009). Community reinforcement and family training (CRAFT): An effectiveness study. Journal of Behavior Analysis in Health Sports Fitness and Medicine, 2(1), 80. https://doi.org/10.1037/h0100376.
Edmond, M. B., Aletraris, L., & Roman, P. M. (2015). Rural substance use treatment centers in the United States: An assessment of treatment quality by location. The American Journal of Drug and Alcohol Abuse, 41(5), 449–457. https://doi.org/10.3109/00952990.2015.1059842.
Fals-Stewart, W., O’Farrell, T. J., Feehan, M., Birchler, G. R., Tiller, S., & McFarlin, S. K. (2000). Behavioral couples therapy versus individual-based treatment for male substance-abusing patients: An evaluation of significant individual change and comparison of improvement rates. Journal of Substance Abuse Treatment, 18(3), 249–254. https://doi.org/10.1016/s0740-5472(99)00059-8.
HealthCare.gov (2022). Enroll in Medicaid or CHIP any time of year. HealthCare Gov. https://www.healthcare.gov/medicaid-chip/getting-medicaid-chip/.
Henderson, C. E., Dakof, G. A., Greenbaum, P. E., & Liddle, H. A. (2010). Effectiveness of multidimensional family therapy with higher severity substance-abusing adolescents: Report from two randomized controlled trials. Journal of Consulting and Clinical Psychology, 78(6), 885. https://doi.org/10.1037/a0020620.
Henderson, J. L., Cheung, A., Cleverley, K., Chaim, G., Moretti, M. E., de Oliveira, C., Hawke, L. D., Willan, A. R., O’Brien, D., & Heffernan, O. (2017). Integrated collaborative care teams to enhance service delivery to youth with mental health and substance use challenges: Protocol for a pragmatic randomized controlled trial. British Medical Journal Open, 7(2), e014080. https://doi.org/10.1136/bmjopen-2016-014080.
Henggeler, S. W. (1999). Multisystemic therapy: An overview of clinical procedures, outcomes, and policy implications. Child Psychology and Psychiatry Review, 4(1), 2–10. https://doi.org/10.1111/1475-3588.00243.
Henggeler, S. W., Pickrel, S. G., & Brondino, M. J. (1999). Multisystemic treatment of substance-abusing and-dependent delinquents: Outcomes, treatment fidelity, and transportability. Mental Health Services Research, 1, 171–184.
Henggeler, S. W., Clingempeel, W. G., Brondino, M. J., & Pickrel, S. G. (2002). Four-year follow-up of multisystemic therapy with substance-abusing and substance-dependent juvenile offenders. Journal of the American Academy of Child & Adolescent Psychiatry, 41(7), 868–874. https://doi.org/10.1097/00004583-200207000-00021.
Henggeler, S. W., Schoenwald, S. K., Borduin, C. M., Rowland, M. D., & Cunningham, P. B. (2009). Multisystemic therapy for antisocial behavior in children and adolescents (2nd ed.). Guilford Press.
Henkel, D. (2011). Unemployment and substance use: A review of the literature (1990–2010). Current Drug Abuse Reviews, 4(1), 4–27. https://doi.org/10.2174/1874473711104010004.
Hogue, A., Schumm, J. A., Maclean, A., & Bobek, M. (2022). Couple and family therapy for substance use disorders: Evidence-based update 2010–2019. Journal of Marital and Family Therapy, 48(1), 178–203. https://doi.org/10.1111/jmft.12546.
Horigian, V. E., Anderson, A., R., & Szapocznik, J. (2016). Family-based treatments for adolescent substance use. Child and Adolescent Psychiatric Clinics, 25(4), 603–628. https://doi.org/10.1016/j.chc.2016.06.001.
IBM SPSS Statistics for Windows, Version 27.0. IBM Corp. Kampman, K., & IBM Corp, & Jarvis, M. (2020). (2015). American Society of Addiction Medicine (ASAM) national practice guideline for the use of medications in the treatment of addiction involving opioid use. Journal of addiction medicine, 9(5), 358. https://doi.org/10.1097/adm.0000000000000166.
Kaur, L., Tadros, E., & Patton, R. (2019). The role of family in youth opioid misuse: A literature review. The Family Journal, 27(4), 429–442. https://doi.org/10.1177/1066480719868705.
Knight, K. E., Menard, S., & Simmons, S. B. (2014). Intergenerational continuity of substance use. Substance Use & Misuse, 49(3), 221–233. https://doi.org/10.3109/10826084.2013.824478.
Knudsen, H. K., & Roman, P. M. (2004). Modeling the use of innovations in private treatment organizations: The role of absorptive capacity. Journal of Substance Abuse Treatment, 26(1), 51–59. https://doi.org/10.1016/s0740-5472(03)00158-2.
Knudsen, H. K., & Roman, P. M. (2015). Medicaid, private insurance, and the availability of smoking cessation interventions in substance use disorder treatment. Psychiatric Services, 66(11), 1213–1220. https://doi.org/10.1176/appi.ps.201400451.
