Abstract
Admission of a preterm or sick full-term infant to the neonatal intensive care unit (NICU) is a stressful experience for parents. Indeed, the ‘NICU experience’ may constitute a traumatic event for parents, distinct from other birth-related trauma, leading to significant and ongoing posttraumatic stress disorder (PTSD) symptoms. However, the rates at which this outcome occurs are not well understood. This review aimed to identify the prevalence of PTSD in mothers and fathers of high-risk infants admitted to the NICU, specifically focusing on the NICU experience as the index trauma. The PRISMA-P: Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols were used to conduct this review. We searched PsycINFO, PubMed, Scopus, EMBASE, Web of Science, ProQuest Dissertations and Theses databases, and reference lists of included articles (1980–2021). Two independent reviewers screened titles and abstracts and conducted the full-text screening assessment. Of the 707 records identified, seven studies met the inclusion criteria. In this systematic review, PTSD symptomatology was assessed by self-report measures rather than a clinical interview. We identified significant variations in the methodologies and quality between studies, with a wide variation of reported prevalence rates of PTSD of 4.5–30% in mothers and 0–33% in fathers. Overall, the findings indicate that up to one-third of parents experience PTSD symptomatology related to the NICU experience. These results emphasize the importance of universal routine antenatal and postnatal screening for symptoms of PTSD to identify parents at risk of distress during the NICU experience and after discharge.
Trial registration: The study protocol was registered with Prospero registration number CRD42020154548 on 28 April 2020.


Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org.
References
Aftyka, A., Rybojad, B., Rozalska-Walaszek, I., Rzoñca, P., & Humeniuk, E. (2014). Post-traumatic stress disorder in parents of children hospitalized in the neonatal intensive care unit (NICU): Medical and demographic risk factors. Psychiatria Danubina, 26(4), 347–352. https://www.scopus.com/inward/record.uri?eid=2-s2.0-84909647121&partnerID=40&md5=9cd5bb49e85a6ab997c5590d0f60f048
Alio, A. P., Lewis, C. A., Scarborough, K., Harris, K., & Fiscella, K. (2013). A community perspective on the role of fathers during pregnancy: A qualitative study. BMC Pregnancy and Childbirth, 13, 60. https://doi.org/10.1186/1471-2393-13-60
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425596
Andersen, L. B., Melvaer, L. B., Videbech, P., Lamont, R. F., & Joergensen, J. S. (2012). Risk factors for developing post-traumatic stress disorder following childbirth: A systematic review. Acta Obstetricia et Gynecologica Scandinavica, 91(11), 1261–1272. https://doi.org/10.1111/j.1600-0412.2012.01476.x
Ayers, S., Eagle, A., & Waring, H. (2006). The effects of childbirth-related post-traumatic stress disorder on women and their relationships: A qualitative study. Psychology, Health and Medicine, 11(4), 389–398. https://doi.org/10.1080/13548500600708409
Bailham, D., & Joseph, S. (2003). Post-traumatic stress following childbirth: A review of the emerging literature and directions for research and practice. Psychology, Health and Medicine, 8(2), 159–168. https://doi.org/10.1080/1354850031000087537
Barr, P. (2010). Acute traumatic stress in neonatal intensive care unit parents: Relation to existential emotion-based personality predispositions. Journal of Loss and Trauma, 15(2), 106–122. https://doi.org/10.1080/15325020903373128
Barr, P. (2012). A dyadic analysis of negative emotion personality predisposition effects with psychological distress in neonatal intensive care unit parents. Psychological Trauma: Theory, Research, Practice, and Policy, 4(4), 347–355. https://doi.org/10.1037/a0024228
Barthel, D., Göbel, A., Barkmann, C., Helle, N., & Bindt, C. (2020). Does birth-related trauma last? Prevalence and risk factors for posttraumatic stress in mothers and fathers of VLBW preterm and term born children 5 years after birth. Frontiers in Psychiatry. https://doi.org/10.3389/fpsyt.2020.575429
Beck, C. T. (2004). Post-traumatic stress disorder due to childbirth: The aftermath. Nursing Research, 53(4), 216–224. https://doi.org/10.1097/00006199-200407000-00004
