Abstract
Cell transplantation is a promising treatment option for spinal cord injury (SCI). However, there is no consensus on the choice of carrier scaffolds to host the cells. This study aims to evaluate the efficacy of different material scaffold-mediated cell transplantation in treating SCI in rats. According to PRISMA’s principle, Embase, PubMed, Web of Science, and Cochrane databases were searched, and relevant literature was referenced. Only original research on cell transplantation plus natural or synthetic scaffolds in SCI rats was included. Direct and indirect evidence for improving hind limb motor function was pooled through meta-analysis. A subgroup analysis of some factors that may affect the therapeutic effect was conducted to understand the results fully. In total, 25 studies met the inclusion criteria, in which 293 rats received sham surgery, 78 rats received synthetic material scaffolds, and 219 rats received natural materials scaffolds. The network meta-analysis demonstrated that although synthetic scaffolds were slightly inferior to natural scaffolds in terms of restoring motor function in cell transplantation of SCI rats, no statistical differences were observed between the two (MD: −0.35; 95% CI −2.6 to 1.9). Moreover, the subgroup analysis revealed that the type and number of cells may be important factors in therapeutic efficacy (P < 0.01). Natural scaffolds and synthetic scaffolds are equally effective in cell transplantation of SCI rats without significant differences. In the future, the findings need to be validated in multicenter, large-scale, randomized controlled trials in clinical practice.
Trial registration: Registration ID CRD42024459674 (PROSPERO).
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal cord injury (SCI) is a severe neurological disorder usually caused by mechanical trauma, such as traffic accidents, falls, and sports-related injuries. Not only can it lead to a series of symptoms, such as severe loss of movement, sensory impairment, and autonomic nervous dysfunction, but it also causes complications, such as neuropathic pain, that seriously impair the patient’s quality of life. SCI is estimated to affect nearly 180,000 people each year due to its high incidence, disability, and death rate (Fitzharris et al. 2014). Currently, the clinical treatment of SCI primarily includes decompression surgery, steroid hormone shock therapy, and neurological rehabilitation exercise (Silva et al. 2014). The above-mentioned treatments alleviated the secondary neuronal degeneration and necrosis to a certain extent. However, due to the highly differentiated and nonrenewable nature of neurons, direct primary neuronal death often makes the prognosis of patients unsatisfactory (Badhiwala et al. 2021; Curt et al. 2008). Theoretically, exogenously restoring neurons is the optimal approach to SCI; thus, cell transplantation (mature nerve cells or stem cells with the potential to differentiate) has emerged as a treatment for SCI (Tetzlaff et al. 2011).
Several preclinical studies demonstrated that stem cells transplanted in SCI animal models could restore synaptic connections and neural networks through direct neuronal regeneration or paracrine effects (Rong et al. 2019; Li et al. 2020; Deng et al. 2015). Some problems still need to be addressed in the large-scale clinical application of cell transplantation in patients with SCI, such as determining the best timing for neural stem cell therapy, the source of neural stem cells, the route of administration of cell transplantation, the number of transplanted cells, and the best combination of treatment. However, advancements in stem cell therapy technology and tissue engineering technology are continuously unlocking the potential of cell transplantation. Therefore, studies should be conducted to comprehensively evaluate and analyze the efficacy of cell transplantation in SCI. Some reports have shown the efficacy of single-cell transplantation in the subacute phase (Ide et al. 2010; Yang et al. 2020) and some reports have started clinical trials (Anderson et al. 2017; Karamouzian et al. 2012; Sugai et al. 2021). In order to achieve the ideal recovery effect of cell transplantation therapy, the emergence of scaffolds has enriched the treatment of cell transplantation. At present, the curative effects of SCI may not be significantly improved through single-cell transplantation, which may be associated with the survival of transplanted cells, directional migration to the lesion site, differentiation, and axonal regeneration of transplanted cells (Yousefifard et al. 2022; Yousefifard et al. 2019). Comprehensive cell transplantation therapy combined with tissue engineering scaffolds became a trend. Scaffolds can fill the gap between lesion sites and serve as a supportive physical medium. Furthermore, they can also preserve the activity of transplanted cells and mediate the directional growth of axons to act as a bridge to restore neural networks. The use of biomaterials can enhance the effect of cell transplantation. In future, scaffold and cell engineering technologies may improve cell survival, integration, and therapeutic efficiency (Zipser et al. 2022). Compared with single-cell transplantation, the therapeutic effect of cell transplantation with scaffold combined therapy is synergistically enhanced, which is more effective in promoting neurological recovery after SCI (Zweckberger et al. 2016; Liu et al. 2013a, b, c). Consequently, many studies on scaffolds combined with cell transplantation were conducted in animal models to pave the way for clinical practice.
Scaffolds are divided into natural biomaterials (such as hyaluronic acid, collagen, and acellular scaffolds) and synthetic biomaterials (polylactic acid-glycolic acid copolymer and polylactic acid), both of which have their advantages (Wang et al. 2015; Kubinová and Syková 2010). The primary advantages of natural biomaterials are their excellent biocompatibility, low immunogenicity, and nontoxic degradation (Libro et al. 2017). Synthetic biomaterials are usually easier to adjust than natural biomaterials. For instance, the porosity, stiffness, and degradation rate of synthetic biomaterials can be altered to match different types of tissue (Subramanian et al. 2009). Concurrently, they also have a low incidence of inflammatory response (Subramanian et al. 2009). Most prior studies on cell transplantation for SCI focused on stem cells or nerve cells in cell transplantation (Antonic et al. 2013), but no systematic review on the selection of scaffolds was exclusively conducted. Therefore, analyzing the therapeutic effects of scaffold-assisted cell transplantation in SCI is necessary, as this will provide a direction for subsequent large-scale clinical trials and applications of patients.
Methods
Literature Search
This meta-analysis was conducted under the requirements listed in the Preferred Reporting Items of Systematic Review and Meta-Analysis (PRISMA). English articles of randomized controlled trials (RCTs) in EMBASE, PubMed, Web of Science, and Cochrane databases were searched until September 2023. Moreover, if the article that met our criteria appeared in its references, the full text from the PubMed database was retrieved to evaluate its suitability for our study. The subject search terms were as follows in all four databases: Spinal Cord Injury AND (“Cell Transplantation” OR “Stem Cell Transplantation”) AND (“Scaffolds” OR “Tissue Scaffolds”). More details could be seen in Supplementary material.