Knudsen, H. K., & Roman, P. M. (2016). The diffusion of acamprosate for the treatment of alcohol use disorder: Results from a national longitudinal study. Journal of Substance Abuse Treatment, 62, 62–67. https://doi.org/10.1016/j.jsat.2015.10.005.
Knudsen, H. K., Ducharme, L. J., & Roman, P. M. (2007). The adoption of medications in substance abuse treatment: Associations with organizational characteristics and technology clusters. Drug and Alcohol Dependence, 87(2–3), 164–174. https://doi.org/10.1016/j.drugalcdep.2006.08.013.
Lam, W. K., Fals-Stewart, W., & Kelley, M. L. (2009). Parent training with behavioral couples therapy for fathers’ alcohol abuse: Effects on substance use, parental relationship, parenting, and CPS involvement. Child Maltreatment, 14(3), 243–254. https://doi.org/10.1177/1077559509334091.
Lander, L., Howsare, J., & Byrne, M. (2013). The impact of substance use disorders on families and children: From theory to practice. Soc Work Public Health, 28(3–4), 194–205. https://doi.org/10.1080/19371918.2013.759005.
Liddle, H. A., Dakof, G. A., Rowe, C. L., Henderson, C., Greenbaum, P., Wang, W., & Alberga, L. (2018). Multidimensional Family Therapy as a community-based alternative to residential treatment for adolescents with substance use and co-occurring mental health disorders. Journal of Substance Abuse Treatment, 90, 47–56. https://doi.org/10.1016/j.jsat.2018.04.011.
McCaul, M. E., Svikis, D. S., & Moore, R. D. (2001). Predictors of outpatient treatment retention: Patient versus substance use characteristics. Drug and Alcohol Dependence, 62(1), 9–17. https://doi.org/10.1016/s0376-8716(00)00155-1.
McCollum, E. E., & Trepper, T. S. (2014). Family solutions for substance abuse: Clinical and counseling approaches. Routledge. https://doi.org/10.4324/9781315809571.
McGovern, M. P., & Carroll, K. M. (2003). Evidence-based practices for substance use disorders. Psychiatric Clinics, 26(4), 991–1010. https://doi.org/10.1016/s0193-953x(03)00073-x.
Morgan, T. B., & Crane, D. R. (2010). Cost-effectiveness of family‐based substance abuse treatment. Journal of Marital and Family Therapy, 36(4), 486–498. https://doi.org/10.1111/j.1752-0606.2010.00195.x.
Morgan, T. B., Crane, D. R., Moore, A. M., & Eggett, D. L. (2013). The cost of treating substance use disorders: Individual versus family therapy. Journal of Family Therapy, 35(1), 2–23. https://doi.org/10.1111/j.1467-6427.2012.00589.x.
National Institute on Drug Abuse (2018). Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition) Retrieved from https://archives.nida.nih.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition on 2024, January 15.
Paino, M., Aletraris, L., & Roman, P. M. (2015). Organizational predictors and use of evidence-based practices in adolescent substance abuse treatment. Substance Abuse, 36(4), 462–469. https://doi.org/10.1080/08897077.2014.960959.
Paino, M., Aletraris, L., & Roman, P. (2016). The relationship between client characteristics and wraparound services in substance use disorder treatment centers. Journal of Studies on Alcohol and Drugs, 77(1), 160–169. https://doi.org/10.15288/jsad.2016.77.160.
Pfeffer, J. (1997). New directions for organization theory: Problems and prospects. Oxford University Press. https://doi.org/10.1093/oso/9780195114348.003.0009.
Pfeffer, J., & Salancik, G. R. (2003). The external control of organizations. [electronic resource]: A resource dependence perspective. Stanford Business Books.
Reiter, M. D. (2019). Substance abuse and the family: Assessment and treatment. Routledge. https://doi.org/10.4324/9780429459573.
Robbins, M. S., Szapocznik, J., & Pe’rez, G. A. (2000). Brief strategic family therapy. Handbook of homework assignments in psychotherapy: Research, practice, and prevention (pp. 133–149). Springer US. https://doi.org/10.1007/978-0-387-29681-4_9.
Robbins, M. S., Mayorga, C. C., Mitrani, V. B., Szapocznik, J., Turner, C. W., & Alexander, J. F. (2008). Adolescent and parent alliances with therapists in brief strategic family therapy with drug-using hispanic adolescents. Journal of Marital and Family Therapy, 34(3), 316–328. https://doi.org/10.1111/j.1752-0606.2008.00075.x.
Rogers, E. M. (2003). Diffusion of innovations (5th ed.). Free.
Ruff, S., McComb, J. L., Coker, C. J., & Sprenkle, D. H. (2010). Behavioral couples therapy for the treatment of substance abuse: A substantive and methodological review of O’Farrell, Fals-Stewart, and colleagues’ program of research. Family Process, 49(4), 439–456. https://doi.org/10.1111/j.1545-5300.2010.01333.x.
Saad, L. (2019). Substance abuse hits home for close to half of Americans. Gallup. https://news.gallup.com/poll/267416/substance-abuse-hits-home-close-half-americans.aspx.