Beck, C. T., & Woynar, J. (2017). Posttraumatic stress in mothers while their preterm infants are in the newborn intensive care unit: A mixed research synthesis. Advances in Nursing Science, 40(4), 337–355. https://doi.org/10.1097/ans.0000000000000176
Benoit, D. (2004). Infant–parent attachment: Definition, types, antecedents, measurement and outcome. Paediatric Child Health, 9(8), 541–545. https://doi.org/10.1093/pch/9.8.541
Bernardo, J., Rent, S., Arias-Shah, A., Hoge, M. K., & Shaw, R. J. (2021). Parental stress and mental health symptoms in the NICU: Recognition and interventions. NeoReviews, 22(8), e496–e505. https://doi.org/10.1542/neo.22-8-e496
Birmingham, R. S., Bub, K. L., & Vaughn, B. E. (2017). Parenting in infancy and self-regulation in preschool: An investigation of the role of attachment history. Attachment and Human Development, 19(2), 107–129. https://doi.org/10.1080/14616734.2016.1259335
Bliese, P. D., Wright, K. M., Adler, A. B., Cabrera, O., Castro, C. A., & Hoge, C. W. (2008). Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. Journal of Consulting and Clinical Psychology, 76(2), 272–281. https://doi.org/10.1037/0022-006x.76.2.272
Bloyd, C., Murthy, S., Song, C., Franck, L. S., & Mangurian, C. (2022). National cross-sectional study of mental health screening practices for primary caregivers of NICU infants. Children, 9(6), 793. https://doi.org/10.3390/children9060793
Bramer, W. M., Rethlefsen, M. L., Mast, F., & Kleijnen, J. (2018). Evaluation of a new method for librarian-mediated literature searches for systematic reviews. Research Synthesis Methods, 9(4), 510–520. https://doi.org/10.1002/jrsm.1279
Brand, S. R., & Brennan, P. A. (2009). Impact of antenatal and postpartum maternal mental illness: How are the children? Clinical Obstetrics and Gynecology, 52(3), 441–455. https://doi.org/10.1097/GRF.0b013e3181b52930
Chang, H. P., Chen, J. Y., Huang, Y. H., Yeh, C. J., Huang, J. Y., Su, P. H., & Chen, V. C. (2016). Factors associated with post-traumatic symptoms in mothers of preterm infants. Archives of Psychiatric Nursing, 30(1), 96–101. https://doi.org/10.1016/j.apnu.2015.08.019
Christie, H., Hamilton-Giachritsis, C., Alves-Costa, F., Tomlinson, M., & Halligan, S. L. (2019). The impact of parental posttraumatic stress disorder on parenting: A systematic review. European Journal of Psychotraumatology, 10(1), 1550345. https://doi.org/10.1080/20008198.2018.1550345
Clottey, M., & Dillard, D. M. (2013). Post-traumatic stress disorder and neonatal intensive care. International Journal of Childbirth Education, 28(3), 23–29. https://www.proquest.com/scholarly-journals/post-traumatic-stress-disorder-neonatal-intensive/docview/1412227235/se-2?accountid=14723
Cook, N., Ayers, S., & Horsch, A. (2018). Maternal posttraumatic stress disorder during the perinatal period and child outcomes: A systematic review. Journal of Affective Disorders, 225, 18–31. https://doi.org/10.1016/j.jad.2017.07.045
DeMier, R. L., Hynan, M. T., Harris, H. B., & Manniello, R. L. (1996). Perinatal stressors as predictors of symptoms of posttraumatic stress in mothers of infants at high risk. Journal of Perinatology, 16(4), 276–280. https://pubmed.ncbi.nlm.nih.gov/8866297/
Feeley, N., Genest, C., Niela-Vilén, H., Charbonneau, L., & Axelin, A. (2016). Parents and nurses balancing parent–infant closeness and separation: A qualitative study of NICU nurses’ perceptions. BMC Pediatrics, 16(1), 1–13. https://doi.org/10.1186/s12887-016-0663-1
Forcada-Guex, M., Borghini, A., Pierrehumbert, B., Ansermet, F., & Muller-Nix, C. (2011). Prematurity, maternal posttraumatic stress and consequences on the mother–infant relationship. Early Human Development, 87(1), 21–26. https://doi.org/10.1016/j.earlhumdev.2010.09.006
Forcada-Guex, M., Pierrehumbert, B., Borghini, A., Moessinger, A., & Muller-Nix, C. (2006). Early dyadic patterns of mother–infant interactions and outcomes of prematurity at 18 months. Pediatrics, 118(1), e107-114. https://doi.org/10.1542/peds.2005-1145
Fowler, C., Green, J., Elliott, D., Petty, J., & Whiting, L. (2019). The forgotten mothers of extremely preterm babies: A qualitative study. Journal of Clinical Nursing, 28(11–12), 2124–2134. https://doi.org/10.1111/jocn.14820
Galea, M., Park, T., & Hegadoren, K. M. (2021). Improving mental health outcomes of parents of infants treated in neonatal intensive care units: A scoping review. Journal of Neonatal Nursing. https://doi.org/10.1016/j.jogn.2017.02.005