Selection Criteria
After removing duplicate references retrieved from the above databases and sorting out all references, the inclusion criteria are as follows:
-
(1)
The animal model of SCI is the rat.
-
(2)
SCI modeling, such as contusion, hemisection, or transection, must be accepted by the mainstream.
-
(3)
The components of the scaffold used for cell transplantation are clear and detailed.
-
(4)
There must be a blank control (SCI group without therapeutic measures). Vehicle group: the rats were injected intrathecal saline or PBS equal to the amount of cell fluid after surgery of causing SCI.
-
(5)
The follow-up time is more than four weeks, and there are outcome measures to evaluate the motor function.
-
(6)
The articles are published in English.
The exclusion criteria are as follows:
-
(1)
Non-English literature and review articles are excluded.
-
(2)
No control group is compared.
-
(3)
The postoperative motor function of rats is not quantitatively reported.
Literature Collection
Two researchers (Jun Li and Zhihua Wang) independently searched for relevant literature from various electronic literature databases and selected all studies that met the above criteria through titles and abstracts (checking the full text if necessary). Both researchers were responsible for assessing whether a manuscript was suitable for inclusion in the meta-analysis. If the two had opposing viewpoints, they would resolve them through group discussion and negotiation until a consensus was reached.
Data Extraction
Two investigators (Zhiping Xie and Tianqi Xu) independently extracted the main data of every article from the selected original researches. The data included (1) basic information about every article, such as the first author and year of publication of every article; (2) detailed information, such as gender and weight of rats, the corresponding number of rats in each group, method of inducing spinal cord injury (contusion, spinal cord hemisection, or transection), cell donor and type, transplanted cell quantity, scaffold material, use of antibiotics, use of immunosuppressants, the time interval from SCI to corresponding transplantation treatment, the duration of prognosis observation, motor function score, and double-blind assessment of motor function. All included literature used Basso–Beattie–Bresnahan (BBB) scores to evaluate the motor function of the hind limbs of rats, and the scores were positively proportional to the recovery of the motor function of rats (Basso et al. 1995). We preferred using digital data reported in the articles. If the data were presented only in the form of charts, PLOT digital software was used to extract data. If necessary, we would contact the corresponding authors of eligible studies via e-mail to obtain sufficient data.
Quality Assessment of Literature
The quality of the included studies was independently evaluated by two authors (Boyu Guo and Meihua Li). Because all included studies were RCTs on rats, Hassannejad et al.’s study was reasonably selected to make an overall judgment on the quality of each study (Hassannejad et al. 2016). They conducted a risk assessment using a 15-item checklist as a guide. They assessed risks from the animal (4 items), assessment (10 items), and housing (1 item) variables for evaluating the quality of the included studies (Table 1). The two authors strictly adhered to the research standards established by Hassannejad et al. If their opinions on a study differed, the group would discuss it until they agreed.
Statistical Analysis
All statistical analyses were conducted using R software (version 5.4.1, Cochrane Collaboration, London). Since the outcome measures of all included studies were presented in the form of continuous data (BBB score), we used Mean ± SD to directly or indirectly compare the therapeutic effects of cell transplantation plus scaffolds of different materials in rats with SCI. As the meta-analysis included different studies and there was relatively significant heterogeneity between studies (P < 0.1 or I2 > 50%), the data were consolidated using a random-effects model. Furthermore, subgroup analyses were performed to trace the source of heterogeneity or the study was subdivided to get a full picture of the results. Published bias was examined using a funnel plot. If the funnel plot was visually symmetric, this indicates that there was no publication bias.
Results
The Characteristics of Included Studies
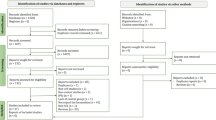
After four databases or interesting citations were comprehensively searched and duplicate references were eliminated, 252 articles were reviewed by title and abstract. After preliminary screening, the full text of 142 articles was reviewed to assess the necessity of inclusion. Finally, 25 articles were included in the network meta-analysis (NMA) (Chen et al. 2014; Deng et al. 2020; Han et al. 2019; Hatami et al. 2009; Hejcl et al. 2010; Hosseini et al. 2016; Jiao et al. 2017; Kim et al. 2016; Liu et al. 2015; Liu et al. 2013a; Liu et al. 2013b; Liu et al. 2022; Marchini et al. 2019; Peng et al. 2018; Raynald et al. 2019; Ropper et al. 2017; Tavakol et al. 2014; Wang et al. 2020; Wang et al. 2016; Wang et al. 2021; Wang et al. 2017; Yang et al. 2017; You et al. 2019; Zaminy et al. 2013;Zarei-Kheirabadi et al. 2020). Figure 1 demonstrates the details of the inclusion assessment.
Of the 25 articles, 24 were two-arm studies, i.e., cell transplantation + scaffolds (natural or synthetic materials) vs. vehicle control group, except for one study that was a three-arm study directly comparing both different types of scaffolds to the control group (Kim et al. 2016). In other words, while nineteen studies compared the efficacy differences between cell transplantation + natural scaffolds in SCI rats and vehicle control group in SCI rats, seven articles focused on synthetic scaffolds (Han et al. 2019; Hejcl et al. 2010; Kim et al. 2016; Liu et al. 2015; Raynald et al. 2019; Ropper et al. 2017; Yang et al. 2017).
A total of 590 SCI rats were examined in different experiments, with 293 SCI rats not receiving any therapeutic intervention (except normal saline or PBS), 78 rats receiving synthetic scaffold-assisted cell transplantation, and 219 rats receiving natural scaffold-assisted cell transplantation. For the study participants, the selected animal models were all rats, and the methods of causing spinal cord injury included contusion (32%), spinal cord hemisection (40%), and spinal cord transection (28%). Regarding intervention, the cell types used for cell transplantation were primarily mesenchymal stem cells (MSCs) and neural stem cells, with a total number of cells transplanted ranging from 10,000 to 5000000 and a time span from injury to therapeutic intervention ranging from immediately to 35 days. For comparison, the vehicle group was used as the control group, while the cell transplantation combined scaffold served as the experimental group. The components of natural scaffolds include collagen, fibroin, acellular, fibrin, and sodium alginate. The synthetic scaffolds were mainly synthetic polymers, such as polylactic-co-glycolic acid (PLGA). In terms of outcomes, the duration of the assessment was all greater than 4 weeks, ranging from 4 weeks to 2 years. The BBB score was used to measure the functionality improvement of the hind limbs, and two or more independent researchers evaluated 80% of the studies to avoid human-induced error (Table 2).