Saatcioglu, O., Erim, R., & Cakmak, D. (2006). Role of family in alcohol and substance abuse. Psychiatry and Clinical Neurosciences, 60, 125–132. https://doi.org/10.1111/j.1440-1819.2006.01476.x.
Santisteban, D. A., Dillon, F., Mena, M. P., Estrada, Y., & Vaughan, E. L. (2005). Psychiatric, family, and ethnicity-related factors that can impact treatment utilization among hispanic substance abusing adolescents. Journal of Social Work Practice in the Addictions, 5(1–2), 133–155. https://doi.org/10.1300/j160v5n01_07.
Smith, J. A., Hayes, N. D., & Smock Jordan, S. (2019). Systemic integration of IFS therapy and 12-step facilitation for substance use: A theoretical discussion. Alcoholism Treatment Quarterly, 37(1), 60–74. https://doi.org/10.1080/07347324.2018.1502032.
Stanton, M. D. (1981). An integrated structural/strategic approach to family therapy. Journal of Marital and Family Therapy, 7(4), 427–439. https://doi.org/10.1111/j.1752-0606.1981.tb01397.x.
Stanton, M. D., & Shadish, W. R. (1997). Outcome, attrition, and family–couples treatment for drug abuse: A meta-analysis and review of the controlled, comparative studies. Psychological Bulletin, 122(2), 170. https://doi.org/10.1037//0033-2909.122.2.170.
Stanton, M. D., & Todd, T. C. (Eds.). (1982). The family therapy of drug abuse and addiction. Guilford Press.
Substance Abuse and Mental Health Services Administration (2020). Substance Use Disorder Treatment and Family Therapy Treatment Improvement Protocol (TIP) series, No. 39. SAMHSA Publication No. PEP20-02-02-012. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2020.
Substance Abuse and Mental Health Services Administration, & Series (2011). H-41, HHS Publication NO. (SMA) 11-4658. Results from the 2010 National Survey on Drug Use and Health: Summary of National findings. Substance Abuse and Mental Health Services Administration. NSDUH.
Szapocznik, J. (2003). Therapy Manuals for Drug Addiction: Brief strategic family therapy for adolescent drug abuse. Manual 5 (No. 3). US Department of Health and Human Services, National Institutes of Health, National Institute on Drug Abuse.
Szapocznik, J., & Williams, R. A. (2000). Brief strategic family therapy: Twenty-five years of interplay among theory, research and practice in adolescent behavior problems and drug abuse. Clinical Child and Family Psychology Review, 3, 117–134. https://doi.org/10.1037/14550-015.
Szapocznik, J., Perez-Vidal, A., Brickman, A., Foote, F. H., Santisteban, D., Hervis, O. E., & Kurtines, W. M. (1988). Engaging adolescent drug abusers and their families into treatment: A strategic structural systems approach. Journal of Consulting and Clinical Psychology, 56, 552–557. https://doi.org/10.1037/0022-006x.56.4.552.
Szapocznik, J., Muir, J. A., & Schwartz, S. J. (2013). Brief strategic family therapy for adolescent drug abuse: Treatment and implementation. Encyclopedia of Addictive Behaviors, 3, 97–108. https://doi.org/10.1016/b978-0-12-398338-1.00011-7.
Tambling, R. R., Russell, B., & D’Aniello, C. (2021). Where is the family in young adult substance use treatment? The case for systemic family therapy for young adults with substance use disorders. International Journal of Mental Health and Addiction, 20, 1659–1670. https://doi.org/10.1007/s11469-020-00471-1.
Vardanian, M. M., Scavenius, C., Granski, M., & Chacko, A. (2020). An International examination of the effectiveness of functional family therapy (FFT) in a Danish community sample. Journal of Marital and Family Therapy, 46(2), 289–303. https://doi.org/10.1111/jmft.12405.
Ventura, A. S., & Bagley, S. M. (2017). To improve substance use disorder prevention, treatment, and recovery: Engage the family. Journal of Addiction Medicine, 11(5), 339–341. https://doi.org/10.1097/adm.0000000000000331.
Werner, D., Young, N. K., Dennis, K., & Amatetti, S. (2007). ). Family-centered treatment for women with Substance Use disorders – history, Key Elements and challenges. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration.
Wong, J., Saver, B., Scanlan, J. M., Gianutsos, L. P., Bhakta, Y., Walsh, J., Plawman, A., Sapienza, D., & Rudolf, V. (2020). The ASAM clinical practice guideline on alcohol withdrawal management. Journal of Addiction Medicine, 14(3S), 1–72. https://doi.org/10.1097/adm.0000000000000668.
Acknowledgements
The project was funded by National Institute on Drug Abuse, grant # R37DA013110, PI: Roman.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chou, J.L., Patton, R., Aletraris, L. et al. Examining Utilization of Family-Based Treatment in Substance Use Treatment Centers. Contemp Fam Ther (2024). https://doi.org/10.1007/s10591-024-09700-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s10591-024-09700-4