Galpin, J. (2013). Posttraumatic stress and growth symptoms in parents of premature infants: The role of rumination type and social support (10058369). https://ueaeprints.uea.ac.uk/id/eprint/49596/
Garthus-Niegel, S., Ayers, S., Martini, J., von Soest, T., & Eberhard-Gran, M. (2017). The impact of postpartum post-traumatic stress disorder symptoms on child development: A population-based, 2-year follow-up study. Psychological Medicine, 47(1), 161–170. https://doi.org/10.1017/s003329171600235x
Ghorbani, M., Dolatian, M., Shams, J., & Alavi-Majd, H. (2014). Anxiety, post-traumatic stress disorder and social supports among parents of premature and full-term infants. Iranian Red Crescent Medical Journal, 16(3), e13461. https://doi.org/10.5812/ircmj.13461
Gondwe, K. W., & Holditch-Davis, D. (2015). Posttraumatic stress symptoms in mothers of preterm infants. International Journal of Africa Nursing Sciences, 3, 8–17. https://doi.org/10.1016/j.ijans.2015.05.002
Goulet, C., Bell, L., St-Cyr, D., Paul, D., & Lang, A. (1998). A concept analysis of parent–infant attachment. Journal of Advanced Nursing, 28(5), 1071–1081. https://doi.org/10.1046/j.1365-2648.1998.00815.x
Goutaudier, N., Lopez, A., Séjourné, N., Denis, A., & Chabrol, H. (2011). Premature birth: Subjective and psychological experiences in the first weeks following childbirth, a mixed-methods study. Journal of Reproductive and Infant Psychology, 29(4), 364–373. https://doi.org/10.1080/02646838.2011.623227
Grosik, C., Snyder, D., Cleary, G. M., Breckenridge, D. M., & Tidwell, B. (2013). Identification of internal and external stressors in parents of newborns in intensive care. The Permanente Journal, 17(3), 36–41. https://doi.org/10.7812/TPP/12-105
Grunberg, V. A., Geller, P. A., Bonacquisti, A., & Patterson, C. A. (2019). NICU infant health severity and family outcomes: A systematic review of assessments and findings in psychosocial research. Journal of Perinatology, 39(2), 156–172. https://doi.org/10.1038/s41372-018-0282-9
Hall, S. L., & Hynan, M. T. (2015). Interdisciplinary recommendations for the psychosocial support of NICU parents. Nature Publishing Group, NPG. https://doi.org/10.1038/jp.2015.147
Heyne, C.-S., Kazmierczak, M., Souday, R., Horesh, D., Lambregtse-van den Berg, M., Weigl, T., Horsch, A., Oosterman, M., Dikmen-Yildiz, P., & Garthus-Niegel, S. (2022). Prevalence and risk factors of birth-related posttraumatic stress among parents: A comparative systematic review and meta-analysis. Clinical Psychology Review, 94, 102157. https://doi.org/10.1016/j.cpr.2022.102157
Hodek, J.-M., von der Schulenburg, J. M., & Mittendorf, T. (2011). Measuring economic consequences of preterm birth—Methodological recommendations for the evaluation of personal burden on children and their caregivers. Health Economics Review, 1(1), 6. https://doi.org/10.1186/2191-1991-1-6
Horesh, D., Garthus-Niegel, S., & Horsch, A. (2021). Childbirth-related PTSD: Is it a unique post-traumatic disorder? Journal of Reproductive and Infant Psychology, 39(3), 221–224. https://doi.org/10.1080/02646838.2021.1930739
Hoy, D., Brooks, P., Woolf, A., Blyth, F., March, L., Bain, C., Baker, P., Smith, E., & Buchbinder, R. (2012). Assessing risk of bias in prevalence studies: Modification of an existing tool and evidence of interrater agreement. Journal of Clinical Epidemiology, 65(9), 934–939. https://doi.org/10.1016/j.jclinepi.2011.11.014
Hynan, M. T., & Hall, S. L. (2015). Psychosocial program standards for NICU parents. Journal of Perinatology, 35(1), S1–S4. https://doi.org/10.1038/jp.2015.141
Hynan, M. T., Mounts, K. O., & Vanderbilt, D. L. (2013). Screening parents of high-risk infants for emotional distress: Rationale and recommendations. Journal of Perinatology, 33(10), 748–753. https://doi.org/10.1038/jp.2013.72
Hynan, M. T., Steinberg, Z., Baker, L., Cicco, R., Geller, P. A., Lassen, S., Milford, C., Mounts, K. O., Patterson, C., Saxton, S., Segre, L., & Stuebe, A. (2015). Recommendations for mental health professionals in the NICU. Journal of Perinatology, 35(1), S14–S18. https://doi.org/10.1038/jp.2015.144
Kersting, A., Dorsch, M., Wesselmann, U., Lüdorff, K., Witthaut, J., Ohrmann, P., Hörnig-Franz, I., Klockenbusch, W., Harms, E., & Arolt, V. (2004). Maternal posttraumatic stress response after the birth of a very low-birth-weight infant. Journal of Psychosomatic Research, 57(5), 473–476. https://doi.org/10.1016/j.jpsychores.2004.03.011