Quality Assessment of the Articles
Among the 25 pieces of literature included, most of the top 14 items of the included studies were considered low risk, indicating the good quality of the articles (Table 1). However, bladder expression was not documented in detail in six studies, and it was unclear whether the BBB score of hind limb movement in SCI rats was evaluated double blind in four studies. Furthermore, most studies did not explain in the literature why some animals were excluded (item 15).
Evidence Network
This NMA contains 19 articles comparing the efficacy of natural material scaffold-assisted cell transplantation and the vehicle control group in treating SCI rats, 7 articles on synthetic material scaffold-assisted cell transplantation, and a direct comparison of natural material against synthetic material scaffolds for the treatment of SCI rats. The red lines between each ball indicate that different interventions are directly compared. The width of the red line can be considered as the number of included studies (Fig. 2).
Functional Outcomes
Our results reveal that both natural scaffold-driven cell transplantation (MD: 6.0; 95% CI 4.8–7.2) and synthetic scaffold-driven cell transplantation (MD: 5.7; 95% CI 3.7–7.7) are superior to the control group in treating SCI rats, with statistically significant differences (Fig. 3). The direct comparison of two different types of scaffolds demonstrates that the synthetic scaffolds are inferior to the natural scaffolds (MD: -0.80; 95% CI -3.8 to 2.2), and the indirect comparisons also acknowledge subtle differences in the efficacy of synthetic materials (MD: -0.28; 95% CI -2.7 to 2.1). In summary, the NMA demonstrated that synthetic scaffold-assisted cell transplantation in SCI rats is less effective than natural materials (MD: -0.35; 95% CI -2.6 to 1.9). However, no statistical difference was observed between the two types of scaffold (Fig. 4).
Subgroup Analysis
I2 was used to test for heterogeneity among the evidence (Fig. 4). Given that I2 was mostly over 50%, the heterogeneity among the evidence was high, so we tried to conduct a subgroup analysis to find the source of heterogeneity. Similarly, the random-effects model was applied to the meta-models.
Subgroup analysis was performed in two cohorts of natural and synthetic materials with respect to gender, mode of SCI injury, origin of cells, time period from injury to treatment, number of cells, whether immunosuppressants were used, whether antibiotics were used, duration of follow-up evaluation of BBB score, and whether the study is double blind or not (Tables 3, 4). Heterogeneity among subgroups of different categorical variables remains large; therefore, the source of heterogeneity between studies has not been tracked. Interestingly, significant differences were observed in terms of efficacy between subgroups with different cell counts in the natural material cohort (P < 0.01), whereas no other subgroup variables affected the difference in efficacy (all P > 0.05), suggesting that the number of cells transplanted is a potential factor influencing SCI treatment. To verify the results’ generalizability, we conducted a subgroup analysis that included cell transplantation with different scaffold types for SCI and its results supported the conclusions described above (Table 5, P < 0.01). However, in the synthetic cohort, cell type and the use of immunosuppressants become the differentiating variables for differences in efficacy (P < 0.01).
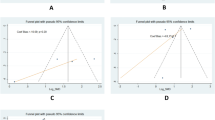
Inconsistency Test
The interventions in the NMA form a closed loop. Because consistency testing is required, the node-splitting method and its Bayes P value are used to evaluate the inconsistencies of our results between direct and indirect outcomes. In Fig. 5, although they are not statistically significant, the direct (MD: -0.85; 95% CI -6.5 to 4.8) and the indirect results (MD: -0.24; 95% CI -2.8 to 2.4) both support that natural materials are better than synthetic materials in SCI rats for cell transplantation. Similarly, the inconsistency test demonstrates that the P value (0.8345) is greater than 0.05, indicating there is no inconsistency in the overall analysis, and the results of direct comparison and indirect comparison are consistent (Fig. 5).
Ranking Probability
The ranking probabilities of these different interventions of the NMA are illustrated in Fig. 6. Ranking probability is used to evaluate the possibility of optimal treatment for SCI rats. According to the ranking probability map, the best probability order of the effect of two different scaffold-assisted cell transplantation on BBB score was natural material (probability = 0.62) > synthetic material (probability = 0.38) > vehicle group (probability = 0).
Convergence Diagnosis
The convergence diagnostic graph is close to 1, indicating that the NMA model fits well (Fig. 7). The trajectory and density map of the included studies are visualized (Fig. 8), and the figure shows that the bandwidth value is close to 0, indicating good convergence.
Publication Bias
Funnel plots are made from the synthetic material cohort, natural material cohort, and all the included literature. They are relatively symmetrical to the naked eye, indicating small publication bias (Fig. 9a–c).
Discussion
Cell transplantation is reviewed as an emerging therapeutic strategy for improving motor function after SCI (Lv et al. 2021). However, the scaffold used as a carrier for cell transplantation has not been thoroughly investigated. Conducting a NMA is of critical importance to compare the efficacy of different types of scaffolds, which can provide reference value for subsequent clinical experiments and even large-scale clinical applications. From the perspective of evidence-based medicine, this study objectively evaluates the rehabilitation effect of cell transplantation on motor function after SCI in rats and compares the efficacy of two different types of scaffolds. In the included studies, the BBB score is used to evaluate the motor function of rats. The higher the score of rats within a certain period after different interventions, the better the prognosis. Our study reveals that cell transplantation can effectively restore the motor function of rats after SCI compared with the vehicle control group, and the natural scaffold seems to be better when considering the type of scaffolds assisted with cell transplantation.
First, our findings show that no matter what type of scaffold-driven cell transplantation is used, it can significantly improve limb movement recovery after SCI in rats when compared to the control group. This result is expected, given that the cell types used for cell transplantation are mostly stem cells known for continuous self-renewal and multidirectional differentiation. They can secrete a variety of nutritional factors to repair damaged tissues and recognize and differentiate into various neurons and glial cells. Based on these unique mechanisms, exogenously supplemented nerve regeneration therapy, that is, cell transplantation, may play a pivotal role in the treatment of SCI by replacing damaged cells, axons, and circuits in the spinal cord.
