Abstract
Objective
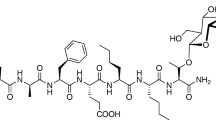
Pharmacological evaluation of the mu-opioid receptor (MOR) agonist properties of NKTR-181 in rodent models.
Methods
Graded noxious stimulus intensities were used in rats to establish the antinociceptive potency and efficacy of NKTR-181 relative to morphine, fentanyl, and oxycodone. Characteristics of MOR agonist actions, as measured by antinociceptive tolerance and cross-tolerance, as well as opioid-induced hyperalgesia (OIH) and naloxone-precipitated withdrawal in NKTR-181- and morphine-dependent in mice, were compared.
Results
NKTR-181 showed dose- and time-related antinociception with similar maximal effects to morphine in the rat and mouse hot-water tail-flick test. No sex or species differences were observed in NKTR-181 or morphine antinociception. Rats treated with NKTR-181 and morphine exhibited decreases in both potency and maximal efficacy as nociceptive stimulus intensity was increased from a water temperature of 50 °C to 54 °C. Evaluation of antinociception at a high stimulus intensity revealed that oxycodone and fentanyl exhibited greater efficacy than either NKTR-181 or morphine. The relative potency difference between NKTR-181 and morphine across all tail-flick studies was determined to be 7.6-fold (90% confidence interval, 2.6, 21.5). The peak antinociceptive effect of NKTR-181 was delayed compared to that of the other opioids and cumulative drug effects were not observed. Repeated treatment with escalating, approximately equi-analgesic doses of NKTR-181 or morphine, produced antinociceptive tolerance and cross-tolerance. Under these pharmacological conditions, OIH and naloxone-precipitated physical dependence were similar for NKTR-181 and morphine.
Conclusions
NKTR-181 had a slower onset, but similar efficacy, to morphine in the models studied supporting reduced abuse potential while maintaining analgesic effect in comparison with current opioids.






Similar content being viewed by others
References
Abreu ME, Bigelow GE, Fleisher L, Walsh SL (2001) Effect of intravenous injection speed on responses to cocaine and hydromorphone in humans. Psychopharmacology 154:76–84
Anantharamu T, Sharma S, Gupta AK, Dahiya N, Singh Brashier DB, Sharma AK (2015) Naloxegol: First oral peripherally acting mu opioid receptor antagonists for opioid-induced constipation. J Pharmacol Pharmacother 6:188–192
Angst MS, Clark JD (2006) Opioid-induced hyperalgesia: a qualitative systematic review. Anesthesiology 104:570–587
Bohnert ASB, Ilgen MA (2019) Understanding Links among opioid use, overdose, and suicide. N Engl J Med 380:71–79
Brat GA, Agniel D, Beam A et al (2018) Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: retrospective cohort study. BMJ 360:j5790
Bryant CD, Roberts KW, Byun JS, Fanselow MS, Evans CJ (2006) Morphine analgesic tolerance in 129P3/J and 129S6/SvEv mice. Pharmacol Biochem Behav 85:769–779
Chan HCS, McCarthy D, Li J, Palczewski K, Yuan S (2017) Designing safer analgesics via mu-opioid receptor pathways. Trends Pharmacol Sci 38:1016–1037
Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL (1994) Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods 53:55–63
Comer SD, Ashworth JB, Sullivan MA, Vosburg SK, Saccone PA, Foltin RW (2009) Relationship between rate of infusion and reinforcing strength of oxycodone in humans. J Opioid Manag 5:203–212
Compton WM, Jones CM, Baldwin GT (2016) Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med 374:154–163
Del Vecchio G, Spahn V, Stein C (2017) Novel Opioid analgesics and side effects. ACS Chem Neurosci 8:1638–1640
Drewes AM, Jensen RD, Nielsen LM et al (2013) Differences between opioids: pharmacological, experimental, clinical and economical perspectives. Br J Clin Pharmacol 75:60–78
Dumas EO, Pollack GM (2008) Opioid tolerance development: a pharmacokinetic/pharmacodynamic perspective. AAPS J 10:537–551
Farre M, Cami J (1991) Pharmacokinetic considerations in abuse liability evaluation. Br J Addict 86:1601–1606
Fields HL, Margolis EB (2015) Understanding opioid reward. Trends Neurosci 38:217–225
Grosser T, Woolf CJ, FitzGerald GA (2017) Time for nonaddictive relief of pain. Science 355:1026–1027
Gudin J, Rauck R, Argoff C et al (2019) Long-term safety and tolerability of NKTR-181 in patients with moderate to severe chronic low back pain or chronic noncancer pain: a phase 3 multicenter, open-label, 52-week study (SUMMIT-08 LTS). Pain Med. https://doi.org/10.1093/pm/pnz169
Heimer R, Hawk K, Vermund SH (2018) Prevalent misconceptions about opioid use disorders in the United States produce failed policy and public health responses. Clin Infect Dis 69:546–551
Hooten WM, Lamer TJ, Twyner C (2015) Opioid-induced hyperalgesia in community-dwelling adults with chronic pain. Pain 156:1145–1152
Kanof PD, Handelsman L, Aronson MJ, Ness R, Cochrane KJ, Rubinstein KJ (1992) Clinical characteristics of naloxone-precipitated withdrawal in human opioid-dependent subjects. J Pharmacol Exp Ther 260:355–363