Kim, W., Lee, E., Kim, K., Namkoong, K., Park, E., & Rha, D. (2015). Progress of PTSD symptoms following birth: A prospective study in mothers of high-risk infants. Journal of Perinatology, 35(8), 575–579. https://doi.org/10.1038/jp.2015.9
Lean, R. E., Rogers, C. E., Paul, R. A., & Gerstein, E. D. (2018). NICU hospitalization: Long-term implications on parenting and child behaviors. Current Treatment Options in Pediatrics, 4(1), 49–69. https://doi.org/10.1007/s40746-018-0112-5
Lefkowitz, D. S., Baxt, C., & Evans, J. R. (2010). Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the neonatal intensive care unit (NICU). Journal of Clinical Psychology in Medical Settings, 17(3), 230–237. https://doi.org/10.1007/s10880-010-9202-7
Leinweber, J., Fontein-Kuipers, Y., Thomson, G., Karlsdottir, S. I., Nilsson, C., Ekström-Bergström, A., Olza, I., Hadjigeorgiou, E., & Stramrood, C. (2022). Developing a woman-centered, inclusive definition of traumatic childbirth experiences: A discussion paper. Birth. https://doi.org/10.1111/birt.12634
Lotterman, J. H., Lorenz, J. M., & Bonanno, G. A. (2019). You can’t take your baby home yet: A longitudinal study of psychological symptoms in mothers of infants hospitalized in the NICU. Journal of Clinical Psychology in Medical Settings, 26(1), 116–122. https://doi.org/10.1007/s10880-018-9570-y
Malin, K. J., Johnson, T. S., Brown, R. L., Leuthner, J., Malnory, M., White-Traut, R., Rholl, E., & Lagatta, J. (2022). Uncertainty and perinatal post-traumatic stress disorder in the Neonatal Intensive Care Unit. Research in Nursing and Health. https://doi.org/10.1002/nur.22261
Malouf, R., Harrison, S., Burton, H. A. L., Gale, C., Stein, A., Franck, L. S., & Alderdice, F. (2022). Prevalence of anxiety and post-traumatic stress (PTS) among the parents of babies admitted to neonatal units: A systematic review and meta-analysis. EClinicalMedicine, 43, 101233. https://doi.org/10.1016/j.eclinm.2021.101233
McKenzie-McHarg, K., Ayers, S., Ford, E., Horsch, A., Jomeen, J., Sawyer, A., Stramrood, C., Thomson, G., & Slade, P. (2015). Post-traumatic stress disorder following childbirth: An update of current issues and recommendations for future research. Journal of Reproductive and Infant Psychology, 33(3), 219–237. https://doi.org/10.1080/02646838.2015.1031646
Moreyra, A., Dowtin, L. L., Ocampo, M., Perez, E., Borkovi, T. C., Wharton, E., Simon, S., Armer, E. G., & Shaw, R. J. (2021). Implementing a standardized screening protocol for parental depression, anxiety, and PTSD symptoms in the Neonatal Intensive Care Unit. Early Human Development, 154, 105279. https://doi.org/10.1016/j.earlhumdev.2020.105279
Obeidat, H. M., Bond, E. A., & Callister, L. C. (2009). The parental experience of having an infant in the newborn intensive care unit. Journal of Perinatal Education, 18(3), 23–29. https://doi.org/10.1624/105812409x461199
Olff, M. (2017). Sex and gender differences in post-traumatic stress disorder: an update. European Journal of Psychotraumatology, 8(sup4), 1351204. https://doi.org/10.1080/20008198.2017.1351204
Ouyang, J. X., Mayer, J. L. W., Battle, C. L., Chambers, J. E., & Inanc Salih, Z. N. (2020). Historical perspectives: Unsilencing suffering: Promoting maternal mental health in neonatal intensive care units. NeoReviews, 21(11), e708–e715. https://doi.org/10.1542/neo.21-11-e708
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. British Medical Journal, 372, n71. https://doi.org/10.1136/bmj.n71
Priebe, K., Kleindienst, N., Schropp, A., Dyer, A., Krüger-Gottschalk, A., Schmahl, C., Steil, R., & Bohus, M. (2018). Defining the index trauma in post-traumatic stress disorder patients with multiple trauma exposure: Impact on severity scores and treatment effects of using worst single incident versus multiple traumatic events. European Journal of Psychotraumatology. https://doi.org/10.1080/20008198.2018.1486124
Rizvydeen, S., & Feltman, D. M. (2022). What happened to dad? The complexity of paternal trauma and ethical care. The American Journal of Bioethics, 22(5), 74–76. https://doi.org/10.1080/15265161.2022.2055213
Roque, A. T. F., Lasiuk, G. C., Radünz, V., & Hegadoren, K. (2017). Scoping review of the mental health of parents of infants in the NICU. Journal of Obstetrics and Gynecology and Neonatal Nursing, 46(4), 576–587. https://doi.org/10.1016/j.jogn.2017.02.005