Second, our NMA results suggest that natural scaffolds are better as cell carriers in cell transplantation. This is reflected in two ways: first, as far as we know, there are very few studies on the treatment of SCI in terms of scaffold types, which highlights the importance of our meta-analysis. The NMA still includes a direct comparison of literature evidence. Direct evidence demonstrates that cell transplantation assisted by natural scaffolds is superior to that by synthetic scaffolds in terms of treating motor function in SCI rats. Moreover, the indirect comparison is completed by the vehicle control group of rats that acts as a transfer connection node, and the analysis results also support the use of natural scaffolds. Based on the above, the generalized consistency hypothesis is established, so the analysis results are of evidence-based significance. The reason for this difference in efficacy may be the poor cell compatibility of the synthetic scaffold, which is prone to the formation of an acidic environment during the degradation process, thus causing certain damage to the cells (Liu et al. 2019a, b). However, natural scaffolds have good biocompatibility, which is reflected in good biodegradability and low side effects. Notably, although the synthetic scaffold is slightly inferior to the natural scaffold in the functional prognosis of SCI rats after surgery, no statistical significance was observed, whether in the direct or indirect comparison of the two scaffold types. Therefore, many high-quality RCTs are warranted to verify our conclusions.
A previous meta-analysis found that acellular spinal cord scaffolds + MSCs were significantly superior to MSCs + other scaffolds when compared to vehicle controls; therefore, acellular spinal cord scaffolds as natural scaffolds strongly support our conclusions about the superiority of natural materials (Yousefifard et al. 2019). However, Yousefifard et al. classified scaffold types in a very specific and nuanced way, specific to the acellular spinal cord, with limited assistance from MSCs. When studies on different scaffolds for MSC transplantation are included in the analysis, our results also suggested that the acellular spinal cord is the optimal relative compared to other scaffolds (data were not present). It should be admitted that our research is relatively broad, aiming to provide a general direction of scaffold type for future research.
Given the broad nature of the NMA conclusions, it is important to recognize that some studies differ significantly, requiring further investigation. In this study, Participants: SCI rats caused by mainstream means; Intervention: rats received cell transplantation or cell transplantation therapy combined with different material scaffolds after SCI; Control or Comparison: the rats were injected saline or PBS equal to the amount of cell fluid after surgery of causing SCI; and Outcome: BBB score, an internationally accepted hindlimb motor function recovery score for rats. As with the PICOS (Participants, Intervention, Control, Outcome, Study design) principle, some details of the intervention (I) and function (O) are worth examining, and the rest of the direction details are almost the same between studies. However, our subgroup analysis of 10 factors did not accurately locate the source of heterogeneity because the number of animals included in the studies was too small to identify significant differentiating variables that led to high heterogeneity. Interestingly, in the subgroup analysis, the cell count was a statistically significant measure of efficacy in treating SCI rats. As a binary variable, 5 × 105 is taken as a critical value of the number of transplanted cells, and we find that a value greater than 5 × 105 is better for subsequent nerve regeneration and recovery in SCI rats. As previously reported, compared to low doses, high-dose transplanted cells can promote the differentiation of transplanted cells into neurons and migration to the injured distal end by regulating the expression of some neurotrophic factors to provide better nutritional support for the site of the spinal cord injury (Teng et al. 2001). Notably, the large number of cells is not always better (Piltti et al. 2017). When the number of stem cells reaches a certain level, more stem cells will lead to a lower proportion of differentiated oligodendrocytes, thus affecting the recovery efficacy, as reported in the meta-analysis by Yousefifard et al. (Yousefifard et al. 2019; Piltti et al. 2017). Their analysis displayed a parabolic trend in the effectiveness of cell dose in the treatment of SCI. Unexpectedly, the use of cell types and immunosuppressive agents can affect the prognosis in the synthetic scaffold cohort. In the natural materials cohort, mesenchymal stem cell is better at improving motor function in SCI rats, but there is no statistical significance. Recently, a systematic review of clinical cell transplantation shows that mesenchymal stem cell ranks first in most of the cells used for transplantation in improving the ASIA Impairment Scale (AIS) grade of SCI patients (Xu et al. 2022). However, only in terms of improvement of motor function, neural stem cell is better than MSC, which is consistent with the results of our synthetic material cohort. This cohort contains only seven studies, and the number of studies between subgroups is not evenly distributed, so this result should be interpreted with caution.
Regarding the optimal timing of cell transplantation, our study shows that no statistical significance in functional recovery was observed between acute (24 h after SCI) and subacute (within 7–10 days after SCI) cell transplantation on both natural and synthetic scaffolds, despite the fact that the acute phase is better. In terms of the transplantation time, some studies reported that the acute phase of SCI has a high rate of apoptosis and inflammatory reactions, resulting in the formation of a toxic microenvironment at the site of spinal cord injury, so glucocorticoid shock therapy is given as a treatment option in the acute phase, and precious cells should be transplanted in the subacute phase (Oh and Jeon 2016). However, our results are similar to those of prior studies; thus, we suggest that transplantation in the acute stage will have better results (Yousefifard et al. 2019). This may be attributed to the fact that secondary damage of SCI typically occurs within a week. Early transplantation of stem cells can effectively mitigate the occurrence of secondary damage and facilitate the restoration of neurological function (Rouanet et al. 2017). Chronic spinal cord injury has many disadvantages in restoring nerve function, including apoptotic neurons in the injured area and surrounding scar tissue, both of which form cavitation that greatly inhibits axon regeneration (Silver and Miller 2004; Hashimoto et al. 2024). In animal studies, cell transplantation combined with scaffolds has also been reported to be effective in chronic SCI with cavity formation, regardless of incomplete or complete SCI injury (Hashimoto et al. 2023; Nori et al. 2018; Liu et al. 2019a, b). Similarly, scaffold is also used clinically, which can improve sensory or motor function in varying proportions in patients with chronic complete SCI (Tang et al. 2022). Therefore, scaffold combined therapy may become a new trend in patients with chronic SCI. However, given that the studies we included did not evaluate enough chronic SCI rats, we cannot draw a firm conclusion about the efficacy of different material scaffold in chronic SCI from our study, which will be an interesting topic for research to address.