Kest B, Palmese CA, Hopkins E, Adler M, Juni A, Mogil JS (2002) Naloxone-precipitated withdrawal jumping in 11 inbred mouse strains: evidence for common genetic mechanisms in acute and chronic morphine physical dependence. Neuroscience 115:463–469
King TE, Joynes RL, Grau JW (1997) Tail-flick test: II. The role of supraspinal systems and avoidance learning. Behav Neurosci 111:754–767
Kousik SM, Napier TC, Carvey PM (2012) The effects of psychostimulant drugs on blood brain barrier function and neuroinflammation. Front Pharmacol 3:121
Leppert W, Woron J (2016) The role of naloxegol in the management of opioid-induced bowel dysfunction. Ther Adv Gastroenterol 9:736–746
Markman J, Gudin J, Rauck R et al (2019) Summit-07: A randomized trial of NKTR-181, a new molecular entity, full mu-opioid receptor agonist for chronic low-back pain. Pain 160:1374–1382
Marsch LA, Bickel WK, Badger GJ et al (2001) Effects of infusion rate of intravenously administered morphine on physiological, psychomotor, and self-reported measures in humans. J Pharmacol Exp Ther 299:1056–1065
Miyazaki T, Choi IY, Rubas W et al (2017) NKTR-181: a novel mu-opioid analgesic with inherently low abuse potential. J Pharmacol Exp Ther 363:104–113
Nath C, Gupta MB, Patnaik GK, Dhawan KN (1994) Morphine-induced straub tail response: mediated by central mu2-opioid receptor. Eur J Pharmacol 263:203–205
Nemmani KV, Grisel JE, Stowe JR, Smith-Carliss R, Mogil JS (2004) Modulation of morphine analgesia by site-specific N-methyl-D-aspartate receptor antagonists: dependence on sex, site of antagonism, morphine dose, and time. Pain 109:274–283
Ossipov MH, Lai J, King T et al (2004) Antinociceptive and nociceptive actions of opioids. J Neurobiol 61:126–148
Ossipov MH, Dussor GO, Porreca F (2010) Central modulation of pain. J Clin Invest 120:3779–3787
Porreca F, Ossipov MH (2009) Nausea and vomiting side effects with opioid analgesics during treatment of chronic pain: mechanisms, implications, and management options. Pain Med 10:654–662
Roeckel LA, Le Coz GM, Gaveriaux-Ruff C, Simonin F (2016) Opioid-induced hyperalgesia: cellular and molecular mechanisms. Neuroscience 338:160–182
Rosen SF, Ham B, Haichin M et al (2019) Increased pain sensitivity and decreased opioid analgesia in T-cell-deficient mice and implications for sex differences. Pain 160:358–366
Rutkow L, Vernick JS (2017) Emergency Legal authority and the opioid crisis. N Engl J Med 377:2512–2514
Schaefer CP, Tome ME, Davis TP (2017) The opioid epidemic: a central role for the blood brain barrier in opioid analgesia and abuse. Fluids Barriers CNS 14:32
Shah A, Hayes CJ, Martin BC (2017) Factors Influencing long-term opioid use among opioid naive patients: an examination of initial prescription characteristics and pain etiologies. J Pain 18:1374–1383
Skolnick P, Volkow ND (2016) Re-energizing the Development of pain therapeutics in light of the opioid epidemic. Neuron 92:294–297
Stein C (2016) Opioid receptors. Annu Rev Med 67:433–451
Tompkins DA, Campbell CM (2011) Opioid-induced hyperalgesia: clinically relevant or extraneous research phenomenon? Curr Pain Headache Rep 15:129–136
Treillet E, Laurent S, Hadjiat Y (2018) Practical management of opioid rotation and equianalgesia. J Pain Res 11:2587–2601
US Food and Drug Administration (2015) Guidance for industry: abuse-deterrent opioids–evaluation and labeling. US Department of Health and Human Services website. https://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm334743.pdf. Accessed: 2019
Vander Weele CM, Porter-Stransky KA, Mabrouk OS et al (2014) Rapid dopamine transmission within the nucleus accumbens: dramatic difference between morphine and oxycodone delivery. Eur J Neurosci 40:3041–3054
Walker G (2018) The opioid crisis: a 21st century pain. Drugs Today (Barc) 54:283–286
Webster LR, Bath B, Medve RA, Marmon T, Stoddard GJ (2012) Randomized, double-blind, placebo-controlled study of the abuse potential of different formulations of oral oxycodone. Pain Med 13:790–801
Webster L, Henningfield J, Buchhalter AR et al (2018) Human abuse potential of the new opioid analgesic molecule NKTR-181 compared with oxycodone. Pain Med 19:307–318
Zollner C, Stein C (2007) Opioids. Handb Exp Pharmacol 177:31–63
Acknowledgements
Phillips Gilmore Oncology Communications provided professional assistance with initial manuscript preparation, which was funded by Nektar Therapeutics.
Funding
L.V., M.Y., Y.L., T.M., and J.Z. are employees of Nektar Therapeutics. W.K.S. is a consultant for Nektar Therapeutics. F.P. received laboratory support for this study from Nektar Therapeutics.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kopruszinski, C.M., Swiokla, J., Lee, Y.S. et al. Preclinical Assessment of the Analgesic Pharmacology of NKTR-181 in Rodents. Cell Mol Neurobiol 41, 949–960 (2021). https://doi.org/10.1007/s10571-020-00816-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10571-020-00816-3