Salomè, S., Mansi, G., Lambiase, C. V., Barone, M., Piro, V., Pesce, M., Sarnelli, G., Raimondi, F., & Capasso, L. (2022). Impact of psychological distress and psychophysical wellbeing on posttraumatic symptoms in parents of preterm infants after NICU discharge. Italian Journal of Pediatrics, 48(1), 13. https://doi.org/10.1186/s13052-022-01202-z
Sanders, M., & Hall, S. (2018). Trauma-informed care in the newborn intensive care unit: Promoting safety, security and connectedness. Journal of Perinatology, 38(1), 3–10. https://doi.org/10.1038/jp.2017.124
Schecter, R., Pham, T., Hua, A., Spinazzola, R., Sonnenklar, J., Li, D., Papaioannou, H., & Milanaik, R. (2020). Prevalence and longevity of PTSD symptoms among parents of NICU infants analyzed across gestational age categories. Clinical Pediatrics, 59(2), 163–169. https://doi.org/10.1177/0009922819892046
Sharp, M., Huber, N., Ward, L. G., & Dolbier, C. (2021). NICU-specific stress following traumatic childbirth and its relationship with posttraumatic stress. Journal of Perinatal and Neonatal Nursing, 35(1), 57–67. https://doi.org/10.1097/jpn.0000000000000543
Shaw, R. J., Bernard, R. S., De Blois, T., Ikuta, L. M., Ginzburg, K., & Koopman, C. (2009). The relationship between acute stress disorder and posttraumatic stress disorder in the neonatal intensive care unit. Psychosomatics, 50(2), 131–137. https://doi.org/10.1176/appi.psy.50.2.131
Shaw, R. J., Bernard, R. S., Storfer-Isser, A., Rhine, W., & Horwitz, S. M. (2013). Parental coping in the neonatal intensive care unit. Journal of Clinical Psychology in Medical Settings, 20(2), 135–142. https://doi.org/10.1007/s10880-012-9328-x
Shaw, R. J., Deblois, T., Ikuta, L., Ginzburg, K., Fleisher, B., & Koopman, C. (2006). Acute stress disorder among parents of infants in the neonatal intensive care nursery. Psychosomatics, 47(3), 206–212. https://doi.org/10.1176/appi.psy.47.3.206
Skene, C., Gerrish, K., Price, F., Pilling, E., Bayliss, P., & Gillespie, S. (2019). Developing family-centred care in a neonatal intensive care unit: An action research study. Intensive and Critical Care Nursing, 50, 54–62. https://doi.org/10.1016/j.iccn.2018.05.006
Soni, R., & Tscherning, C. (2021). Family-centred and developmental care on the neonatal unit. Paediatrics and Child Health, 31(1), 18–23. https://doi.org/10.1016/j.paed.2020.10.003
Stacey, S., Osborn, M., & Salkovskis, P. (2015). Life is a rollercoaster…What helps parents cope with the Neonatal Intensive Care Unit (NICU)? Journal of Neonatal Nursing, 21(4), 136–141. https://doi.org/10.1016/j.jnn.2015.04.006
Vanderbilt, D., Bushley, T., Young, R., & Frank, D. A. (2009). Acute posttraumatic stress symptoms among urban mothers with newborns in the neonatal intensive care unit: A preliminary study. Journal of Developmental and Behavioral Pediatrics, 30(1), 50–56. https://doi.org/10.1097/DBP.0b013e318196b0de
Waddington, C., Van Veenendaal, N. R., O’Brien, K., Patel, N., & International Steering Committee for Family Integrated Care. (2021). Family integrated care: Supporting parents as primary caregivers in the neonatal intensive care unit. Pediatric Investigation, 5(2), 148–154. https://doi.org/10.1002/ped4.12277
Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5). https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp
Wilcoxon, L. A., Meiser-Stedman, R., & Burgess, A. (2021). Post-traumatic stress disorder in parents following their child’s single-event trauma: A meta-analysis of prevalence rates and risk factor correlates. Clinical Child and Family Psychology Review, 24(4), 725–743. https://doi.org/10.1007/s10567-021-00367-z
World Health Organization. (2019a). ICD-11: International classification of diseases. WHO. https://icd.who.int/
World Health Organization. (2019b). International statistical classification of diseases and related health problems (11th ed.). WHO. https://icd.who.int/
World Health Organisation. (2022). Preterm birth. WHO. https://www.who.int/news-room/fact-sheets/detail/preterm-birth
Yee, W., & Ross, S. (2006). Communicating with parents of high-risk infants in neonatal intensive care. Paediatrics and Child Health, 11(5), 291–294. https://doi.org/10.1016/j.jad.2016.10.009
Yildiz, P. D., Ayers, S., & Phillips, L. (2017). The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. Journal of Affective Disorders, 208, 634–645. https://doi.org/10.1016/j.jad.2016.10.009
Funding
This review was supported by a University of Queensland Research Scholarship, Royal Brisbane and Women's Hospital Foundation Grant and Postgraduate Scholarship and contributes to a Doctor of Philosophy Program.