One of the advantages of our study is that the subjects included in the study are all rats. We excluded studies on monkeys, dogs, and other animals during the inclusion process to avoid the analytical bias caused by species differences as much as possible. Moreover, we searched many databases to incorporate sufficient literature to avoid publication bias. Because the included literature not only used contusion or complete transection intervention to cause complete SCI but also used spinal cord hemisection to make incomplete SCI in rats, our included studies are universal in the SCI types of various severity. However, limitations should be concerned. Firstly, many of the rat models of spinal cord injury used in these included studies differ from clinical conditions, such as transection and hemisection (Sharif-Alhoseini et al. 2017). Secondly, it is should be admitted the BBB score is subjective (Basso et al. 1995), but the vast majority of the studies we included were double blind in their functional assessment, so the shortcomings of subjectivity can be avoided. Finally, there is still considerable heterogeneity between studies, so the results need to be treated critically. It should be emphasized that there are few studies on the functional recovery of chronic SCI for combined treatment, so it is recommended that subsequent clinical trials focus on acute spinal cord injury (Hejcl et al. 2010). Large-scale, high-quality animal model experiments are warranted to validate our results.
Conclusion
Natural scaffolds and synthetic scaffolds are equally effective in cell transplantation of SCI rats without significant differences. In the future, the findings need to be validated in multicenter, large-scale RCTs in clinical practice.
Data Availability
The data on rats was obtained from the published literature after searching databases; no available data exist.
References
Anderson KD, Guest JD, Dietrich WD, Bartlett Bunge M, Curiel R, Dididze M, Green BA, Khan A, Pearse DD, Saraf-Lavi E, Widerström-Noga E, Wood P, Levi AD (2017) Safety of autologous human Schwann cell transplantation in subacute thoracic spinal cord injury. J Neurotrauma 34(21):2950–2963. https://doi.org/10.1089/neu.2016.4895
Antonic A, Sena ES, Lees JS, Wills TE, Skeers P, Batchelor PE, Macleod MR, Howells DW (2013) Stem cell transplantation in traumatic spinal cord injury: a systematic review and meta-analysis of animal studies. PLoS Biol 11(12):e1001738. https://doi.org/10.1371/journal.pbio.1001738
Badhiwala JH, Wilson JR, Witiw CD, Harrop JS, Vaccaro AR, Aarabi B, Grossman RG, Geisler FH, Fehlings MG (2021) The influence of timing of surgical decompression for acute spinal cord injury: a pooled analysis of individual patient data. Lancet Neurol 20(2):117–126. https://doi.org/10.1016/s1474-4422(20)30406-3
Basso DM, Beattie MS, Bresnahan JC (1995) A sensitive and reliable locomotor rating scale for open field testing in rats. J Neurotrauma 12(1):1–21. https://doi.org/10.1089/neu.1995.12.1
Chen J, Zhang Z, Liu J, Zhou R, Zheng X, Chen T, Wang L, Huang M, Yang C, Li Z, Yang C, Bai X, Jin D (2014) Acellular spinal cord scaffold seeded with bone marrow stromal cells protects tissue and promotes functional recovery in spinal cord-injured rats. J Neurosci Res 92(3):307–317. https://doi.org/10.1002/jnr.23311
Curt A, Van Hedel HJ, Klaus D, Dietz V (2008) Recovery from a spinal cord injury: significance of compensation, neural plasticity, and repair. J Neurotrauma 25(6):677–685. https://doi.org/10.1089/neu.2007.0468
Deng LX, Walker C, Xu XM (2015) Schwann cell transplantation and descending propriospinal regeneration after spinal cord injury. Brain Res 1619:104–114. https://doi.org/10.1016/j.brainres.2014.09.038
Deng WS, Ma K, Liang B, Liu XY, Xu HY, Zhang J, Shi HY, Sun HT, Chen XY, Zhang S (2020) Collagen scaffold combined with human umbilical cord-mesenchymal stem cells transplantation for acute complete spinal cord injury. Neural Regen Res 15(9):1686–1700. https://doi.org/10.4103/1673-5374.276340
Fitzharris M, Cripps RA, Lee BB (2014) Estimating the global incidence of traumatic spinal cord injury. Spinal Cord 52(2):117–122. https://doi.org/10.1038/sc.2013.135
Han IB, Thakor DK, Ropper AE, Yu D, Wang L, Kabatas S, Zeng X, Kim SW, Zafonte RD, Teng YD (2019) Physical impacts of PLGA scaffolding on hMSCs: recovery neurobiology insight for implant design to treat spinal cord injury. Exp Neurol 320:112980. https://doi.org/10.1016/j.expneurol.2019.112980
Hashimoto S, Nagoshi N, Shinozaki M, Nakanishi K, Suematsu Y, Shibata T, Kawai M, Kitagawa T, Ago K, Kamata Y, Yasutake K, Koya I, Ando Y, Minoda A, Shindo T, Shibata S, Matsumoto M, Nakamura M, Okano H (2023) Microenvironmental modulation in tandem with human stem cell transplantation enhances functional recovery after chronic complete spinal cord injury. Biomaterials 295:122002. https://doi.org/10.1016/j.biomaterials.2023.122002
Hashimoto S, Nagoshi N, Nakamura M, Okano H (2024) Regenerative medicine strategies for chronic complete spinal cord injury. Neural Regen Res 19(4):818–824. https://doi.org/10.4103/1673-5374.382230
Hassannejad Z, Sharif-Alhoseini M, Shakouri-Motlagh A, Vahedi F, Zadegan SA, Mokhatab M, Rezvan M, Saadat S, Shokraneh F, Rahimi-Movaghar V (2016) Potential variables affecting the quality of animal studies regarding pathophysiology of traumatic spinal cord injuries. Spinal Cord 54(8):579–583. https://doi.org/10.1038/sc.2015.215