Author information
Authors and Affiliations
Contributions
We would like to thank academic librarian Mr. Lars Eriksson from the University of Queensland for developing this review's search strategy.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical Approval
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: Search Terms
(Information Sources PsycINFO, 1980 to November to 26 November 2021) | ||
|---|---|---|
Search number | Query | Results |
4 | ((("Stress Disorders, Post-Traumatic"[Mesh] OR "PTSD"[tiab] OR "post-traumatic stress disorders"[tiab] OR "post-traumatic stress disorder"[tiab] OR "posttraumatic stress disorders"[tiab] OR "posttraumatic stress disorder"[tiab] OR PTSS[tiab] OR "post-traumatic stress symptomatology"[tiab])) AND ((('Intensive Care'[tiab] OR 'neonatal intensive care’[tiab] OR 'Intensive Care Units[tiab] OR 'nicu'[tiab])) AND (('Intensive Care'[tiab] OR 'neonatal intensive care’[tiab] OR 'Intensive Care Units[tiab]OR 'nicu'[tiab])))) AND (('infant'[tiab] OR ‘newborn’[tiab] OR ‘neonate’[tiab] OR ‘prematurity’[tiab] OR ‘low birth weight’[tiab] OR ‘Hospitalised infant’[tiab])) | 67 |
3 | ('infant'[tiab] OR ‘newborn’[tiab] OR ‘neonate’[tiab]OR ‘prematurity’[tiab] OR ‘low birth weight’[tiab] OR ‘Hospitalised infant’[tiab]) | 406,709 |
2 | (('Intensive Care'[tiab] OR 'neonatal intensive care’[tiab] OR 'Intensive Care Units[tiab]OR 'nicu'[tiab])) AND (('Intensive Care'[tiab] OR 'neonatal intensive care’[tiab] OR 'Intensive Care Units[tiab]OR 'nicu'[tiab])) | 171,848 |
1 | ("Stress Disorders, Post-Traumatic"[Mesh] OR "PTSD"[tiab] OR "post-traumatic stress disorders"[tiab] OR "post-traumatic stress disorder"[tiab] OR "posttraumatic stress disorders"[tiab] OR "posttraumatic stress disorder"[tiab] OR PTSS[tiab] OR "post-traumatic stress symptomatology"[tiab]) | 51,250 |
Appendix 2: Summary of Characteristics of Studies
First Author/Year/Country/Design | Sample (n) size | Parents age (mean) | Gestational age weeks (mean) | Infant’s weight g (mean) | Outcome measures | Clinical cut-off | PTSD event specified | Timepoints (postpartum) | Prevalence of probable PTSD (n, %) | Findings |
|---|---|---|---|---|---|---|---|---|---|---|
Barr, 2012, Australia; Prospective cohort study | Couples (n = 67) | Fathers 33.5 Mothers 31.0 | > 34 | NR | PCL-S DSM-IV (Self-report) | ≥ 44 | NICU Experience re-experiencing (“Repeated, disturbing memories, thoughts, or images of your NICU experience?”); avoidance (“Avoid thinking about or talking about your NICU experience or avoid having feelings related to it?”); and hyperarousal (“Being ‘super alert’ or watchful on guard?”) | 13 months | Nil (0) Fathers 6 (4.5%) Mothers | 4.5% of mothers and no fathers met clinical cut-off for PTSD. Mothers who met the clinical cut-off for PTSD had a previous history of ASD. There was a relationship between PTSD and chronic guilt with guilt-proneness and fear of death as a predictor of psychological distress |
Galpin, 2013, United Kingdom; Cross-sectional Correlational study | Fathers (n = 30) Mothers (n = 53) | Fathers 31 Mothers 31 (Median) | Range 30–36 | Range 1500–3500 | IES-R DSM-IV (Self-report) | 33 | The experience of having a premature baby hospitalized on the neonatal unit | 4–8 weeks post-discharge | 1 (3%) Fathers 10 (19%) Mothers | 19% of mothers and 3% of fathers met the clinical cut-off for probable PTSD. This study demonstrated positive correlations between PTSD and Post traumatic growth |
Lefkowitz, 2010, United States of America; Prospective study | Fathers (n = 25) Mothers (n = 60) | Fathers 33 Mothers 29 | Range < 30 and ≥ 30 | NR | PCL DSM-IV (Self-report) | One or more re-experiencing symptoms, three or more avoidance symptoms, and two or more arousal symptoms over the past month | Their infant's admission to the NICU | T2— ≥ 30 days post-admission (Median days 33) | 2 (8%) Fathers 9 (15%) Mothers | 15% of mothers and 8% of preterm infants' fathers met the clinical cut-off for PTSD. Positive correlations of PTSD included a family history of depression, anxiety, serious mental illness, and ASD |
Lotterman, 2019, United States of America; Longitudinal study | Mothers (n = 76) | 32.45 | 33.53 | NR | PCL DSM-IV (Self-report) | 38 | During hospitalization | T2—6 months | 15.8% Mothers | At 6 months, 15.8% of mothers of preterm infants met the clinical cut-off for symptoms of PTSD. There were no differences in symptoms at baseline and again at 6 months |
Schecter, 2020, United States of America; Longitudinal prospective study | Mothers Fathers (n = 80) | NR | 29% Extremely Preterm (< 28) 33% Very Preterm (28 to < 32) 38% Moderate to Late Preterm (33 to 37 weeks) 9% Full-term (> 37 weeks) | NR | PCL-C DSM-IV (Self-report) | > 30 | First day in the NICU and first week in the NICU | < 1 year and > 1 year | 9% Fathers 17% Mothers | 17% of mothers and 9% of fathers met the clinical cut-off for symptoms of PTSD at 12 months follow-up. There were no statistical differences in PTSD symptoms across gestational age or in mothers or fathers |
Shaw, 2009, United States of America; Prospective study | Mothers Fathers (n = 18) | Fathers 37 Mothers 33.96 | 30.89 | 1664.39 | DTS DSM-IV (Self-report) | 38 and 39 | Their reactions to having an infant hospitalized in the NICU | T2—4 months | 2 (33%) Fathers 1 (9%) Mothers | 33% of fathers and 9% of mothers met the clinical cut-off for symptoms of PTSD at 4 months. Significant correlations were found between ASD and PTSD |
Shaw, 2013, United States of America; Longitudinal study | Mothers (n = 50) | Mothers 32.7 | 31.9 | 1757 | DTS DSM-IV (Self-report) | ≥ 40 | During or after having an infant in the NICU | T2—1 month after discharge from hospital | 15 (30%) Mothers | 30% of mothers of preterm infants met the clinical cut-off for probable PTSD. Correlations of PTSD include ASD, dysfunctional coping, and years of education |
Appendix 3: PRISMA 2020 Checklist
Section and topic | Item # | Checklist item | Location where item is reported |
|---|---|---|---|
TITLE | |||
Title | 1 | Identify the report as a systematic review | 1 |
ABSTRACT | |||
Abstract | 2 | See the PRISMA 2020 for Abstracts checklist | 1 |
INTRODUCTION | |||
Rationale | 3 | Describe the rationale for the review in the context of existing knowledge | 4 |
Objectives | 4 | Provide an explicit statement of the objective(s) or question(s) the review addresses | 5 |
METHODS | |||
Eligibility criteria | 5 | Specify the inclusion and exclusion criteria for the review and how studies were grouped for the syntheses | 5 and 7 |
Information sources | 6 | Specify all databases, registers, websites, organizations, reference lists, and other sources searched or consulted to identify studies. Specify the date when each source was last searched or consulted | 5 |
Search strategy | 7 | Present the full search strategies for all databases, registers and websites, including any filters and limits used | Appendix 1 |
Selection process | 8 | Specify the methods used to decide whether a study met the inclusion criteria of the review, including how many reviewers screened each record and each report retrieved, whether they worked independently, and if applicable, details of automation tools used in the process | 6 |
Data collection process | 9 | Specify the methods used to collect data from reports, including how many reviewers collected data from each report, whether they worked independently, any processes for obtaining or confirming data from study investigators, and if applicable, details of automation tools used in the process | 6–7 |
Data items | 10a | List and define all outcomes for which data were sought. Specify whether all results that were compatible with each outcome domain in each study were sought (e.g., for all measures, time points, analyses), and if not, the methods used to decide which results to collect | 6–7 |
10b | List and define all other variables for which data were sought (e.g., participant and intervention characteristics, funding sources). Describe any assumptions made about any missing or unclear information | 6–7 | |
Study risk of bias assessment | 11 | Specify the methods used to assess risk of bias in the included studies, including details of the tool(s) used, how many reviewers assessed each study and whether they worked independently, and if applicable, details of automation tools used in the process | 7 |
Effect measures | 12 | Specify for each outcome the effect measure(s) (e.g., risk ratio, mean difference) used in the synthesis or presentation of results | 6–7 |
Synthesis methods | 13a | Describe the processes used to decide which studies were eligible for each synthesis (e.g., tabulating the study intervention characteristics and comparing against the planned groups for each synthesis (item #5)) | 6–7 |
13b | Describe any methods required to prepare the data for presentation or synthesis, such as handling of missing summary statistics, or data conversions | 6–7 | |