Hatami M, Mehrjardi NZ, Kiani S, Hemmesi K, Azizi H, Shahverdi A, Baharvand H (2009) Human embryonic stem cell-derived neural precursor transplants in collagen scaffolds promote recovery in injured rat spinal cord. Cytotherapy 11(5):618–630. https://doi.org/10.1080/14653240903005802
Hejcl A, Sedý J, Kapcalová M, Toro DA, Amemori T, Lesný P, Likavcanová-Mašínová K, Krumbholcová E, Prádný M, Michálek J, Burian M, Hájek M, Jendelová P, Syková E (2010) HPMA-RGD hydrogels seeded with mesenchymal stem cells improve functional outcome in chronic spinal cord injury. Stem Cells Dev 19(10):1535–1546. https://doi.org/10.1089/scd.2009.0378
Hosseini SM, Sharafkhah A, Koohi-Hosseinabadi O, Semsar-Kazerooni M (2016) Transplantation of neural stem cells cultured in alginate scaffold for spinal cord injury in rats. Asian Spine J 10(4):611–618. https://doi.org/10.4184/asj.2016.10.4.611
Ide C, Nakai Y, Nakano N, Seo TB, Yamada Y, Endo K, Noda T, Saito F, Suzuki Y, Fukushima M, Nakatani T (2010) Bone marrow stromal cell transplantation for treatment of sub-acute spinal cord injury in the rat. Brain Res 1332:32–47. https://doi.org/10.1016/j.brainres.2010.03.043
Jiao G, Lou G, Mo Y, Pan Y, Zhang Z, Guo R, Li Z (2017) A combination of GDNF and hUCMSC transplantation loaded on SF/AGs composite scaffolds for spinal cord injury repair. Mater Sci Eng C 74:230–237. https://doi.org/10.1016/j.msec.2016.12.017
Karamouzian S, Nematollahi-Mahani SN, Nakhaee N, Eskandary H (2012) Clinical safety and primary efficacy of bone marrow mesenchymal cell transplantation in subacute spinal cord injured patients. Clin Neurol Neurosurg 114(7):935–939. https://doi.org/10.1016/j.clineuro.2012.02.003
Kim YC, Kim YH, Kim JW, Ha KY (2016) Transplantation of mesenchymal stem cells for acute spinal cord injury in rats: comparative study between intralesional injection and scaffold based transplantation. J Korean Med Sci 31(9):1373–1382. https://doi.org/10.3346/jkms.2016.31.9.1373
Kubinová S, Syková E (2010) Nanotechnologies in regenerative medicine. Minim Invasive Ther Allied Technol 19(3):144–156. https://doi.org/10.3109/13645706.2010.481398
Li L, Zhang Y, Mu J, Chen J, Zhang C, Cao H, Gao J (2020) Transplantation of human mesenchymal stem-cell-derived exosomes immobilized in an adhesive hydrogel for effective treatment of spinal cord injury. Nano Lett 20(6):4298–4305. https://doi.org/10.1021/acs.nanolett.0c00929
Libro R, Bramanti P, Mazzon E (2017) The combined strategy of mesenchymal stem cells and tissue-engineered scaffolds for spinal cord injury regeneration. Exp Ther Med 14(4):3355–3368. https://doi.org/10.3892/etm.2017.4939
Liu J, Chen J, Liu B, Yang C, Xie D, Zheng X, Xu S, Chen T, Wang L, Zhang Z, Bai X, Jin D (2013) Acellular spinal cord scaffold seeded with mesenchymal stem cells promotes long-distance axon regeneration and functional recovery in spinal cord injured rats. J Neurol Sci 325(1–2):127–136. https://doi.org/10.1016/j.jns.2012.11.022
Liu J, Chen Q, Zhang Z, Zheng Y, Sun X, Cao X, Gong A, Cui Y, He Q, Jiang P (2013) Fibrin scaffolds containing ectomesenchymal stem cells enhance behavioral and histological improvement in a rat model of spinal cord injury. Cells Tissues Organs 198(1):35–46. https://doi.org/10.1159/000351665
Liu Y, Ye H, Satkunendrarajah K, Yao GS, Bayon Y, Fehlings MG (2013) A self-assembling peptide reduces glial scarring, attenuates post-traumatic inflammation and promotes neurological recovery following spinal cord injury. Acta Biomater 9(9):8075–8088. https://doi.org/10.1016/j.actbio.2013.06.001
Liu C, Huang Y, Pang M, Yang Y, Li S, Liu L, Shu T, Zhou W, Wang X, Rong L, Liu B (2015) Tissue-engineered regeneration of completely transected spinal cord using induced neural stem cells and gelatin-electrospun poly (lactide-co-glycolide)/polyethylene glycol scaffolds. PLoS ONE 10(3):e0117709. https://doi.org/10.1371/journal.pone.0117709
Liu D, Li X, Xiao Z, Yin W, Zhao Y, Tan J, Chen B, Jiang X, Dai J (2019) Different functional bio-scaffolds share similar neurological mechanism to promote locomotor recovery of canines with complete spinal cord injury. Biomaterials 214:119230. https://doi.org/10.1016/j.biomaterials.2019.119230
Liu S, Xie YY, Wang B (2019) Role and prospects of regenerative biomaterials in the repair of spinal cord injury. Neural Regen Res 14(8):1352–1363. https://doi.org/10.4103/1673-5374.253512
Liu S, Yang H, Chen D, Xie Y, Tai C, Wang L, Wang P, Wang B (2022) Three-dimensional bioprinting sodium alginate/gelatin scaffold combined with neural stem cells and oligodendrocytes markedly promoting nerve regeneration after spinal cord injury. Regen Biomater 9:rbac038. https://doi.org/10.1093/rb/rbac038
Lv B, Zhang X, Yuan J, Chen Y, Ding H, Cao X, Huang A (2021) Biomaterial-supported MSC transplantation enhances cell–cell communication for spinal cord injury. Stem Cell Res Therapy 12(1):36. https://doi.org/10.1186/s13287-020-02090-y
Marchini A, Raspa A, Pugliese R, El Malek MA, Pastori V, Lecchi M, Vescovi AL, Gelain F (2019) Multifunctionalized hydrogels foster hNSC maturation in 3D cultures and neural regeneration in spinal cord injuries. Proc Natl Acad Sci USA 116(15):7483–7492. https://doi.org/10.1073/pnas.1818392116
Nori S, Khazaei M, Ahuja CS, Yokota K, Ahlfors JE, Liu Y, Wang J, Shibata S, Chio J, Hettiaratchi MH, Führmann T, Shoichet MS, Fehlings MG (2018) Human oligodendrogenic neural progenitor cells delivered with chondroitinase ABC facilitate functional repair of chronic spinal cord injury. Stem Cell Rep 11(6):1433–1448. https://doi.org/10.1016/j.stemcr.2018.10.017
Oh SK, Jeon SR (2016) Current concept of stem cell therapy for spinal cord injury: a review. Korean J Neurotrauma 12(2):40–46. https://doi.org/10.13004/kjnt.2016.12.2.40
Peng Z, Gao W, Yue B, Jiang J, Gu Y, Dai J, Chen L, Shi Q (2018) Promotion of neurological recovery in rat spinal cord injury by mesenchymal stem cells loaded on nerve-guided collagen scaffold through increasing alternatively activated macrophage polarization. J Tissue Eng Regen Med 12(3):e1725–e1736. https://doi.org/10.1002/term.2358
Piltti KM, Funes GM, Avakian SN, Salibian AA, Huang KI, Carta K, Kamei N, Flanagan LA, Monuki ES, Uchida N, Cummings BJ, Anderson AJ (2017) Increasing human neural stem cell transplantation dose alters oligodendroglial and neuronal differentiation after spinal cord injury. Stem Cell Rep 8(6):1534–1548. https://doi.org/10.1016/j.stemcr.2017.04.009
Raynald ShuB, Liu XB, Zhou JF, Huang H, Wang JY, Sun XD, Qin C, An YH (2019) Polypyrrole/polylactic acid nanofibrous Scaffold cotransplanted with bone marrow stromal cells promotes the functional recovery of spinal cord injury in rats. CNS Neurosci Therap 25(9):951–964. https://doi.org/10.1111/cns.13135
Rong Y, Liu W, Wang J, Fan J, Luo Y, Li L, Kong F, Chen J, Tang P, Cai W (2019) Neural stem cell-derived small extracellular vesicles attenuate apoptosis and neuroinflammation after traumatic spinal cord injury by activating autophagy. Cell Death Dis 10(5):340. https://doi.org/10.1038/s41419-019-1571-8
Ropper AE, Thakor DK, Han I, Yu D, Zeng X, Anderson JE, Aljuboori Z, Kim SW, Wang H, Sidman RL, Zafonte RD, Teng YD (2017) Defining recovery neurobiology of injured spinal cord by synthetic matrix-assisted hMSC implantation. Proc Natl Acad Sci USA 114(5):E820-e829. https://doi.org/10.1073/pnas.1616340114
Rouanet C, Reges D, Rocha E, Gagliardi V, Silva GS (2017) Traumatic spinal cord injury: current concepts and treatment update. Arq Neuropsiquiatr 75(6):387–393. https://doi.org/10.1590/0004-282x20170048
Sharif-Alhoseini M, Khormali M, Rezaei M, Safdarian M, Hajighadery A, Khalatbari MM, Safdarian M, Meknatkhah S, Rezvan M, Chalangari M, Derakhshan P, Rahimi-Movaghar V (2017) Animal models of spinal cord injury: a systematic review. Spinal cord 55(8):714–721. https://doi.org/10.1038/sc.2016.187
Silva NA, Sousa N, Reis RL, Salgado AJ (2014) From basics to clinical: a comprehensive review on spinal cord injury. Prog Neurobiol 114:25–57. https://doi.org/10.1016/j.pneurobio.2013.11.002
Silver J, Miller JH (2004) Regeneration beyond the glial scar. Nat Rev Neurosci 5(2):146–156. https://doi.org/10.1038/nrn1326
Subramanian A, Krishnan UM, Sethuraman S (2009) Development of biomaterial scaffold for nerve tissue engineering: biomaterial mediated neural regeneration. J Biomed Sci 16(1):108. https://doi.org/10.1186/1423-0127-16-108
Sugai K, Sumida M, Shofuda T, Yamaguchi R, Tamura T, Kohzuki T, Abe T, Shibata R, Kamata Y, Ito S, Okubo T, Tsuji O, Nori S, Nagoshi N, Yamanaka S, Kawamata S, Kanemura Y, Nakamura M, Okano H (2021) First-in-human clinical trial of transplantation of iPSC-derived NS/PCs in subacute complete spinal cord injury: study protocol. Regen Therapy 18:321–333. https://doi.org/10.1016/j.reth.2021.08.005
Tang F, Tang J, Zhao Y, Zhang J, Xiao Z, Chen B, Han G, Yin N, Jiang X, Zhao C, Cheng S, Wang Z, Chen Y, Chen Q, Song K, Zhang Z, Niu J, Wang L, Shi Q, Chen L, Yang H, Hou S, Zhang S, Dai J (2022) Long-term clinical observation of patients with acute and chronic complete spinal cord injury after transplantation of NeuroRegen scaffold. Sci China Life Sci 65(5):909–926. https://doi.org/10.1007/s11427-021-1985-5
Tavakol S, Aligholi H, Gorji A, Eshaghabadi A, Hoveizi E, Tavakol B, Rezayat SM, Ai J (2014) Thermogel nanofiber induces human endometrial-derived stromal cells to neural differentiation: in vitro and in vivo studies in rat. J Biomed Mater Res A 102(12):4590–4597. https://doi.org/10.1002/jbm.a.35117
Teng J, Takei Y, Harada A, Nakata T, Chen J, Hirokawa N (2001) Synergistic effects of MAP2 and MAP1B knockout in neuronal migration, dendritic outgrowth, and microtubule organization. J Cell Biol 155(1):65–76. https://doi.org/10.1083/jcb.200106025
Tetzlaff W, Okon EB, Karimi-Abdolrezaee S, Hill CE, Sparling JS, Plemel JR, Plunet WT, Tsai EC, Baptiste D, Smithson LJ, Kawaja MD, Fehlings MG, Kwon BK (2011) A systematic review of cellular transplantation therapies for spinal cord injury. J Neurotrauma 28(8):1611–1682. https://doi.org/10.1089/neu.2009.1177
Wang J, Zheng J, Zheng Q, Wu Y, Wu B, Huang S, Fang W, Guo X (2015) FGL-functionalized self-assembling nanofiber hydrogel as a scaffold for spinal cord-derived neural stem cells. Mater Sci Eng C 46:140–147. https://doi.org/10.1016/j.msec.2014.10.019
Wang TG, Xu J, Zhu AH, Lu H, Miao ZN, Zhao P, Hui GZ, Wu WJ (2016) Human amniotic epithelial cells combined with silk fibroin scaffold in the repair of spinal cord injury. Neural Regen Res 11(10):1670–1677. https://doi.org/10.4103/1673-5374.193249