13c | Describe any methods used to tabulate or visually display results of individual studies and syntheses | 6–7 | |
13d | Describe any methods used to synthesize results and provide a rationale for the choice(s). If meta-analysis was performed, describe the model(s), method(s) to identify the presence and extent of statistical heterogeneity, and software package(s) used | N/A | |
13e | Describe any methods used to explore possible causes of heterogeneity among study results (e.g., subgroup analysis, meta-regression) | N/A | |
13f | Describe any sensitivity analyses conducted to assess robustness of the synthesized results | N/A | |
Reporting bias assessment | 14 | Describe any methods used to assess risk of bias due to missing results in a synthesis (arising from reporting biases) | 7 |
Certainty assessment | 15 | Describe any methods used to assess certainty (or confidence) in the body of evidence for an outcome | N/A |
RESULTS | |||
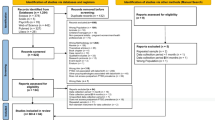
Study selection | 16a | Describe the results of the search and selection process, from the number of records identified in the search to the number of studies included in the review, ideally using a flow diagram | 7 and Fig. 1 |
16b | Cite studies that might appear to meet the inclusion criteria, but which were excluded, and explain why they were excluded | 7 | |
Study characteristics | 17 | Cite each included study and present its characteristics | Table 1 |
Risk of bias in studies | 18 | Present assessments of risk of bias for each included study | 7 |
Results of individual studies | 19 | For all outcomes, present, for each study: (a) summary statistics for each group (where appropriate) and (b) an effect estimate and its precision (e.g., confidence/credible interval), ideally using structured tables or plots | N/A |
Results of syntheses | 20a | For each synthesis, briefly summarize the characteristics and risk of bias among contributing studies | |
20b | Present results of all statistical syntheses conducted. If meta-analysis was done, present for each the summary estimate and its precision (e.g., confidence/credible interval) and measures of statistical heterogeneity. If comparing groups, describe the direction of the effect | N/A | |
20c | Present results of all investigations of possible causes of heterogeneity among study results | 8 | |
20d | Present results of all sensitivity analyses conducted to assess the robustness of the synthesized results | N/A | |
Reporting biases | 21 | Present assessments of risk of bias due to missing results (arising from reporting biases) for each synthesis assessed | Figure 2 |
Certainty of evidence | 22 | Present assessments of certainty (or confidence) in the body of evidence for each outcome assessed | N/A |
DISCUSSION | |||
Discussion | 23a | Provide a general interpretation of the results in the context of other evidence | 9 |
23b | Discuss any limitations of the evidence included in the review | 10 | |
23c | Discuss any limitations of the review processes used | 10 | |
23d | Discuss implications of the results for practice, policy, and future research | 9–10 | |
OTHER INFORMATION | |||
Registration and protocol | 24a | Provide registration information for the review, including register name and registration number, or state that the review was not registered | 1, 5 |
24b | Indicate where the review protocol can be accessed, or state that a protocol was not prepared | 5 | |
24c | Describe and explain any amendments to information provided at registration or in the protocol | 5 | |
Support | 25 | Describe sources of financial or non-financial support for the review, and the role of the funders or sponsors in the review | 10 |
Competing interests | 26 | Declare any competing interests of review authors | 10 |
Availability of data, code and other materials | 27 | Report which of the following are publicly available and where they can be found: template data collection forms; data extracted from included studies; data used for all analyses; analytic code; any other materials used in the review | 10 |
Rights and permissions
About this article
Cite this article
McKeown, L., Burke, K., Cobham, V.E. et al. The Prevalence of PTSD of Mothers and Fathers of High-Risk Infants Admitted to NICU: A Systematic Review. Clin Child Fam Psychol Rev 26, 33–49 (2023). https://doi.org/10.1007/s10567-022-00421-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10567-022-00421-4