Wang YH, Chen J, Zhou J, Nong F, Lv JH, Liu J (2017) Reduced inflammatory cell recruitment and tissue damage in spinal cord injury by acellular spinal cord scaffold seeded with mesenchymal stem cells. Exp Therap Med 13(1):203–207. https://doi.org/10.3892/etm.2016.3941
Wang J, Chu R, Ni N, Nan G (2020) The effect of Matrigel as scaffold material for neural stem cell transplantation for treating spinal cord injury. Sci Rep 10(1):2576. https://doi.org/10.1038/s41598-020-59148-3
Wang XH, Tang XC, Li X, Qin JZ, Zhong WT, Wu P, Zhang F, Shen YX, Dai TT (2021) Implantation of nanofibrous silk scaffolds seeded with bone marrow stromal cells promotes spinal cord regeneration (6686 words). Artif Cells Nanomed Biotechnol 49(1):699–708. https://doi.org/10.1080/21691401.2021.2013250
Xu X, Liang Z, Lin Y, Rao J, Lin F, Yang Z, Wang R, Chen C (2022) Comparing the efficacy and safety of cell transplantation for spinal cord injury: a systematic review and Bayesian network meta-analysis. Front Cell Neurosci 16:860131. https://doi.org/10.3389/fncel.2022.860131
Yang EZ, Zhang GW, Xu JG, Chen S, Wang H, Cao LL, Liang B, Lian XF (2017) Multichannel polymer scaffold seeded with activated Schwann cells and bone mesenchymal stem cells improves axonal regeneration and functional recovery after rat spinal cord injury. Acta Pharmacol Sin 38(5):623–637. https://doi.org/10.1038/aps.2017.11
Yang Y, Cao TT, Tian ZM, Gao H, Wen HQ, Pang M, He WJ, Wang NX, Chen YY, Wang Y, Li H, Lin JW, Kang Z, Li MM, Liu B, Rong LM (2020) Subarachnoid transplantation of human umbilical cord mesenchymal stem cell in rodent model with subacute incomplete spinal cord injury: preclinical safety and efficacy study. Exp Cell Res 395(2):112184. https://doi.org/10.1016/j.yexcr.2020.112184
You K, Chang H, Zhang F, Shen Y, Zhang Y, Cai F, Liu L, Liu X (2019) Cell-seeded porous silk fibroin scaffolds promotes axonal regeneration and myelination in spinal cord injury rats. Biochem Biophys Res Commun 514(1):273–279. https://doi.org/10.1016/j.bbrc.2019.04.137
Yousefifard M, Nasseri Maleki S, Askarian-Amiri S, Vaccaro AR, Chapman JR, Fehlings MG, Hosseini M, Rahimi-Movaghar V (2019) A combination of mesenchymal stem cells and scaffolds promotes motor functional recovery in spinal cord injury: a systematic review and meta-analysis. J Neurosurg Spine 32(2):269–284. https://doi.org/10.3171/2019.8.spine19201
Yousefifard M, Askarian-Amiri S, Nasseri Maleki S, Rafiei Alavi SN, Madani Neishaboori A, Haghani L, Vaccaro AR, Harrop JS, Lu Y, Rahimi-Movaghar V, Hosseini M (2022) Combined application of neural stem/progenitor cells and scaffolds on locomotion recovery following spinal cord injury in rodents: a systematic review and meta-analysis. Neurosurg Rev 45(6):3469–3488. https://doi.org/10.1007/s10143-022-01859-4
Zaminy A, Shokrgozar MA, Sadeghi Y, Noroozian M, Heidari MH, Piryaei A (2013) Mesenchymal stem cells as an alternative for Schwann cells in rat spinal cord injury. Iran Biomed J 17(3):113–122. https://doi.org/10.6091/ibj.1121.2013
Zarei-Kheirabadi M, Sadrosadat H, Mohammadshirazi A, Jaberi R, Sorouri F, Khayyatan F, Kiani S (2020) Human embryonic stem cell-derived neural stem cells encapsulated in hyaluronic acid promotes regeneration in a contusion spinal cord injured rat. Int J Biol Macromol 148:1118–1129. https://doi.org/10.1016/j.ijbiomac.2020.01.219
Zipser CM, Cragg JJ, Guest JD, Fehlings MG, Jutzeler CR, Anderson AJ, Curt A (2022) Cell-based and stem-cell-based treatments for spinal cord injury: evidence from clinical trials. Lancet Neurol 21(7):659–670. https://doi.org/10.1016/s1474-4422(21)00464-6
Zweckberger K, Ahuja CS, Liu Y, Wang J, Fehlings MG (2016) Self-assembling peptides optimize the post-traumatic milieu and synergistically enhance the effects of neural stem cell therapy after cervical spinal cord injury. Acta Biomater 42:77–89. https://doi.org/10.1016/j.actbio.2016.06.016
Acknowledgements
Not applicable.
Funding
The present study was supported by the National Natural Science Foundation of China (Grant No. 82260248).
Author information
Authors and Affiliations
Contributions
Zhihua Wang and Jun Li contributed to conceptualization, methodology, literature collecting, and writing and original manuscript draft. Meihua Li contributed to funding acquisition, literature evaluation, and writing, reviewing, and editing of the manuscript. Tianqi Xu and Zhiping Xie contributed to data collecting and statistical analysis and writing, reviewing, and editing of the manuscript. Boyu Guo contributed to literature evaluation.
Corresponding authors
Ethics declarations
Competing Interests
We declare no potential conflict of interest in the study.
Ethical Approval
The data on rats are obtained from the published literature after searching databases; no ethics approval is needed.
Consent to Participate
For the studies that had been published in the past, no consent to participate is necessary.
Human and Animal Ethics
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Z., Li, J., Xu, T. et al. The Efficacy of Different Material Scaffold-Guided Cell Transplantation in the Treatment of Spinal Cord Injury in Rats: A Systematic Review and Network Meta-analysis. Cell Mol Neurobiol 44, 43 (2024). https://doi.org/10.1007/s10571-024-01465-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10571-024-01465-6